Early Learning in Medicine (ELM)
Second and Third Year
Handbook 2021
Te Whare Wānanga o Otāgo / University of Otago
Te Kura Hauora o Ōtākou / OTAGO MEDICAL SCHOOL
- 1 -
CONTENTS
WELCOME TO ELM ......................................................................................................................................... 4
Confronting material in the medical school curriculum ................................................................................... 4
OVERVIEW ..................................................................................................................................................... 5
Introduction ...................................................................................................................................................... 5
The relationship between learning in Health Science First Year (HSFY) and ELM ............................................ 5
The educational philosophy of the ELM curriculum ......................................................................................... 5
The Purpose of ELM .......................................................................................................................................... 6
Outcomes of ELM ............................................................................................................................................. 6
Structure of ELM ............................................................................................................................................... 8
THE RELATIONSHIP BETWEEN the four components of ELM ........................................................................... 8
Medical ScienceS .............................................................................................................................................. 8
Integrated Cases ............................................................................................................................................... 9
Clinical Skil s ...................................................................................................................................................... 9
Early Professional Experience (EPE) .................................................................................................................. 9
LEARNING STYLE IN ELM .............................................................................................................................. 10 ASSESSMENT, ATTENDANCE & THE AWARD OF TERMS ................................................................................ 11
Monitoring your progress ............................................................................................................................... 11
Award of Terms Requirements ....................................................................................................................... 12
Terms denied .................................................................................................................................................. 12
Absences ......................................................................................................................................................... 13
Recording your attendance at compulsory educational events ..................................................................... 14
What happens if you miss a compulsory educational event? ........................................................................ 14
Notifying Absences ......................................................................................................................................... 15
Absence for greater than 3 days – Leave of absence ..................................................................................... 15
THE PROGRESS REPORT ............................................................................................................................... 17
Flow chart for monitoring student progress in ELM ....................................................................................... 18
IN-COURSE ASSESSMENTS ........................................................................................................................... 20
Terms requirements ELM 2 ............................................................................................................................ 22
Terms requirements ELM 3 ............................................................................................................................ 23
IN-COURSE ASSESSMENTS .............................................................................................................................. 24
ELM 2 & 3: In-Course OBJECTIVE STRUCTURED CLINICAL EXAM (In-Course OSCE) ....................................... 24
ELM 2 & 3: CLINICAL SKILLS ONLINE WRITTEN TesTS ..................................................................................... 24
ELM 2 & 3: IN-COURSE OBJECTIVE STRUCTURED PRACTICAL EXAM (OSPE) .................................................. 24
ELM 2 & 3: INTEGRATED CASES Tests ............................................................................................................. 24
ELM 2 EPE TEST ............................................................................................................................................... 26
EPE COMMUNITY CLINICAL PLACEMENTS Years 2 and 3 ............................................................................... 27
END OF YEAR ASSESSMENTS .......................................................................................................................... 28
AWARD OF DISTINCTIONS .............................................................................................................................. 29
DEAN’S COMMENDATION .............................................................................................................................. 30
Rules for Final Exams ...................................................................................................................................... 31
EXAM IMPAIRMENT ........................................................................................................................................ 31
Special Examinations/ASSESSMENTS ............................................................................................................. 32
GENERAL INFORMATION ............................................................................................................................. 34
Timetables ...................................................................................................................................................... 34
Scholarships available to second year students ............................................................................................. 34
Dean’s Medical Student Research Scholarships ............................................................................................. 34
Undertaking additional study ......................................................................................................................... 34
- 2 -
Vaccinations .................................................................................................................................................... 34
Culturally sensitive issueS ............................................................................................................................... 35
Anatomy museum .......................................................................................................................................... 35
Communication .............................................................................................................................................. 35
Processes for handling course concerns or complaints .................................................................................. 36
Recording lectures, patient interviews and clinical presentations ................................................................. 36
Student problem directory ............................................................................................................................. 37
NON-ACADEMIC PROBLEMS ........................................................................................................................... 37
First Aid (ELM 2 only) ...................................................................................................................................... 37
Health Sciences library ................................................................................................................................... 37
IMPORTANT DOCUMENTATION ................................................................................................................... 40
Privacy and Confidentiality ............................................................................................................................. 40
Access to notes and handling of written material .......................................................................................... 40
Release of Information ................................................................................................................................... 41
Medical student rights .................................................................................................................................... 41
THE USE OF ONLINE SOCIAL MEDIA ............................................................................................................... 41
Opportunities for Research ............................................................................................................................ 42
Division of Class for ALM ................................................................................................................................ 42
MED 2 AND 3 TEXTBOOK LISTING ................................................................................................................ 48 STUDENT SUPPORT AND WELLBEING ........................................................................................................... 52
Medical student support/student wel being .................................................................................................. 52
University Student Health Services ................................................................................................................. 52
Students with disabilities ................................................................................................................................ 53
International student support ........................................................................................................................ 53
School of Physiotherapy Clinics ...................................................................................................................... 54
CODE OF CONDUCT ..................................................................................................................................... 55 GRADUATE PROFILE ..................................................................................................................................... 60 POLICIES ...................................................................................................................................................... 62
Transfer between Schools of the Otago Medical School ................................................................................ 62
Transfers between Otago and Auckland Medical School ............................................................................... 62
ACADEMIC GUIDELINES ............................................................................................................................... 64
INTEGRITY AND ACADEMIC MISCONDUCT ..................................................................................................... 64
GOOD ACADEMIC PRACTICE ........................................................................................................................... 64
Code of Practice for Fitness to Practise .......................................................................................................... 64
Policy on transmissible and blood-borne infections for medical students ..................................................... 65
- 3 -
WELCOME TO ELM
Welcome to the Early Learning in Medicine Programme, which over the next two years, wil provide
you with a sound understanding of the foundations of the medical and clinical sciences. Medicine
comprises a broad array of learning that is both stimulating and challenging, and which wil continue
until the day you retire. We are confident that we wil be able to share the sense of excitement that
learning in medicine and working with patients offers. The breadth of medicine wil allow you to
consider a diversity of careers in many locations. Whatever your career choice the privilege of
working with patients and their families offers the greatest rewards. We look forward to working
with you to develop your learning and interest.
Medical students are part of a profession which dates from antiquity and which has high standards
to maintain. Whilst students are not yet bound by the ful professional constraints imposed upon
practicing doctors, it is important that you have a good appreciation of the professional
requirements for medicine.
CONFRONTING MATERIAL IN THE MEDICAL SCHOOL CURRICULUM
The medical school curriculum includes potentially emotional y challenging material. Covering such
material is an unavoidable part of a comprehensive undergraduate medical curriculum. Issues
related to suffering and mortality are explored and some of the topics may remind you of what you
or your loved ones have experienced. Patients stories are sometimes presented through various
mediums (e.g., interviews, video, paper cases) and these can be real, raw, and vulnerable accounts
of living with illness. Hearing these stories or reflecting on challenging issues may lead to a range of
emotional responses, including distress.
Feeling distress in response to sensitive topics and human pain is normal. You wil learn to manage
these feelings as you pass through medical school, along with ways of protecting your own health
and wel being. This is part of each student’s professional identity formation, where a student
progresses from being a non-expert at the beginning of medical school to a doctor by the end. It
might be useful to remember that this process is just beginning for second- and third-year medical
students, so don’t be hard on yourself or others if you feel distressed by a topic. Some of you might
have no strong emotional response to some of the topics while others might be distressed, both are
normal responses. Support is available, and you wil not be alone in these feelings.
The curriculum topics (e.g. lecture titles) usually give you some idea of the type of material that wil
be covered: different topics may be difficult for some students. If you recognise that a particular
topic may be distressing for you, it wil be important to use self-care strategies before, during and/or
after these topics are covered. The Medical School makes support available through the lecturer,
tutor, Associate Dean of Student Affairs for ELM, Student Health and Counsel ing, the Associate
Deans for Māori and Pacific and OUMSA. Should your performance in an assessment be affected by
an encounter you find particularly confronting, a Special Consideration form should be completed
and filed (refer to the
Assessment Policy and Procedures document).
- 4 -
OVERVIEW
INTRODUCTION
The teaching in ELM is divided into four interrelated components:
• The Medical Sciences
• Clinical Skil s Module
• Early Professional Experience Module
• Integrated Cases Module
The four components in the Early Learning in Medicine [ELM] curriculum are interlinked and build on
material delivered in Health Sciences First Year [HSFY]. They promote learning from a clinical
perspective and therefore link strongly with the Advanced Learning in Medicine [ALM] curricula in
the Dunedin, Christchurch and Wel ington Schools. The learning programme is based on the
outcomes defined in the Otago Medical School Curriculum Map (https://medmap.otago.ac.nz/ui/).
THE RELATIONSHIP BETWEEN LEARNING IN HEALTH SCIENCE FIRST YEAR (HSFY) AND ELM
The HSFY curriculum delivers foundation medical sciences. ELM delivers more advanced medical
sciences, as wel as clinical sciences, and linkages with HSFY material are identified. The learning
culture of the ELM curriculum is different from HSFY and is more complex. In particular, the Year 2
and Year 3 course can be seen as one very large integrated paper, where all material delivered has
relevance across the whole programme. At the beginning of Year 2, it can be hard to see the
linkages, but these become more evident as Year 2 progresses. The MB ChB is delivered in what is
known as a ‘spiral curriculum’. The basic premise is that topics are revisited multiple times during
the degree, and at each new instance the previous information about that topic is enhanced in
terms of complexity and/or inter-relatedness with other aspects of curriculum. In this way your
depth (and breadth) of understanding increases as you progress through the curriculum. Looking for
these linkages wil enhance your understanding of the material and the practice of medicine.
THE EDUCATIONAL PHILOSOPHY OF THE ELM CURRICULUM
The educational philosophy of the ELM curriculum is based on the fol owing principles:
• Paral el learning of medical and clinical sciences
• The acquisition of both factual knowledge and conceptual understanding
• The ability to learn independently
• The recognition of the interplay of body, mind and physical/social/environmental
(biopsychosocial) factors in illness
• The patient centred approach to care
• The empathic and compassionate approach to care
• The development of professionalism
• The importance of self-awareness in health care workers
• The acknowledgment of uncertainty in medicine
• Learning in a variety of contexts, particularly in the community.
- 5 -
THE PURPOSE OF ELM
The purpose of the Early Learning in Medicine programme is to build on the students prior learning
and develop, for a further two years, the scientific foundations of medical practice and to begin the
acquisition of the knowledge, skil s and attitudes required for professional practice. Specifical y, it
aims to:
1. Lay the foundations of basic sciences on which medical practice resides/relies and facilitate
this learning by explicitly identifying the clinical relevance and contexts in which this
knowledge wil be applied safely in clinical practice.
2. Introduce the clinical skil s used in a medical consultation, giving context and relevance to
the medical sciences, and enabling the application of medical sciences to clinical practice.
3. Establish the foundations of understanding the broad social and cultural concepts and
contexts of medical practice and systems of healthcare.
4. Establish an appreciation of the patient as a unique person and partner in health care.
5. Begin the students’ professional identity formation and understanding of professionalism.
6. Establish habits of life-long learning, including both independent self-directed learning and
collaborative learning.
7. Introduce the knowledge and skil s of critical thinking and reflection required for clinical
practice.
OUTCOMES OF ELM
On completion of ELM a student should be able to:
1. Describe the normal structure and function of human body systems.
2. Describe the pathophysiology and clinical features (signs and symptoms) of common
conditions.
3. Illustrate the application of medical sciences knowledge to common clinical presentations
and conditions.
4. Describe standard diagnostic and treatment options for common clinical presentations and
conditions.
5. Conduct a routine patient consultation using effective communication and attending to
interview structure and relevant content.
6. Perform core components of a physical examination.
7. Locate and evaluate information from a range of sources and apply this information to new
situations with academic integrity.
8. Work effectively both independently and collaboratively.
9. Demonstrate effective oral and written communication skil s.
10. Demonstrate an understanding of the way biological, psychological and social factors
interact in health and disease.
11. Demonstrate an understanding of and commitment to the principles of patient-centred
medicine
.
12. Identify the role of the Treaty of Waitangi as a framework to focus on Maori health
advancement and addressing current health inequities.
13. Identify the relevant frameworks to understand how societal beliefs/values impact on
clinical decision-making and specifically create and/or maintain health inequities within
cultural groups.
14. Identify the special relationship between New Zealand and Pacific communities in Aotearoa
and the region, and New Zealand’s obligation to improve Pacific Health outcomes.
15. Describe the impact of the social, economic and relevant determinants of health on the
practice of medicine.
16. Describe the responsibilities, obligations and privileges of being a doctor, including an
appreciation of the importance as a health professional of self-care.
- 6 -
17. Demonstrate appropriate ethical and professional behaviour, based on an awareness of
personal moral values, and knowledge and understanding of principles of medical ethics.
- 7 -
STRUCTURE OF ELM
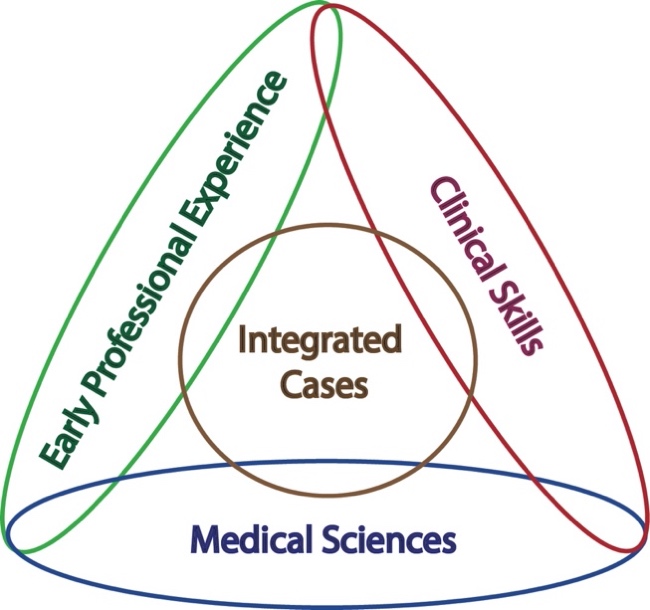
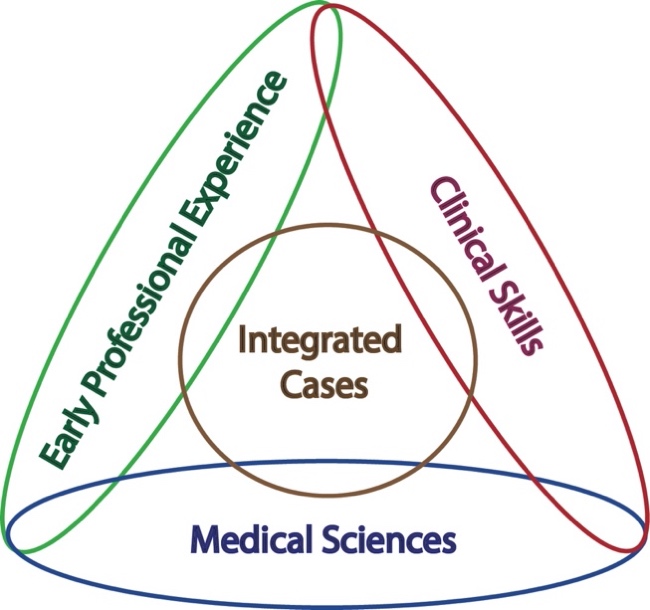
THE RELATIONSHIP BETWEEN THE FOUR COMPONENTS OF ELM
Figure 1. A schematic diagram of the integrative nature of the ELM programme
MEDICAL SCIENCES
The Medical Sciences delivers the theoretical knowledge which provides the foundation for
understanding the scientific basis of medicine and clinical practice. The Medical Sciences comprise
many individual modules which fal into two categories: block or vertical modules.
Block modules: there are 11 block modules, 5 in Year 2 and 6 in Year 3, which are mainly based on
body systems and are usually presented over 4 weeks with up to 10 lectures, 2 labs and one module
tutorial per week. The Integrated Cases run in parallel and reflect the material being presented in
the block module. The main contributors are anatomy, physiology, biochemistry, pharmacology,
microbiology and clinical disciplines.
Vertical modules: there are 17 vertical modules which are spread over Years 2 and 3. These are not
based on body systems but represent disciplines that are relevant to most medical problems e.g.
ethics, blood, genetics etc. They are presented as dispersed lectures or groups of lectures and,
whenever possible, in a way that is relevant to the material being presented concurrently in the
other programme modules. The appreciation of the relevance of vertical module material may not
always be immediately obvious but this builds up over time (as part of the spiral curriculum).
- 8 -
There are three vertical modules, Early Professional Experience, Clinical Skil s and Integrated Cases,
which differ from the other vertical modules in that they each are taught in weekly 2 hour small
group tutorial sessions.
INTEGRATED CASES
This vertical module is a central component of the curriculum whereby clinical scenarios are
presented in tutorials to illustrate application of the medical sciences to clinical practice. Cases are
designed to promote students understanding of whole patient care in clinical medicine, by
integrating material from all modules across ELM and applying it to a patient’s presenting
problem(s). Along with the Clinical Skil s module, Integrated Case introduces students to the process
of clinical reasoning, with the emphasis being on the student developing an enquiring, structured
approach to deduce what may be possible reasons for the health issues in various patients.
CLINICAL SKILLS
Using the Calgary Cambridge model of communication skil s as a base, this vertical module is focused
on the medical consultation, i.e. introduction to the patient, taking a medical history using evidence-
based communication techniques, basic physical examination, and introductory clinical reasoning.
This necessitates contact with simulated patients and the development of an appreciation of the
broad factors contributing to illness. Physical examination of peers is an important part of this
module.
The Otago Medical School expects all students to participate as examinees and
examiners unless there are compelling reasons not to do so. Peer examination in this context
promotes a healthy learning environment and encourages development of professionalism, an
awareness of the patient perspective, and the appropriate gaining of consent.
EARLY PROFESSIONAL EXPERIENCE (EPE)
EPE provides early opportunities to work with real patients and practicing health professionals. In
doing so, you wil encounter many professional issues that are integral to understanding the roles
and responsibilities of being a doctor. In brief, the aims of this vertical module are to provide some
initial experiences and early understanding of:
• The subjective experiences of illness and the patient’s personal context (family, beliefs,
culture and so on)
• The student-patient relationship and the doctor-patient relationship
• The delivery of health care in various social contexts
• Chronic illness, palliative care and end of life issues
• Working with other health professionals
• Becoming a doctor (developing personal and professional resilience, practising safely).
There are two main clinical placements in community settings in EPE: in Year 2 students work as
assistant caregivers in aged-care facilities; in Year 3 they spend a week in rural communities during
Community Contact Week. Links to the other modules are made by students over the course of
ELM. EPE aims to help you bridge the gaps between medical theory and the realities of clinical
practice.
- 9 -
LEARNING STYLE IN ELM
Progressive learning - progressive learning describes the sequence of learning medical sciences to
understand the scientific basis of illness and the major clinical conditions and their management.
Progressive learning commences in HSFY and proceeds through ELM and ALM reaching ful
application and understanding towards the end of ALM. Science concepts and clinical conditions
are visited repeatedly through the whole curriculum. Full understanding of medicine requires a
step-by-step learning approach so cannot be achieved in the ELM years. It is crucial to keep this fact
in mind to prevent feeling frustrated at times.
How much independent learning is there in ELM? - independent learning is an important feature of
undergraduate medicine, starting in ELM and progressing through ALM. We promote the concept
of
guided independent learning where objectives, key concepts and a structure for learning is given,
but there is no formal teaching provided and students work on their own or in small groups. We do
not initially use the terms self-directed or problem-based learning in the ELM curriculum as this
implies that students need to identify their own learning needs. However, self-directed learning wil
be achieved by the end of the ALM course. Independent learning is not the same as personal study
or revision, it is the independent achievement of learning for a specified component of the
curriculum. The ELM programme contains at least 16 hours of independent learning per week
during which independent tasks can be completed.
Group learning - group learning is an important part of medical training as health professionals
usually function within a group or team. Group learning in tutorials and to complete independent
learning tasks is promoted, as the group members wil have a diversity of skil s to apply to problem
solving. Working cooperatively in groups may represents a culture change as we are seeking group
excellence as much as individual excellence. The culture of learning in ELM should be that of
achieving high competence, actively contributing to the learning of the group and enjoying the
learning environment.
The weekly timetable - the weekly timetable normally contains up to 24 hours of teaching contact
and at least 16 hours of independent learning time. The timetable comprises lectures, laboratories
and tutorials. There is usually a maximum of 10 lectures per week. The Year 3 timetable is very
similar to the Year 2 timetable. The timetable runs from 9am until 6pm, with the occasional 8am
lecture.
Moodle - Moodle is ELM’s learning management system (LMS), which provides the outcomes and
objectives for modules and laboratories, handouts for lectures and lecture power points as wel as
course information and notices. Summary handouts for lectures and power-point presentations are
placed on Moodle. Discussion boards are provided and are monitored by teaching staff.
- 10 -
ASSESSMENT, ATTENDANCE & THE AWARD OF TERMS
Assessment in ELM provides information to both you and staff on how you are progressing. It can
be used both to guide your future learning and to inform decisions on whether you have attained
the standard required to progress to the next year of the MB ChB course. There are three elements
that must
ALL be passed each year, to progress: Terms, the Written component, and the Clinical
Skil s component. It is worthwhile noting that Professional Conduct is considered both as part of the
process of awarding Terms, and as a stand-alone factor when considering whether students are
ready to progress to the following year.
ELM uses a two-step process with respect to passing each year. First you must be awarded Terms.
The awarding of Terms requires you to have completed a given set of tasks as prescribed (the ful list
of Terms requirements is shown below). Having been awarded Terms, you are admitted to the end-
of-year examinations. Decisions on whether you are ready to progress wil then be made on the
basis of your aggregated in-course and end-of-year Clinical Skil s and Written assessments.
In-course assessments and Terms requirements are closely linked in ELM. In-course assessments
may contribute a percentage weighting to your final grade, or they may be what is commonly cal ed
formative (and thus
do not contribute a percentage weighting to your final grade). All assessments
are designed to have a formative component, i.e. they aid your learning by providing you with
feedback on your mastery of the topic being assessed, and guidance as to how you can improve your
skil s/knowledge.
ELM considers assessments that contribute a percentage weighting to your final
grade AND those that do not, as EQUALLY important. Both types of assessments contribute to
decisions about your readiness to progress to the following year.
Additional y, and again, equal y as important, your Terms requirements include the need for you to
demonstrate
satisfactory professional conduct during the year. Medical practice is performed and
delivered through significant interactions with other people: patients, colleagues and other staff.
Doctors are expected to use the knowledge they have gained
in service of others (patients and
society);
they are therefore required to behave in a particular way. As you progress through the
MB ChB programme, you wil note that we place as much emphasis on how you behave, as what you
know or what skil s you can perform. Learning appropriate professional behaviour and committing
to the standards of your profession is a long-term, life-long endeavour.
Acting professionally has both innate (who you naturally are) and learned components. There are
many learning opportunities related to professionalism in ELM. From an assessment perspective,
we evaluate your professional conduct based on the choices you make. This includes, but is not
limited to, whether you: attend compulsory educational events; notify us in a timely manner of
absences from compulsory events (put in an apology); are on time; attend scheduled meetings;
participation in, and interactions with members of your tutorial and laboratory groups; and your
interactions with academic and professional staff, and the members of the DHBs and public you
encounter during your studies. Not meeting these expectations is known as a failure to engage, as
your engagement must be sufficient to enable your own learning.
MONITORING YOUR PROGRESS
Becoming a doctor, and developing as a doctor in training, is a non-linear process. Everyone learns
at different rates and we all have different strengths and weaknesses. Part of the role of the ELM
programme is to provide you with support when you need it. To be able to do this, we monitor your
progress closely.
- 11 -
This is done through obvious formats, such as assessments and attendance records, and also,
through
Progress Reports. Progress Reports are used by tutors to raise awareness of any potential
issues at an early stage, so that students can be notified and learning plans agreed upon. The ELM
Student Progress Committee (SPC) meets three times a year to review each student’s current and
past records, and to make recommendations about student progress. In most cases, students wil be
noted as having made satisfactory progress for any given SPC reporting period.
Where there are issues to be resolved, this wil usually be done using our
Conditional Pass system.
It is highly likely that at some stage as you progress through the MB ChB, you wil receive a
Conditional Pass (CP), so don’t be alarmed if you are notified by the ELM SPC that you need to
meet with us to discuss a CP. A CP is not a final grade: each CP comes with a set of
Conditions to
Pass. These conditions wil be related to the concern(s) the SPC have about your progress. For
example, we may be concerned that you have an unacceptable number of unnotified absences (a
marker of poor professional behaviour), so your Conditions to Pass may be not to have any
unnotified absences in the next reporting period. When Conditions to Pass are met, a CP is
converted to
Pass After Conditions Met (PACM). In this context, a CP should be viewed as an
opportunity to learn, not as an admonishment. If, however, Conditions to Pass are not met, the final
grade becomes a
Fail. Whereas in ALM a single Fail leads to Terms being denied, in ELM a Fail wil be
considered alongside all other information about your performance, in making Terms
recommendations.
AWARD OF TERMS REQUIREMENTS
The award of Terms is made by the Board of Censors 2/3 based on recommendations made by the
ELM Student Progress Committee and the Fitness to Practice Committee.
Where a student has satisfactorily completed all in-course requirements and there are no
outstanding concerns re professional conduct, they wil be granted Terms, and may sit their end-of-
year examinations.
TERMS DENIED
The Board of Censors wil usually deny Terms to a student on the recommendation of the ELM
Student Progress Committee and/or the Fitness to Practice Committee where:
a) a student has generic or non-isolated deficits in performance and/or,
b) does not undertake, as prescribed and scheduled, more than one Terms requirement for
reasons not approved under the Special Consideration or Leave of Absence process and/or,
c) has total absences from the compulsory educational events for the year of greater than
25% and/or,
d) where there are concerns regarding the student’s professional conduct, which includes
unnotified absences from compulsory educational events.
If Terms are denied the student cannot sit the end-of-year exams and wil be required to repeat the
year or, in the case of a student who has already repeated a year, wil usually result in exclusion
from the course.
- 12 -
ABSENCES
Attendance at laboratory and tutorial sessions, and whole class briefings/clinical
demonstrations is compulsory and you are required to inform in writing (preferably
email) the relevant staff member and Jude Hodge ([email address]) of
any absence, preferably before, but failing this, as soon as possible after your
absence. Failure to meet this requirement wil be recorded on your Progress
Report. Registers wil be kept when your attendance is a requirement for the
awarding of Terms. For example, you all MUST swipe your Student ID cards, sign
the attendance register or ensure your presence has been recorded electronically
each time at laboratories and tutorials, or you will be marked as absent. Note:
recording another student’s presence when they are not there or asking another
student to record your presence when you are not there, would be considered an
act of Academic Misconduct.
If you are absent from classes it is your responsibility to catch up with any work missed
and to
inform your tutor/ lab demonstrator
and the ELM administrator, [email address] of your
absence.
Please note that the policy for the three tutorial based ELM modules – Integrated Cases,
Early Professional Experience and Clinical Skills – is that you cannot swap tutorial groups.
However, there may be extenuating circumstances when this wil be allowed but approval must first
be obtained from the module convenor.
Our guiding philosophy is that medical students are responsible, motivated adults who are expected
to participate actively in assessing their own learning progress. Part of that self-assessment involves
making decisions about your engagement with the various learning opportunities that are part of
the ELM curriculum. We understand that you wil have developed your own learning style, and your
own practices with regard to attendance at and engagement in various classes (lectures,
laboratories, tutorials
etc.). Nevertheless, ELM promotes a culture of engagement that involves
being there in the moment, particularly in smal group settings, where the values and cultural norms
of medicine can be model ed and assimilated. Absences from tutorials means there wil be fewer
opportunities to test yourself out in relation to peers, less chance to hear yourself speak and to see
your own reflections in the reactions of others, including tutors, and less chance to work collegially
and contribute to the development of your colleagues. In brief, tutorials (and to a lesser extent
laboratories and lectures) are where students learn how to
be a doctor, which entails a great deal
more than learning the necessary medical knowledge. Tutorials and bedside learning with patients
are where knowledge and skil s can be demonstrated.
For these reasons we have designated specified educational events as compulsory, and attendance
at these is a Terms requirement. Any session designated as a tutorial or a laboratory is compulsory.
Other events may also be designated as compulsory (e.g. whole class briefings and clinical
demonstration lectures), this wil be made clear to you. We place an emphasis on these learning
opportunities because they have an experiential component. This means that there is something
involved in this experience that you cannot otherwise ful y get the benefit of without being there; it
involves something that cannot be replicated by only reading about it, listening to or watching it.
In general, lectures are not compulsory. Nevertheless, our expectation is that you wil attend the
large majority of your lectures (we understand that there may be occasions for health or personal
reasons you wil have to miss a lecture). We know that podcasting/watching videos of lectures is a
growing trend, and we consider podcasts to be an invaluable
revision tool. We
do not consider
- 13 -
podcasts as a suitable replacement for being at your lectures. There are multiple reasons for this,
including forming positive habits of engagement with learning opportunities, the value of being part
of a shared experience with your classmates, the opportunities to discuss the material being covered
with peers and lecturers, and, on the occasion when guests are brought into the lecture to share
their experiences as part of your learning, respect for those guests who give up their time for your
benefit. It is not professionally courteous nor respectful when people make time in their day to help
you, if three-quarters of the lecture theatre is empty because a large proportion of the class could
not make time in their day to come and engage.
RECORDING YOUR ATTENDANCE AT COMPULSORY EDUCATIONAL EVENTS
Attendance wil be recorded when it a requirement for the award of terms. It is your responsibility
to ensure you have been marked as present. For example, you MUST swipe your Student ID card,
scan the QR code or sign the attendance register as directed at laboratories and tutorials
etc. For
some classes, your tutors wil have an electronic register that they wil complete. Often it wil be
obvious that your tutor has taken the attendance for that session. However, for those occasions
where you are not sure if attendance has been taken, it is not impolite to check with your tutor if
they have noted your presence (tutors wil be told that you have been told it is OK to ask).
Note: recording another student’s presence when they are not there or asking another student to
record your presence when you are not there, will be considered an act of Academic Misconduct
and be dealt with under the appropriate University statutes. Additionally, it would be noted as
unprofessional behaviour by the SPC, under the label of dishonest behaviour.
It is also worthwhile mentioning that as part of monitoring your professional conduct, we ask tutors
to note if you are late. Repeated late arrival is unprofessional and discourteous (disrespectful
behaviour). If you are late, it is polite to apologise to the group, perhaps quietly and briefly if
someone is speaking or an activity is taking place, and then more overtly at an appropriate moment
(a fulsome explanation for your lateness to the whole group is not required, particularly if the reason
for your absence is of a personal nature, but you may wish to provide a more detailed explanation to
your tutor at the appropriate time).
WHAT HAPPENS IF YOU MISS A COMPULSORY EDUCATIONAL EVENT?
Whilst we expect you to organise your general day-to-day life activities so that they do not prevent
you from attending compulsory educational events, we understand that from time to time, for
health or other personal reasons, you wil miss a compulsory educational event. Such absences
need to be considered in two important ways.
First, as a professional courtesy, we expect that you wil notify us of any foreseen or unforeseen
absences from compulsory educational events (see below for the notification process).
We make an
important distinction between notified and unnotified absences in the context of professional
behaviour.
Second, as discussed above, compulsory educational events have experiential aspects that are
important for your development as a doctor. Importantly, some of the learning from these
experiential aspects is incredibly difficult to assess formal y (e.g. the ability to work in groups, to be
a leader, to listen thoughtfully to others), and we assume that you gain the learning by being present
and being engaged.
We become concerned if we note that you have a large number of total absences, or you have a
large number of absences for particular components of the course. You can see from the Terms
denied criteria, that absences in excess of 25% of the total compulsory educational events for the
- 14 -
year, even if those absences are for good reasons, wil see you being denied Terms and failing the
year.
However,
and very importantly, the 25% threshold should
not be viewed as a target number,
where it is OK to have absences up to that value. Historical y, most ELM students have no or less
than a handful of absences from compulsory educational events. If you are absent from a
compulsory educational event it is
your responsibility to catch up with any work missed. If we
notice that you are accumulating a concerning number of absences, either overall or from specific
compulsory educational events, it is highly likely that SPC wil assign you a CP related to those
absences and provide you with an associated set of things you must do to account for the material
that has been missed (as wel as other conditions related to not repeating those behaviours).
It may even be that you are required to meet with the Assessment Convenor or other staff without
waiting for SPC intervention, if we are sufficiently worried about your progress. We know how hard
you have worked to get into the medical programme, so we are very sensitive to even small
numbers of absences, as it is often an indicator that there are circumstances in your personal life
that are preventing you from engaging in the very thing you have worked so hard to achieve. As
part of our monitoring of absences, we wil typically involve the Associate Dean of Student Affairs,
who is there to support you, should we notice an increase in absences.
NOTIFYING ABSENCES
If you are going to miss a compulsory educational event, you are required to inform the relevant
staff member (typical y your tutor or laboratory supervisor)
and Jude Hodge
([email address]) of any absence in writing (i.e. by email), preferably before, but failing
this, as soon as possible after your absence.
We make an important distinction between notified
and unnotified absences in the context of professional behaviour.
If you know in advance you are going to miss a class, we expect you to email
beforehand. If you are
unexpectedly sick, it is acceptable for you to email as soon as possible after your absence. When
emailing, please provide a brief reason for your absence.
ABSENCE FOR GREATER THAN 3 DAYS – LEAVE OF ABSENCE
We are aware, that over the course of your two years in ELM, there may be occasions where you
require a prolonged absence for important personal events or illness. To support you through these
absences, we have a more formal approval process known as
Leave of Absence. This process
identifies both the impact the absence wil have on your studies/attendance at ELM educational
events, and how we can support you (if required) to manage your absence.
Approval (or otherwise) of Leave of Absence applications is given by the Associate Dean of Students
Affairs (ADSA), who wil meet with you as part of this process. Usual y, with appropriate supporting
documentation, leave for extended illness or exceptional personal circumstances (e.g.,
bereavement) is approved.
- 15 -
The granting of leave is discretionary and considered case by case. When deciding on leave
applications, the fol owing wil be taken into consideration:
• Learning or professional development opportunities afforded by the activity for which leave
is sought
• The family or community importance of the student attending the activity
• Whether the student has extenuating personal circumstances
• Whether the student is participating in a national or international sporting or cultural event
• Whether the student is presenting, organising or representing a group at a conference or
meeting
• The proportion of the module for which the student wil be absent
• The reason the activity cannot be undertaken during scheduled holidays
• The length of leave relative to the activity for which leave is sought
• The importance of missed teaching or assessment, and the student’s ability to catch up on
missed activities
• The student’s total leave in that year and any other leave in that module
• The student’s total absences during the year and any other absences in that module
Note that having leave approved does not exempt the compulsory educational events missed
from being counted towards your total absences for the year. The approval means there are no
issues from a professional conduct perspective (you have done the right thing by going through the
right process), but you are stil missing learning opportunities. The implications of this wil be
discussed with you during the approval process.
Leave of Absence forms can be obtained from MedMoodle or the ELM Hub in the Hunter Centre.
Full details of the application process can be found on the form.
Appropriate supporting documentation wil be required for all leave applications. Details of what is
required can be discussed with the ADSA, but typically a medical certificate is required for illness,
evidence of a bereavement may be provided with a copy of a death certificate or death notice, and
national representation requires a letter from the appropriate national organisation.
Note that failure to attend class where a leave application is declined wil be considered
unprofessional conduct and wil be brought to the attention of the Student Progress Committee.
- 16 -
THE PROGRESS REPORT
WHAT IS THE PURPOSE OF THIS REPORT?
This form helps tutors to identify students in the ELM course whose development of professionalism
and general performance does not meet acceptable standards. The reports are fil ed in three times
per year to enable a cumulative central record to be kept which wil extend through all years in
Medical School. In addition, these reports provide information that may be used to inform
decisions on the awarding of Terms and Distinction.
WHAT MAY BE ASSESSED WITH THIS FORM?
Tutors wil use this form to report observations of your performance with regard to the professional
behaviours as identified in the Student Code of Conduct which you have signed and a copy of which
appears in this handbook fol owing the Student Support and Wel being section. Other aspects
related to your learning may also be evaluated.
HOW IS THE PROGRESS REPORT FORM USED?
Tutors in EPE, Clinical Skil s, Integrated Cases and some of the Medical Science modules fil in these
forms for each student three times per year. If tutors have concerns, they wil discuss those
concerns with the student, then pass the form to the Student Progress Committee (SPC) that
monitors all incoming reports. Depending on the nature of the issues, students may be contacted by
the Convenor of one of the three tutorial-based modules – Integrated Cases, Clinical Skills or EPE,
the Chair of the Assessment Subcommittee, the Assessment Convenor, the Chair of the SPC or the
Associate Dean of Student Affairs for further discussion. In some cases, this may involve identifying
appropriate remedial activities.
WHAT ARE THE CONSEQUENCES OF ONGOING ISSUES?
The ELM Board of Censors wil examine the record of each student having difficulties. On the basis
of the student’s record and his or her progress on remedial activities reported by the SPC and the
Associate Dean for Student Affairs, the Board wil decide if the student should be granted Terms.
Students who do not engage in remedial activities after being advised to do so may not be granted
Terms.
Students are advised that copies of the Progress Report forms for each of the tutorial-based
modules wil be posted on Moodle prior to their first use in the first semester of each year.
- 17 -
FLOW CHART FOR MONITORING STUDENT PROGRESS IN ELM
Attendance Records
In-course
Assessments:
Online Written
Students
Progress
Clinical Skil s Exams
wil be
Clinical Skil s In-
Pacific
ELM2
ELM3
reports
Health
Humanities
contacted
completed by
Course OSCEs and
Immersio
Hauora
Selective
and meet
Clinical Skil s,
reflective
Research
Māori
with the ELM
annotations, OSPE.
Smart
n Day
week and
and
Integrated
and
Community
Assessment
Cases, EPE
Case Based
assessme
assessmen
Contact
Convener
modules
question
nt
t
Week
as unnotified
Assessments,
and/or
Genetics
excessive
assignment, EPE
notified
essay/ assessment
absences
arise
ELM Assessment
Sub-committee
meets
prior to SPC meeting
to review incoming
reports
>3
2-3
unnotified
and/or
unnotified
significant
absences
OR >9
notified
absences
notified
during
absences
during
review
period
review period
Referred
to
Letter from
Student
receives a letter from the ELM SPC AND meets
ELM
ELM
with the Chair of the ELM SPC, and the ELM Assessment
Student
Assessment
Convener or ELM Medical Education Advisor
Progress
Sub-
Committee
committee
(ELM SPC)
Referred
Failure to complete all Terms requirements and in-
to
course assessments and/or serious unsatisfactory
Associate
progress reports and/or significant absences
Dean of
a recommendation that the student have Terms
Student
deferred or denied (refer 2.3.3)
Affairs
(ADSA)
Referred
Board of Censors for ELM 2 and ELM 3 receive Terms
to Fitness
recommendations and determine if student should have
to Practise
Terms deferred or denied.
Committee
(FtPC)
- 18 -
GENERAL
Where not otherwise stipulated, the fol owing general rules apply:
• Students must observe strict confidentiality in all matters relating to clinical presentations.
• Students are expected to display a standard of behaviour appropriate to a professional
course.
• Only ELM students may attend sessions in the ELM Course.
- 19 -
IN-COURSE ASSESSMENTS
ELM has in-course assessments that can either be summative (which contribute marks to the end of
year mark) or formative (which provide information on your progress). The summative in-course
assessments collectively contribute 20%-25% to the final mark of either the Clinical Skil s or Written
components. You must complete all summative and formative in-course assessments to be awarded
Terms and be allowed to sit the final examination. If you fail to complete these assessments, you
wil normally be deemed to have an unsatisfactory year’s work and wil be denied Terms.
You wil be advised about the times and, where appropriate, the venues for these
assessments/assignments by the convenors of modules and courses, details wil also be posted on
Moodle.
If you have questions or concerns relating to assessment, please contact please contact the
assessment team ([email address]).
The tables below show you the in-course summative assessments, their contribution to your end of
year mark, and how they relate to and aggregate with end-of-year assessments.
ELM 2 ASSESSMENTS
In-Course Assessments
End-of-Year Assessments
Assessment
Assessment format
Associated
Assessment
Associated
component
weighting
format
weighting
Clinical Skil s Online Written Test #1 (Semester 1)
5%
OSCE
80%
Online Written Test #2 (Semester 2)
15%
Written
OSPE (Semester 1)
5%
SAQ/MCQ
68%
papers
Integrated Cases Test #1 (Semester 1)
4%
OSPE
7%
EPE Test (Semester 1)
5%
Integrated Cases Test #2 (Semester 1)
6%
Genetics Assignment (Semester 2)
5%
ELM 3 ASSESSMENTS
In-Course Assessments
End-of-Year Assessments
Assessment
Associated
Assessment
Associated
component
Assessment format
weighting
format
weighting
Clinical Skil s Online Written Test #1 (Semester
10%
OSCE
75%
1)
Online Written Test #2 (Semester 2) 15%
Written
OSPE (Semester 1)
5%
SAQ/MCQ
73%
papers
Integrated Cases Test (Semester 1) 4%
OSPE
7%
Renal Test (Semester 1)
6%
EPE Reflective Essay (Semester 2)
5%
- 20 -
Students must gain Terms, meet the Pass criteria for both the Clinical Skil s and the Written
components, and have no issues regarding professional conduct, in order to gain a Pass for the year.
NOTE: The Clinical Skil s and the Written components are stand-alone components for the purposes
of decisions about passing the year.
YOU MUST PASS BOTH COMPONENTS TO PASS THE YEAR, and
MARKS CANNOT BE TRANSFERRED FROM ONE COMPONENT TO ANOTHER i.e. they cannot
compensate for each other.
Below is a summary of the Terms requirements (including both the summative assessments above,
and other formative assessments and learning activities).
- 21 -
TERMS REQUIREMENTS ELM 2
Terms refers to the requirements a student must complete to be permitted to sit final examinations.
Students are expected to submit a Leave of Absence/Special Consideration application if they do
not fulfil any of the Terms requirements listed below
In order to be granted Terms and be eligible to sit the end-of-year exams a student must have:
1. Demonstrated satisfactory professional conduct including (with the exception of an
acceptable level of notified absences), attending all compulsory education sessions and
events
2. Attended the
Pacific Health Immersion Day and satisfactorily completed
the
associated assessment (Semester 1)
3. Completed the
in-Course History-taking OSCE and
Examination OSCE at the assigned
times, and satisfactorily completed the
associated reflective analyses (Semester 1)
4. Completed
both in-course Clinical Skills on-line written assessments* (Semesters 1
and 2)
5. Completed both
in-course Integrated Cases assessments* (Semesters 1 and 2)
6. Completed the
in-course OSPE* (Semester 1)
7. Completed the
in-course EPE assessment* (Semester 1)
8. Completed all four modules within the
ResearchSmart course (Semesters 1 and 2)
9. Attended the
Hauora Māori Week and satisfactorily completed
the associated
assessment (Semester 2)
10. Completed the
in-course Genetics assignment* (Semester 2)
11. Satisfactorily completed their
Personal Drug Formulary, consisting of 10 reports on
drugs selected from the Core Drug List provided (Semester 2)
12. Attended the assigned
EPE clinical placement (Semester 1 or 2) and satisfactorily
completed the
Reflective essay (Semester 2)
A professional approach to educational opportunities (point 1 above) is expected in regard to those
Terms requirements that specify completion rather than performance at a certain standard, and to
the Retained Knowledge Test. Where a student has demonstrated below-standard performance in
any domain, declining additional learning opportunities may be considered an indicator of below-
standard professional conduct.
*Those Terms requirements contributing a percentage weighting to the end-of-year aggregated
marks on which progress decisions are made, are asterisked.
- 22 -
TERMS REQUIREMENTS ELM 3
Terms refers to the requirements a student must complete to be permitted to sit final examinations.
Students are expected to submit a Leave of Absence/Special Consideration application if they do
not fulfil any of the Terms requirements listed below
In order to be granted Terms and be eligible to sit the end-of-year exams a student must have:
1. Demonstrated satisfactory professional conduct including (with the exception of an
acceptable level of notified absences), attending all compulsory education sessions and
events
2. Completed the
in-course History-taking OSCE and the
Examination OSCE at the assigned
times and satisfactorily completed the
associated reflective analyses (Semester 1)
3. Completed
both in-course Clinical Skills on-line written assessments* (Semesters 1 and 2)
4. Attended al
Inter-Professional Education (IPE) sessions and satisfactorily completed the
group project (Semester 1)
5. Completed the
in-course Integrated Cases assessment* (Semester 1)
6. Attended all
EPE Humanities Selective sessions and satisfactorily completed the
associated assignment(s) (Semester 1)
7. Completed the
in-course OSPE* (Semester 1)
8. Completed the
in-course Renal assessment* (Semester 1)
9. Completed the
in-course EPE Reflective essay* (Semester 2)
10. Attended the
Pacific Health Immersion Day (Semester 2)
11. Attended the
in-course EPE Community Contact Week (CCW) at the assigned time
and
satisfactorily completed the individual and group reports (Semester 2)
12. Satisfactorily completed their
Personal Drug Formulary, consisting of 20 reports on drugs
selected from the Core Drug List provided (this includes the 10 drug reports completed in
ELM2), and satisfactorily completed a
group presentation on drug interactions (Semester
2)
A professional approach to educational opportunities (point 1 above) is expected in regard to those
Terms requirements that specify completion rather than performance at a certain standard, and to
the Retained Knowledge Test. Where a student has demonstrated below standard performance in
any domain, declining additional learning opportunities may be considered an indicator of below-
standard professional conduct.
*Those Terms requirements contributing a percentage weighting to the end-of-year aggregated
marks on which progress decisions are made, are asterisked.
- 23 -
IN-COURSE ASSESSMENTS
ELM 2 & 3: IN-COURSE OBJECTIVE STRUCTURED CLINICAL EXAM (IN-COURSE OSCE)
Two In-Course OSCE’s wil occur as part of Clinical Skil s tutorials in Semester 1. There wil be an In-
Course History OSCE assessing the history taking competency and an In-Course Examination OSCE
assessing competency of clinical examination skil s. They wil both be held in Semester One in your
usual tutorial time. The In-Course OSCE’s wil be marked on the ELM 1 to 5 scale by a clinical skil s
tutor. The In-Course OSCE’s wil be recorded, and you wil use the recordings to make reflective
annotations using the Bracken software. Your own tutor wil respond to your annotations.
• The OSCEs are designed to assess the clinical skil s of history taking and clinical examination.
Regular informal review of clinical skil s wil also be provided by tutors during the year and
individual feedback wil be provided to you.
Attendance and completion of the In-Course History OSCE and the In-Course Examination OSCE, and
the associated reflective annotations are Terms requirements.
ELM 2 & 3: CLINICAL SKILLS ONLINE WRITTEN TESTS
In the Clinical Skil s online written tests, knowledge of ELM Clinical Skil s and developing clinical
reasoning wil be assessed using videos, multiple choice questions, images, and “fil in the gaps”
questions. Two online written tests wil be run outside of scheduled tutorial times. The first
assessment wil be in the second half of Semester 1 and the second assessment wil be in the first half
of Semester 2.
• In ELM 2 the first written test wil contribute 5% to your final mark in Clinical Skil s and the
second written test wil contribute 15% to your final mark in Clinical Skil s.
• In ELM 3 the first written test wil contribute 10% to your final mark in Clinical Skil s and the
second written test wil contribute 15% to your final mark in Clinical Skil s.
The In-Course Clinical Skil s Online Written Tests are Terms requirements.
Dates/times for the tests wil be confirmed in Semester 1.
ELM 2 & 3: IN-COURSE OBJECTIVE STRUCTURED PRACTICAL EXAM (OSPE)
An In-Course OSPE wil be held in Semester 1 in for ELM 2 (Friday 11th June) and ELM 3 (Wednesday
9th June). Both assessments wil consist of laboratory-based questions related to the learning
objectives covered in Semester 1.
Attendance and completion of the In-Course OSPE is a Terms requirement and wil contribute 5%
(ELM 2 and ELM 3) to the final Written mark.
ELM 2 & 3: INTEGRATED CASES TESTS
The Integrated Case Tests are designed to assess your ability to synthesise, integrate and apply your
knowledge of the medical sciences to clinical practice. Inherent in this is testing the development of
your clinical reasoning and ability to think on your feet. These tests wil also measure your ability to
explain key concepts coherently using appropriate language. All tests wil be written under exam
conditions over a 30-40-minute period. You wil be briefed on the tests via a Moodle message in the
weeks prior to the assessment.
- 24 -
Completion of all tests is a Terms requirement and, as indicated below, contribute towards the final
Written mark:
ELM 2
Test #1: Semester 1, Thursday 27th May 2021 at 1:45pm (4%)
Test #2: Semester 2, Tuesday 10th August 2021 at 2:00pm (6%)
ELM 3
Test: Semester 1, Wednesday 14th April 2021 at 11:00am (4%)
Any changes to these dates and times wil be notified via Moodle.
- 25 -
ELM 2 EPE TEST
Early Professional Experience (EPE) Programme: Short Answer Question (SAQ) and Situational
Judgment Test (SJT). These are short written assessments sat under exam conditions near the end
of Semester 1, which test your knowledge of learning from the first three units in EPE. Both tests
wil be based on clinical and professional scenarios; the SJT requires judgment between various
response options.
EPE Test: Semester 1, Friday 25th June 2021 at 12:00pm (5%)
ELM 2 GENETICS ASSIGNMENT
As part of the Genetics vertical module you undertake a self-directed learning exercise on a specific
genetic disease. This research project involves critical thinking, literature analysis, an oral
presentation (in tutorials), and submission of a written assignment.
The Genetics assignment is due Semester 2, Sunday 12th September 2021 at 11.55pm
The Genetics assignment wil contribute 5% to the final Written mark.
ELM 2 EPE CLINICAL PLACEMENT: PROFESSIONAL BEHAVIOURS and REFLECTIVE ESSAY
The purpose of the essay associated with the Clinical Placement is to demonstrate your capacity for
self-awareness, monitoring of your own development, and your approach to professional
responsibilities and behaviours. Further details about the clinical placement wil be provided in the
EPE Clinical Placement Tutorial Guide.
There are two essay options:
1. Review and discuss your learning in the EPE clinical placement. Describe, analyse and discuss
what you have learnt from this experience in terms of training to become a doctor;
Or
2. What has been the most powerful learning experience for you this year? What did this
experience mean to you as a student or future doctor; what are you able to take away as your
learning?
Length: 1500 - 2000 words in 1.5 spacing in a Word document (not PDF or Pages). Feedback wil be
provided by EPE Tutors. Further details wil be provided in the Tutorial Guide.
The Reflective Essay is due Semester 2, Sunday September 19th at 11:55pm (any changes to this date
and time wil be notified via Moodle).
RESEARCH SMART
ResearchSmart is an online programme designed by the Medical Library as preparation for written
assignments and future research. It wil help you develop information literacy skil s and serves as a
guide to the best use of resources and services provided through the University Library.
ResearchSmart consists of four modules, all of which must be completed online. Completion of all
modules is a Terms requirement.
ResearchSmart wil be available from 2nd March to 18th July (11:55pm) 2021.
- 26 -
ELM 3 RENAL TEST
A case-based test, with a mixture of long and short format questions (essay-like and short-answer
question-like, respectively) wil be undertaken as part of the Renal module in Semester 1.
The Renal Test wil contribute 6% to the final Written mark.
Renal Test: Semester 1, Friday 25th June 2021 at 3:00pm
EPE3 REFLECTIVE ESSAY
The topic of this essay is:
Responding to suffering – implications for me and my future practice.
In this essay, please consider your role as a future doctor in caring for patients with suffering,
palliative or end of life care needs with reference to your learning in Unit 6 as wel as to patients you
have met, interviewed or observed in ELM. More details wil be provided in Unit 6 (Pal iative care)
and on Moodle.
Length: 1500 - 2000 words in 1.5 spacing in a Word document (not PDF or Pages).
The Reflective Essay is due Semester 2, Sunday 15th August at 11:55pm (any changes to this date and
time wil be notified via Moodle).
The EPE Reflective Essay wil contribute 5% to the final Written mark.
EPE COMMUNITY CLINICAL PLACEMENTS YEARS 2 AND 3
In Year 2, all students wil have a 5-week clinical placement in a community residential care facility
and wil have an on-site assessment by the nurse manager (this is related to the Professional
Behaviours and Reflective Essay activity).
In Year 3 there wil be a one-week Community Contact Week (CCW) with an associated report.
Attendance and completion of these allocated clinical placements is a Terms requirement. The
fol owing table provides a guide to the expectations about your professional behaviour (planning,
commitment and so on) before, during and after your clinical placements.
Professional expectations and behaviours associated with the Clinical Placement
Planning
Commitment
Responsibility
Contribution
Documentation
Overall grade
Proactively
Makes no
Proactive
Satisfactory
Hands in the RCF
All items
engages with
changes to
behaviour in
teamwork and
Attendance and
completed
administrator
scheduling of
relation to
contribution to
Assessment
satisfactorily,
about
shifts at the
illness or injury
the care of
Report to tutors
no negative
preferences
resthome
(advises OMS
residents while at at the follow up
reports from
and timing of
(unless severe
admin and
the resthome, as tutorial
admins or RCF
placement (in
personal or
resthome in
measured by the
staff.
town, out of
family il ness)
advance), helps RCF Assessment
town,
to organize
Report (routinely
weekends,
catch-up shifts
completed by
weekdays,
nurse managers
personal
on completion of
commitments)
5 shifts
More information wil be provided in the introductory lecture about your clinical placements as wel
as in the Clinical Placement tutorial guide.
- 27 -
END OF YEAR ASSESSMENTS
At the end of the year there wil be the fol owing assessments:
ELM 2
Written component:
• Three 3-hour exams consisting of case-based short answer questions (SAQ) (two-thirds) and
multiple-choice questions (MCQ) (one third), which may cover any of the learning objectives
addressed during the year (i.e. material from block and vertical modules, Integrated Cases,
Clinical Skil s and Early Professional Experience). Clinical Skil s is included here not because
the intention is to assess in detail Clinical Skil s material (which is assessed in the Clinical
Skil s component), but because as an integrated programme, it is highly likely your
knowledge from Clinical Skills will be relevant to some questions in the exams.
• One 1-hour OSPE, which wil consist of approximately 50 questions that wil include
questions on anatomy (including histology) and pathology.
• The mark obtained in the SAQ/MCQ papers and OSPE wil contribute 75% (68% for
SAQ/MCQ papers and 7% for OSPE) to the final Written mark. Note that a minimum mark of
45% is required in the end of year OSPE to pass the Written component.
Examples of previously used case-based short answer examinations are available on the Central
Library website (there is a hot link in the blue banner of the website) and the URL is:
http://www.library.otago.ac.nz/exams/index.html
Clinical Skills component:
• One OSCE (Objective Structured Clinical Examination) consisting of 8 x 7-minute stations,
marked on a 1 to 5 scale. These stations wil be drawn from the defined tasks outlined in the
Clinical Skil s objectives and wil include clinical examination and history taking skil s. A
sequential testing approach is taken. All students wil initially attempt 4 OSCE stations
(consisting of two History Taking and two Clinical Examination stations). Those students
whose performance can be categorised as clearly and safely above the required standard
from these first 4 stations wil be exempt from completing the remaining 4 stations.
Such a student must have:
• Raised no serious concerns related to professional or unsafe practice.
• A mean station mark higher than 3.00 (i.e. an aggregate score of 13 or more).
• No station mark less than 3.
• An aggregated in-course and end-of-year Clinical Skil s mark of 3.00 or greater
Students whose performance cannot be categorised as clearly and safely above the required
standard wil be required to complete the remaining 4 stations, with decisions made on
performance in all 8 stations.
The mark obtained in the end of year OSCE wil contribute 80% of the final Clinical Skil s mark.
In order to progress to Year 3 a student
must pass both the Written and Clinical Skills components.
- 28 -
ELM 3
Written component:
• Three 3-hour exams consisting of case-based short answer question (SAQ) papers (two-
thirds) and MCQs (one third), which may cover any of the learning objectives addressed
during the year (i.e. material from block and vertical modules, Integrated Cases, Clinical Skil s
and Early Professional Experience). Clinical Skil s is included here not because the intention
is to assess in detail Clinical Skills material (which is assessed in the Clinical Skills
component), but because as an integrated programme, it is highly likely your knowledge
from Clinical Skil s wil be relevant to some questions in the exams.
• One 1-hour OSPE, which wil consist of approximately 50 questions that wil include
questions on anatomy (including histology) and pathology.
• The mark obtained in the SAQ/MCQ papers and OSPE wil contribute 80% (73% for
SAQ/MCQ papers and 7% for OSPE) to the final Written mark. Note that a minimum mark of
45% is required in the end of year OSPE to pass the Written component.
Examples of previously used case-based short answer examinations are available on the Central
Library website (there is a hot link in the blue banner of the website) and the URL is:
http://www.library.otago.ac.nz/exams/index.html
Clinical Skills component:
• One OSCE (Objective Structured Clinical Examination) consisting of a maximum of 8 x 7-
minute stations, marked on a 1 to 5 scale. These stations wil be drawn from the defined
tasks outlined in the Clinical Skil s objectives and wil include clinical examination and history
taking skil s. A sequential testing approach is taken. All students wil initially attempt 4
OSCE stations (consisting of two History Taking and two Clinical Examination stations).
Those students whose performance can be categorised as clearly and safely above the
required standard from these first 4 stations wil be exempt from completing the remaining
4 stations.
Such a student must have:
• Raised no serious concerns related to professional or unsafe practice.
• A mean station mark higher than 3.00 (i.e. an aggregate score of 13 or more).
• No station mark less than 3.
• An aggregated in-course and end-of-year Clinical Skil s mark of 3.00 or greater
Students whose performance cannot be categorised as clearly and safely above the required
standard wil be required to complete the remaining 4 stations, with decisions made on
performance in all 8 stations.
The mark obtained in the end of year OSCE wil contribute 75% of the final Clinical Skil s mark.
In order to progress to Year 4 a student
must pass both the Written and Clinical Skills components.
AWARD OF DISTINCTIONS
Distinction wil be awarded to those students achieving an excellent performance standard in their
assessments. This wil normally require a mean aggregated score of 4.20 or greater, with a minimum
score of 3.80 in each of the aggregated in-course and end-of-year scores for the Written and Clinical
Skil s components.
- 29 -
The student’s professional conduct (there should be no current concerns about a student regarding
their professional conduct), and staff and student nominations for a Dean’s Commendation may also
be taken into account when awarding a student Distinction.
DEAN’S COMMENDATION
Students receiving at least 2 nominations from staff and 10 from peers, and who have met their
Terms requirements, wil receive a Commendation from the Dean of the Otago Medical School.
- 30 -
RULES FOR FINAL EXAMS
1. You must be on time for the exam - if you are late beyond a designated cut-off time you wil
not be admitted to the exam.
2. You are not permitted to take papers into the exam room other than those
provided/allowed as part of the examination.
3. Devices with communication capability are not allowed in the examination or in the
sequestered areas before or after the examination this includes smart watches and mobile
phones.
4. No watches are allowed in the OSCE.
5. If you are unwel when an exam is held, and your performance was impaired you should
obtain a Special Consideration application form from Student Affairs and complete this
within 24 hours of the exam. You wil also have to provide a medical certificate.
NOTES ABOUT EXAMINATIONS
Examinations in the medical course are conducted under the general examination regulations of the
University 2021 and under the regulations of the Otago Medical School (University of Otago
Calendar, 2021, Examination Regulations).
You should note that you are required to sit all relevant papers in the final examinations in October
and November and you may not defer sitting any paper(s) until the special examinations. Note also
that no candidate shall communicate with an examiner regarding an examination before results are
published, except through the Manager, Student Administration (University of Otago Calendar,
2021, Examination Regulations).
EXAM IMPAIRMENT
The following is summarised from the MB ChB Assessment Policy and Procedures Manual
(https://www.otago.ac.nz/oms/education/mbchb/current-students/resources/policies-
guides/index.html)
Special Consideration for students with temporary health conditions or exceptional circumstances
affecting performance
Refer also: University of Otago Special Consideration in Final Examinations policy
MB ChB students do NOT apply through eVision for Special Consideration for assessments.
One purpose of assessments and examinations is to inform progress decisions, based on whether
students have achieved a standard equivalent to a Fail, Conditional Pass, Pass, Potential Distinction,
or Distinction in in-course assessment; or a Fail, Pass, or Distinction for the year.
A student may have some temporary impairment arising in the two weeks before the assessment,
and in effect at the time of an assessment that may affect their performance and hence the result.
Alternatively, a student’s performance may be impacted by a health-related event during an
assessment e.g. a nosebleed or by their finding an assessment item particularly disturbing.
Special Consideration regulations are intended to apply in cases where a student’s performance is
seriously impaired, or absence is due to health-related events or other exceptional circumstances
- 31 -
beyond a student’s control. Students and staff should be aware that the Medical School has its own
processes in relation to applications for Special Consideration in in-course assessments and final
examinations.
Special Consideration in end-of-year assessments
As stated in 5.4 of the Examination and Assessment Regulations 2014 section of General Regulations,
aegrotat passes are not offered to students in the MB ChB programme.
In general, if a student is unable to sit an examination on a particular day because of acute il ness or
other exceptional circumstances at the time of the examination OR considers that their performance
in any examination has been seriously impaired due to il ness or other exceptional circumstances,
they should
notify the ELM Associate Dean for Student Affairs (ADSA) and the Otago Medical
School Office of their intention to submit a Special Consideration application preferably before,
but always within 1 business day of the examination.
The Medical School
Special Consideration application form is available from the offices of the
Associate Dean of Student Affairs.
Applications should be completed and submitted as soon as possible after the last examination for
which Special Consideration is sought, preferably within 1 business day, but always within 5 calendar
days, e.g. if your last examination is on the 20th, your application is due no later than the 25th.
As the ELM Board of Censor’s BoCs meets very soon after the completion of end-of-year
examinations, students applying for Special Consideration should understand that there may be
significant delays in receiving their final grade should the completed application postdate the BoC
meeting.
The application and supporting documentation wil be considered by an advisory group consisting of
the Director ELM, ELM ADSA, Associate Dean of Medical Education and the ELM Assessment
Convenor who may ask examination organisers to act as information providers in reaching a
decision.
To preserve the confidentiality of claimants the advisory group wil report only the degree of
impairment of to the BoC.
At the discretion of their BoC, a student whose application for Special Consideration is accepted may
be offered the opportunity to sit an alternative assessment (mandatory in the case of missed end-of-
year examinations). The Board wil ensure that the alternative assessment for a student who has
missed, rather than failed, an assessment is added to the col ective evidence and is equal y robust as
that missed.
Where a student’s result is close to a decision-making threshold(fail/pass/distinction), adjustments
accepted by the Board in making their decision may lead to a decision that is different to that of the
result alone.
SPECIAL EXAMINATIONS/ASSESSMENTS
Special examinations and other additional assessments deemed appropriate by the Boards of
Censors to inform progress decisions.
Admission to Special assessments is granted by the student’s BoC, who reviews the student’s Terms
status and professional conduct in making their decision.
- 32 -
Refer to:
2.3.3 Award of Terms and
2.4 Decision making at the end of ELM2 and ELM3
Special assessments as a deferred end-of-year examination (Special (incomplete) assessments)
The Board of Censors may grant students an opportunity to sit a Special assessment to those who
for exceptional reasons such as il ness, family bereavement etc. were unable to sit the scheduled
end-of-year assessments.
Students are notified of their admission to Special (incomplete) assessments by email from the
Medical School Administration, fol owing the BOC’s meeting.
Students who consider that the exceptional circumstances that prevented them sitting the end-of-
year assessments wil also prevent them sitting the Special assessment, should contact the OMS
office ([email address])and the ELM Associate Dean of Student Affairs as soon as
possible.
• Students sitting Special (incomplete) assessments are not required to pay the University of
Otago Special examination fee.
• Students sitting Special (incomplete) assessments wil receive a Distinction, Pass, or Fail
result; this is not identified as a SC (Special Consideration) on their academic record.
• Students who do not sit the Special (incomplete) assessment would be general y be
expected to repeat the year, where eligible.
• Students sitting Special (incomplete) assessments are general y not offered a Special (re-sit)
assessment should they fail to Pass the Special (incomplete) assessment.
Special (re-sit) assessments
If a student fails to demonstrate a satisfactory performance in an end-of-year assessment, they
may be al owed to sit a Special assessment with equivalent coverage of domains and core
elements. They wil be required to pass this Special assessment prior to entering the next year of
their course.
• Students sitting Special (re-sit) assessments are required to pay the University of Otago
Special examination fee.
• Students sitting a Special (re-sit) examination wil receive a Pass or Fail result; this is
identified as a SC (Special Consideration) on their academic record.
• Students who do not sit the Special (re-sit) assessment would be expected to repeat the
year, where eligible.
Consequences
Students are normal y al owed to repeat a year of the medical course only once. If a student who has
previously repeated a year of their course then fails to reach the pass criteria at the end of the year
(and in a Special assessment, if offered), their BoC wil usual y recommend to the Otago Medical
School Academic Board that they be excluded from further attendance in the medical course.
ELM2 and ELM3 students comprehensively failing both the OSCE and written components (refer
2.4.5 in MB ChB Assessment Policy and Procedures Manual)) would
not usually be offered Special
(re-sit) assessments
- 33 -
GENERAL INFORMATION
TIMETABLES
Please note that the ELM teaching day extends from 9am until 6pm, with the occasional 8am
lecture.
All streams wil have one tutorial in the 4-6pm time slot routinely. Others may be added as
necessary.
Unfortunately, we cannot move students between tutorial groups or streams to avoid these tutorial
obligations unless they have extenuating personal reasons, such as childcare arrangements.
Please note that the timetable is subject to continual change (sometimes daily). The timetable is
published on Moodle and this is the most up to date version.
SCHOLARSHIPS AVAILABLE TO SECOND YEAR STUDENTS
Information on scholarships is available on
https://www.otago.ac.nz/oms/education/mbchb/current-students/support/scholarships/
DEAN’S MEDICAL STUDENT RESEARCH SCHOLARSHIPS
Otago Medical School is a research-intensive and research-lead medical school. Building clinician
scientist capacity and promoting research intensity is the top priority for the Otago Medical School.
This scholarship is provided to encourage medical students to undertake research over a period of
12 months while pursuing usual academic study for the MBChB programme. The opportunity is
voluntary (no academic credits) and suited for students who are interested in pursuing a clinician-
scientist pathway and to become scientific leaders in their professional careers in future.
The scholarship wil be advertised at the end of each academic year for Dunedin based MB ChB
students enrol ing in ELM3, ALM4 and ALM5 at the Dunedin Campus the fol owing year. The
number of scholarships wil be determined at the time of advertisement.
UNDERTAKING ADDITIONAL STUDY
If you wish to enrol in any additional course of study during Years 2 or 3 you must first gain
permission from the ELM Director. The medical course is a ful time and intensive course of study in
itself, however, in some circumstances permission to undertake additional study is approved. You
wil need to provide evidence that it wil not interfere with your performance in Medicine. Each case
wil be considered on its own merits.
VACCINATIONS
Second year
All students entering Medical School wil be assessed for the need for vaccination. Individuals with
possible exposure to tuberculosis wil be referred to a respiratory physician for further assessment
and management. Students who are non-immune to Rubella and Hepatitis B wil be offered
vaccination. Students found to have HBsAg wil be referred to Student Health Services for further
management.
- 34 -
Third year
Students should be ful y vaccinated for Hepatitis B and Rubella, and Tuberculosis testing should have
been performed. Immune status information is available through the Immunisation Service contact
person: Melanie Philip ([email address])
Student Health Services
Te Ratoka Hauora Akoka
University of Otago
Cnr Walsh and Albany Streets
PO Box 56, DUNEDIN 9054
Telephone: (03) 479 8212
Freephone: 0800 479 821
For further information please refer to the Faculty Policies website: http://micn.otago.ac.nz/faculty-
policies.
IF VACCINATION IS NOT COMPLETED BY THE END OF ELM 3, TERMS WILL BE DEFFERED AND YOU
WILL NOT BE ABLE PROGRESS TO 4TH YEAR UNTIL SATISFACTORY COMPLETION OF THE
VACCINATION PROGRAMME.
CULTURALLY SENSITIVE ISSUES
Medical students are required to participate in all laboratory, practical and clinical activities, which
include activities that may not be usual in your culture. In the professional classes, some aspects of
the teaching wil require individuals to practise certain techniques on each other, which may require
you to partly undress and may involve body contact between students. Training is done under close
supervision and all students are required to participate, as it is essential for their acquisition of
clinical skil s. Assistance for students experiencing difficulties in this area is available, on request,
from the Students Affairs Office.
ANATOMY MUSEUM
Information about the Museum can be found at http://anatomy.otago.ac.nz clicking on the Facilities
and Services link and then Anatomy Museum. Information can also be found on Moodle.
COMMUNICATION
Please inform the Student Affairs Office, ground floor, Sayers Building of any change of address and
also update your details via e-vision.
E-Mails
The Medical School uses your student e-mail address as the main way of communicating with the
whole class, as wel as individuals. It is your responsibility to clear your e-mails daily and keep your
in-box as empty as possible so that you may receive new e-mails. Class e-mails that bounce back are
automatically discarded, so you may not be aware that you have missed an important
announcement.
Staff will not send mail to personal addresses (e.g., Hotmail or Yahoo).
It is strongly recommended that you DO NOT redirect your student e-mail to a Yahoo, Gmail or
Hotmail, etc. account.
- 35 -
Just as in written letters, there is an etiquette to email use that is respectful of the receiver. Emails
require introductions or salutations (‘Dear [name]’ or ‘Kia ora [name]’ ), clear writing without
shorthand, and the writer’s name at the end with a suitable acknowledgement such as ‘Best wishes’
or ‘Nga mihi’.
Mail
Mailboxes are located on the first floor, Dunedin Hospital (foyer of Colquhoun & Barnett Lecture
Theatres). Second- and Third-year mail is posted in the left-hand set of boxes.
Notice boards
These are located in the Hunter Centre outside the ELM Hub.
PROCESSES FOR HANDLING COURSE CONCERNS OR COMPLAINTS
If you are unhappy or have concerns with aspects of the ELM programme or staff members try:
•
instant resolution: if you can make your feelings known to the person most directly involved,
you may be able to resolve the issue straight away.
•
assistance from a staff member: you can seek advice from your Lab Supervisor, Module
Convenor, ELM Course Administrator, Director of the ELM Programme, or the relevant Head
of Department.
•
register a concern with the ELM Programme: this is an informal system for you to flag a
concern anonymously and in writing. If a number of similar concerns are received the ELM
Programme wil act to resolve the issue. See your Education Representative to obtain the
form for completion. Forms are available in the Hunter Centre outside the
Module/Assessment Administrator office.
•
mediation assistance: you can contact the University Mediator ([email address]) for
advice. If you wish to accept mediation the Mediator wil assist you and the other person to
talk through your problem.
•
register a formal complaint: if the preceding processes are not effective you can register a
formal complaint with the University. To read the Policy go to:
http://www.otago.ac.nz/humanresources/policies/EthicalBehaviour/index.html
RECORDING LECTURES, PATIENT INTERVIEWS AND CLINICAL PRESENTATIONS
Recording of patient interviews or clinical demonstrations by students is NOT permitted under any
circumstances.
Patients have not been asked for permission and it is inappropriate for students or others to request
permission at the time of the demonstration. Please ensure that you respect the confidentiality
implicit in all clinical demonstrations.
Please note that only students enrol ed in MICN201 and MICN301 are permitted to attend teaching
sessions, including patient interviews and clinical presentations.
- 36 -
STUDENT PROBLEM DIRECTORY
If you:
Are unwell and unable to attend, you must directly notify
your tutor(s) before any tutorials that day,
as wel as
the ELM Administrator [email address])
Need to apply for absence from classes for longer than 3 days:
go to the office of the Associate Dean for Student Affairs (Ground Floor, Sayers Building for a form or
download from Moodle)
Have been absent for longer than 3 days due to il ness:
inform the office of the Associate Dean for Student Affairs, and the ELM Administrator
([email address], and provide a medical certificate as soon as possible as wel as a Leave
of Absence form
Have a question about computer tests or exams:
contact the Assessment Administrator or Convenor ([email address])
Have a question about your academic progress or general academic matters:
contact the ELM Administrator ([email address]) for an appointment with the Director
Need to discuss confidentially a personal or health related matter which is affecting your studies:
contact the Associate Dean for Student Affairs ([email address])
NON-ACADEMIC PROBLEMS
If, during the year, you have problems of a personal nature, which are affecting your coursework you
are advised to contact the Student Affairs Office, Ground Floor, Sayers Building to let them know of
your difficulties.
FIRST AID (ELM 2 ONLY)
Students must provide a certified copy of an appropriate current New Zealand first aid certificate as
part of their application for admission. This certificate must have been gained through a NZQA
registered training provider who is authorised to assess NZQA first aid standards. The certificate
should include at least NZQA Standard 6401 and NZQA Standard 6402, but students are
recommended to obtain a qualification, which includes the higher NZQA Standard 6400. The
fol owing are a selection of recommended training courses:
• OUSA (Comprehensive First Aid)
• St John (First Aid Level Two)
• New Zealand Red Cross (Comprehensive First Aid Course)
• MediTrain (Comprehensive First Aid Course)
HEALTH SCIENCES LIBRARY
The Health Sciences Library, a branch of the University Library, is found on the first, second and third
floors of the Sayers Building (opposite Dunedin Hospital’s main entrance). See
https://www.otago.ac.nz/library or information about the University Library.
Hours
See https://www.otago.ac.nz/library/hours or Library notice boards for variations and changes
relating to opening hours.
- 37 -
Information and Research Skills
Through the Liaison Service the library offers a range of support for individuals, small groups and
whole classes. Contact your Subject Librarian to make an appointment (see the Health Sciences tab
at https://otago.libguides.com/liaison)
For access to key resources look at your Subject Guide https://otago.libguides.com/medicine. Note
that some point of care tools are available via mobile devices.
Borrowing material (see https://www.otago.ac.nz/library/quicklinks/borrowing/index.html
)
Loan Periods Print Up to 50 items for 4 weeks with 3 renewals. You can renew non-Reserve
items: books through the My Account section of the Library
Catalogue https://www.otago.ac.nz/library/primo/redirect/myAccount.ht
ml.
Reserve Up to three items for 2 hours during opening hours This material may be
Collectio booked in advance and renewed if not required by another borrower.
n (print):
Overdue fines: Reserve Collection: $0.10 per minute ($6 per hour)
Recalled Overdue Items: $3 per day
Please note that the library does not accept cash. You can pay fines using EFTPOS or your ID card.
Photocopying
Multifunction printers/copiers are situated on the First, Second and Third floors: the current cost
is 10c per A4 page. Information on copyright regulations is posted on notice boards near copiers.
University of Otago Student ID cards can be loaded with credit for copying and printing (note that
hospital ID cards cannot be loaded with credit). Visitors can borrow cards which have to be loaded
with credit before use.
Computers and Printing (see https://www.otago.ac.nz/library/using-the-library/print-copy-
scan/printcopyscan.html)
All University Libraries are wireless enabled, although you wil have to configure your device to
connect to the University network. The Health Sciences Library has desktop computers, mono and
colour printers available for student use. You wil need your username and password to use desktop
computers.
Interloans Service
Items which are not held in the Library may be requested at no charge, except for loans from outside
Australasia. Apply through the Interloans Service. See
https://www.otago.ac.nz/library/interloan.html
Students with Disabilities
There is a small study carrel - the Lee Gibson Room - available in the Health Sciences Library for
students with a disability. Bookings must be made through the Disability and Information Support
- 38 -
Office. Special equipment can be made available to Health Sciences Library users through the
Disability and Information Support Office as required. See
https://www.otago.ac.nz/library/disability/index.html.
Please let Health Sciences Library staff know if there is any way that we can assist.
Health Sciences Contact details
Service Desk/Renewals
479-7401
Health Sciences Librarian
479-7403
Health Sciences Liaison Librarians
479-7407, 479-7237, 479-7459
Email
[email address], [email address]
- 39 -
IMPORTANT DOCUMENTATION
The fol owing are important documents relating to patient privacy and confidentiality that you
should be aware of. Even though these issues are more compel ing in the Advanced Learning in
Medicine Course you need to apply the principles on a more limited scale during the ELM course.
PRIVACY AND CONFIDENTIALITY
Medical students are expected to observe the same high standards of confidentiality and respect for
privacy as govern the behaviour of all doctors and healthcare professionals. These standards are set
in the Privacy Act 2020 and the Health Information Privacy Code 2020 (The Privacy Code or HIPC).
The Privacy Code outlines specific rules regarding the collection, storage and disclosure of health
information in relation to identifiable patients. The basic rule is that no information about any
patient should be given to any other person without the permission of the patient concerned. This
applies to al health information and not only to that which the patient might regard as particularly
sensitive. It applies to the simple fact that an individual is a patient in the hospital or GP rooms as
wel as to details of their condition. It also includes situations such as reports to lawyers, NZ Police,
ACC and various other statutory bodies. There are some limited and specific exceptions where
disclosure of information without the consent of the patient is permitted or authorized by law and
you wil learn about these over the next years of your training.
It is important to remember that patients share information with health professionals within a
relationship of trust and in order to assist the professional to help them with their health problem.
Respecting that trust and maintaining respect for privacy and confidentiality is fundamental to the
doctor-patient relationship and achieving the best outcome for the patient.
ACCESS TO NOTES AND HANDLING OF WRITTEN MATERIAL
Students should only access patient notes with the consent of the patient and where the patient is
under the care of the team to which the student is attached. Notes of patients not under the care of
the team should not be accessed except where the student has an alternate legitimate reasons to do
so and also has specific consent from the patient.
Official patient hospital records must never be taken away from the clinical areas or out of the
hospital. Photocopying of patient notes by medical students is not permitted in any circumstances.
Material written by students which may contain patient-related information (eg case histories)
should not have any ‘unique identifiers’ (eg name, date of birth, address or national number). If
these notes require work outside the hospital (eg library) great care must be taken to ensure they
remain secure and private. Once patient related notes are no longer required they should be
disposed of in a secure fashion in one of the bins provided by the SDHB.
In addition to legal restraints around patient related health information, students are required to
discuss any matters referring to the Dunedin Campus and SDHB with the Dean BEFORE disclosing
information to outside agencies or bodies.
The following points should be also kept in mind:
Medical students should refrain from giving a patient a blanket guarantee of confidentiality, as this
may contravene their accountability to their supervising clinician. Whether information is acquired
at interview or from the clinical record, patients have a right to know the use(s) that wil be made of
the information [written assignment, oral presentation to a tutorial group, one to one discussion
with a tutor, etc], and what steps wil be taken to assure the privacy of the information [such as de-
- 40 -
identifying]. Medical students should make sure when, if at al , a copy of an assignment should be
placed in the patient's notes, and patients should be informed of this
Medical students should be meticulous in assuring the security of written assignments and other
notes relating to patients, even if de-identified, and should regularly dispose of material which has
passed its use by date through an approved destruction process.
Care should be taken to ensure that discussion of a patient for clinical education takes place in a
secure setting where what is said cannot be overheard by others and where there is thus no risk of
what is discussed being mis-interpreted.
Under no circumstances is a medical student permitted to take photographs of a patient or patient
information, or to make any video or audio recording of any interaction with or observation of a
patient. If photographs or recordings are needed for educational purposes, they wil be sought by
the supervising clinician using current protocols.
RELEASE OF INFORMATION
Various pieces of legislation including the Health Information Privacy Code and Health Act, outlines
circumstances where personal details may be released without the consent of the patient or their
representatives. The Privacy Act does not apply if release of information is required under other
legislation. For example, the notification of infectious diseases is required under Section 74 of the
Health Act.
Medical students must not release any information under these provisions without first consulting
the senior clinician working in this area. Students who make unauthorized disclosure of personal
health information wil be subject to disciplinary action, and may also be in breach of the Privacy Act
and the Health Information Privacy Code.
Students are required to consult with the Associate Dean of Student Affairs BEFORE disclosing
information about the School or any of the DHB institutions to the news media.
MEDICAL STUDENT RIGHTS
Medical students have the right to decline to participate in clinical teaching/or patient care if there
are concerns, ethical or otherwise about the activity; concern about their own competency, lack of
knowledge, or lack of understanding of the duties/tasks/responsibilities involved; or conscientiously
believe there is a lack of explanation or supervision.
THE USE OF ONLINE SOCIAL MEDIA
The Internet immediately connects us with the public domain, and we must continue to avoid
making comments or posting material that could be interpreted as breeching the boundaries of
patient-doctor confidentiality.
While blogging, tweeting and other social networking avenues are, for the most part, wel
intentioned, there is the potential for these activities to have future adverse consequences. As
members of a professional community with high ethical standards, any comments, images and
material you may leave on a personal page could embarrass you when seeking future employment.
Any photos of patients, aspects of patient care, procedures etc MUST NOT be placed on social
media. This includes material that you might gather while you are on elective overseas. The rule of
thumb in this situation is to behave exactly as you would in New Zealand. The standards that you
wil be held to account over, are the same.
- 41 -
Code of Health and Disability Services Consumers Rights
This is available for viewing at: www.hdc.org.nz
OPPORTUNITIES FOR RESEARCH
Bachelor of Medical Science with Honours (Third and Fifth Years)
This is a ful -time, one-year course enabling a student to undertake research in an area of medical
science that particularly interests them. It involves doing some original research under supervision
and the writing of a thesis. Tuition fees are waived by the Otago Medical School and scholarships
are available. Applications close the 1st Friday in August. A seminar for interested students wil be
held on in the Octagonal Room, 1st floor, DPH. The course may be undertaken in Wel ington,
Christchurch or Dunedin at the end of the Third or Fifth Years of the Medical Course and it must be
completed within one year. For details on the regulations refer to the University of Otago Calendar,
and, for advice, consult the Associate Dean for Student Affairs, or Associate Dean Research,
Associate professor Aniruddha Chatterjee (phone: 479 7172, email:
[email address]).
Summer research scholarships (all years)
Over the summer vacation at any stage in the medical course, students may apply for a Summer
Research Scholarship. The scholarships involve supervised research for a 10-week period fol owing
which students write a short report and may be required to give an oral presentation. There is a
grant paid to successful students. Notices about the Summer Scholarships are put up on notice
boards in mid-June and the due date for applications is usually late August. Contact persons are as
fol ows:
Dunedin:
Christchurch:
Wel ington:
Dr Manon Knapen
Virginia Irvine
Christine Groves
Research & Development Research Officer
Research Office
Health Sciences
Christchurch School of
Wel ington School of
Administration
Medicine
Medicine
P.O. Box 56
P O Box 4345
P O Box 7343
Dunedin 9054
Christchurch
Wel ington
DIVISION OF CLASS FOR ALM
Facilities for the teaching of the Fourth, Fifth and Sixth years of the course for MBChB are provided
in the University of Otago, Schools of Medicine in Dunedin, Christchurch and Wel ington. After
completion of Third year, the class wil be divided (three-ways) and each student allocated to one of
the three schools for the remainder of the course. In dividing the class for years 4, 5 and 6, account
wil be taken of each student’s personal preference as far as possible. However, if the number of
applicants for entry to any one of the schools of medicine exceeds the number of places available, a
ballot wil be held to determine which students wil be required to take a place in one of the other
schools (University of Otago Calendar). This includes international students who wil be allocated
among the three schools. This is to ensure an even distribution of International students in all
centres.
No transfer is possible between the Auckland and Otago Schools of Medicine at this stage in the
programme. Class meetings to discuss the class division process wil be held during the third year of
the medical course. This process wil be finalised by the end of August of each year.
- 42 -
Student Parents in the 3rd Year Class Division
Student parents can request exemption from being balloted in the division of the medical class
during 3rd year. Prior to the ballot taking place, the Student Affairs Office wil email the 3rd year
class to seek applications for exemption under this policy. From this point, it is the responsibility of
the student parent to notify the Student Affairs to confirm they wish to be exempt.
Please see further information on Support for Parents regarding class division -
https://www.otago.ac.nz/medicine/current-students/resources/policies-guides/index.html
Below is an example of the process you wil go through for Class Division. Please read this carefully
so that you ful y understand the process and sign the declaration cover sheet. Agreeing to this
policy is a condition of entry into Medicine.
- 43 -
Third Year Medical Class 2021
Timetable for Choice of School of Medicine for 2021 (Dates to be confirmed)
Monday 22 February 2021
9.20 am, University of Otago, Castle 2 Lecture Theatre. Outlining
timeline for class division.
Colquhoun - Reminder about class division process.
Meet with sponsored and private international students in third
year, 12 pm, Octagonal Room, 1st floor Dunedin Hospital.
Colquhoun Lecture Theatre. Representatives from the University
of Otago, Schools of Medicine in Dunedin, Christchurch and
Wel ington speak to class. Moodle School preference
questionnaire opens.
Moodle preference questionnaire closes at 5 pm. If you do not
choose your preference, you wil be allocated to the school(s)
with the least numbers.
Students wil be advised, via Moodle of numbers and any need
for a Bal ot. If necessary, students who are prepared to change
their preference must notify Student Affairs Office, in writing by
TBA
Colquhoun Lecture Theatre further update on numbers and
notification if ballot required. If so, ballot wil take place, in
conjunction with OUSMA. Letters of confirmation of school
placement and/or ballot letters emailed to student within two
days. An appeal Form wil be attached to these emails for those
who have been bal oted.
Students who have ben bal oted wil be instructed to write a
letter of not more than three pages, outlining the reasons they
believe their appeal should be considered.
Appeal forms returned to Student Affairs Office by 5 pm.
Deliberations of Appeal Committee outcome emails sent to those
balloted.
Declaration:
We wish to remind al students that you cannot be guaranteed a place in the School of Medicine of
your choice for the Fourth, Fifth and Sixth years of the Medical Course, and that you signed a
- 44 -
declaration at the beginning of your second year, agreeing to accept direction, if necessary, to one of
the University of Otago, Schools of Medicine in Dunedin, Christchurch, or Wel ington after
completing the Third Year of the Course.
Timeline for Integrated/Double Degree (dates and times to be confirmed)
Integrated/Double Degree
BMedSc (Hons) Seminar for third- and fifth-year medical students, 1-2 pm, Octagonal Room, first
floor, Dunedin Hospital. Topics to be placed on Moodle.
Closing Date for BMedSc(Hons) applications is Friday 6 August 2021.
All Integrated/Double Degree applications and applications for
withdrawal, close with the Manager, Faculty of Medicine by 5
pm.
Withdrawal & Readmission Guidelines
Any student wishing to withdraw from the medical course either temporarily or permanently is
advised to discuss this decision early with the Associate Dean of Student Affairs (Ground Floor of the
Sayers building).
These procedures should be read in conjunction with MB ChB Regulation 7 – Withdrawal from the
Programme.
Note: Deferrals before the end of the third week of Second Year
A student who withdraws before the end of the third week of the course in the year of admission to
second year classes and wishes to recommence the following year must first obtain approval for a
deferral, which wil be considered by the Medical Admissions Committee. Any such applications wil
be dealt with under the regulations governing admission to the programme.
1. Permanent Withdrawal
Students who withdraw from the medical course permanently (including students who
withdraw without approval and students who fail to communicate their intentions within 12
months of when they last enrol ed or for any 12-month period) have no right to be
considered for readmission. However, note Regulation 7cii.
Exit Options – Qualification
Students who withdraw permanently and who have passed 3rd year Medicine may be
entitled to apply for the award of a Bachelor of Health Sciences (BHealSc) degree with no
further study or enrolment.
Exit Option – Additional Study required
I. (After award of the BHealSc) in 300 level papers to complete a Diploma for Graduates
(DipGrad) in certain disciplines
II. to complete a Bachelor of Science (BSc) or Bachelor of Biomedical Science
(BBiomedSc) degree in certain disciplines,
III. in some cases, a Bachelor of Medical Science (Honours) BMedSc(Hons).
IV. for some students to complete a Bachelor of Arts (BA) or Diploma in Public Health -
Master of Public Health.
- 45 -
Further details about Exit Options are provided in the document “Exiting from the Medical
Course after 3rd Year” on the Otago Medical School (OMS) website
www.otago.ac.nz/medicine.
2. Temporary Withdrawal
Withdrawals for more than one year wil not be approved other than for exceptional
circumstances (but see MBChB/PhD)
Permission to withdraw with a right to apply for re-admission must be granted by the OMS
Academic Board prior to withdrawal, prospectively. Applications for withdrawal should be
made to the Associate Dean Student Affairs/(ADSA). See also note 4 – application deadline.
OMS Academic Board wil take into account the reasons for withdrawing, suitability for
readmission, preparedness for readmission and availability of places in the programme. See
also (c) below. Students who withdraw from the course for more than one year must show
cause why they should be allowed re-entry. In general withdrawal for more than one year,
apart from integrated degree studies, wil not be permitted. Any such student who can re-
enter the course may be required to resit specified examinations or undergo other forms of
evaluation determined by the Dean, Otago Medical School, to ensure that they are prepared
to progress to the next part of the course.
Categories for which temporary withdrawal for one year may be approved are:
I. Integrated programme of study, i.e. BMedSc(Hons), BSc or BBiomedSc, BA, DPH/MPH
See (a) below
II. Other academic study (between 3rd & 4th year or between 5th & 6th year). See (a)
below
III. Health (at any time). See (b) below
IV. Compassionate or parental responsibilities i.e. care of a child (at any time). See (b)
below
V. Travel – where a case is made that a “gap” year would be beneficial to the student
(between 3rd & 4th year or between 5th & 6th year). See (c) below
VI. Other – individual circumstances e.g. significant financial hardship (at any time). See
(c) below.
SPECIAL NOTES
a) Refer category 2(i) - Following 3rd Year or 5th Year - Students who withdraw to complete an
Integrated/Double Degree qualification such as a BMedSc(Hons), BSc, BBiomedSc, BA,
DPH/MPH or category 2(i ) other academic study, which has been approved by OMS
Academic Board, are guaranteed re-admission to the course in the next academic year.
Refer to Other Study Options documents on the OMS website www.otago.ac.nz/medicine.
Students approved for admission to MBChB/PhD are also approved for two years temporary
withdrawal according to the structure of the Integrated programme.
b) Refer categories 2(i i) and (iv) - Health or compassionate reasons - Students who withdraw
from the course for health or on compassionate grounds must apply for readmission by the
1 of June in the preceding academic year (or at the time of their withdrawal if that time is
after 1 June in the preceding year). Students applying for readmission wil be interviewed by
the ADSA or the Dean, Otago Medical School. Students who withdraw from the course on
health grounds wil be required at this time to provide a full medical or psychological report
including a description of the student’s il ness, treatment, and current state of health, with
an opinion about their fitness or otherwise to re-join the course, OMS Academic Board wil
allow re-admission, if it is considered that the student wil be able to complete the course.
Students who withdraw for two or more years may be required to resit specified
- 46 -
examinations to ensure that they are adequately prepared to progress to the next part of
the course.
c) Refer categories 2(v) and (vi) – Travel/Gap year (following 3rd or 5th year) and Other. -
Students who withdraw from the course under these categories must apply for re-entry by
the 1 of June of the preceding academic year. Students applying for re-entry wil be
interviewed by the ADSA or the Dean, Otago Medical School. Students withdrawing under
categories 2(iv) and 2(v) are required to provide a statement – not more than one A4 page,
at the time of withdrawal outlining their plans for the gap year/year off. The OMS Academic
Board wil consider and rank applicants for readmission. The OMS shall determine the
number of places available in the year of readmission. Where the number of students for
readmission exceeds the number of available places, then the ranking wil determine which
are successful applicants. In general, proposals which include plans for further study or
community service are more likely to be ranked highly. It is suggested that plans be
discussed with the ADSA.
In exceptional circumstances students may be able to withdraw between 2nd or 3rd year, or
between 4th and 5th year. Applications should be made to the ADSA. The ADSAs group shall
consult as necessary and a recommendation be made to the Dean, OMS. If withdrawal is
approved, all conditions and requirements for readmission as stated above shall apply.
1. Campus Al ocation
Students who withdraw for any reason after having commenced at a particular Campus
(Dunedin, Christchurch, Wel ington) would normal y be readmitted to the Campus they were
previously allocated to but could be directed to another Campus. The ADSAs from the three
Campus’ shall consult and a recommendation be made to the Dean, OMS
2. Application deadline
Students seeking withdrawal from study in the following Calendar year shall complete the
‘Application for Withdrawal Form’ and submit it to the appropriate ADSA no later than the
first Friday in August. Applications received after this date wil be considered only for
exceptional reasons or reasons beyond the student’s control.
- 47 -
MED 2 AND 3 TEXTBOOK LISTING
Note many of these textbooks are available as e-books through the Health Sciences Library. You are
advised to defer buying these until you have discussed possible purchases with course or module
convenors.
ESSENTIAL – total cost to student $958.50 (2020 prices)
ANATOMY
Drake, R.L., Vogl, W. & Mitchel , A.W.M.
Gray’s Anatomy for Students, 4rd Edition.
Churchil Livingstone, 2010.
ISBN:
9780323393041 $144.50
Covers clinical anatomy relevant to Musculoskeletal, Respiratory, Cardiovascular and Gastrointestinal
Block Modules in Years 2 and Regional and Clinical Anatomy and Renal Block Modules in Year 3 of
ELM. Good clear colour diagrams
Library notes: Available as ClinicalKey ebook. 9 print copies of 4th ed. in Reserve Collection
PHYSIOLOGY
Hal , J.E.
Guyton and Hal Textbook of Medical Physiology, 13 Edition, 2015
Saunders Elsevier
ISBN:
9781455770052 $199.50
Library notes: Available as ClinicalKey ebook. 1 print copy of 13th ed. in Reserve Collection
PHARMACOLOGY
Goodman & Gilman's Pharmacological Basis of Therapeutics, Thirteenth Edition, by Brunton, L.L.,
Chabner, C.B.A. & Knol mann, B.C. 13th Edition
ISBN-13:
9781259584732 $387.50
This is an extensive illustrated pharmacological text with a worldwide reputation as the core text for
therapeutics. It is available electronical y through the library.
Library notes: Available as Access Pharmacy ebook. No print copy of 13th ed. in Reserve Collection.
EARLY PROFESSIONAL EXPERIENCE (EPE) PROGRAMME
Wilson H, Cunningham W. Being a doctor;
Understanding Medical Practice.
University of Otago Press, Dunedin, 2013.
ISBN:
9781877578366 $32.50
This book is a very useful resource for all stages of training, both undergraduate and postgraduate. It
covers many aspects of undergraduate learning and of clinical work, including the more challenging
areas. Because it is written by teachers at Otago University, there are chapters that are specifically
relevant for EPE, Professional Development, and Clinical Skil s. There are two copies in the Library,
one in Closed Reserve. E Chapters are also available through the library.
- 48 -
Library notes: Available as ProQuest ebook. No print copy in Reserve Collection.
CLINICAL SKILLS
Nicholas Talley and Simon O’Connor
Clinical Examination: a systematic guide to physical diagnosis, 8th Edition.
Churchil Livingstone, 2010.
ISBN:
9780729542593 $194.50
Wil be held by the Medical Library, on reserve for students' reference. Tutorial notes in your
Workbooks wil make explicit references to pages in the textbooks where you can find extra
information.
You should note too that recently, Elsevier (the medical publishing company) granted our University
rights to mount the video segments that accompany the Talley and O'Connor textbook on a password-
protected internal web site. These video segments of physical examination skil s have been uploaded
and can be accessed from a link that you wil find in the Clinical Skil s resources on your MedMoodle
site.
Library notes: Available as ClinicalKey ebook. No print copy of 8th ed. in Reserve Collection
OPTIONAL BUT NOT REQUIRED
(1)
Crook, M.A.
Clinical Chemistry and Metabolic Medicine, 8th Edition (2012.
Hodder Arnold, 2006.
ISBN 9781444144147 $103.50
This text is highly recommended as it contains required reading for second year (Chemical
Pathology) and for third year (Endocrine Module and Clinical Biochemistry)
Library notes: No ebook available. 1 print copy of 8th ed. in Reserve Collection
(2)
Field, M., Pol ock, C., Harris, D.
The Renal System, 2nd Edition (2010)
Churchil Livingstone, 2001.
ISBN: 9780702033711 $60.50
(Covers renal physiology and pathophysiology around common clinical presentations – clear
concise explanation of renal physiology)
Library notes: Available as ClinicalKey ebook. 1 print copy of 2nd ed. in Reserve Collection
(3)
Immunology textbook
Mim’s
Medical
Microbiology
and
Immunology
6th
Edition
(Elsevier)
(https://www.elsevier.com/books/mims-medical-microbiology-and-immunology/goering/978-
0-7020-7154-6). $122.50
Library notes: Available as ClinicalKey ebook. No print copy of 6th ed. in Reserve Collection
Extra options for immunology:
For a concise overview: Immunology: An Illustrated Outline (Garland Science)
(https://www.routledge.com/Immunology-An-Illustrated-
Outline/Male/p/book/9780815345015). $47.50
Library notes: No ebook. 1 print copy of 5th ed. in Reserve Collection
- 49 -
For more detailed information: Kuby Immunology 8th edition (MacMil an International)
(https://www.macmil anihe.com/page/detail/?k=9781319114701&utm_source=Closer&utm
_medium=email&utm_campaign=2934_LIFES_Closer_Marketo_ML_ANZ_Punt&utm_conten
t=image_jacket_9781319114701&mkt_tok=eyJpIjoiWmpVeFl6RXhNVEEwT0RBeiIsInQiOiIyVE
RFZ0phTjN1MGptM2FFV0FBYzhBT3g4aUtCNWhYT3UxWDlHM0VMSnpHeGpCMyttMklVUGZj
S1RZU2tQcklENnlYNVh0QUNHTnJQQ3ZpQ3VQbWxqUUI2OUtqZkRpMVczcVRuUmVTbmRzZj
dGcHh6NWw3ZEsrVTVXTXFVR29uayJ9
Library notes: No ebook. 1 print copy of 8th ed. in Reserve Collection
(4)
Moore, K.L., Dalley, A.F.
Clinically Oriented Anatomy, 8th Edition.Lippincott Wil iams and Wilkins, 2017.
ISBN: 9781496347213 $146.50
Library notes: Available as LWW ebook. No print copy of 8th ed. in Health Sciences Library Reserve
Collection
(5)
Young, B., & Heath, J., (Editors)
Wheater's Functional Histology: A Text & Colour Atlas, 6th Edition (2013)
Churchil Livingstone, 2006.
ISBN: 9780702047473 $124.50
A useful core text of Histology)
Library notes: Available as ClinicalKey ebook. 2 print copies of 6th ed. in Reserve Collection
(6)
Longmore, M., Wilkinson, I., Turmezei, T., Cheung, C,K.
Oxford Handbook of Clinical Medicine, 10th Edition (2017)
Oxford University Press, 2007.
ISBN: 10th EDITION ISBN 9780199689903 $65.50
This a really useful handbook relating to clinical medicine. It is designed for junior medical
officers but stil offers accessible, relevant information for medical students at all levels of the
undergraduate programme).
Endorsed by Integrated Case
Library notes: Available as Oxford Uni Press ebook. No print copies of 10th ed. in Reserve Collection
PATHOLOGY
Kumar, V,. Abbas, A., and Aster J.
Robbins and Cotran
Pathologic Basis of Disease
10th edition
Saunders
ISBN: NEW 10TH EDITION
978-1-4557-2613-4 (ninth edition) $174.50
Hardcover ISBN: 9780323531139
Hardcover ISBN: 9780323609920
eBook ISBN: 9780323609951
eBook ISBN: 9780323609937
eBook ISBN: 9780323609944
Imprint: Elsevier
Published Date: 15th June 2020
- 50 -
The book covers more in depth information on the basic principles of Pathology and systemic
pathology, which is important for case-based teaching programme)
Library notes: Available as ClinicalKey ebook. 1 print copy of 10th ed. is on order for Reserve Collection
OR
Kumar, V,. Abbas, Fausto and Mitchel
Robbins Basic Pathology
Either 9th Edition, (2012) or 10th Edition, (2017)
Saunders.
ISBN: 9780323353175 $152.50
9781416029731 (hbk.) (8th Edition)
1416029737 (hbk.) (8th Edition)
9780808923664 (International ed.) (8th Edition)
0721692745 (7th Edition)
The book covers the basic principles of Pathology and systemic pathology, which is important
for case-based teaching programme
Library notes: Available as ClinicalKey ebook. 2 print copies of 10th ed. in Reserve Collection
METABOLISM – for reference only (purchase is not recommended)
Baynes, J W and Dominiczak, M H (2018) – Medical Biochemistry (5th Edition)
Library notes: Available as ClinicalKey ebook. 1 print copy of 5th ed. in Reserve Collection
Campbel and Farrel (2017) – Biochemistry (9th edition)
Library notes: No ebook. No copies of 9th ed. in Reserve Collection
Ferrier D R and Harvey, R A (2014) – Lippincott’s Illustrated Reviews: Biochemistry (6th
Edition)
Library notes: No ebook of 6th ed. No copies of 6th ed. in Reserve Collection
HAEMATOLOGY
Howard, M,R., & Hamilton, P,J.,
Haematology: an illustrated colour text, 4th Edition.
Churchil Livingstone, 2013
ISBN-13: 978-0702051395
ISBN-10: 070205139X (paperback)
This short text provides a basic preclinical and clinical introduction to Haematology
- 51 -
STUDENT SUPPORT AND WELLBEING
MEDICAL STUDENT SUPPORT/STUDENT WELLBEING
The link to the Student Affairs Student Support page is
https://medschool.otago.ac.nz/course/view.php?id=1309
This page includes some brief information about Student Affairs, some wel being resources , contact
information, and a link to be able to report concerns about intimidating behaviour in the learning
environment.
We very much welcome any comment about suggested developments and resources that people
have found useful that we could link from the page.
Reporting intimidating behaviour
The issues of reporting intimidating behaviour and implementing the informal reporting mechanism
recommended by a workshop of students and staff, were what drove this development initially. The
document endorsed by the Otago Medical School Executive is on the page, as is a link to a reporting
form. When someone submits a form, an email goes to Student Affairs who collate the forms and
pass them on to the newly formed Behavioural Assessment Team for discussion about action. We
wil email students regularly to remind them to use the reporting form if incidents of concern have
occurred. You may choose whether to put your name, email, or student group on the page. These
details would allow some feedback to you on what action was taken.
The reporting form is housed outside of Moodle and is confidential and secure - it is not linked to
your identity in any way unless you decide to include your name or other details.
Support for students is always available from Student Affairs. Just get in touch using the contact
details on the page.
Also on the page is a link to announcements on student support and wel being. We hope as time
goes on to use this more and more to tel students about support and wel being initiatives and
information.
UNIVERSITY STUDENT HEALTH SERVICES
University Student Health
Student Health Services is an enhanced primary care team providing holistic health care to students
of the Dunedin campus. The mental health and wel -being of students is a high priority and the
whole team are skil ed and familiar on how to engage on these issues with students. The team
includes GPs, nurses & mental health professionals. Students can make an initial appointment with
the mental health support team by contacting Student Health directly 0800-479-821.
The mental health & wel -being team is an approachable & responsive group of health professionals
dedicated to supporting students in their academic journey; this includes assisting academic staff
who recognise that a student may need assistance. The mental Health & Wel -being team provides a
range of programmes: educational, crisis response, individual and group depending on student need
and preference.
- 52 -
STUDENTS WITH DISABILITIES
If you have a disability or condition which, may adversely affect your studies please let your lecturer
or tutor know. They are reliant on you to make your needs known and wil try to meet these needs
wherever possible. The Dunedin School of Medicine has a staff member whose responsibility it is to
advise and advocate on behalf of students with disabilities and provide additional support in
conjunction with the Disability Information and Support Office.
The Disability Information and Support office provides students who are deaf, or who have long-
term injury, disability or medical condition with the resources they need in order to meet their goals
while enrol ed at the University. These resources are also available to students with hidden
disabilities such as learning, psychological or psychiatric disabilities. Students are encouraged to
contact the office at any time for support or information relating to the services available, or the
disabilities area in general. The key to any form of study is planning. If you think you may need
assistance, it is crucial you contact Disability Information and Support as soon as possible.
For more information, request a copy of the Disability Information and Support Handbook or
alternatively, visit the Disability Information and Support website <www.otago.ac.nz/disabilities>
• Phone: (03) 479 8245
• Fax: (03) 479 8221
• Email: [email address]
NZMSA Medical Student Welfare Webpage
For further information, please refer to: http://www.nzmsa.org.nz
INTERNATIONAL STUDENT SUPPORT
International Student Advisors
Coming to live and study in a new environment has many challenges and rewards. The International
Office supports international students from over 90 different countries to make the most of their
stay in Dunedin. The advisers are available all year round on a confidential basis to help
international students with advice and information on:
• International Student Orientation Programme
• Cultural adjustment
• Homesickness
• General health and wel being
• Letters confirming a student’s status
• Student services and support
• Flatting and accommodation
You can come and speak to an adviser at any time between 9.00am and 4.30pm, Monday to Friday,
no appointment is necessary. Their office is in the Basement, North End, Clocktower Building. You
can also phone them on 479 5777/ 479 5921 or email [email address].
Immigration
At the International Office we can process most applications for student visas on campus.
For further information refer to the website or email the Visa Officer.
• Website: www.otago.ac.nz/immigration/visas.html
• Email: [email address]
Student Mentor Programme
The International Office runs a Mentor programme to help new international students feel at home
in their new environment. New students are matched with senior students to provide friendly one-
- 53 -
on-one support and advice on settling into Dunedin and University life. The Mentor programme has
regular social events with the opportunity to meet other students and Mentors. If you are
interested in being part of the programme either as a Mentor or a Mentee, please email us at
[email address]
SCHOOL OF PHYSIOTHERAPY CLINICS
The School of Physiotherapy has two clinics offering services to students located at the School of
Physiotherapy on Great King St and at Unipol, Forsyth Barr Stadium
• Our Physiotherapists are highly qualified and have a diverse range of postgraduate
qualifications and clinical experience. They can help with a variety of problems including all
musculoskeletal injuries from neck and back pain to sports injuries and wel as neurological
and balance conditions.
• Our clinics also have a strong emphasis on healthy lifestyles and can help you kick start yours
with advice and help on types of activity best suited to you.
• You can book an appointment with a qualified staff member without any obligation to see a
physiotherapy student.
• A reduced fee applies for patients, ACC or private, who see our supervised physiotherapy
students.
• No referral required
For further information, please contact:
Clinic Reception
Phone: 479 5757
Fax: 479 5161
Email: [email address]
Website: http://physio.otago.ac.nz/clinics
- 54 -


CODE OF CONDUCT
Code of Professional Conduct for Medical Students at the
Universities of Auckland and Otago
In learning to be a doctor you are required to meet certain professional responsibilities and
expectations. These arise from your increasing involvement with patients, whānau and the wider
community as your learning progresses on your way to becoming a doctor. In particular, as you learn
to be a doctor in Aotearoa/New Zealand it is important to recognise your obligations to uphold
Māori rights under te Tiriti o Waitangi. Our position within the Pacific region and our formal
relationships with Pacific Island nations also require a commitment to Pacific peoples. As healthcare
professionals, we must strive to achieve equitable health outcomes for all, particularly Māori and
Pacific Peoples. Patients and whānau place significant trust in the medical profession and also in
those learning to be a doctor. Whenever you meet people, you represent the Medical School, the
University, and the medical profession. Your behaviour both within and outside of the clinical
environment should uphold the reputation of the medical profession that you are joining.1
This Code sets out basic principles that are central to these responsibilities and expectations. It is
important that you are aware of these principles from the beginning of your learning in medicine. It
is important that you familiarise yourself with this Code so that you are aware of what your
responsibilities are, and what is expected of you. These principles form the basis of your
professional development and wil inform the assessment of your professional practice during your
time at medical school. Your University is committed to supporting you in upholding this Code and
encourages you to know where and how to access specialist support services. Any breach of these
standards could undermine patient trust in the medical school and medical profession.
We ask that you read through this Code and sign the form below to acknowledge your commitment
to comply with the principles in it. This form must be signed before you can begin learning to be a
doctor.
Notes:
• These principles apply to all communications and interactions as a learner in medicine, including
electronic communications. Special care is required to ensure patient confidentiality.2 Caution is
necessary when sharing your own personal information and/or that of colleagues on social
networking sites.3
• This code applies in NZ and overseas, and also applies to overseas medical students in NZ.
• This code operates in conjunction with current Acts, Regulations and Codes of Practice that you
wil need to become familiar with during your learning. These include the MCNZ Good Medical
Practice (2016), and all relevant Medical Council Statements, the Code of Health and Disability
- 55 -
Services Consumers’ Rights (1996), the Privacy Act (2020), the Health Information Privacy Code
(2020), the Health Practitioner Competence Assurance Act (2003) and the NZMA Code of Ethics.
A. Interactions with patients and their whānau
1. Respecting patients and their whānau:
As a medical student I wil :
1.1. Treat patients and their whānau respectful y and considerately.
1.2. Establish meaningful connections with patients and their whānau using
whakawhanaungatanga.
1.3. Recognise that cultural safety requires me to reflect on how my own views and biases
impact on clinical interactions and the care I provide to patients.
1.4. Respect the worldviews, values and cultural beliefs of patients and their whānau
members.
1.5. Not impose my own cultural values, beliefs and practices on patients or discriminate
against any person on the basis (for example) of age, sex, gender identity, ethnicity,
sexual orientation, religion, creed, political affiliation, economic, social or health status.
1.6. Respect the dignity, privacy, tikanga and the right of patients to exercise control over
their own body.
1.7. Respect the autonomy of patients.
1.8. Ensure my presentation and attire are appropriate to enable effective and respectful
interaction with patients and whānau.
2. Not exploiting patients:
As a medical student I wil :
2.1. Prioritise patient wellbeing in pursuit of my learning.
2.2. Not exploit any patient, whether physical y, sexual y, emotional y, or financial y. Any
sexual interaction with a patient is unacceptable.
3. Obtaining informed consent for your interaction with patients:
While your clinical supervisor is responsible for obtaining consent for your interaction with patients,
in many circumstances you may still need to ask patients for their permission for their one-on-one
interaction with you. Follow the guidance in the document ‘Medical Students and Informed
Consent’4.
As a medical student I wil :
3.1. Ensure that patients and their substitute decision makers (where applicable) are aware
of my role and the purpose and nature of any proposed interaction with them.
3.2. Acknowledge and accept that patients may refuse or withdraw consent to interact with
me at any stage, without any compromise to their health care.
3.3. Recognise the role of whānau in supporting the patient’s decision making processes.
4. Appreciating the limits of my role:
As a medical student I wil :
4.1. Acknowledge the level of my skil s, experience and knowledge, and not represent myself
as more competent or qualified than I am and correct any such misunderstandings that
arise.
4.2. Not give advice or provide information to patients, whānau or the general public, that is
beyond my level of knowledge and expertise. When asked for such comment, I wil
direct that person to an appropriate professional.
4.3. Not initiate any form of treatment, except under supervision or in an emergency where
no-one more able or qualified is available to provide timely intervention and recognising
the limits of my own knowledge and skil s.
- 56 -
B. Personal and professional expectations
5. Acting honestly, reliably and with integrity
As a medical student I wil :
5.1. Take responsibility for my own actions and inactions.
5.2. Be punctual and notify where this is not possible.
5.3. Meet deadlines, negotiating variations where appropriate.
5.4. Abide by the academic integrity policies of my university and not plagiarise another’s
work or research.
5.5. Be accountable for completing tasks.
5.6. Complete documents accurately and truthful y.
6. Maintaining patient confidentiality:
Patient information is confidential. Disclosure without patients’ permission or other legally
acceptable justification is inconsistent with the trust required in medical practice and has the
potential to cause harm and/or distress. Patient information may be discussed with peers and
professional staff who are directly involved in the care of that patient, and, on occasion with
colleagues, in a setting where confidentiality is protected. As a medical student I wil :
6.1. Hold all patient information in confidence, including after patients have ended
treatment or died.
6.2. Respect patients’ right to determine who should be provided with their personal
information.
6.3. Not remove or copy patient-related material without specific permission, and handle
such material in accordance with 6.4.
6.4. Ensure that all my documents and images containing patient information are de-
identified, kept in a secure place in a way that prevents unauthorised access, and
securely destroyed when no longer required.3
6.5. Be aware of the limited circumstances in which breaches of confidentiality may be
justified or required.
6.6. Not access patient information unless I am involved in their care, or have a legitimate
reason and permission from those authorised to give such permission.
7. Accepting responsibilities to the profession:
Doctors have a responsibility to the profession and to the public to maintain high standards of care;
this wider responsibility is over and above individual responsibility for their own clinical competence.
As a medical student, I wil :
7.1. Report matters of serious concern in a timely and professional manner, including those
which may impact on immediate patient safety, to those with the authority to act.
7.2. Be respectful and careful when using social networking sites or public forums.
7.3. Not exploit my role as a medical student for personal gain.
7.4 Give constructive evaluation and feedback as appropriate on medical education
programmes.
C. Relationships with staff and colleagues
8. Respecting staff and colleagues:
As a medical student I wil :
8.1. Show respect to all members of the health care team and ancil ary staff.
8.2. Show respect to teaching and non-teaching staff.
8.3. Show respect to simulated patients, volunteers and peers.
8.4. Not exploit my peers, or others, particularly those in a vulnerable or more junior
position to myself.
- 57 -
8.5. Hold in confidence information about my peers and staff gathered in learning situations,
but recognise that there are limited circumstances in which breaches of confidentiality
to appropriate persons may be justified.
D. Commitment to continuing improvement in practice, self and others
9. Research and system quality improvement :
As a medical student undertaking or associated with research or system quality improvement
activities I wil :
9.1. Adhere to all the ethical principles in the appropriate national guidelines. Ensure I have
appropriate ethical oversight and any required consultation and ethical processes.
10. Maintaining personal well being:
As a medical student I wil :
10.1. Attend to my own health and wel being.
10.2. Acknowledge that my physical and psychological health impacts on my ability to
function in my role with patients and staff.
10.3. Promptly seek appropriate assistance and notify the Student Affairs Office (Otago), or
Director of Medical Student Affairs (Auckland) in the event that il ness or impairment
interferes with my ability to carry out my role, or my ability to learn,
10.4. Be aware that misuse of substances (including alcohol) impacts on health and fitness to
practise, and may cross the boundaries of legality, which becomes a professional
conduct issue.
10.5. Remain aware of the wellbeing of my colleagues, and support them, to the extent that
I am able, to seek help when needed.
11. Holding a positive attitude to learning:
As a medical student I wil :
11.1. Commit to continued learning and the development of skil s.
11.2. Recognise that my learning needs are valid and important.
11.3. Be prepared to seek and respond to constructive feedback on my own performance.
11.4. Identify barriers that impede my learning and notify my academic supervisor.
11.5. Show respect and observe tikanga in working with human cadavers, human tissue and
animal tissue.5
11.6. Engage in self reflection to enable me to identify my learning needs.
11.7. Actively engage to make the most of educational and clinical opportunities to extend
my knowledge and further my skil s with appropriate support and supervision.
11.8. Care for my peers, provide support in learning opportunities, and work col aboratively
and respectfully in all situations.
11.9. Be prepared, when called upon, to provide constructive feedback to my peers on their
performance.
References
1. Medical Council New Zealand (2020) Unprofessional Behaviour Available from:
www.mcnz.org.nz/assets/standards/e4ddbfd758/Statement-on-unprofessional-behaviour.pdf
2.A Guide to Social Media & Medical Professionalism (2019). Available from:
https://ama.com.au/sites/default/files/documents/2020%20AMA%20Social%20Media%20Guide%2
0FINAL_0.pdf
3. Taking and sharing images of patients policy documents from the relevant University.
4. Bagg, W., et al. (2015) ‘Medical Students and informed consent’ NZMJ Vol 128 No 1414.
5. Code of Conduct issued by the Anatomy Department at the relevant University.
- 58 -
December 2010, Reviewed 2013, 2015, 2020. Date for next review 2025.
I have read the Code. I undertake to comply with it and seek clarification on any areas of uncertainty.
I agree to familiarise myself with any subsequent revisions.
Family name: _____________________________
(BLOCK LETTERS)
Given name: ______________________________
Date: ______________
Student Number____________________
Signature: _________________________________
- 59 -
GRADUATE PROFILE
The attributes of a graduate from the Otago Medical School are set out in the University of Otago
Medical Graduate Profile:
On completion of the University of Otago MB ChB programme, the graduate should be competent to
practise safely and effectively as a first-year doctor (intern) and have an appropriate foundation for
further training in any branch of medicine. Specifical y, the graduate should have the fol owing skil s
and attributes.
Personal Attributes
1. The capacity to be a critical thinker, capable of weighing, evaluating and integrating new
information into his or her understanding of issues
2. The ability to evaluate his or her own professional functioning and to act to remedy
limitations of knowledge, skil s and attitudes throughout his or her career.
3. The ability to extrapolate from knowledge and principles to solve new problems.
4. An awareness of his or her professional limitations, and a wil ingness to seek help when
these limitations are met.
5. The ability and wil ingness to learn and to appreciate that learning continues throughout life.
6. The ability and wil ingness to facilitate the learning experience of individuals, groups and
communities, both within and beyond the health sector.
7. Information literacy, including the ability to locate, evaluate and use information in a range
of contexts.
8. The ability to be organised and the skil s for time management, so that time and resources
are used effectively and efficiently.
9. A dedication to appropriate ethical behaviour, based on a wel -developed awareness of his
or her own moral values, and knowledge and application of principles of medical ethics.
10. An awareness of his or her own needs as a person, how health needs might impact on
competence to practise and an ability to access appropriate support or healthcare for him or
her self.
11. A commitment to the fundamental importance of the interdependence between research,
medical knowledge and professional practice.
12. A commitment to advocate for the health needs of individuals and communities.
Interactive Attributes
1. A caring and empathetic attitude to others.
2. Respect for, and an ability to co-operate with colleagues, competence in teamwork and an
understanding of the roles of other health professionals and healthcare teams.
3. A respect for patients and a dedication to work with patients to optimise their health and
wel being.
4. Respect for, and an ability to respond to the cultural context and aspirations of patients,
colleagues, other health care workers and communities.
5. An understanding of and an ability to respond to the obligations of the Treaty of Waitangi
6. Oral and written communication skil s, including an ability to communicate effectively with
individuals, groups and communities, both within and beyond the health sector.
Disciplinary Attributes
1. A sound knowledge of the philosophical, scientific and ethical principles underlying the
practice of medicine and an ability to apply this knowledge as part of competent medical
practice.
- 60 -
2. A sound understanding of the legal framework surrounding medical practice in New Zealand.
3. A sense of social responsibility and an understanding of the contribution of doctor, health
services, society and political influences to the health outcomes of patients.
4. A commitment to the principles of patient-centred medicine.
5. Knowledge of factors impacting on inequalities in health outcomes.
6. Knowledge of factors impacting on the health status of Maori and other cultures.
7. Skil s in eliciting, documenting and presenting the history of a patient's problems and the
relevant physical examination findings.
8. Skil s in problem solving and formulation of differential diagnoses.
9. Skil s in the management of common medical conditions, including; informing and
negotiating, the performance of relevant clinical procedures, assessment of prognosis,
prescribing skil s, knowledge of drug therapy and care of the dying patient.
10. Skil s in the management of emergencies and other serious medical conditions.
11. An awareness of, and the skil s to manage, uncertainty in medical interpretation and
decision making.
12. An ability to maintain proper boundaries between personal and professional roles.
13. An understanding of the role played by individuals and society in the development of
disease and the maintenance of wel being.
14. A sense of social responsibility and an understanding of the roles and functions of healthcare
institutions in the social and political environment.
15. An appreciation of the global perspective of medicine, and an informed sense of the impact
of the international community on New Zealand and New Zealand's contribution to the
international community.
- 61 -
POLICIES
TRANSFER BETWEEN SCHOOLS OF THE OTAGO MEDICAL SCHOOL
• Once a student is placed in a Campus School of Medicine (DSM, UOC or UOW) the student is
expected to remain at that School until completion of sixth year.
• A student who wishes to transfer to another Campus School of Medicine after being placed
in a School for fourth year, but fourth Year has yet to commence, wil address his/her
request to change Schools directly to the Associate Dean of Student Affairs, Dunedin School
of Medicine. This wil be dealt with as an allocation of school in third year, as opposed to
transfer.
• Transfers wil not normally be considered during, or between, fourth and fifth year, but may
be considered for sixth year. Applications are to be submitted to the Campus School
Associate Deans of Student Affairs/Undergraduate Education by 2 April in the year prior to
transfer.
• The Dean of the Otago Medical School wil only approve transfers if places are available, and
the Deans of the respective Schools support the transfer (principles contained in the MB ChB
regulation Division of Class after Third Year in the University of Otago Calendar wil be
considered).
• Transfers between DSM, UOC and UOW are not necessarily on a one-to-one basis but the
total numbers at each school wil be considered with a view to maintaining the agreed
numbers of places for each school (eg 80 DSM, 110 UOC, 110 UOW).
• Criteria for assessing eligibility and priority for transfer shall be determined by the Deans
and Associate Deans of Student Affairs/Undergraduate Education DSM, UOC and UOW
• Elective quarters in 6th Year cannot be guaranteed for transferring students. The School to
which the student is transferring shall make the final decision on Elective quarters.
TRANSFERS BETWEEN OTAGO AND AUCKLAND MEDICAL SCHOOL
• A student who wishes to transfer to the Medical Programme, University of Auckland, for
sixth year wil apply in writing to the Associate Dean for Student Affairs/Undergraduate
Education at the Campus School of Medicine they are currently attending. The application
is to be received by 2 April in the year prior to transfer, i.e. when a student is in the fifth
year of the medical course.
• Transfers wil only be approved on a one-to-one swap with a student from the Medical
Programme, University of Auckland.
• Students must have an acceptable standard of performance in the course.
• The home institution wil notify current Vulnerable Children Act 2014 compliance and
clearance to the host institution prior to the transfer commencing.
• Students must provide evidence of special reasons for transfer and the Associate Deans for
Student Affairs at Otago and the relevant staff at Auckland shall determine the criteria and
assess applications against these criteria.
• As the Sixth Year Course in Auckland commences in early January of each year, trainee
interns from Otago who transfer to Auckland, wil be required to commence the year in mid-
November with a 4-week elective. Following completion of this in early January, they would
then join the Auckland programme. Elective attachments in Auckland are for a period of 10
weeks and must be undertaken under one institution, and in one specialty at a time
allocated by the University of Auckland Medical Programme.
- 62 -
• The Elective quarter cannot be guaranteed for Otago students transferring to Auckland.
The Auckland Programme staff shall make the final decision on Elective quarters. Auckland
students transferring to Otago wil be allocated 4th Quarter Electives. This enables the
Auckland student to complete the programme and meet the earlier graduation deadlines for
the Auckland programme.
• Auckland students transferring to Otago wil undertake the ful Otago sixth year programme,
i.e. from November to November.
• Otago students at Auckland are not enrol ed students so wil have academic visitor status ID
cards, which may potentially restrict access to some student facilities, services and academic
prizes as wel as public transport discounts. They may use the library but if borrowing is
needed, it wil be provided by their home institution.
Note:
Deans of Dunedin, Christchurch, Wel ington and the University of Auckland delegate to their
Associate Deans of Student Affairs/Undergraduate Education (ADSA) and relevant staff at Auckland
the authority to recommend transfers out of and into their School. All transfers are monitored by the
ADSA (Dunedin) on behalf of the Otago Medical School to ensure applicants from all Schools have
equal opportunity to transfer.
- 63 -
ACADEMIC GUIDELINES
INTEGRITY AND ACADEMIC MISCONDUCT
Academic integrity means being honest in your studying and assessments. It is the basis for ethical
decision-making and behaviour in an academic context. Academic integrity is informed by the values
of honesty, trust, responsibility, fairness, respect and courage. Students are expected to be aware
of, and act in accordance with, the University’s Academic Integrity Policy.
Academic Misconduct, such as plagiarism or cheating, is a breach of Academic Integrity and is taken
very seriously by the University. Types of misconduct include plagiarism, copying, unauthorised
collaboration, taking unauthorised material into a test or exam, impersonation, and assisting
someone else’s misconduct. A more extensive list of the types of academic misconduct and
associated processes and penalties is available in the University’s Student Academic Misconduct
Procedures.
It is your responsibility to be aware of and use acceptable academic practices when completing your
assessments. To access the information in the Academic Integrity Policy and learn more, please visit
the University’s Academic Integrity website at www.otago.ac.nz/study/academicintegrity or ask at
the Student Learning Centre or Library. If you have any questions, ask your lecturer.
Academic Integrity Policy
(www.otago.ac.nz/administration/policies/otago116838.html)
Student Academic Misconduct Procedures
(http://www.otago.ac.nz/administration/policies/otago116850.html)
GOOD ACADEMIC PRACTICE
Information concerning acknowledgement and referencing of academic material is available on
Moodle
CODE OF PRACTICE FOR FITNESS TO PRACTISE
Medical students are part of the medical profession. Whilst students do not yet enjoy the privileges
accorded to qualified practitioners and are not yet bound by the ful professional constraints
imposed upon practising doctors, it is vital that issues that may affect their current or future fitness
to practise are fairly and transparently addressed by the Otago Medical School and its Schools.
The Code of Practice for Fitness to Practise outlines the policy and mechanisms of the University of
Otago OMS to assess and act on issues fairly and equitably concerning a student’s Fitness to
Practise.
It is expected that, at graduation, our students wil meet the expectations of the University of Otago
Medical Graduate Profile, through their personal attributes, teaching and learning during the course,
and support from staff.
Throughout the undergraduate programme, the assessment processes wil include steps to identify
and monitor any students who might not meet the graduate profile standards through problems
with health, or with professional attitudes and behaviour both within and outside the teaching
environment. In the normal course of events, the assessment wil be conducted by the relevant
Student Progress Committee (SPC). But in cases of particular concern, referral is made to the Fitness
to Practice Committee (FtPC). The Committee provides support, remediation and monitoring of
- 64 -
potential or actual Fitness to Practise needs of students who do not meet graduate profile
standards. The FtPC has the power to recommend the granting or withholding of terms where
ongoing issues are unresolved.
If there is any issue relating to this statement that you feel may be important to your circumstances
now, or which arises during your time in medical school, please make contact with the Otago
Medical School's Associate Dean for Student Affairs through the Student Affairs Office.
POLICY ON TRANSMISSIBLE AND BLOOD-BORNE INFECTIONS FOR MEDICAL STUDENTS
It is a condition of entry to the Otago Medical School MB ChB course, that students accept and
adhere to the Policy on Transmissible and Blood-borne Infections for Medical Students and the
associated fitness to practice policy. The policies are based on guidelines produced by the Medical
Council of New Zealand (MCNZ). All prospective medical students are required to undergo testing
for serological status for HIV, hepatitis B (HBsAg and HBsAb), for antibodies induced by hepatitis C,
measles, mumps and rubel a prior to application for entry into second year medicine. Varicella
testing is required if the student has no history of clinical chickenpox or uncertainty exists over a
history for this infection.
All prospective medical students wil be required to provide a report from their general practitioner
stating the results of the tests and provide attached copies of the lab results.
All prospective medical students who are not immune on initial testing and not infected, should be
vaccinated against hepatitis B, measles, mumps, rubel a and varicella, and should be retested to
confirm immunity fol owing vaccination. Testing and vaccination wil occur in year 1, before the
student enters Medical School. All Students in their 2nd year are required to have a Two Stage
Mantoux test to screen for exposure to or infection with tuberculosis. The process involves two
tuberculin injections and readings over a period of 2 weeks. Any student who has a positive test wil
be required to have a chest x-ray to determine whether evidence of tuberculosis is present and be
referred to a specialist Chest Physician if required.
Medical students found to have hepatitis B (HBV) infection wil be required to have a test to
determine whether HBV DNA is present at a high concentration in their blood. Medical students
who are HBV positive may have some limitations imposed upon their clinical training to minimise
risk to patients. The Associate Dean of Student Affairs wil meet with the student and discuss any
required actions and limitations.
Chronic infection with hepatitis B, hepatitis C or HIV alone do not at present justify refusing a
student access to study as a medical student in New Zealand, but some limitation of future
professional work activities may exist, notably in surgery. It is important that affected students
recognise that these infections may adversely affect clinical medical career opportunities both in
New Zealand and overseas.
Medical students who know or believe themselves to be infected with hepatitis B, hepatitis C or HIV,
or who may be at risk from these infections due to behaviour that has a risk for transmitting blood-
borne viruses, could put patients at risk and so must seek appropriate counsel through the Associate
Dean (Student Affairs) and act upon that advice. This advice could include a requirement to limit
practice in certain ways. No medical student with such infection wil be allowed to continue in
clinical training based on his/her own personal assessment of their risk status. It is regarded by the
MCNZ as unethical, and could be deemed professional misconduct, for a doctor so infected to act in
a way that puts a patient at risk, as assessed by peer review. Non-compliance with this policy may
result in the student having to leave the programme.
- 65 -