 Briefing to the
Incoming
Minister
Part A: The New Zealand Health and
Briefing to the
Incoming
Minister
Part A: The New Zealand Health and
Disability System
2020
health.govt.nz
Contents
Introduction
1
Summary
3
Our vision for the future is pae ora – healthy futures
5
Our vision for the future of the health and disability system is pae ora –
healthy futures
5
Our system is performing well for many New Zealanders as we move towards
our goal of pae ora – healthy futures
5
Health equity is central to achieving pae ora
6
The Ministry is committed to Te Tiriti o Waitangi and achieving pae
ora for Māori
9
COVID-19 emerged as the system already faced multiple long-term
challenges
11
Long-standing system chal enges are well-documented, including in the final
report of the Health and Disability System Review
11
COVID-19 remains as a significant challenge and provides an
opportunity for transforming the system
15
The Ministry has work underway to support transforming the system
and achieving pae ora
17
Leading the public health response to COVID-19 and delivering the
Government’s elimination strategy
17
Improving the performance of district health boards’ financial sustainability,
capital infrastructure, and employment relations bargaining
17
Implementing the Government’s response to He Ara Oranga (Report of the
Government Inquiry into Mental Health and Addiction) and transforming New
Zealand’s approach to mental health and addiction
18
And delivering work across seven focus areas to support the immediate
priorities
19
Medium term: Harnessing what is good and laying the foundations for
change
19
What next?
20
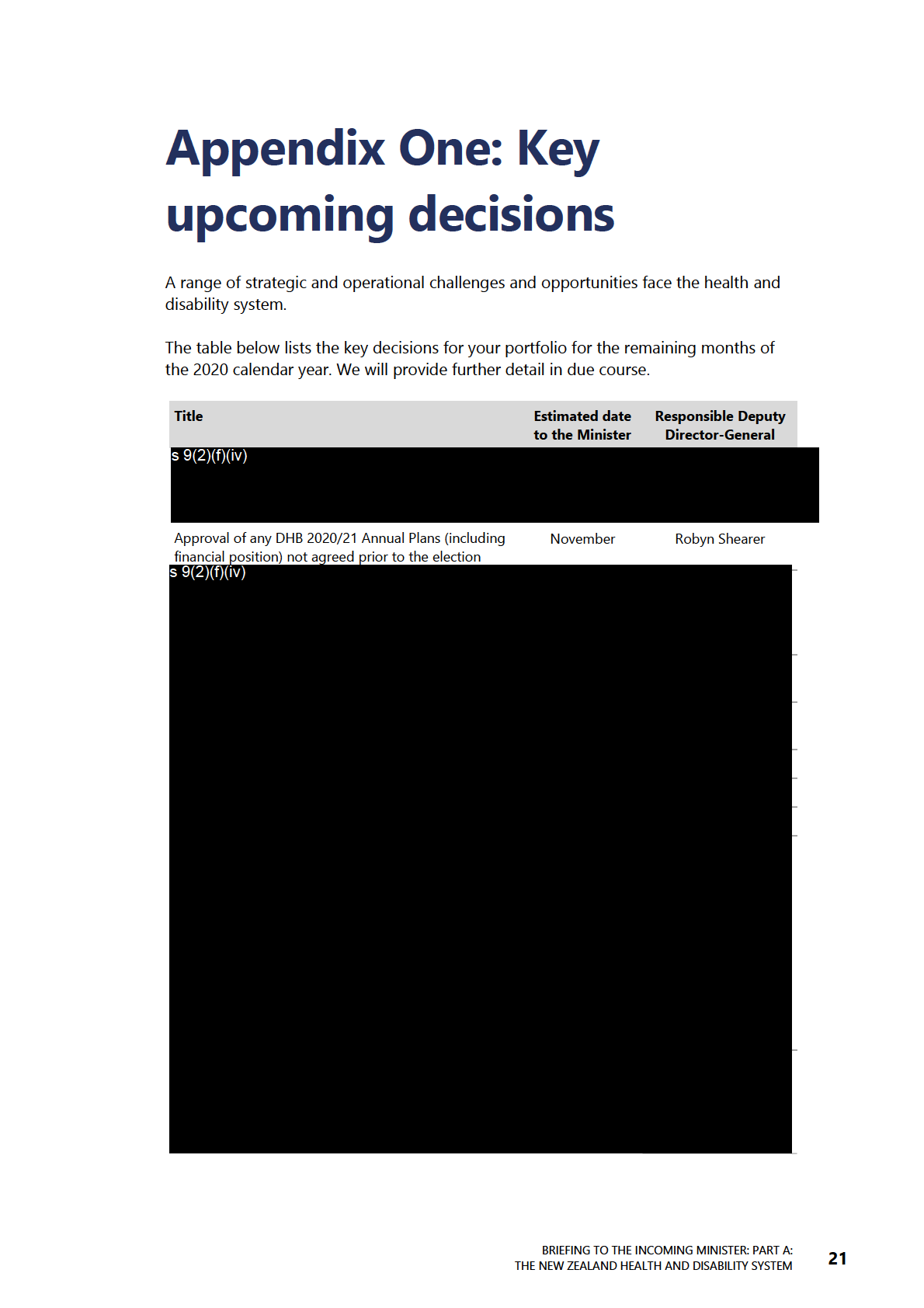
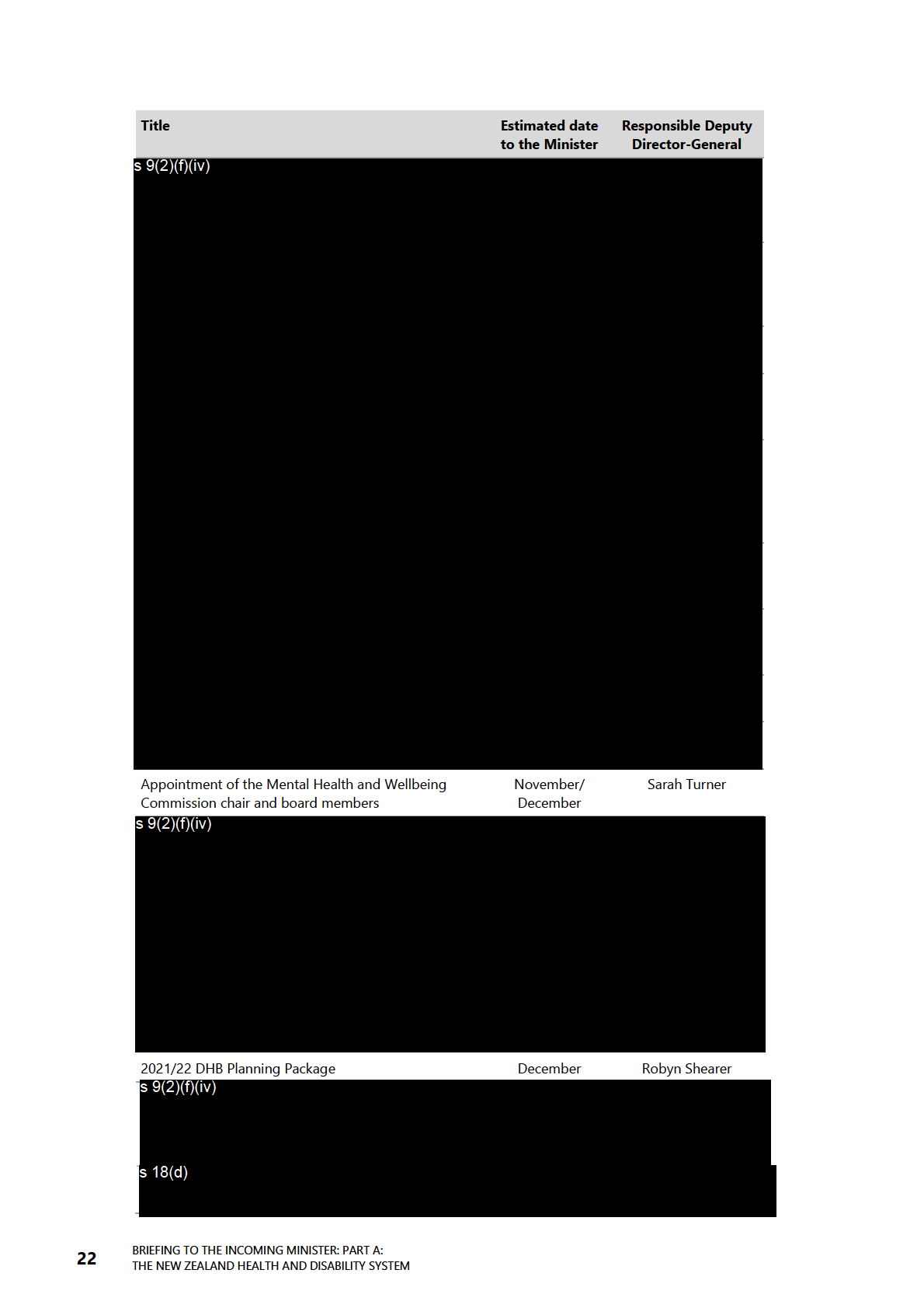
Appendix One : Key upcoming decisions
21
References
23
BRIEFING TO THE INCOMING MINISTER: PART A:
iii
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
List of Figures
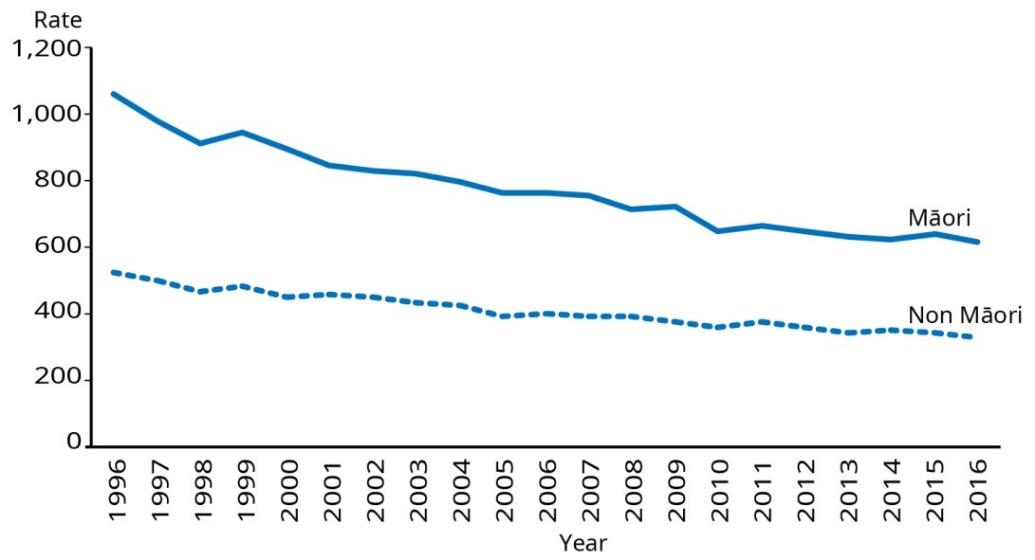
Figure 1: Mortality rates for Māori and non-Māori, 1996–2016
6
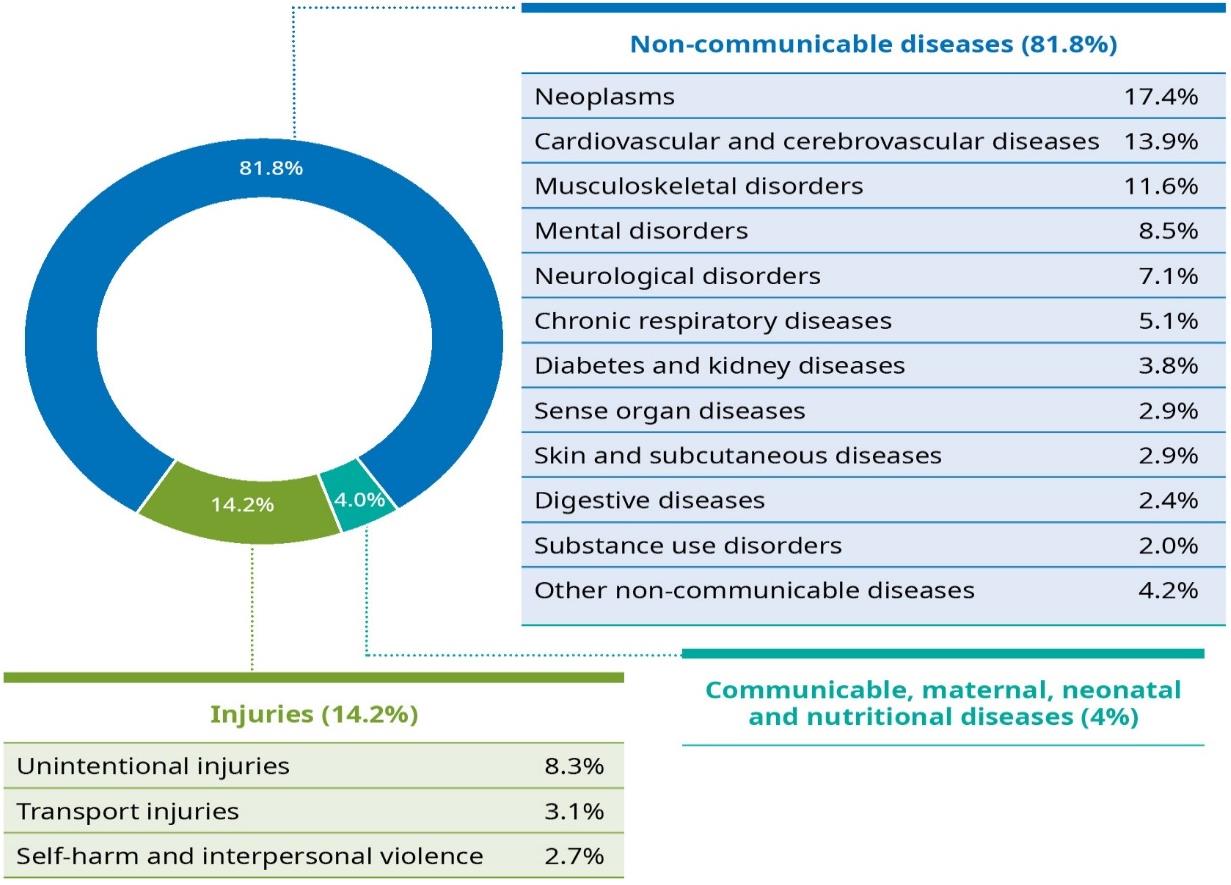
Figure 2: Contribution of various causes to overall disease burden
7
Figure 3: The determinants of health and their relative contribution to our health
outcomes
8
iv
BRIEFING TO THE INCOMING MINISTER: PART A:
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
Introduction
E te Minita, tēnā koe
Congratulations on your appointment as Minister of Health. The Ministry of Health is
committed to supporting you to implement the Government’s policy direction.
Our health and disability system – and the health of that system – have never been
more in the spotlight in New Zealand and international y than they are now. COVID-19
(KOWHEORI-19) is driving a new interest in ‘how are things working’ within our system
– and, of course, ‘how could they work better’.
Aotearoa New Zealand’s successful and adaptive response to COVID-19 has
demonstrated,
inter alia, the strengths of New Zealand’s health and disability system; it
has also highlighted areas for improvement that wil help us address some of our key
long-term challenges. The success to date provides a pointer for wider system change:
leadership, strongly engaging our committed workforce, both clinical and non-clinical;
and ongoing review and improvement.
Whilst we have achieved significant success to date in eliminating COVID-19 from our
communities, the pandemic remains a major focus for our work as its impacts will be
with us for some time to come. Alongside this, as a country we need to make rapid
progress on the key chal enges we face, many of which are global, around ongoing
inequities, workforce availability, the impact of non-communicable diseases, dealing
with complex public health problems, and funding.
The New Zealand health and disability system is complex and relies heavily on strong
and enduring relationships to ensure it delivers for New Zealanders. In this respect, it is
not unique and the challenges we are grappling with are shared with other countries
whether they are high, medium or low income. What is unique to New Zealand is the
need for a committed cultural approach, grounded in Te Tiriti o Waitangi
(Te Tiriti). The health and disability system has not always done a good job of meeting
its obligations to Māori under the Treaty and this is a core driver behind the Ministry’s
vision of pae ora – healthy futures, and our response to Hauora: Report on Stage One
of the Health Services and Outcomes Kaupapa Inquiry (WAI2575). We are committed
to doing better for Māori and other groups to ensure equity of access to, experience of
and outcomes from care.
Both the COVID-19 situation and the recent Health and Disability System Review (the
Review) provide a unique opportunity to refresh the strategic direction for the health
and disability system, to improve equity and shift the system towards a sustainable and
joined-up future that puts the wellbeing of New Zealanders at the centre. There is an
opportunity and imperative to ‘transform’, not just ‘reform’, the system. We are keen to
discuss your priorities for transformation and the pathway for change in the context of
COVID-19.
BRIEFING TO THE INCOMING MINISTER: PART A:
1
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
My leadership team and the wider Ministry look forward to meeting you and
supporting you as you take up your new portfolio.
Nāku noa, nā
Dr Ashley Bloomfield
Director-General of Health
2
BRIEFING TO THE INCOMING MINISTER: PART A:
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
Summary
Now is an important time for New Zealand’s health and disability system. The health
and wellbeing of New Zealanders is critical to the economic, social and cultural
wellbeing of the nation, communities and whānau.
Responding to the COVID-19/KOWHEORI-19 pandemic has chal enged the system like
never before. We have achieved success with our science-driven and adaptive
elimination strategy. Our response to COVID-19 has shown both the quality of our
workforce and, through them, the system’s ability to be agile and embrace change
under a clear common purpose and leadership. Looking ahead, COVID-19 and the
Health and Disability Review – Final Report – Pūrongo Whakamutunga provide an
opportunity to better serve people in New Zealand. While the overall health of New
Zealanders is generally improving – we are living longer in better health – we must
keep improving in order to achieve pae ora – healthy futures for all New Zealanders.
These improvements, including a stronger focus on prevention and population health,
are critical to address health inequity for Māori, Pacific peoples, disabled people and
other groups.
COVID-19 emerged as the health and disability system was already responding to
long-term challenges. Those challenges include: meeting the needs of a growing and
ageing population; how we work together and with our partners to prevent future il
health, especially from non-communicable diseases such as diabetes, heart disease and
cancers; strengthening leadership and accountability across the system; meeting our
obligations under Te Tiriti and ensuring equitable outcomes; training and retaining a
skilled and adaptable workforce; rebuilding and repairing our physical infrastructure;
and investing in transformative technology, particularly data and digital – all while
ensuring financial sustainability in a chal enging economic climate.
There are many assets to build on, including the strength of a highly skilled and deeply
committed workforce, successes and lessons from COVID-19, population-based
approaches and a wil ingness to innovate. In the near-term, this means responding
relentlessly to COVID-19 while improving district health board (DHB) performance and
implementing the Government’s response to He Ara Oranga (Report of the
Government Inquiry into Mental Health and Addiction). In the medium- to longer-term
there is opportunity to map out a pathway, initially in the context of COVID-19, to
position the system to better meet the health and disability needs of current and future
generations of people calling New Zealand/Aotearoa home. We are keen to discuss
your priorities for reform and the pathway for change.
As kaitiaki of this system and principal health advisor to the Government, the Ministry
wil work with you to improve the health and disability outcomes of New Zealanders
and deliver on the Government’s priorities for the health portfolio.
BRIEFING TO THE INCOMING MINISTER: PART A:
3
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
This document describes the strategic context and current state of the health and
disability system and the medium-term focus areas to meet the chal enges of the
future and to achieve the long-term vision of pae ora – healthy futures for all people in
New Zealand.
Appendix One provides a list of the initial key decisions for you as the incoming
Minister. A handbook of the organisations and responsibilities of the Health and
Disability System is included as Part B of this briefing. A series of secondary briefings
on COVID-19 and other priority issues wil be provided to you separately.
4
BRIEFING TO THE INCOMING MINISTER: PART A:
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
 Our vision for the future is
Our vision for the future is
pae ora – healthy futures
Our vision for the future of the health and
disability system is pae ora – healthy
futures
The concept of pae ora promotes the wellbeing of al New Zealanders and enables
them to improve or maximise their health and independence. Pae ora has three
elements, summarised below:
Our system is performing well for many
New Zealanders as we move towards our
goal of pae ora – healthy futures
Compared with other high-income countries, New Zealand performs relatively well on
overall population health indicators, and many continue to improve over time. For
example: New Zealanders are living longer and spending more years in good health;
infant mortality has reduced; smoking rates are declining, with very low rates among
teenagers; oral health for children is improving; cancer screening service coverage has
increased leading to early detection and earlier treatment; and amenable mortality
(which is associated with health system performance) decreased for all groups.
These improvements reflect important policy, funding and implementation decisions,
coupled with commitment of health system leaders, clinicians, planners and funders to
work with their communities and with Māori to change models of service delivery,
implement advances in treatments and health technologies, and deliver more
integrated services.
BRIEFING TO THE INCOMING MINISTER: PART A:
5
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
It is in this context the system has responded to the unprecedented international
challenge of COVID-19. Public health services have mobilised rapidly to monitor and
respond to the emergent threat, including delivering one of the highest per capita
testing rates in the world. Service models have been redesigned and reprioritised
where necessary to ensure sufficient overall capacity to deal with a surge in infections
(including ramping up contact tracing) and tailored approaches to delivering services
for Māori and Pacific peoples have been facilitated through government investment,
community involvement and service innovation.
Health equity is central to achieving pae ora
While strong overall progress on population health is being made, there are continued
inequitable outcomes for some groups, including Māori, Pacific peoples,
socioeconomically deprived people, rural people, disabled people and people with
mental health and addiction needs. As a result of COVID-19, there may also be
disproportionate impacts on these groups/regions depending on where outbreaks
occur. Life expectancy is increasing for Māori males and females, but remains 7.3 and
6.8 years below that of non-Maori males and females. Mortality rates are also falling
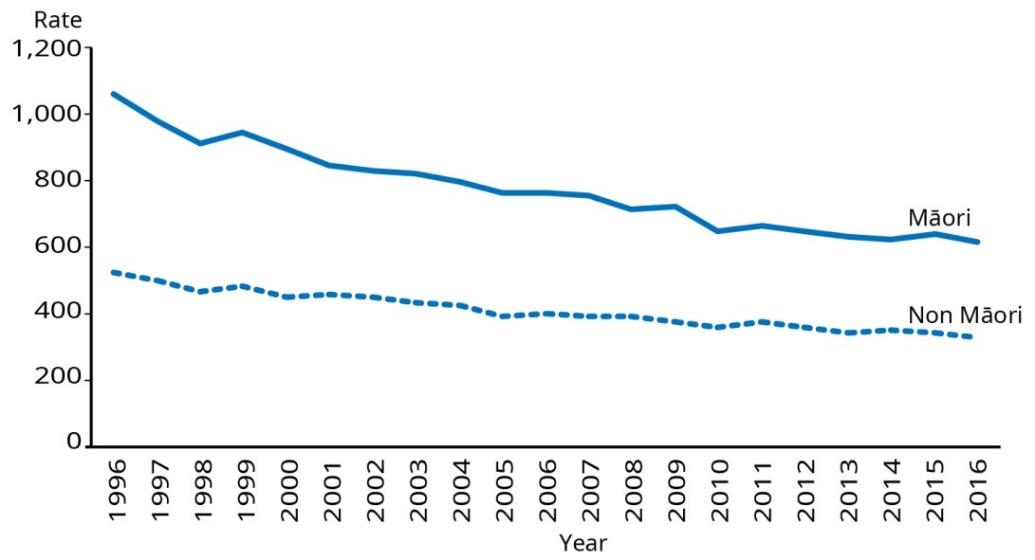
(improving) for Māori but remain higher than non-Māori (Figure 1).
Figure 1: Mortality rates for Māori and non-Māori, 1996–2016
In common with other high-income countries, non-communicable diseases (such as
cancer/neoplasms, cardiovascular disease and mental il ness) contribute the most to il
health and early death in New Zealand (81.8%) (Figure 2). These diseases are a
significant driver of health inequities for Māori, Pacific peoples and other groups and
are important risk factors for poor COVID-19 outcomes.
6
BRIEFING TO THE INCOMING MINISTER: PART A:
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
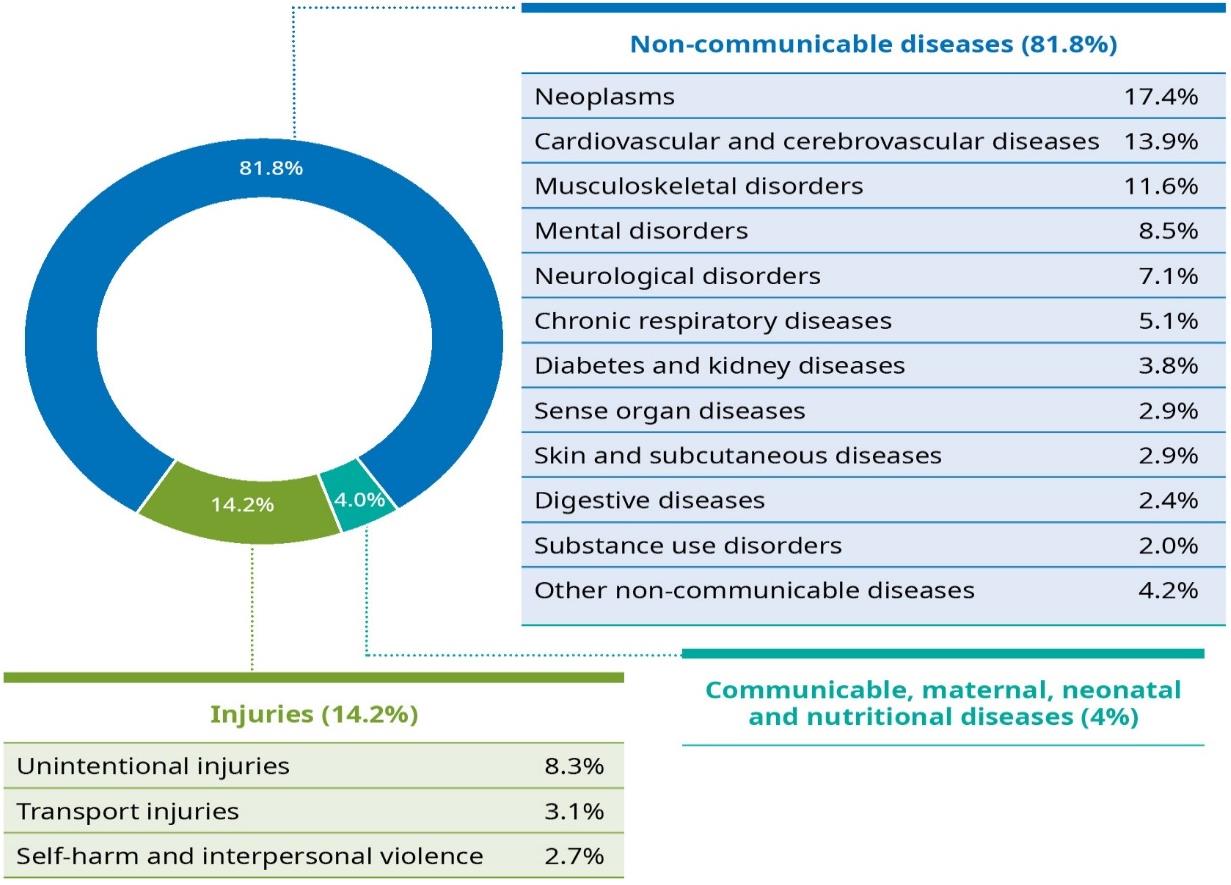 Figure 2: Contribution of various causes to overall disease burden
Figure 2: Contribution of various causes to overall disease burden
Source: Global Burden of Disease Collaborative Network, 2018
The wider determinants of health and wel being have an impact on
equitable health outcomes
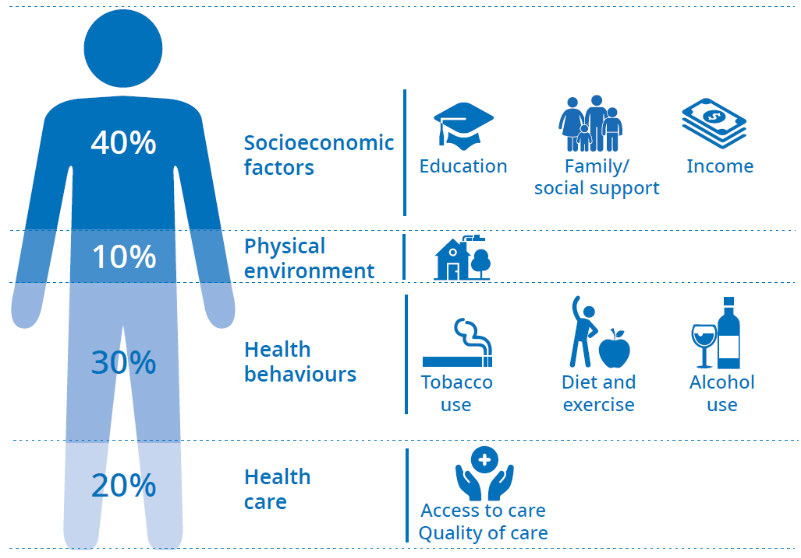
The wider determinants of health and wellbeing play a major role in overall health and
wellbeing (Figure 3). That is, people’s health is substantially influenced by the physical
environment, social and economic factors, culture, spiritual beliefs, and by their
behaviour. Individuals have varying levels of control over these determinants. In many
ways, these factors are structural – they are embedded in how our society functions
and so constrain the level of choice people have.
The health and disability system has an important role to play, working alongside other
agencies, to address these wider determinants of wel being. There is a range of
important work underway to support this in the health and disability system and
between agencies to address key health determinants such as reducing poverty,
improving educational outcomes, increasing access to healthy housing, reducing
homelessness and tackling family and sexual violence. Work is also underway to
support people to make healthy behaviours (such as improved nutrition, increased
physical activity and being smokefree) including working with industry and
strengthening/modernising regulatory settings.
BRIEFING TO THE INCOMING MINISTER: PART A:
7
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
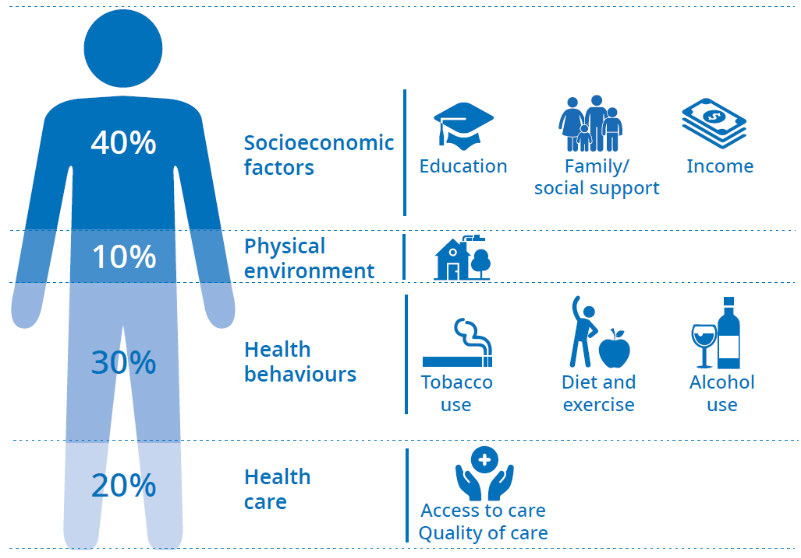 Figure 3: The determinants of health and their relative contribution to our health
Figure 3: The determinants of health and their relative contribution to our health
outcomes
Source: Adapted from the Institute for Clinical Systems Improvement (2014)
There are barriers to equitable health outcomes
There is a range of barriers to equitable health outcomes, including racism,
discrimination, cost, transport and information accessibility, that prevent some people
from having fair access to health services and disability supports. These inequities
reduce the resilience of our whole population to evolving and increasing demands on
the health system which are brought by demographic shifts, changing expectations,
and public health threats.
The Review defined racism as a social system based on historical and political
inequalities that results in systemic privileging of some groups over others, and found
that self-reported experiences of racism, including by health professionals, is higher for
Māori, Pacific peoples and Asian peoples compared with European/other people.
Contributing to these institutional barriers are low levels of Māori and Pacific
representation among the health workforce. Achieving equitable outcomes wil require
a deliberate investment in workforce and other initiatives that support fair access to,
experience of and outcomes from care and support.
8
BRIEFING TO THE INCOMING MINISTER: PART A:
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
The Ministry is committed
to Te Tiriti o Waitangi and
achieving pae ora for Māori
The Ministry is committed to fulfil ing the special relationship between Māori and the
Crown under Te Tiriti. The Ministry, as the kaitiaki of the health and disability system
(under article 1 of Te Tiriti), has the responsibility to enable Māori to exercise authority
over their health and wellbeing (under article 2) and achieve equitable health outcomes
for Māori (under article 3) in ways that enable Māori to live, thrive and flourish as
Māori.
The principles of Te Tiriti, as articulated by the Courts and the Waitangi Tribunal,
provide the framework for how we wil meet our obligations under Te Tiriti in our day-
to-day work. The 2019 Hauora report recommends the fol owing principles for the
primary health care system, which are also applicable to the wider health and disability
system.
•
Tino rangatiratanga: The guarantee of tino rangatiratanga, which provides for
Māori self-determination and mana motuhake in the design, delivery and
monitoring of health and disability services.
•
Equity: The principle of equity, which requires the Crown to commit to achieving
equitable health outcomes for Māori.
•
Active protection: The principle of active protection, which requires the Crown to
act, to the fullest extent practicable, to achieve equitable health outcomes for Māori.
This includes ensuring that it, its agents, and its Treaty partner are well informed on
the extent and nature of Māori health outcomes and efforts to achieve Māori health
equity.
•
Options: The principle of options, which requires the Crown to provide for, and
properly resource, kaupapa Māori health and disability services. Furthermore, the
Crown is obliged to ensure that all health and disability services are provided in a
culturally appropriate way that recognises and supports the expression of hauora
Māori models of care.
•
Partnership: The principle of partnership, which requires the Crown and Māori to
work in partnership in the governance, design, delivery and monitoring of health
and disability services. Māori must be co-designers, with the Crown, of the primary
health system for Māori.
BRIEFING TO THE INCOMING MINISTER: PART A:
9
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
Meeting our obligations under Te Tiriti is necessary to realise the overall aims of
He Korowai Oranga: Māori Health Strategy and achieve outcomes for the health and
disability system as a whole. The Ministry has developed action plans, including
Whakamaua: Māori Health Action Plan 2020-2025 (Whakamaua) and
Whāia Te Ao
Mārama 2018–2022: The Māori Disability Action Plan for tangata whāikaha (Māori with
disabilities) which serve to support these aims and set a direction to improve outcomes
for Māori. Whakamaua also positions the health and disability system to continue
protecting the health of iwi, hapū, whānau and Māori communities in the face of the
COVID-19/KOWHEORI-19 pandemic.
Improving access and outcomes in the health and disability system for Māori wil
require a transformation programme that invests early and in the right things to
support Māori individuals, whānau, hapū and iwi. This includes redirecting funding so
that it gets to communities and supporting Māori to take ownership in the design and
development of services that meet their needs and aspirations. Transformation is
already underway in mental health and addiction, where there has been significant
investment of Budget 2019 funding in primary mental health and addiction services.
Māori are identified as a priority population across al new service investment, but the
Ministry has also ringfenced 20 percent of funding available for service delivery
exclusively for kaupapa Māori services. The Ministry is trialling new approaches to
procuring kaupapa Māori services designed to align better with a Māori world view
and support the success of Māori providers.
10
BRIEFING TO THE INCOMING MINISTER: PART A:
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
COVID-19 emerged as the
system already faced
multiple long-term
challenges
Long-standing system challenges are well-
documented, including in the final report of
the Health and Disability System Review
The New Zealand health and disability system faces a range of cost pressures. These
include pressures from the response to COVID-19, as well as changes in demographics,
funding levels and patterns of il ness. Compared with some other high-income
countries (Schneider EC, Sarnak DO, Squires D, et al, 2017), New Zealand spends a
smal er share of national income on health care per capita, performs well in terms of
care process and administrative efficiency, but is lower ranked on equity (‘equity’ in this
study means the difference between low- and high-income adults on the 11 measures
related to timeliness, financial barriers to care and patient-centred care). However,
what we spend is only one part of the picture: we need to consider all of our levers,
and not just additional investment, to ensure that we use funding more effectively and
implement changes that move us closer to our vision of pae ora.
The health and disability system does not deliver equitable
outcomes for al
As noted above, there are inequitable outcomes for some groups, including Māori and
Pacific peoples. The system needs to work differently to meet our Te Tiriti obligations
and improve Māori health and social outcomes. The Review has recommended a Māori
Health Authority be established as an independent departmental agency advising the
Minister of Health. This recommendation wil be considered by the Transition Unit in
DPMC which is leading the provision of advice on the response to the Review. The
consideration of equity is now key to the work programme of the Ministry.
BRIEFING TO THE INCOMING MINISTER: PART A:
11
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
Demand for health and disability services is evolving and growing
Demand is driven by population growth and ageing, increasing complexity in
New Zealanders’ health- and disability-related needs and changing expectations of
what the system should deliver. Health funding has failed to keep pace with growing
demand since the Global Financial Crisis. For example, challenges such as the 2016
Havelock North campylobacter outbreak, the 2019 Measles outbreaks, the attack on
Christchurch Mosques and the Whakaari/White Island volcanic eruption have stressed
already stretched system capacity, including public health services. In August 2020, the
Ministry commenced a programme of work to establish a National Public Health
Service, to strengthen the system of public health in New Zealand to respond to
COVID-19 and other threats, and respond to the critical weaknesses identified in recent
reviews.
The system is complex with a high degree of devolved decision
making, with organisations not always col aborating around the
needs of individuals and communities
The Review notes the overlap in the functions of organisations and lack of clarity on
mandates which leads to duplication of effort, inefficiency and reduced accountability
for performance. Stronger national and regional service planning and commissioning,
particularly of specialist services, is needed. Calls for investment to be redirected within
the system have been documented in
He Ara Oranga, Hauora: Report on Stage One of
the Health Services and Outcomes Kaupapa Inquiry (WAI2575) and the Final Report of
the Review. At their core, these reports suggest both increased investment and a
significant shift in the way services are designed and funded, with a greater focus on
prevention and upstream investment on the individuals, families and populations who
use the system. These suggestions wil be considered in the response to the Review.
The aged care sector current system’s regulatory environment is a good example of
this chal enge. The environment is somewhat fragmented, involving different processes
and bodies, and it is difficult to achieve sufficient coordination and leadership of the
improvement work needed. The Ministry is developing advice on potential changes to
this environment and these changes wil be considered alongside the response to the
Review.
12
BRIEFING TO THE INCOMING MINISTER: PART A:
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
The health system is operating at capacity and COVID-19 has added
more pressure
COVID-19 Alert Levels 3 and 4 changed patterns in demand. Some areas saw demand
decrease eg, emergency department admissions. In other areas, the deferral of
services, alongside individuals delaying seeking care has led to a significant backlog,
eg, planned care interventions. All DHBs are focused on reducing the number of
patients waiting longer than intended for services and have seen some success, and
the Ministry is supporting DHBs with additional funding for service delivery and
improvement. However, timely access to planned care remains a chal enge and further
impacts are likely if COVID-19 alert levels increase in the future. Additional y, evidence
of demand patterns fol owing other significant events suggests that the effect of
COVID-19 on people’s mental wellbeing may result in an increased demand for mental
health and addiction services and social supports.
The supply and diversity of the workforce remains chal enging
Health and disability services are delivered by an aging and committed workforce of
more than 220,000, including doctors, nurses, allied health professionals and non-
regulated Kaiāwhina (care and support) workers. Currently, the Ministry and DHBs have
limited oversight of undergraduate training and education, which impact significantly
on overall health workforce supply.
The current workforce pipeline is vulnerable to economic and environmental impacts,
as seen during the COVID-19 response, which disrupted the flow of international
workers on whom our system heavily depends. The health and disability workforce
must adapt and respond rapidly to new technology and ways of working.
The health and disability workforce does not currently reflect the diversity of
New Zealand’s population. However, there are promising signs among Māori and
Pacific graduates of clinical training, particularly nursing.
The Ministry is also responsible for ensuring that employment relations decisions,
including bargained settlements, are made in line with the Government’s expectations.
This is a complex environment with many unions and col ective agreements. Effects
from settlements (for example, on pay equity) can flow on across the sector and
government. When combined with traditional workforce growth these factors are a
significant chal enge for developing and implementing models of care that al ow the
workforce to deliver services in different ways.
BRIEFING TO THE INCOMING MINISTER: PART A:
13
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
The system needs a clear investment pathway of both operating
and capital funding
Vote Health has grown from actual expenditure in 2015/16 of $15.280 billion to
budgeted expenditure in 2020/21 of $20.269 billion, an increase of $4.989 billion over
five years (Treasury, 2019, Vote Health). For the year ending June 2019, Health
accounted for 21 percent of total Core Crown Spending (Treasury, 2019, Financial
Statements). The Treasury Statement on the Long-Term Fiscal Position (2016) projected
that government spending on health would need to rise from 6.2 percent of GDP in
2015 to 6.8 percent in 2030 and 8.3 percent in 2045, just to maintain the current offer –
investment that wil only be achievable with significant trade-offs in other areas.
The financial performance of our DHBs varies and has deteriorated in recent years. The
fundamental driver of this was the cumulative impact of funding levels below those
needed to meet ongoing cost pressures. Higher levels of investment over the last three
years have stabilised the DHBs’ overall financial position, but some individual DHBs had
accumulated significant deficits. DHBs have reported an unaudited sector-wide deficit
of $874 million for the year ended 30 June 2020. After allowing for the impact of one-
off items not included in the 2019/20 Annual Plans, the result is an underlying deficit of
$497 million, which is in line with budget. Key drivers of DHB financial positions include
workforce costs, investment in technology and infrastructure, and significant full-time
equivalent growth in their provider arms. The Review cal ed for fewer DHBs and this
wil be considered in the work to respond to the Review.
Disability support services have also come under pressure in recent years due to the
increasing demand for support and the associated costs. There are also increasing
demand side pressures, for example increasing demand for access to rehabilitation
services such as cochlear implants for adults.
14
BRIEFING TO THE INCOMING MINISTER: PART A:
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
COVID-19 remains as a
significant challenge and
provides an opportunity for
transforming the system
The unprecedented internal challenge of COVID-19 has disrupted the norm but
showed the strengths of the system, led to new ways of working and resulted in a
number of positive outcomes.
We have achieved success with our science-driven and responsive elimination strategy.
New Zealand’s knowledge capital has played a critical role in our response to
COVID-19. Our science workforce supported our evidence-based approach with its
capacity to work across agencies and sectors and its ability to absorb evidence and
participate in international research and development networks. This approach has
been discussed international y and creates a model for a system where science and
evidence play a much stronger role in the design and evaluation of the health and
disability system and its performance.
The system showed its ability to be agile, adaptive and to embrace change under a
clear common purpose and leadership. Our public health, clinical and management
workforce was in the spotlight and demonstrated just how highly skilled and deeply
committed these people are to the health and disability support needs of
New Zealanders.
We have seen major progress in areas that had previously proven elusive, including in
the use of telehealth and virtual consultations. And new partnerships have been
established within and between organisations and their communities, with increased
participation leading to more effective, bespoke solutions. For example new ways of
working have led to an increase of Māori uptake of flu vaccinations, and food parcels
including health and hygiene packs.
The use of population-based approaches helped the system provide tailored support
to Māori and Pacific peoples which was crucial in the August 2020 outbreak. The
Ministry developed and implemented Māori and Pacific Health COVID-19 Response
Plans. The plans and their updates provide frameworks for protecting, preventing and
mitigating the impacts of COVID-19 within Māori and Pacific communities, including
actions supported by the Māori Health Funding Package and actions to facilitate
communication in Pacific communities.
BRIEFING TO THE INCOMING MINISTER: PART A:
15
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
We want to capitalise on the positive lessons of COVID-19. Opportunities for change
include shifts in technology; new care pathways; greater cross-sector and community
col aboration and focus on vulnerable populations; and maximising workforce capacity.
Risks include the health and psychosocial effects of COVID-19 on populations already
experiencing inequity in the health and disability system, the effect of an economic
downturn on the sustainability of services and supports and maintaining a workforce
while border controls are in place. The Ministry’s priorities reflect lessons learnt from
COVID-19 but also focus on maintaining the current system and preparing it for
reform.
16
BRIEFING TO THE INCOMING MINISTER: PART A:
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
The Ministry has work
underway to support
transforming the system
and achieving pae ora
Our immediate priorities are critical activities that maintain and improve the health of
New Zealanders and strengthen the current system alongside the COVID-19 response.
Our priorities for the
short term include:
Leading the public health response to
COVID-19 and delivering the Government’s
elimination strategy
To date, we have successfully implemented an elimination strategy in response to
COVID-19, meaning we continue to have a low number of cases. In the short term we
want to build on the successes of our approach while retaining the capacity and
capability to alter our response as required.
Improving the performance of district
health boards’ financial sustainability,
capital infrastructure, and employment
relations bargaining
DHB performance concerns have become more acute over the last few years, with
financial performance of many DHBs deteriorating and service performance metrics
falling below expectations in some cases. DHB performance must improve in these
areas to support better and more equitable health outcomes for New Zealanders. We
are delivering the DHB Performance Programme, which aims to strengthen
performance by improving the way we appoint, induct and develop leaders; the way
we lead system and service planning; the way we support innovation and
improvement; how we measure and monitor performance; how we engage with the
sector; and how we leverage performance through accountability frameworks.
BRIEFING TO THE INCOMING MINISTER: PART A:
17
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
Building system capacity to deliver health services for New Zealand’s growing and
ageing population is a priority. The Government has provided significant levels of
capital investment in recent years and supported the embedding of a new Health
Infrastructure Unit (established in November 2019) to support national asset
management planning, investment strategy and design and infrastructure
development. Currently we are overseeing or leading 88 health capital projects,
including major redevelopments such as the new Dunedin Hospital for Southern DHB.
The Ministry is also responsible for ensuring that employment relations decisions,
including bargained settlements, are made in line with the Government’s expectations.
This is a complex environment with many unions and col ective agreements. Effects
from settlements (for example, on pay equity) can flow on across the sector and
government. The significant chal enge is developing and implementing models of care
that al ow our workforce to deliver services in different ways.
Implementing the Government’s response
to He Ara Oranga (Report of the
Government Inquiry into Mental Health and
Addiction) and transforming New Zealand’s
approach to mental health and addiction
The Ministry is progressing work to implement the Government’s response to
He Ara
Oranga (Report of the Government Inquiry into Mental Health and Addiction). He Ara
Oranga called for urgent action to transform New Zealand’s approach to mental health
and addiction and ensure that people have more options for accessing the support
they need, when and where they need it. This work is more important now than ever as
it wil support our recovery from the psychosocial impacts of the COVID-19 pandemic.
Work is under way to deliver the substantial Budget 2019 mental wellbeing package.
This includes expanding access to and choice of primary mental health and addiction
services and how these services can be integrated into different settings, eg, schools.
Work is also underway to update the long-term pathway to guide and sequence
actions to implement the response to He Ara Oranga. This pathway wil reflect the
post-COVID-19 environment, building on the actions outlined in the national
psychosocial and mental wellbeing recovery plan, Kia Kaha, Kia Māia, Kia Ora Aotearoa.
18
BRIEFING TO THE INCOMING MINISTER: PART A:
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
And delivering work across seven focus
areas to support the immediate priorities
We want to take steps now to embed the strategic direction of the Review, lessons
learnt from COVID-19, in preparation for the Government’s response to the detailed
recommendations of the Review. Accordingly, the Ministry has identified the fol owing
set of action areas to progress in the next year. Many wil help address long-standing
known issues and contribute to improving inequity of health outcomes.
1.
Commissioning for better health outcomes for Māori and all New Zealanders
2.
Strengthening system leadership at all levels
3.
Strengthening public health services
4.
A modern, digitally enabled health system
5.
Improving delivery of primary and community care
6.
Investing in intelligence and insights to modernise and improve the system
7.
Strengthening focus on system quality and safety.
The Ministry wil provide you with a more detailed briefing on our work across these
seven actions in due course.
Medium term: Harnessing what is good and
laying the foundations for change
Previous changes to the health and disability system have been criticised for
insufficient planning, lack of fol ow-through with implementation and insufficient
monitoring and evaluation to understand the impact. Planning for the transition and
transformation of the system during this phase can help change this. A Transition Unit
has been established in the Department of Prime Minister and Cabinet to deliver the
detailed policy and design work on the Government’s response to the Review. The
Ministry has seconded staff to the Transition Unit to support this work. We are primed
to support and help lead the Government’s development and implementation of
proposed system changes.
We know that more substantive changes to the system wil be needed to deliver the
outcomes we expect for all New Zealanders and ensure that the system is sustainable
and equitable. New, more cost-effective ways of preventing ill health and delivering
care and support are required to meet demand and provide consistent experiences for
people using services. To invest well wil require better insights into population health,
the quality of services and the way services are currently delivered, to appropriately
manage cost pressures to improve effectiveness, productivity and efficiency, reduce
waste and increase health equity. We also need to consider all our levers and those of
our partner agencies, not just additional investment, to ensure that funding is used
more effectively and implement changes that move the system closer to our vision of
pae ora – healthy futures.
BRIEFING TO THE INCOMING MINISTER: PART A:
19
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
What next?
We realise this is a particularly busy time for the system but as COVID-19 has
highlighted this system is agile. We already have work underway to create change to
achieve pae ora – healthy futures and wil support you to deliver your priorities for
reform in the context of COVID-19.
We look forward to discussing our work and how we can best support you to achieve
the Government’s priorities for the health and disability system.
20
BRIEFING TO THE INCOMING MINISTER: PART A:
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM
References
Global Burden of Disease Col aborative Network. 2018.
Global Burden of Disease Study
2017 (GBD 2017) Results. Seattle, United States: Institute for Health Metrics and
Evaluation (IHME).
Institute for Clinical Systems Improvement. 2014.
Going Beyond Clinical Walls: Solving
Complex Problems. URL:
http://www.nrhi.org/uploads/going-beyond-clinical-
walls-solving-complex-problems.pdf.
Schneider EC, Sarnak DO, Squires D, et al. 2017.
Mirror, Mirror 2017: International
comparison reflects flaws and opportunities for better US health care.
The Commonwealth Fund.
Treasury. 2019.
Financial Statements of the Government of New Zealand for the Year
Ended 30 June 2019. URL:
https://treasury.govt.nz/publications/year-end/financial-
statements-2019 (accessed 5 May 2020).
Treasury. 2019.
Vote Health – Health Sector – Estimates 2019/20. URL:
https://treasury.govt.nz/sites/default/files/2019-05/est19-v6-health.pdf (accessed 5 May 2020).
BRIEFING TO THE INCOMING MINISTER: PART A:
23
THE NEW ZEALAND HEALTH AND DISABILITY SYSTEM