133 Molesworth Street
PO Box 5013
Wellington 6140
New Zealand
T+64 4 496 2000
16 December 2020
L. Nichols
By email: [FYI request #13450 email]
Ref:
H202007785
Dear L. Nichols
Response to your request for official information
Thank you for your request under the Official Information Act 1982 (the Act) which was
transferred by the Central Region Technical Advisory Services Limited (TAS) to the Ministry of
Health on 14 October 2020. On 12 November 2020, the due date for responding to this request
was extended under section 15A of the Act, as further consultation was required.
You asked for information relating to the Ambulance Service Level Collaboration Charter (the
Charter) and the Terms of Reference (the ToR). You also requested information relating to the
‘New Zealand Ambulance Sector Design Working Group’. I wish to inform you that the latter
group does not exist.
The Ambulance Service Level Collaboration was set up to strengthen the interface between key
funders of ambulance services. The key funders are the Ministry of Health, Accident
Compensation Corporation (ACC) and the 20 district health boards (DHBs).
Your request included named individuals who are not connected to the Collaboration, but who
are members of a Clinical Governance Design Working Group (CGD Working Group). The CGD
Working Group was established by the National Ambulance Sector Office (NASO) to consider
and advise on how ‘clinical governance’ can better operate as part of the emergency ambulance
sector and improve the quality of patient care. There is no direct relationship between the CGD
Working Group and the Ambulance Service Level Collaboration.
A copy of your full request and information in response to each question is outlined in Appendix
One of this letter.
I trust this information fulfils your request. Under section 28(3) of the Act you have the right to
ask the Ombudsman to review any decisions made under this request. The Ombudsman may
be contacted by email at:
[email address] or by cal ing 0800 802 602.
Please note that this response, with your personal details removed, may be published on the
Ministry of Health website at:
www.health.govt.nz/about-ministry/information-
releases/responses-of icial-information-act-requests.
Yours sincerely
Clare Perry
Acting Deputy Director-General
Health System Improvement and Innovation
Appendix One
# Requested information
Response
1
“Please provide a copy of the Final
The Charter and ToR for the Ambulance
Draft of the Ambulance Service
Service Level Collaboration are available at:
Collaboration Charter ("The Charter")
https:/ www.health.govt.nz/new-zealand-health-
and the Terms of Reference for this
system/key-health-sector-organisations-and-
Collaboration ("The ToR").”
people/national-ambulance-sector-office-
naso/emergency-ambulance-services-
eas/ambulance-service-level-collaboration.
This part of your request is therefore refused
under section 18(d) of the Act, as the
information requested is publicly available.
2
“Please provide any briefing papers,
One document titled
‘Options Paper –
internal memos and discussion
Collaboration Charter and Terms of Reference
documents relating to the Charter and – June 2020’ has been identified in scope of
the TOR.”
this part of your request. This is being released
with some information withheld under section
9(2)(g)(i) of the Act, to maintain the ef ective
conduct of public affairs through the free and
frank expression of opinions by or between
members of an organisation during the course
of their duty.
This was a working draft that provided options
for consideration on the form and function of a
collaborative arrangement between the three
ambulance funders, that being ACC, the
Ministry, and the 20 DHBs facilitated through
TAS.
3
“Please disclose authorship of The
The contributing authors of the Charter and the
Charter and The TOR. If external input ToR were ACC, the Ministry of Health, and the
from other groups, agencies or
20 DHBs facilitated through TAS. TAS is an
organisations has occurred directly or agency of the 20 DHBs.
indirectly, in making contributions to
The Charter and/or The TOR, please
make this clear, on a section by
section basis where possible. Please
outline on what basis such input has
been used.”
4
“If The Charter and The TOR have
There is no ‘New Zealand Ambulance Sector
been shared, published, socialised or
Design Working Group’. There is a CGD
disclosed elsewhere, with any
Working Group, which is a NASO-initiated
individuals, organisations or groups
group to consider and advise on how ‘clinical
outside the NZ Ambulance Sector
governance’ can better operate in the
Design Working Group or TAS, please emergency ambulance sector and improve the
disclose this, AND which individuals,
quality of patient care. There is no direct
organisations or groups these
relationship between the CGD Working Group
documents have been shared with (eg and the Ambulance Service Level
professional associations, clinical
Collaboration.
networks, professional medical
colleges, or
As noted in the response to part 1 of your
committees/subcommittees of any of
request, the Charter and the ToR for the
those bodies or groups). Please also
Ambulance Service Level Collaboration were
disclose in each/any instance where
made publicly available on the Ministry of
this has happened, the date when The Health website on 8 October 2020. Prior to
Charter and The TOR have been first
being made publicly available, the Charter and
made available to such individuals,
the ToR were not shared with any other party
organisations or groups.”
outside of ACC, the Ministry of Health and the
20 DHBs facilitated through TAS.
5
“If The Charter and The TOR have not As noted in the response to part 1 of your
been made available to other
request, the Charter and the ToR for the
representative bodies for all the
Ambulance Service Level Collaboration were
relevant and readily identifiable
made publicly available on the Ministry of
medical (PRIME GPs, General
Health website on 8 October 2020. Prior to
Practice, Urgent Care, Rural
being made publicly available, the Charter and
Hospitalist Doctors, ICU, Anaesthetics the ToR were not shared with any other party
and Emergency Medicine Specialist
outside of ACC, the Ministry of Health and the
representative groups or professional
20 DHBs facilitated through TAS.
colleges), nursing (NZNO, COASTN)
and paramedic (St John Ambulance,
The Charter and the ToR guide group members
Wellington Free Ambulance, and the
that are party to the Ambulance Service Level
many aeromedical provider
Collaboration. These parties include the
organisations) sectors in NZ, please
Ministry of Health, ACC and the 20 DHBs as
clarify who made this decision, and on they are the key ambulance services funders.
what basis.”
6
“In addition, if The Charter and The
TOR have not been made available to
the member organisations of
Ambulance NZ, please clarify who
made this decision, and on what
basis.”
7
“Please clarify the role TAS have had As an agency of the 20 DHBs, the role of TAS
in developing The Charter and The
during the development of the Charter and the
TOR, and the role that TAS have had
ToR was to coordinate their feedback. The
in any decisions to disclose, share,
CGD Working Group is a NASO-initiated group
publish or socialise these documents
to consider and advise on how ‘clinical
outside TAS and the NZ Ambulance
governance’ can better operate as part of the
Sector Design Working Group.”
emergency ambulance sector and improve the
quality of patient care. The CGD Working
Group is not involved in the ‘ambulance
collaboration’ that is the subject of this request
for information and is not involved in wider
‘Ambulance Sector’ design.
As noted in response to parts 4, 5 and 6 of your
request, the Charter and the ToR for the
Ambulance Service Level Collaboration were
publicly released on the Ministry website on 8
October 2020.
8
“Please clarify if TAS staff have
The CGD Working Group is a NASO initiated
reviewed a copy of the Conflict of
group to consider and advise on how ‘clinical
Interest register for either the NZ
governance’ can better operate as part of the
Ambulance Sector Design Working
emergency ambulance sector and improve the
Group, or any other groups or
quality of patient care. The CGD Working
organisations that The Charter or The Group is not involved in the ‘ambulance
TOR may have been shared with,
collaboration’ that is the subject of this request
AND if these COI registers have been for information and has not been involved in
considered in making decisions to
wider ‘Ambulance Sector’ design. The Charter
disclose/share The Charter and/or The and the ToR were not shared with the CGD
TOR.”
Working Group.
9
“Please provide all emails, either to or The ‘New Zealand Ambulance Sector Design
from staff in TAS, in relation to
Working Group’ does not exist. The Ministry
developing, and in relation to sharing, has no record of any communication between
disclosing, publishing or socialising
the Ambulance Service Level Group and the
these documents outside TAS and the CGD Working Group (Mr David Waters, Dr Alex
NZ Ambulance Sector Design Working Psirides, Dr Tony Smith, Dr Grant Christey, and
Group, including all emails to or from
Ms Norma Lane) nor any record of documents
the members of the NZ Ambulance
or emails concerning the Charter of the ToR
Sector Design Working Group on
being disclosed, shared, published or socialised
these matters, from January 1 2020,
with the CGD Working Group. As such, this part
until the date of this request. (The
of your request is refused under section 18(g)
members of the NZ Ambulance Sector of the Act, as the information requested is not
Design Working Group are Mr David
held by the Ministry or another agency subject
Waters, Dr Alex Psirides, Dr Tony
to the Act.
Smith, Dr Grant Christey, and Ms
Norma Lane).”
10 “Please provide all emails on this AND
on all other matters, either to or from
TAS Staff, to or from the members of
the NZ Ambulance Sector Design
Working Group, in relation to this or
any other matters, from 1 January
2020 until the date of this request.”
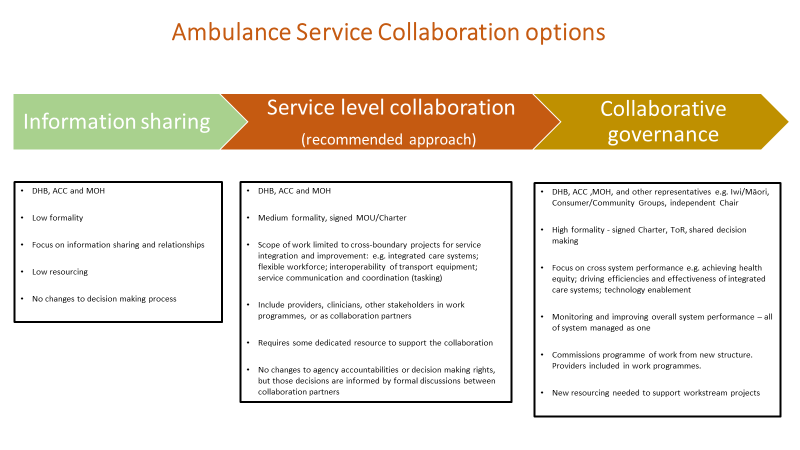
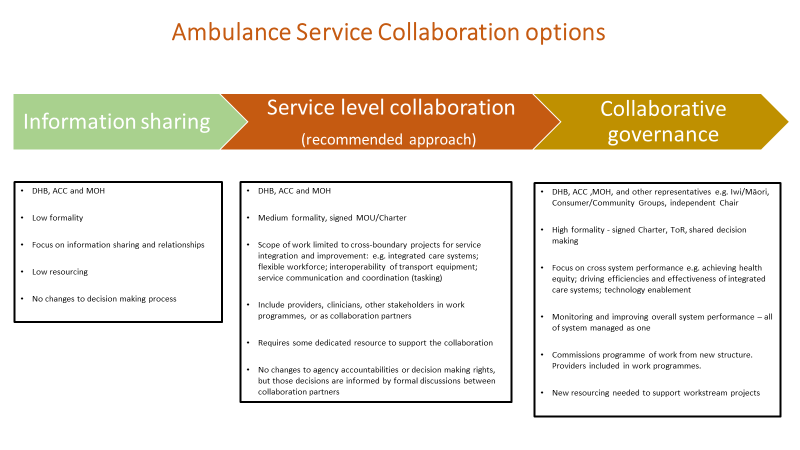
At the last meeting of the executive leads, the following decisions were made:
1. To initially focus the collaboration on the middle of the options below, with the desire to
move to a more inclusive collaborative governance model over time. Suggested timeframe
was 12-18 months.
1982
Act
Information
2. To appoint an independent Chair.
3. To provide a modest resource for secretariat support, location TBC.
4. Not to include broader participation immediately, but expect the individual organisations
leading each project to apply the RASCI approach to identify what groups should be included
and how.
5. That additional consultation with DHBs was not required before the collaboration was put in
Official
place.
6. That success of the collaboration would be measured by increased trust and resilience,
having clear deliverables and outcomes, funding and service delivery being determined by
the
need not driven by providers,
Ambulance Service Collaboration Charter
Charter Statement
under
This document outlines our shared commitment, objectives and the key principles and rules of
engagement for the Ambulance Service Collaboration (the “Collaboration”) and may be used by any
other network/group within the Collaboration.
Question 1: Is there agreement that this ambulance governance charter may be
used across all levels/structures of the ambulance system?
What would
Released
Question 2: Should the charter statement reflect the starting point (service level) or desired end
point (broader cross sector model)?
Option one – reflects progression from initial service Option two -reflects end point of inclusive model
level
and service level as interim
The collaboration is an inclusive collaborative
The Collaboration is a service level collaboration
1982
governance structure. As it will take some time to
focused on projects that advance service integration establish this model, the interim form of the
and improvement. It is expected that the
collaboration will include only the Ministry of
collaboration will evolve toward a more
Health, ACC and DHBs.
Act
inclusive and collaborative governance structure
with a wider scope once the current parties have
been able to demonstrate its effectiveness.
The Collaboration is directed by members who have been appointed by their organisations to work
collectively towards the Collaboration’s goals. Members are not appointed as representatives of specific
organisations or communities of interest, but because collectively they provide a range of competencies
required for the Collaboration to achieve its mandate.
Information
Question 3:
Is this description of non-representative membership desirable? What implications does it have for
how parties nominate members? What implications does it have for the future state of the
collaboration where members will be specifically carrying a position or view of the group they
Official
represent (for example iwi or consumer members)
the
Parties
The parties to this Collaboration are the Ministry of Health, the Accident Compensation Corporation
and the 20 district health boards.
under
Purpose of this Charter
The purpose of this Charter is to guide the Collaboration’s organised approach for transformation
change that will ensure ambulance services are sustainable, safe and an effective part the wider health
system, contributing to better health outcomes for all New Zealanders.1
Released
1 In pursuit of this purpose, the parties will have regard to the the goals of the NZ Ambulance Service Strategy
(2010), and the broader objectives of the NZ primary care, health and disability strategies
To do this the Collaboration will focus on system improvement and performance of ambulance
services, including:
Question 4: Should the purpose be limited to what is within the direct influence of the parties, or
expanded to wider sector goals?
Option Two: a more expansive purpose
1982
Option One: a more limited purpose
• improving equity of access for Maori,
rural and vulnerable populations
• improving integration across systems and
• improving patient health outcomes at a
services
Act
population level
• improving information transparency and
• improving integration across systems and
ambulance service funding approach
services
• improving information transparency and
ambulance service funding approach
• managing strategic relationships across
ambulance services, the health sector,
and professional’s Colleges.
Information
Strategic Goal and Priorities
The Collaboration’s goal is to support increasingly integrated and coordinated ambulance services that
cross boundaries between primary, community and hospital services, delivering a seamless patient
journey that is implemented within a ‘Best for Patient, Best for System’ approach.
Question 5: Does the goal/priority statement above need to be expanded by the options below
Official
and is it fair/reasonable to measure the success of the collaboration against the achievement of
these goals?
the
Option One:
Option two: some or all of the following statements
MOH, ACC and DHB health priorities
The Collaboration will achieve this goal through the
initial phase of establishment to a full ambulance service
under collaboration by:
• aligning our strategic areas of focus to government
health priorities and
• driving efficient, effective and safe services to
support good clinical governance, innovation and
plan collectively how to increase operational
efficiencies
• building capacity and capability of air ambulance
Released
services and transport systems at local, regional
and national levels
• enabling data and information sharing to improve
equity of access to air ambulance and health
services.
• striving for equitable access to ambulance and
healthcare services across all populations
Scope
The scope of the Collaboration is the interface between primary care and emergency ambulance and
DHB funded health services, including where the following services interact:
•
1982
Emergency Air Ambulance Services (EAAS)
• Emergency Road Ambulance Services (ERAS)
• Patient Transfer Services (PTS)
•
Act
Inter-Hospital Transfers (IHT)
• Primary Response in Medical Emergencies Service (PRIME)
• Communications Centres
• Telephone health advice and triage
• Interface between ambulance services, extended care pathways, Community Health, Primary
and Secondary Care, After Hours, Emergency Departments and Accident and Emergency Care
The following are out of scope of the Collaboration
• Emergency Response System e.g. NZ Police, Fire and Emergency NZ
• Core operational functions and Ministerial responsibilities of the Ministry of Health and ACC
Information
• Contract management arrangements, issues and day-to-day management of ambulance
services
Collaboration Principles
The foundation of the Charter is a commitment to act in good faith to reach consensus decisions
based on ‘Best for Patient, Best for System’. As members of the Collaboration we will conduct
Official
ourselves in a manner consistent with the following Collaboration principles, by:
• focusing on strategic decision making to support the purpose of the Collaboration
• making decisions by consensus, focusing on what is ‘Best for Patient, Best for System’ over the
the
long term
• supporting decisions made within the Collaboration, regardless of individual views
• conducting ourselves with honesty and integrity, and build a high-trust environment
• adopting an open and transparent approach to sharing information
•
under
respecting the rights, obligations and accountabilities of the members and their organisations
• holding each other to account for achievement of the objectives and demonstrating the
principles of the Collaboration.
Functions
Question 6: How expansive should the functions be? Would you expect this collaboration to drive
the work in response to a crisis (eg the issues that needed to be resolved in response to Covid-19)
and if so, does anything need to be added to allow for that?
Released
The functions of the Collaboration group are to:
Option One: More limited functions
Option Two: functions in option one, plus
• provide direction and monitoring of the
• provide system leadership, building
agreed programme of work
sustainability, resilience and connections
• commission and authorise resourcing for
relevant to the agreed work programmes
agreed joint projects from within
of the NASO and DHBs
representative’s organisations
• provide strategic advice in support of the
• receive high-level reporting on strategic
national ambulance strategic programme
projects and clinical governance
and provide advice to NASO within the
1982
decisions
mandate set by Ministers, the ACC Board
• request and receive advice to / from the
and national DHB Chief Executives Group
National Ambulance Clinical Network and
Act
other relevant groups. Note: this group
has not yet been established
Decision making
Question 7: Given the nature of the authorising environment, particularly Government Agency’s
responsibilities as advisors to Ministers, should the following statement on the limitations of the
Collaboration’s decision making be included?
Information
Nothing in this Charter changes the existing accountabilities, funding arrangements, decision making
rights, or legal obligations of any agency. Decisions are made by the Collaboration within the
mandate each member holds on behalf of their agency and/or Minister. Decisions that fall outside of
existing mandates will be referred to the appropriate decision maker, as required. Collaboration
members will provide advice to the relevant decision maker that includes the views of the
Official
Collaboration.
the
Evaluation of the Collaboration
This Collaboration will be reviewed in 12 – 18 months, by members, to evaluate its performance
against the Charter principles, functions and Terms of Reference objectives. Learnings from the
under
service level collaboration phase will inform any changes to this Charter and the Collaboration Terms
of Reference.
Members signed up to the Charter
Released
Name:
Signature:
Date:
1982
Appendix
s 9(2)(g)(i)
Act
Information
Official
the
under
Released
s 9(2)(g)(i)
1982
Act
Information
Official
the
under
Released
Ambulance Service Level Collaboration Terms of Reference
The Ambulance Service Collaboration Group (The Group).
Introduction
Question 9: is an introduction to the TOR necessary, if so, is the text below accurate and sufficiently
concise?
1982
s 9(2)(g)(i)
Act
Information
Official
the
under
Purpose
The Group will be responsible for the establishment and leadership of the service level collaboration,
to lead and guide the strategic programme for system integration.
The Group will provide leadership and direction for integrated and coordinated ambulance services
through clinically-led service development and implementation within a ‘best for patient, best for
system’ approach.
Released
In the first instance the Group’s priority is to approve a strategic programme and where required
this may include determining the feasibility of projects, implementation plans and agreed outcomes.
The Group will work with the DHB/ACC strategic relationship governance group and the NASO
2 Fixed wing refers to pre-hospital transportation by ambulance services
leadership group to agree the strategic programme. Implementation of the strategic programme
remains the responsibility of the relevant organisations (DHB, ACC, MoH and NASO).
Question 10: Is the highlighted text above necessary, the function to agree a work programme is
already listed in the Charter
1982
The Ambulance Service Collaboration Charter outlines the scope, functions and the principles for
working.
Act
Membership
Independent Chair
DHB executive leader
ACC executive leader
MoH executive leader
Ex-offico (in attendance)
Secretariat support
NASO manager, when invited
Information
DHB strategic advisor / DHB ambulance programme, when invited
Project leads, when invited
Question 11:
Official
Chair – The executive group previously agreed to an independent chair, does this remain the wish of
the group?
the
At this point in the establishment of the Collaboration, would membership be extended beyond ACC,
MOH and DHB representatives? If so, who of the following and are there others?
Road and Air ambulance providers
Community
under
Iwi
Health Consumer
Clinical Network Chair (noting this is not yet established)
Member Roles and Responsibilities
Released
Question 12: Is the level of detail of the roles and responsibilities of the Chair and members
necessary? – the behaviours are outlined under the collaboration principles in the Charter
document. The role of the secretariat would be retained.
The Chair of the Group will have responsibility for:
• chairing the meetings
• managing the process of conflict resolution and holding Group members to the
Collaboration Charter principles
• facilitating Group discussion and summing up key themes to reach decisions
• summing up key messages/outputs of meetings to the Group
• ensuring the Group stay focused to the purpose and expected outcomes
• working with relevant programme leads and secretariat support to set Group agendas
1982
Roles and responsibilities of Group members
• supporting clinical leadership, in particular promoting an environment for working together
Act
to reach decisions that ensure ‘best for system, best for patient’
• fostering an open and transparent approach to sharing information including reporting of
the Collaboration work programme and achievements
• communicating to agreed parties key messaging following meetings
• working with relevant teams/groups to support system improvements
• following through on assigned/delegated actions from Group meetings
Role and responsibilities of the Group’s secretariat support
The DHBs, ACC and MOH will fund the secretariat support functions to the Group and will include
the following responsibilities:
Information
• ensuring that administrative support is provided to the Group
• taking minutes of the Group meetings and distributing draft copy to the chair and Group
members within one week of the meeting date
• preparing agendas in partnership with the chair and collating meeting papers, ensuring the
agenda and papers are circulated to Group members at least one week in advance
Official
• maintaining a meeting action register and member conflict of interest register
• dealing with correspondence on behalf of the chair
• scheduling meetings on an annual basis
the
Decision Making
The Group will aim for consensus decision making informed by good data and clinical expertise.
Communication and engagement responsibilities for the strategic programme, projects and
under
processes is defined through the Responsible, Accountable, Supported, Consulted, Informed (RASCI)
model. The RASCI shown in Appendix 1 is a living document and will be updated periodically.
Meetings
It is anticipated that Group meetings will initially be held monthly via
teleconference/videoconferencing as determined by key milestones. Meetings may be held less
frequently once the programme settles.
Released
Conflict of Interest
All members must agree to disclose any perceived or actual conflict of interest. This applies to any
and all existing and potential conflicts of interest.
Question 13: Is there a need for a dispute resolution process, or is this the role of the Chair?
Members will be required to sign the Charter document
Question 14: Is this statement necessary?
1982
Act
This terms of reference will be reviewed at the same time as the Charter (after 12-18 months).
Information
Official
the
under
Released
Document Outline