2021
First Edition. Date: 31 January 2021
Additional information to come relating to Assessment. (See also 2021 MB ChB Assessment Policies and
Procedures Guide.)
Disclaimer
While all responsible efforts have been made to ensure that the information contained in this publication is
correct at the time of printing, matters covered in this publication are subject to change.
The University reserves the right to change courses and course requirement at any time.
31 January 2021
2
Introduction
This document is a guide for students (and staff) in years 4 and 5 of the Advanced Learning in Medicine (ALM)
programme at Otago Medical School – Dunedin Campus (OMS-DC).
Fourth years: Welcome to the challenge of moving into a new environment. Where the focus in ELM was on
you as students, the ALM programme is based in the clinical environment, in which the primary focus in on
patients and their care.
Now that you are working within and alongside health care teams, your understanding of your professional
role can be put into practice. Be aware of expectations, which are there to protect you as well as others.
Continue to work collaboratively, and ask for help when you need it.
Fifth years: Your challenge is to apply, consolidate, and continue to build on what you have learned to date.
Throughout ALM, you will have many opportunities to learn from your patients, from each other, and from
the workplace. We encourage you to take these opportunities, even when they are unexpected, and to enjoy
how they help you develop towards becoming a doctor. The University of Otago, Otago Medical School and
your campus all want to see you succeed. We look forward to working with you in the future as Trainee Interns,
and colleagues.
This Handbook
Within this Handbook you will find information about all aspects of the ALM 4 and 5 programme including, but
not limited to:
Key dates for the coming year
Contact details for academic and administrative staff
Important policies relating to your conduct as a clinical medical student, including Southern DHB
expectations about your behaviour while you are learning in their facilities
Overview information relating to the learning framework and constituent parts of the programme
Assessment polices and procedures
Information about research opportunities available to you
Preliminary information about the Trainee Intern year
All the information contained herein is also available on Moodle, where you will also find additional details
that expand on the material included in this document.
This is a living document and as such we expect some content to evolve over the year. Updated information
will be made available as necessary, and will be appropriately signposted as such.
3
link to page 8 link to page 9 link to page 10 link to page 11 link to page 12 link to page 13 link to page 14 link to page 15 link to page 16 link to page 16 link to page 16 link to page 16 link to page 17 link to page 17 link to page 17 link to page 17 link to page 17 link to page 18 link to page 18 link to page 18 link to page 18 link to page 19 link to page 19 link to page 19 link to page 20 link to page 21 link to page 21 link to page 21 link to page 23 link to page 23 link to page 24 link to page 25 link to page 26 link to page 26 link to page 27 link to page 28 link to page 28
Table of Contents
Welcome from the Dean _________________________________________________________________ 8
Welcome from OUMSA President __________________________________________________________ 9
OMS Dunedin Dean’s Department and Administrative Staff for 2021 ____________________________ 10
ALM 4 Block Module Convenors and Administrators __________________________________________ 11
ALM 5 Block Module Convenors and Administrators __________________________________________ 12
Vertical Module Convenors and Administrators ______________________________________________ 13
4th Year Undergraduate Medical Course dates 2021 _________________________________________ 14
5th Year Undergraduate Medical Course dates 2021 _________________________________________ 15
General Information ___________________________________________________________________ 16
General Notes _________________________________________________________________________ 16
Notices/updates ________________________________________________________________________ 16
Communication: Checking your student email ________________________________________________ 16
Communication: Cellphones, iPads or Laptops _______________________________________________ 17
Communication: Social medial and the medical profession _____________________________________ 17
Recording of patient interview and clinical presentations ________________________________ 17
Guide to academic conduct _______________________________________________________________ 17
University and Hospital Identification ____________________________________________________ 17
Attendance and Leave __________________________________________________________________ 18
Application for Leave ____________________________________________________________________ 18
Consideration of Leave Application ________________________________________________________ 18
Sick Leave, Bereavement Leave or other Emergency ___________________________________________ 18
Dealing with Missed Sessions _____________________________________________________________ 19
Public Holidays _________________________________________________________________________ 19
Attendance at clinical rounds while unwell __________________________________________________ 19
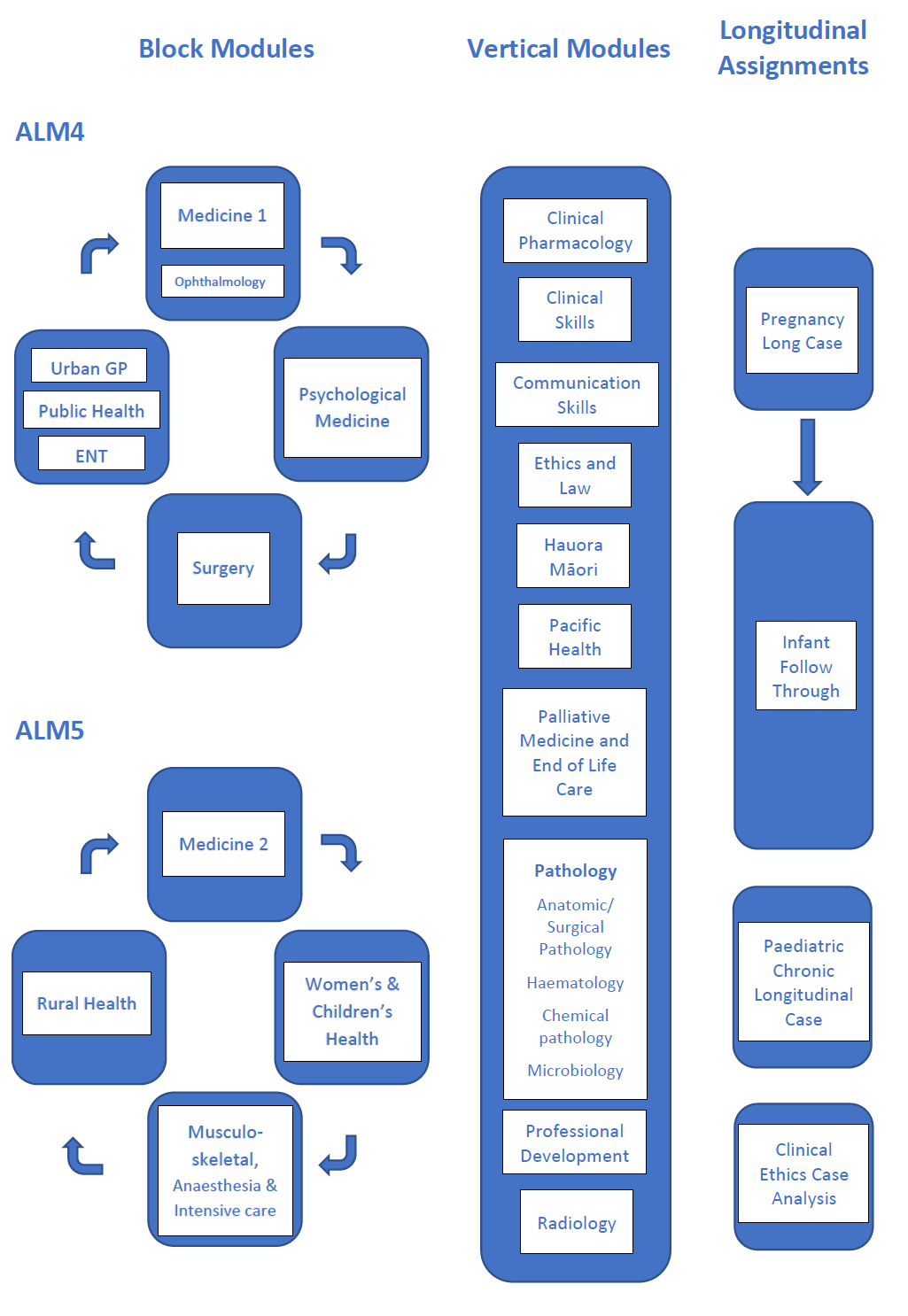
Overview of the ALM programme at Dunedin Campus ________________________________________ 20
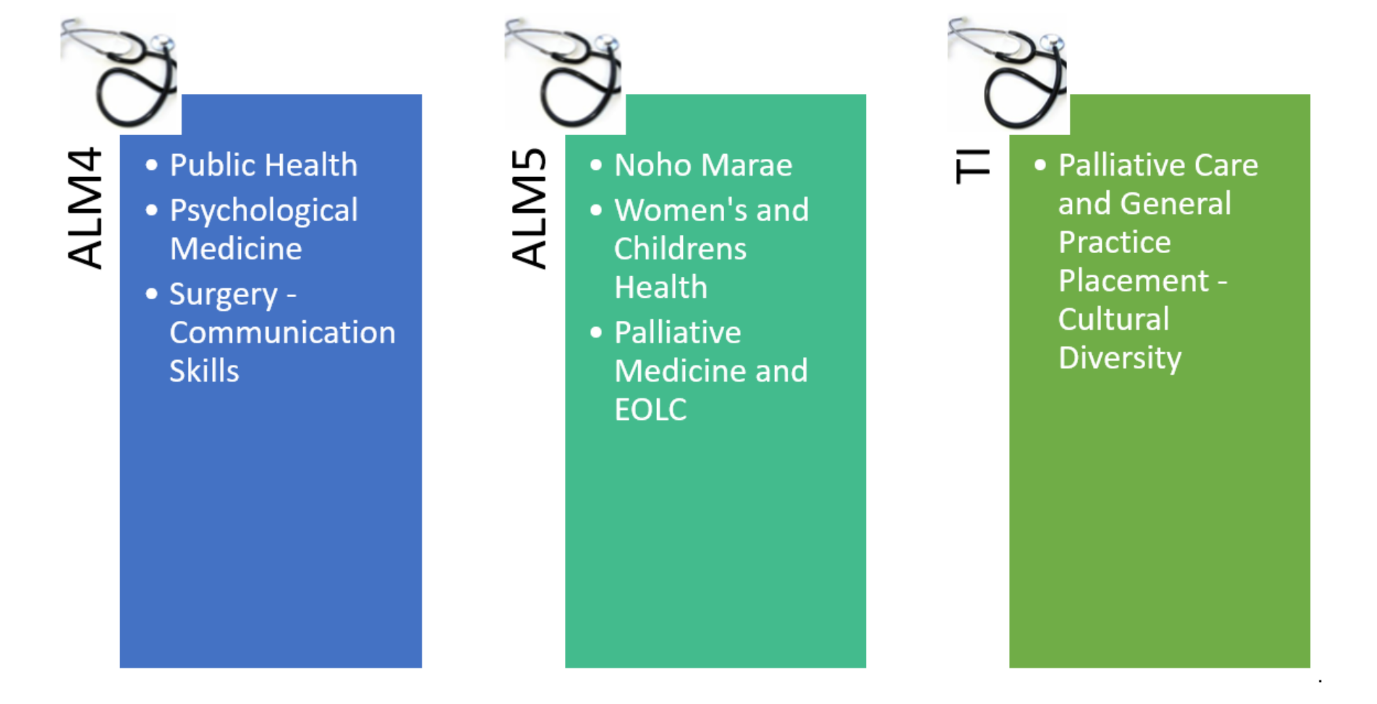
Overview of ALM 4 Block Modules ________________________________________________________ 21
Medicine 1 (including Ophthalmology) ______________________________________________________ 21
Psychological Medicine __________________________________________________________________ 21
Surgery _______________________________________________________________________________ 23
Urban General Practice Module ___________________________________________________________ 23
Public Health Module ___________________________________________________________________ 24
ENT/ Otorhinolaryngology, Head and Neck Surgery (ORLHNS) Module ____________________________ 25
ALM4 Longitudinal Assignments __________________________________________________________ 26
Pregnancy Long Case (PLC) _______________________________________________________________ 26
Infant Follow-Through Long Case __________________________________________________________ 27
Overview of ALM5 Block Modules _________________________________________________________ 28
Medicine 2 ____________________________________________________________________________ 28
4
link to page 28 link to page 29 link to page 30 link to page 31 link to page 31 link to page 31 link to page 32 link to page 32 link to page 32 link to page 33 link to page 33 link to page 34 link to page 36 link to page 36 link to page 37 link to page 37 link to page 38 link to page 39 link to page 40 link to page 40 link to page 41 link to page 41 link to page 41 link to page 41 link to page 42 link to page 42 link to page 42 link to page 42 link to page 43 link to page 43 link to page 44 link to page 44 link to page 44 link to page 44 link to page 44 link to page 44 link to page 46 link to page 46 link to page 46
Child Health and Reproductive Medicine Module (WCH) _______________________________________ 28
Musculoskeletal, Anaesthesia and Intensive Care _____________________________________________ 29
Rural Health Module ____________________________________________________________________ 30
ALM5 Longitudinal Assignments __________________________________________________________ 31
Paediatric Chronic Longitudinal Case _______________________________________________________ 31
Clinical Ethics Case Analysis _______________________________________________________________ 31
Overview of Vertical Modules ____________________________________________________________ 32
Clinical Pharmacology ___________________________________________________________________ 32
Clinical Skills ___________________________________________________________________________ 32
Communication Skills ____________________________________________________________________ 33
Ethics and Law _________________________________________________________________________ 33
Hauora Māori __________________________________________________________________________ 34
Pacific Health __________________________________________________________________________ 36
Palliative Medicine and End-Of-Life Care ____________________________________________________ 36
Pathology _____________________________________________________________________________ 37
Professional Development________________________________________________________________ 37
Radiology _____________________________________________________________________________ 38
Rural Medicine Immersion Programme (RMIP) for ALM5 ______________________________________ 39
Options for TI Year ___________________________________________________________________ 40
TI Year Elective ______________________________________________________________________ 40
Research Opportunities _______________________________________________________________ 41
Summer Studentships _________________________________________________________________ 41
Bachelor of Medical Science with Honours (BMedSci(Hons)) ____________________________________ 41
Intercalated MB ChB/PhD ______________________________________________________________ 41
Student welfare and services_____________________________________________________________ 42
Student Affairs _________________________________________________________________________ 42
Medical Education Unit __________________________________________________________________ 42
Reporting Concerns: ___________________________________________________________________ 42
Otago University Medical Students’ Association Inc (OUMSA) ___________________________________ 43
The New Zealand Medical Association (NZMA) _______________________________________________ 43
Class representatives ____________________________________________________________________ 44
Students with impairments _______________________________________________________________ 44
International student support _____________________________________________________________ 44
Māori Centre – Te Huka Mātauraka ________________________________________________________ 44
Pacific Island Research & Student Support Unit _______________________________________________ 44
Student Health Services __________________________________________________________________ 44
Working in a Clinical Setting _____________________________________________________________ 46
Chaperoning ___________________________________________________________________________ 46
Dress and appearance ___________________________________________________________________ 46
5
link to page 47 link to page 47 link to page 47 link to page 47 link to page 48 link to page 49 link to page 49 link to page 50 link to page 50 link to page 51 link to page 52 link to page 52 link to page 52 link to page 52 link to page 53 link to page 55 link to page 55 link to page 55 link to page 55 link to page 55 link to page 56 link to page 56 link to page 56 link to page 56 link to page 56 link to page 56 link to page 57 link to page 57 link to page 57 link to page 58 link to page 58 link to page 58 link to page 59 link to page 59 link to page 59 link to page 59 link to page 59 link to page 60 link to page 60 link to page 60
Culturally-sensitive issues ________________________________________________________________ 47
Dress requirements in theatre ____________________________________________________________ 47
Professional behaviour: General ___________________________________________________________ 47
Professional etiquette and practical ethics for clinical education (teaching, learning & assessment) _____ 47
Clinical examination of patients ___________________________________________________________ 48
Professional behaviour: Supervision ________________________________________________________ 49
Medical student rights ___________________________________________________________________ 49
Privacy and Confidentiality _______________________________________________________________ 50
Access to notes and handling of written material _____________________________________________ 50
Release of Information __________________________________________________________________ 51
School Buildings and Facilities ____________________________________________________________ 52
Fraser Building _________________________________________________________________________ 52
Otago Clinical Skills Lab (OCSL) ____________________________________________________________ 52
General computing information ___________________________________________________________ 52
Health Science Library ___________________________________________________________________ 53
Southland Hospital Invercargill ___________________________________________________________ 55
Arrival ________________________________________________________________________________ 55
Travel arrangements ____________________________________________________________________ 55
Orientation ____________________________________________________________________________ 55
Contact details: ________________________________________________________________________ 55
Associate Dean (Southland) _______________________________________________________________ 56
MRSA clearance ________________________________________________________________________ 56
ID / access cards ________________________________________________________________________ 56
Photocopier and Southern District Health Board computer use __________________________________ 56
Car parking ____________________________________________________________________________ 56
Library ________________________________________________________________________________ 56
Dunedin Campus Computer Facility in Invercargill_______________________________________ 57
Computer help in Invercargill _____________________________________________________________ 57
Doctors' Residence______________________________________________________________________ 57
Videoconferencing Room ______________________________________________________________ 58
Zoom room ___________________________________________________________________________ 58
Contacts _____________________________________________________________________________ 58
Complaints and/or concerns ______________________________________________________________ 59
Timaru Hospital _______________________________________________________________________ 59
Associate Dean (South Canterbury) and Administrator _________________________________________ 59
OTAGOHub ____________________________________________________________________________ 59
Student Accommodation: 13A, B, C & D Queen Street, Timaru __________________________________ 59
The West Coast _______________________________________________________________________ 60
What is the region like? __________________________________________________________________ 60
Te Nikau, Grey Hospital and Health Centre __________________________________________________ 60
6
link to page 60 link to page 60 link to page 61 link to page 61 link to page 61 link to page 62 link to page 63 link to page 73 link to page 74 link to page 74 link to page 74 link to page 74 link to page 74 link to page 74 link to page 74 link to page 75 link to page 75 link to page 75 link to page 75 link to page 75 link to page 75 link to page 75 link to page 76 link to page 76 link to page 76 link to page 76 link to page 76 link to page 77 link to page 77 link to page 77 link to page 77 link to page 77 link to page 77 link to page 77 link to page 78
Prior to travel to the West Coast ___________________________________________________________ 60
Transport to the West Coast ______________________________________________________________ 60
Accommodation ________________________________________________________________________ 61
Clinical Placements _____________________________________________________________________ 61
Contact Details _________________________________________________________________________ 61
Facilities ______________________________________________________________________________ 62
SDHB Code of Conduct and Integrity (District) _______________________________________________ 63
Key policies and regulations related to the MB ChB __________________________________________ 73
University of Otago Medical School Prizes and Dunedin Campus Prizes and Awards ________________ 74
Otago Medical School ___________________________________________________________________ 74
Batchelor Memorial Medal and Prize in Gynaecology and Obstetrics ___________________________ 74
Stanley Batchelor Memorial Prize in Surgery _______________________________________________ 74
Colquhoun Memorial Medal in Clinical Medicine _____________________________________________ 74
The Rita Gardner Travelling Scholarship in Medicine _________________________________________ 74
T W J Johnson Memorial Prize in Clinical Medicine _____________________________________________ 74
Emily Hancock Siedeberg Memorial for the Best Overall Woman Student _______________________ 75
Psychological Medicine Prize ______________________________________________________________ 75
J M Watt Prize in Paediatrics and Child Health _______________________________________________ 75
Dunedin Campus _______________________________________________________________________ 75
Marjorie McCallum Medal in Medicine ____________________________________________________ 75
James Renfrew White Prize in Orthopaedic Surgery ________________________________________ 75
Patricia Buckfield Prize in Paediatrics _____________________________________________________ 75
Sir Gordon Bell Prize in Surgery ____________________________________________________________ 76
Paediatric Artistic Expression _____________________________________________________________ 76
Mary Shaw Surgical Prize _________________________________________________________________ 76
Stanley Wilson Prize ______________________________________________________________________ 76
Sir Bernard Dawson Prize in Clinical Obstetrics and Gynaecology _______________________________ 76
Professor Basil James Prize in Psychological Medicine ________________________________________ 77
RNZCGP Otago/JAD Iverach Prize in General Practice __________________________________________ 77
JAD Iverach Prize in Medicine _____________________________________________________________ 77
Inkster-Ross Memorial Prize _______________________________________________________________ 77
Elective Report Award ____________________________________________________________________ 77
University Bookshop Prize for Best Student Contribution to Medical Education _______________ 77
John Russell Ritchie Prize (to be confirmed if available in 2021) ________________________________ 77
Kōhatu – Centre for Hauora Māori Excellence Awards ________________________________________ 78
7
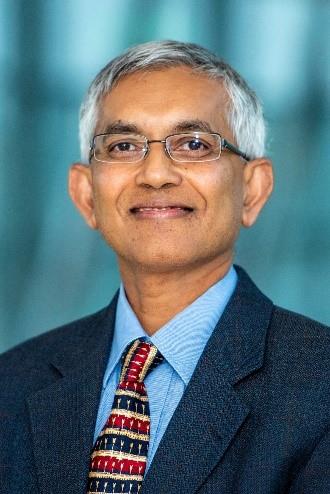
Welcome from the Dean
Warm welcome (or if you are a 5th year, welcome back) to the Advanced Learning
in Medicine programme at the Otago Medical School – Dunedin campus.
You made the right choice and we are delighted to have you at the Otago Medical
School – Dunedin campus.
We hope you had a refreshing break and that you are looking forward to an exciting
and fulfilling year learning how to be a great doctor. During your time here you will
begin to make the patterns of medical life that will continue rest of your career –
you will see examples of variety of professional practices from our committed and
outstanding academic and clinical staff. Many will be inspiring and leaders in their
respective field. We pride ourselves on high standards of care and teaching and will
try and offer you excellent opportunities for learning. Please talk to staff about your
experience as we are always learning and want to improve and provide you the best
learning environment in New Zealand. I would be delighted to talk to any of you that want to bring significant
issues to me directly or through the student committee.
An important partner for us in offering the right environment for learning is the Southern DHB. Their staff also
recognise the value of having students within our services. As students, you need to respect and add value to
this relationship, remembering that your influence will affect many other students behind you. Key to all that
we do is a respectful and empathic attitude to all patients – maintain that under all circumstances, even when
you are stressed.
One issue to note is the DHB policy on taking photos of patients on personal cell phones. This is not allowed
by either DHB staff or by you as students at the OMS-Dunedin campus. Bear this in mind, and if you need a
clinical image, ask a DHB or staff member about how to go about doing this (requires full written informed
consent, a record in the clinical notes and for the photo to be taken using a dedicated camera for this purpose,
and stored in the clinical record).
Finally, there is abundant research opportunities in each area of clinical medicine. OMS-Dunedin campus
actively encourages you to get involved in clinical research to develop a clinician-scientist career. Care of
individuals or groups with health problems is wonderfully rewarding, often day to day, but there is even
greater long-term satisfaction possible if you find out what works best by conducting research. Research and
clinical practice contributes to each other and elevate both disciplines. If you are interested in immersing
yourself in medical research, BMedSci(Honours) or an intercalated MBChB/PhD degree pathway will set you
far ahead in a rewarding academic clinician career in Medicine.
We hope that your year will be exciting, rewarding and successful and we very much looking forward to
teaching and mentoring each and every one of you.
Kind Regards
Professor Rathan M. Subramaniam
MBBS, BMedSci, PhD, MPH, MClinEd, FRANZCR, FACNM, FSNMMI, FAUR
Dean, University of Otago Medical School
8
Welcome from OUMSA President
Kia ora!
Welcome to your ALM years of medical school! Over the next two years you will be getting your first look at
the inner workings of the hospital system. There will be daily hands-on learning with real patients which can
be a daunting concept, but you will soon find your groove and we at OUMSA hope to make this transition
smoother for you. It can be challenging being a student in an environment that is primarily a workplace and a
place of care, and we all want your learning experience to be the best that it can be.
The Otago University Medical Students’ Association (OUMSA) changes slightly during the ALM years from what
you would have experienced previously during medical school. One of the main differences is that we now
have a much smaller cohort, and so who makes up our team has changed. On our executive committee we
have the President & Vice-President coordinating all the activities. We then have 3 officers – Education,
Welfare and Social who coordinate any portfolios that fall into these categories and who work with your
appointed representatives. The representatives are voted for by your class – we have a 4th year education rep,
welfare rep & social rep (as well as representatives for the other 2 year groups.) Combined, these 14 people
make up your OUMSA executive. We continue to work with the ELM OUMSA executive throughout the year.
Our goal for you during your 4th and 5th years of medical school is to ensure that your education is being
supported, you make some quality memories with you peers, and your mental health is cared for throughout.
We also like to support other community groups around Dunedin.
So what does this look like for you? We run tutorials to support you through your 5th year exams. We organise
the Wine & Cheese, full year dinners, sports opportunities, tramps, ski trip, wellness activities, and when you
get through the ALM years we make sure graduation is a big celebration. And this is just what we have planned
so far!
Keen to get involved? We are always wanting new people and ideas on our OUMSA exec. Look out for
information about elections to get involved, or contact your officers/year reps to ask how you can contribute.
Congratulations on making it to this point! The clinical years are what we came here for so remember to make
the most of them!
Ngā mihi,
Maddy Hutton
OUMSA President 2021
9
OMS Dunedin Dean’s Department and Administrative Staff for 2021
Position
Name
Dean of Otago Medical School
Professor Rathan Subramaniam
[email address]
Dunedin Campus
Associate Dean Medical Education
Assoc Prof Ralph Pinnock
[email address]
e-Learning Facilitator
Dr Steve Gallagher
[email address]
Education Advisor (ALM)
Dr Megan Anakin
[email address]
Medical Education Unit Administrator
Angela King
[email address]
Associate Dean for Student Affairs (ALM)
Dr Penny Eames
[email address]
Student Affairs Manager
Jillian Tourelle
[email address]
Student Affairs Reception/Admin
Erin Flannery
[email address]
Invercargill Campus (Southland Hospital)
Associate Dean, Southland
Mr K Richter
[email address]
Administrator
Madge Storm
[email address]
Timaru Hospital
Associate Dean, South Canterbury
Ms M Steel
[email address]
Administrator
Jehan Cunningham-Beynon
[email address]
10
ALM 4 Block Module Convenors and Administrators
Surgery
Mr Andrew Audeau (Convenor)
[email address]
Ruth Mullenger (Administrator)
[email address]
Medicine (including Ophthalmology)
Dr Steve Johnson (Co-Convenor)
[email address]
Ms Lis Heath (Co-Convenor)
[email address]
Dr Keluchi Ogbuehi (Ophthalmology Convenor)
[email address]
Anne Ryalls (Teaching Administrator)
[email address]
Urban General Practice and ENT
Dr Kristin Kenrick (Convenor)
[email address]
A/Prof Patrick Dawes (ENT Convenor)
[email address]
Liz Dijkstra (Administrator)
[email address]
Public Health
Dr Sarah Donald (Convenor)
[email address]
Kelsey Den Boestert (Administrator)
[email address]
Psychological Medicine
Dr Yoram Barak (Convenor)
[email address]
Anita Admiraal (Co-ordinator)
[email address]
Sandra Paterson (Administrator)
[email address]
Pregnancy long case
Dr Kate Coffey (Co-Convenor)
[email address]
Ms Sally McNeill (Midwife)
Mel O’Brien (Administrator)
[email address].nz
Infant Follow-Through
Dr Jason Wister (Co-Convenor)
[email address]
11
ALM 5 Block Module Convenors and Administrators
Women’s and Children’s Health
A/Prof Mike Stitely (Co-Convenor, O & G)
[email address]
Dr Liza Edmonds (Co-Convenor, Paeds)
[email address]
Iloma Mollison (Administrator)
[email address]
Rural Health
Dr Peter Radue (Convenor)
[email address]
Liz Dijkstra (Administrator)
[email address]
Musculoskeletal, Anaesthesia and Intensive Care
Prof David Gwynne-Jones (Convenor)
[email address]
Aroha Meikle (Administrator)
[email address]
Medicine II
Assoc Prof Gerry Wilkins (Overall Module Convenor, and Cardiology Attachment Convenor)
[email address]
Dr Jack Dummer (Respiratory Medicine Attachment Convenor)
[email address]
Anne Ryalls (Administrator)
[email address]
12
Vertical Module Convenors and Administrators
Clinical Pharmacology
Associate Professor David Reith
[email address]
Clinical Skills (including Communication Skills)
Dr Peter Radue (Convenor, Clinical Skills)
[email address]
Dr Ohad Dar (Convenor, Simulation)
[email address]
Dr Jane Millichamp (Communication Skills)
[email address]
Angela King (Administrator)
[email address]
Ethics and Law
A/Prof Neil Pickering (Co-Convenor)
[email address]
Dr Simon Walker (Co-Convenor)
[email address]
Hauora Māori
Prof Jo Baxter (Convenor)
[email address]
Tūī Kent (Administrator)
[email address]
Pacific Health
Dr Tava Tafuna'I (Convenor)
[email address]
Sina Mualia (Administrator)
[email address]
Palliative Medicine and End of Life Care
Ms Lis Health (Convenor)
[email address]
Pathology (including Microbiology)
Prof Ian Morison (Convenor)
[email address]
Professional Development
Dr Nigel Thompson
[email address]
Angela King (Administrator)
[email address]
Radiology
Professor Terry Doyle (Convenor)
[email address]
Whole Class Learning
Dr Kristin Kenrick (Convenor)
[email address]
Angela King (Administrator)
[email address]
13
4th Year Undergraduate Medical Course dates 2021
1st Semester
Monday 1 February to Friday 11 June
Whole Class Learning Week 1
Monday 1 February to Friday 5 February
Waitangi Day [observance]
Monday 8 February
Semester Commences
Tuesday 9 February to Thursday 1 April
Mid-Semester break
Friday 2 April to Sunday 11 April [1 week]
[includes Easter and Otago Anniversary Day]
Semester resumes
Monday 12 April to Friday 23 April
Whole Class Learning Week 2
Monday 12 April to Friday 16 April
ANZAC Day [observance]
Monday 26 April
Semester resumes
Tuesday 27 April to Friday 4 June
Queen’s Birthday
Monday 7 June
Semester resumes
Tuesday 8 June to Friday 11 June
June Vacation
Saturday 12 June to Sunday 27 June [2 weeks]
2nd Semester
Monday 28 June to Friday 29 October
Semester commences
Monday 28 June to Friday 20 August
Mid-Semester break
Saturday 21 August to Sunday 29 August [1 week]
Whole Class Learning Week 3
Monday 30 August to Friday 3 September
Semester resumes
Monday 30 August to Friday 22 October
Labour Day
Monday 25 October
Semester resumes
Tuesday 26 October to Friday 29 October
14
5th Year Undergraduate Medical Course dates 2021
1st Semester
Tuesday 9 February to Friday 11 June
Whole Class Learning Week 1
Tuesday 9 February to Friday 12 February
Semester Commences
Monday 15 February to Thursday 1 April
Mid-Semester break
Friday 2 April to Sunday 11 April [1 week]
[includes Easter and Otago Anniversary Day]
Semester resumes
Monday 12 April to Friday 23 April
Whole Class Learning Week 2
Monday 12 April to Friday 16 April
ANZAC Day [observance]
Monday 26 April
Semester resumes
Monday 27 April to Friday 4 June
Queen’s Birthday
Monday 7 June
Whole Class Learning Week 3
Tuesday 8 June to Friday 11 June
June Vacation
Saturday 12 June to Sunday 27 June [2 weeks]
2nd Semester
Monday 28 June to Friday 5 November
Whole Class Learning Week 4
Monday 28 June to Friday 2 July
Semester commences
Monday 5 July to Friday 20 August
Mid-Semester break
Saturday 21 August to Sunday 29 August [1 week]
Semester resumes
Monday 30 August to Friday 15 October
Whole Class Learning Week 5
Monday 18 October to Friday 22 October
Labour Day
Monday 25 October
Study Week
Tuesday 26 October to Friday 29 October
OSCE
Saturday 30 October
Written Exams
Monday 1 November to Friday 5 November
15
General Information
General Notes
Years 4 and 5 have been designed to help you apply your knowledge to practical situations and to help you
develop from a student to an apprentice doctor. During the year you will complete block and vertical modules.
Block Moduless are generally attachments to a particular clinical setting for a period of weeks. Vertical
Modules provide a more longitudinal focus on a particular area of learning over the year.
Each module has its own set of Learning Objectives and Assessments. Details about these can be found on the
relevant Moodle page.
The best way to get the most out of your year is to take as many opportunities as you can to meet patients, to
find out about their problems and then to synthesise this with your theoretical knowledge. We encourage you
to read about the conditions that your patients have. This is a great way to help your theoretical knowledge
“stick” in your mind.
You will never know everything, so learning to identify important gaps and working out ways to fill them are
important lifelong skills. Don’t expect therefore to be taught everything. Rather, by seeing the common and
important conditions in your patients we hope you will be stimulated to identify and prioritise your own
learning.
The educational philosophies in the ALM course should articulate effectively with those of the ELM course.
Teaching and learning should:
Take place in hospital, ambulatory care, and community settings
Maximise exposure to patients and to team working with other health professionals by incorporating
the student into the healthcare team
Encourage self-directed learning driven by history and findings of patients
Explicitly describe the objectives and learning outcomes.
Ensure that concepts are understood as well as facts
Incorporate vertical modules throughout ALM-4 attachments in a way which complements the clinical
content.
Allow progressive acquisition of clinical skills with frequent observed formative assessment
Ensure on-going development of professional attitudes and behaviour
The curriculum map indicates to students and staff the key elements of learning within the MB ChB
programme, demonstrating how they are organised, structured and related/linked to each other. It links these
elements to opportunities in the curriculum where students are likely to encounter them and to resources to
help them learn. As such it provides the best overview of the curriculum and how the various parts are related
to each other.
Notices/updates
All timetable updates, handbooks, term dates, forms, policies etc will be available on Moodle. Please check
this on a daily basis for all regular updates.
Communication: Checking your student email
It is important to check and clear your student email on a regular basis. Any correspondence from the Medical
School will be via Moodle or your student email. If you have any problems please contact ASK-IT.
16
Communication: Cellphones, iPads or Laptops
Use cellphones, iPads or laptops in a considerate manner: receiving calls, texting, tweeting and/or updating
your FB status during tutorials is not acceptable behaviour.
Communication: Social medial and the medical profession
The Internet immediately connects us with the public domain and we must continue to avoid making
comments or posting material that could be interpreted as breeching the boundaries of patient-doctor
confidentiality.
While blogging, tweeting, and other social networking avenues are, for the most part, well intentioned, there
is the potential for these activities to have future adverse consequences. As members of a professional
community with high ethical standards, any comments, images and material you may leave on a personal page
could embarrass you when seeking future employment. Any photos of patients, aspects of patient care,
procedures, etc, must not be placed on social media. This includes material that you might gather while you
are on elective overseas. The 'rule of thumb' in this situation is to behave exactly as you would in New Zealand.
The standards that you will be held to account over, are the same.
Recording of patient interview and clinical presentations
Recording of patient interview or clinical demonstrations by students is not permitted under any
circumstances. Patients have not been asked for permission and it is inappropriate for students or others to
request permission at the time of the demonstration. Please ensure that you respect the confidentiality
implicit in all clinical demonstrations.
Guide to academic conduct
https://www.otago.ac.nz/study/academicintegrity/index.html
Over the course of your studies you will be required to submit a wide variety of work in a range of styles and
formats. The purpose of this guide is to introduce you to good practice and help you avoid poor or
unacceptable academic practice.
The Academic Grievance Procedure For Students, section 3.1.5 requires that, 'A clear statement on the nature
and unacceptability of academic dishonesty, including cheating, plagiarism and fabrication or falsification of
data will be provided to the students by the Course Co-ordinator or the department.' This appendix fulfils that
requirement.
University and Hospital Identification
New Southern DHB identification badges will be issued at the start of fourth year. This ID badge is to be used
during both fourth and fifth year. You must display your ID clearly at all times when in clinical areas.
You will be required to display your University ID, Southern DHB ID, and OMS-DC name badge.
17
Attendance and Leave
Students are expected to attend all (100%) learning opportunities to gain experience, and should demonstrate
enthusiasm, professionalism and commitment to learning. Individual modules will clarify their expectations of
attendance at the beginning of each module. Unsatisfactory attendance may result in terms being deferred or
denied. This particularly applies to all block and vertical module teaching in ALM.
It is however acknowledged that a student may wish to have leave from time to time to attend to personal or
extracurricular matters.
Staff and students have agreed that the process of applying for and having leave approved should be easy,
and without unnecessary barriers. The approval of leave and the decisions about any catch-up work needed
should be fair and reasonable and involve discussion where necessary with the student.
Application for Leave
Students are required to seek approval for all leave and once approved, should notify in advance, appropriate
convenors/administrators, supervisors or tutors. Where possible, planned leave should be requested six weeks
in advance.
Leave requests are submitted on line
https://medschool.otago.ac.nz/course/view.php?id=1760§ion=6
If the leave requested is for longer than 3 days it also needs approval from the Associate Dean (Student Affairs).
Normally, this would involve a brief meeting with the Associate Dean.
If students wish to discuss the process of applying for student leave, the Student Affairs Office can provide
information.
Consideration of Leave Application
When staff are considering approval of leave applications, the following points will be taken into consideration:
Learning or professional development opportunities afforded by the activity
The family or community importance of the student attending the activity
Whether the student has extenuating personal circumstances
Whether the student is participating in a national or international sporting or cultural event
Whether the student is presenting, organising or representing a group at a conference or meeting
The proportion of the module being requested as leave
The reason the activity cannot be undertaken during scheduled holidays
The length of leave relative to the activity
The importance of missed teaching or assessment, and the student’s ability to catch up on missed
activities
The student’s total leave in that year and any other leave in that module
Whether the leave will benefit the wellbeing of the student
If a student’s application for leave is denied by the module convenor(s), or any catch-up required is seen as
being unreasonable by the student, the student may appeal to the Associate Dean (Student Affairs). An
ultimate appeal of a leave decision by the ADSA, can be made to the Dean of the campus in ALM or the Director
of the ELM programme in ELM.
Sick Leave, Bereavement Leave or other Emergency
If a student is unable to attend learning sessions or their attachment due to illness or other reasons the
appropriate tutor(s), module convenor(s), the ELM Administrator (for ELM students) and the Student Affairs
Office must be notified on the first day of the absence and on any subsequent days. This is the student’s
responsibility. It is important not only because of the missed learning opportunities, but also because staff
18
frequently arrange clinics and patients to be available for students so need to know if the student will not be
present. A medical certificate is required for any student absence because of illness for more than 3 days. It
is important that students absent themselves from work if ill, in order to avoid infecting vulnerable patients.
The length of time taken for bereavement leave is also considered on an individual basis. Please note that
evidence of bereavement should be provided i.e.: copy of death certificate, death notice etc.
Dealing with Missed Sessions
Please note in ALM it is the student’s responsibility to arrange any necessary catch up with the relevant module
convenor(s). Normally, in ALM, an approved absence of one or two days on a module would not need to be
made up, provided no essential teaching sessions or experience was missed. Above one or two days, if missed
content/experience cannot be completed within the module, this may lead to a module result of ‘Incomplete’
and a plan made to allow completion. Unexplained absences or absences when leave has already been turned
down, may be considered as unprofessional behaviour when it comes to assessment decisions.
Public Holidays
ALM4/5 Students are not required to work Public holidays
Attendance at clinical rounds while unwell
It is unprofessional to expose patients to risk of infection. Students scheduled for a clinical round whilst unwell
should consider the welfare of those with whom they will be in contact, both patients and colleagues. If in
doubt, please seek advice of staff.
19
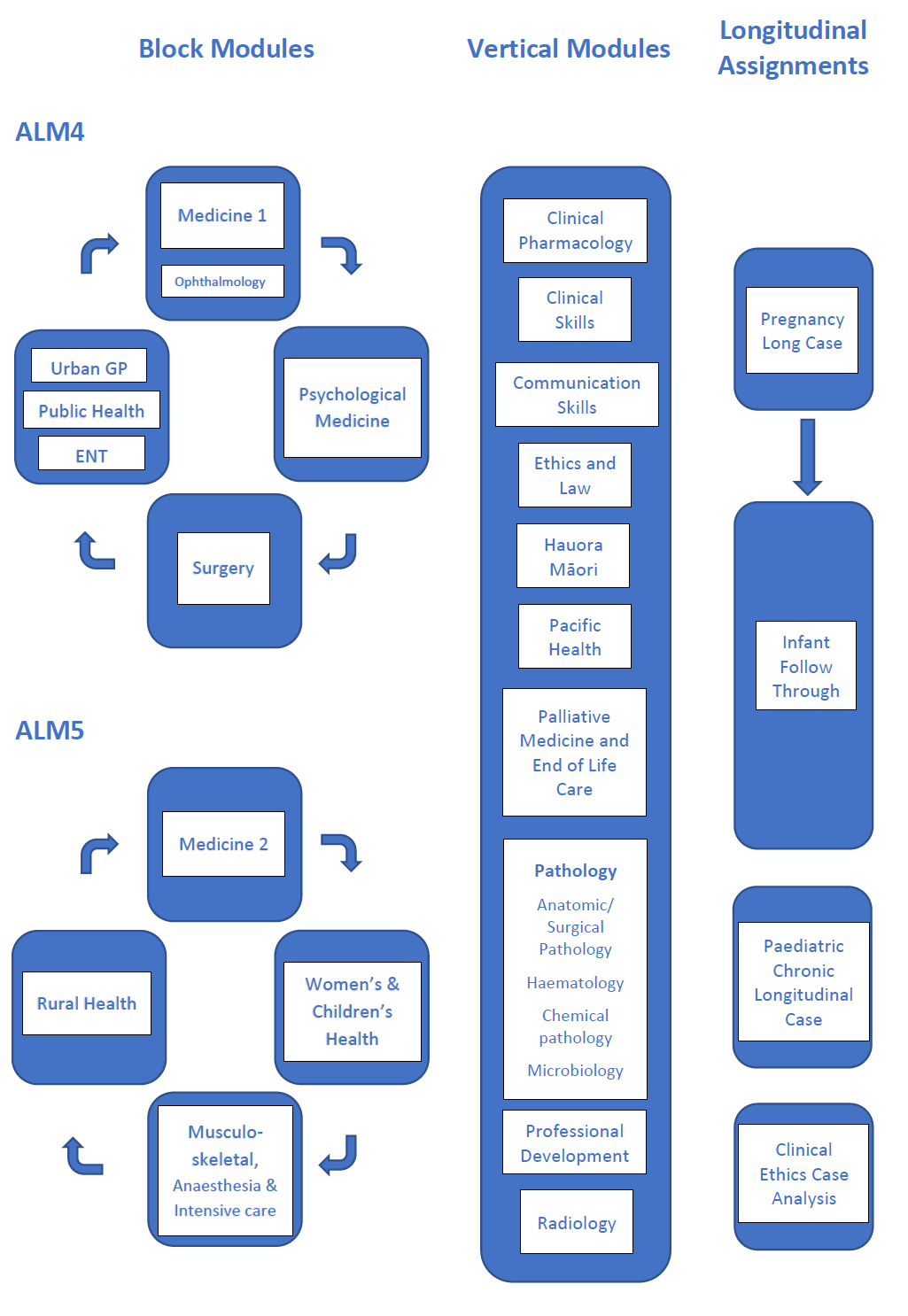
Overview of the ALM programme at Dunedin Campus
20
Overview of ALM 4 Block Modules
Medicine 1 (including Ophthalmology)
The ALM4 Medicine Module is comprised of two four-week attachments that include Internal Medicine (IM)
and Older Person’s Health (OPH). For IM, you will be based in either Dunedin, Timaru or Invercargill (2 students
in Timaru and 2 in Invercargill for each four week attachment). One student will undertake their OPH
attachment in Timaru during weeks 5 – 8. Due to limited capacity in OPH, 4 or 5 students will be placed with
an internal medicine team for their OPH run (OPH/IM), while following the OPH timetable and taking part in
the OPH teaching.
Ambulatory Medicine Teaching is integrated across the whole module and provides focussed, systems-based
teaching with volunteer teaching-patients, and revision of clinical skills with supervision and feedback from
senior clinicians. This teaching occurs in the Otago Clinical Skills Lab (OCSL), Eye clinic and the 9th floor clinic
rooms. Attendance at these teaching events is compulsory.
Vertical module teaching also occurs across the eight-week attachment, including: pathology, pharmacology,
ethics, radiology and communication skills.
Assessment
Summative assessment comprises:
a long case examination (observed history, examination, differential diagnosis and plan for an
inpatient)
an end of run MCQ.
You must pass both these to achieve terms.
To achieve Terms, you must also:
Achieve a satisfactory Clinical Appraisal for each attachment
Achieve a satisfactory PASAF at the end of the module
Out of hours requirements
All students are expected to be available to attend out of hours when their team is on call. This will include
some evenings and weekends, and depend in part on the consultant physician for the team. Additional
information about out of hours expectations is available in the module handbook.
Psychological Medicine
The Psychological Medicine attachment is an eight week module that includes attachments in acute and
longterm management settings. Some students will do a four week placement on the West Coast.
The field of psychiatry includes the primary care sector and the secondary (specialist psychiatry) sector. A basic
knowledge of how to assess and manage patients with a psychiatric disorder is essential and this attachment
is your opportunity to acquire the skills and knowledge to do this. You will learn about the major psychiatric
disorders, develop skills in assessment, in particular the mental state examination and risk assessment, and in
communicating psychiatric findings concisely. It is important to understand mental health problems and
mental illness as a complex interaction of biological, psychological, social and spiritual aspects which all need
to be considered in the therapeutic approach to the patient.
Learning Objectives:
Demonstrate knowledge of the core psychiatric disorders: presentation, diagnostic considerations and
management
Take a psychiatric history, perform a mental state examination and use the Te Whare Tapa Whā model
to learn about the patient as a person
Demonstrate an ability to undertake a risk assessment
21
Assess and quantify cognition; use rating scales to assess depression, anxiety and substance use;
consider relevant cultural, legal and ethical issues in assessment.
Clinical Placements
Students will be assigned to two clinical areas during their attachment, changing over at week 5. Clinical areas
include Wakari Hospital, Dunedin Hospital, Southland Hospital, Te Nikau Hospital (Greymouth) and Community
Mental Health Teams. Students also spend time after-hours with the emergency psychiatry teams.
Teaching sessions
Are scheduled throughout the attachment and are usually case-based. Topics included psychiatric and risk
assessment, the core disorders, history of psychiatry, promotion of recovery and wellbeing. Some sessions are
small group sessions to promote discussion of specific topics. We also use simulation sessions for active
practice and feedback.
Assessment
You will be assessed on your academic work, your clinical skills, participation in learning activities and your
professional attitudes during your attachment.
Formative:
Summative:
Participation in Hauora Maori session
Case Presentation
Participation in Simulation session
Brief Focused Interviews
World of Difference reflective report
Logbook section
Student-generated MCQ
On-line test
Clinical Tutor Evaluation
PASAF
Teamwork
Working as part of a team is integral to your learning experience and you will learn how team members work
together with the patient and their whānau/families and carers. Support each other as you encounter a range
of challenging experiences. Take care of your emotional as well as your physical wellbeing and make the most
of opportunities to discuss and seek support from the clinical and academic team.
We hope that you enjoy this attachment and the many learning experiences offered.
Out of hours requirements
All students will be expected to do at least one evening shift (5.30pm to 10.30pm) at an Emergency Psychiatric
Services during the course of the attachment.
There are no weekend or Public Holiday requirements for the module.
West Coast
During the Psychological Medicine attachment two students at a time will have a clinical placement based in
Greymouth. Travel and accommodation arrangements are made by the Department. Students will be notified
of arrangements and receive a handbook detailing all the information required for this placement.
The West Coast District Health Board serves a population of 32,000 people over an area that is 600km long.
Its isolation and geographical nature provides many challenges and students will have opportunities to
experience how health care is delivered in a rural setting together with the warm West Coast hospitality.
22
Surgery
Your eight week attachment in Surgery will be split into two four week runs. During these runs you will be part
of a surgical team. There are six teams in Dunedin, and two in Invercargill. There are two or three students on
each team, so four students will be assigned to Invercargill for each four week run.
After having been assigned for four weeks to one team, you will rotate to a different team for the remaining
four weeks. These teams constitute your “home base” and one of the team’s tutors will be your home tutor.
Medical students are not visitors – we consider you a member of the team. Observations of and close contact
with patients can bring out aspects which may have been overlooked by other members of the medical
team. You can assist in patient care by informing and discussing your concerns with others in the medical
team. Please, feel at home on the wards. All patients, whether elective or acute, are allocated to a student
who will follow that patient from admission to discharge. You are expected to attend operations on your own
patients and will often be invited to scrub.
During your time with us we would like to see you develop and hone your history taking and examination
skills. Make the most of your contacts with patients – perform a complete examination whenever possible!
Tutorials
Each week during your attachment there will be five x 1 hour group tutorials covering core topics. These
include Full Group (presented by consultant), Whole Group Case-based (presented by students and a
consultant), and Pathology (presented by pathologist and surgery consultant). Attendance at these tutorials is
compulsory.
Assessments
PASAF. After completion of the attachment, each student will be discussed in a conference where all clinical
tutors contribute to your assessment for “performance within the team” as well as supply the information
needed for the “Professional Attitudes and Skills Assessment Form” (PASAF). Your home tutor will discuss the
PASAF with you in the last week of the attachment
CASE WRITE-UP (week 4). One surgical case history is to be completed during the attachment
CASE APPRECIATION (week 6). You will complete an essay/case appreciation of approximately 1000 – 1200
words - choose a specific surgical question that relates to one of your own patients.
LOGBOOK: Each student will be provided with a case notebook to record activities and patients during the
attachment, to be handed in for assessment.
On the last day of the run there the following assessments:
MCQ/ Clinical based question: Comprises 10 MCQ questions (10 marks) and 1 clinical based question
(15 marks). These will cover topics learned during your surgical run (25 minutes).
OSCE stations: There will be two 5 minute OCSE stations. Two areas of clinical skills will be tested from
clinical examination, history taking and explanation and planning.
Out of hours requirements
All students will be expected to attend during weeknight evenings when their team is on call. They will also be
expected to attend for one weekend half-day when their team is on call. There is no requirement to be present
on Public Holidays.
Urban General Practice Module
This is a 5 week module that sits alongside the 3 week Public Health module. Together these attachments
constitute an 8 week quarter for the year. ENT teaching and clinics are also incorporated in this quarter, taking
place during the middle 6 weeks.
During the GP Module you will attend a combination of tutorials and simulated clinics, and 10 clinical sessions
with a GP in his or her practice. Ideally while on placement, we would like you to include at least one session
23
with a Practice Nurse, who is an integral member of the Primary Care team. At least four students each quarter
will do their GP placement in Invercargill.
A clinical session will generally be a half-day, either in the morning or the afternoon. Start and finish times will
vary from practice to practice.
Department-based morning sessions will begin at 9.00am, while afternoon tutorials will start at 1.30pm or
2pm, as indicated in the Module timetable. These are a mixture of whole group tutorials and small group work.
Seesions in the Clinical Skills Lab will start at either 8.45am or 9.00am, as indicated in the Module timetable.
These sessions include a clinical skills workshop, and a series of simulated clinics (called SECO clinics.) You will
be given plenty of information about these clinics in the orientation to the Module, which takes place on the
first day of the attachment.
The timetable for the run will be available on Moodle for each quarter, and a hardcopy is made available for
those who would like it. It has been configured so that most of the department-based teaching will take place
in the first and fifth weeks of the attachment, with plenty of time available in the middle three weeks to
undertake your GP sessions.
Students based in Invercargill will follow a different timetable for weeks 2 – 4 of the placement, and will be
briefed by our Invercargill teaching staff. Tutorial content delivered in Invercargill mirrors that being taught in
Dunedin.
Assessment
The attachment concludes with summative assessments, which take the form of a 5-station OSCE and an SAQ
test.
You are also required to submit a reflective essay on your SECO clinic experience (max 1000 words), and
demonstrate satisfactory clinical skills and professionalism while on placement with a GP.
The final day of the module involves a one-to-one PASAF meeting for feedback with one of the Module tutors.
Out of hours requirements
There are no after hours requirements for this Module, however students are welcome to attend after hours
clinics with their host GP if the opportunity arises.
Public Health Module
The Public Health module is three weeks long, and is mainly classroom-based with some self-
directed work. This module runs in conjunction with the Pacific Health vertical module, which includes the
Pacific Immersion Programme – during which you will live with a local Pacific family for a weekend and take
part in family and community events (COVID Alert Level dependent). Some of you will also attend ENT clinics
during this rotation.
Content
The Public Health module builds on some of the concepts taught during the ELM programme, and develops
your ability to apply these concepts using real world examples. Topics covered include Epidemiology/ Critical
Appraisal; Public Health Ethics; Health Economics; Health Promotion; Qualitative Research; Occupational
Medicine; Healthcare for people who are Intersex, Non-binary, and Transgender; Envirinmental Health;
Hauora Māori issues in Public Health; Communicable Disease/Outbreak Management; Health Systems; and
Screening.
Site Visits (COVID Alert Level dependent)
During the module, you will visit a community organisation that provides a public health service (e.g. drinking
water treatment facility, needle exchange, Kiwi Harvest). These visits are undertaken in small groups, and your
group will present the details of your visit to the other students later in the module. A factory visit is
undertaken as part of the Occupational Medicine unit, and a visit to the local Public Health Unit at Wakari
Hospital is part of the Communicable Diseases teaching. The Hauora Māori day takes place at Te Kāika, a
community hub located in Caversham that provides medical, dental, physiotherapy, and social services.
24
NB. Transport is provided to Te Kāika and the factory visit, but you will need to organise your own transport for
the Public Health Unit and community visits.
Assessment
There are three assessments in this module.
1. End of run test (40%). This is a one hour test, the format is similar to the Public Health SAQ in the
5th year exam. You must get 60% on this test to pass the module.
2. Study design assignment (40%). This is an essay-style assignment for which you will design an
observational study (cohort or case-control study). You will work with a partner to design the study,
but must submit individual assignments (2,500 words)
3. Participation in Pacific Immersion Programme + reflective essay (20%)
Out of hours requirements
One weekend of the Module encompasses the Pacific Immersion Programme. Detailed information about this
weekend is available on the Pacific Health Moodle page.
ENT/ Otorhinolaryngology, Head and Neck Surgery (ORLHNS) Module
The ORLHNS module is embedded in the Urban General Practice and Public Health Modules. You will find
plenty of supporting material on Moodle: Lectures with voice over, written notes, and “presentations”. These
cover the syllabus and complement your clinical teaching.
Clinical teaching takes place on Tuesday and Friday afternoons between 2pm and 3.30pm. You are split into
small groups for this teaching, and will receive a roster indicating when it is your turn to attend these sessions.
There are also six tutorials on Tuesdays at 4pm. These are whole group sessions. The timetable for teaching
tells you what material is relevant for the tutorials.
The clinical teaching includes simulation activities, each will have an introduction followed by the activity. Each
activity takes about 30 minutes. You will also see a patient in clinic, so it is important that you are appropriately
dressed for this interaction.
Assessment
Towards the end of your module, you are required to complete an on-line assessment. This is available on
Moodle and the material provided covers the questions in the assessment. You are expected to pass this
assessment as part of the run. More than 75% correct is a pass, you are allowed 4 attempts. So far no-one has
failed to pass the assessment, so don’t get too worried; it is part of your learning experience.
Out of hours requirements
There are no after hours requirements for this Module.
25
ALM4 Longitudinal Assignments
Pregnancy Long Case (PLC)
This attachment gives you the opportunity to share in a pregnancy, labour, delivery and postnatal experience
with a family and their midwife. Within reason, commitments to this attachment are to be prioritised over
Block Module requirements. If a potential conflict arises between commitments then you should discuss this
with your Block Module Convenor.
At the start of ALM4, you will be informed which quarter you will do your pregnancy long case. This will be
timetabled around when you are in Dunedin, rather than on an out-of-town placement. If for some reason
there are extraordinary circumstances making it difficult for you to undertake the PLC attachment at a
particular time of year, please contact Mel O’Brien
([email address]) as soon as you have
identified these, and we will try our best to help you.
You will be assigned to a pregnant woman who is due to give birth soon and who has agreed to have a medical
student involved in her care. The midwife looking after the woman is one of our midwife tutors (who is
experienced in teaching medical students) and will get you as involved as possible, especially during the labour
and birth. You will also have a home tutor who is one of the Women’s Health University Lecturers, who will
help you navigate the PLC and will mark your assignment. If you are assigned to be with a woman who gives
birth before you have had an opportunity to attend an antenatal visit with her, your home tutor is the person
with whom you should discuss this.
The learning outcome for this attachment is to gain an understanding of ‘normal’ pregnancy and birth, which
can be straightforward or complicated, but is generally unpredictable, and always exciting. Once you have
been assigned a pregnant woman, which usually happens 1-2 weeks into the quarter of your
Pregnancy Long Case attachment, you will arrange to meet her and attend at least one antenatal visit, and be
present at the birth, then see her in the postnatal period. Usually you will then follow that baby for your
Paediatric Infant Follow-Through.
At the end of the PLC you will be able to:
Take an obstetric history
Conduct an obstetric examination including blood pressure, urinalysis, estimate the size of the fetus
by measuring the fundal height, determine the fetal lie, presentation and position by palpation, and
record the fetal heart rate
Describe the principles of antenatal care including risk assessment
Describe the stages of labour, and the principles of management of labour and childbirth
Write a reflection on your involvement in the woman’s care and birth
Describe the principles of postnatal care
Describe the breast changes in pregnancy and lactation with reference to your mother and baby
Assessment
This module is assessed by both the midwife tutor that supervises the clinical portion of the long case (via an
assessment form), and a written assignment of around 3000 words. As part of the assignment you will take an
obstetric history and consider the risk assessment for the pregnancy, labour, delivery, and describe postnatal
care. We ask you to describe the normal physiology of birth and lactation, and to consider any pathological
or ethical issues that might arise for your pregnant person and their whanau. The assignment is to be handed
in 10 working days after the birth.
26
Infant Follow-Through Long Case
The infant follow-through case is an opportunity to follow an infant from birth to 18 months. The case will
start in ALM4, when you are assigned a mother to follow in the pregnancy long case. It continues into ALM5,
with a submission date in September of ALM5.
You will have the opportunity to be at the infant’s delivery, talk to the family about their experience, learn
about new born care, and participate in examining an infant. You will then continue to follow the infant by
visiting the family up to 18 months. You will be engaging with the family about their experiences with a new
child, learn about feeding, immunizations, and track the development of your infant from a new born to 18
months. This is a great opportunity to observe gross motor, fine motor, social, cognitive, and language at
various developmental stages.
It is up to you to initiate and maintain contact with your assigned family. If you are having difficulty doing this
you should contact the Long Case convenor.
27
Overview of ALM5 Block Modules
Medicine 2
(Information from Moodle. May be updated during the year.)
The seven week ALM5 Medicine Module comprises an introductory week of whole group learning, then two-
week attachments with Cardiology, Respiratory Medicine and one other medical specialty.
There are also outpatient clinics and ambulatory days in Oncology, Endocrinology and Renal medicine.
To achieve Terms for Year 5 Medicine you must:
1. Pass the requirements for the Cardiology, Respiratory, Medical Specialties and Ambulatory Medicine
as described in relevant sections of the handbook.
2. Submit 2 case write-ups at a satisfactory standard.
3. Pass the OSCE examination.
An overall PASAF form will be completed for the module. This will be discussed with you individually on the
last day of the module.
Out of hours requirements
To be advised
Child Health and Reproductive Medicine Module (WCH)
This seven-week module comprises two combined attachments:
Child Health - approximately 60% of the course
Reproductive medicine - approximately 40% of the course
Over the seven-week module, there will be a mixture of teaching tutorials and some case based interactive
sessions.
Your Child Health clinical experience will be in the Children’s Unit, NICU and outpatient setting. Reproductive
medicine’s clinical experience will be in theatre, inpatient and the outpatient setting. Most students will spend
at least two weeks of this module in Invercargill.
Students describe this as a busy run with the two attachments, but their feedback has reported how organised
and supported their time with us was.
Assessment
Summative Assessment during this attachment:
Child Health case write-up with critical appraisal
Reproductive medicine case synopsis
Reproductive medicine case presentation
End of attachment MCQs
End of attachment online OSCE
Out of hours requirements
To be advised; includes one weekend on Acute/on-call Paediatrics, hours 8.30am to 11.00pm both days.
28
Musculoskeletal, Anaesthesia and Intensive Care
(Information from Moodle. May be updated during the year.)
This is an integrated teaching module incorporating four main disciplines: Orthopaedics, Rheumatology,
Anaesthesia and Intensive Care. The course has been designed to assist you in bridging the gap between the
ELM Course where the emphasis has been on basic sciences like anatomy, physiology, pathology etc. and the
Trainee Intern year which focuses on clinical skills and problem solving.
The module is divided into a 7 week clinical attachment and two block teaching days which are part of the
Whole Class Learning (WCL) weeks. Teaching includes time on the wards, in outpatients’ clinics, in tutorials
and in theatre.
In 2021 some students will do some of the placement in Invercargill, with the aim of some students completing
the whole module in Invercargill from 2022.
Assessment
In Course Assessment
This will be based on the following:
Satisfactory attendance including rostered nights and weekend acute attachments
Satisfactory participation in team activities
End-of-Attachment Assessment
The end of attachment assessment will comprise
at least 3 observed 7-minute OSCE stations, covering orthopaedics, rheumatology and emergency
management
57 extended matching MCQs (computer-delivered)
At the end of the OSCE there will be a feedback session with the examiners where the exam will be discussed
with the students.
Assessment of non-academic skills
Each student will also be assessed on the standard University of Otago Assessment form for Medical Students
(PASAF) by the orthopaedic consultant whose team you have been attached to.
Out of hours requirements
All students will be rostered to an on-call Acute team and expected to attend during weeknight evenings
(5.00pm tp 11.00pm) with that team. They will also be expected to attend for an acute weekend, hours 8.30am
to 11.00pm both days. There is no requirement to be present on Public Holidays.
29
Rural Health Module
All placements are outside of Dunedin
Rural Health offers a valuable opportunity to challenge yourself in preparation for your Trainee Intern year:
significantly expanding and consolidating your knowledge and skills
integrating and applying everything you have learned so far
actively participating in the clinical work of your placement (under appropriate supervision), as part
of the team caring for patients.
During Week 1 you will be based at the Department of General Practice and Rural Health. We have a
busy programme of tutorials, simulated patient clinics and other activities designed to prepare you for
the rural clinical environment, activate your pre-existing knowledge and skills, and identify your priorities
for learning. You will also need to finalise arrangements for your placement, including travel, accommodation
and record-keeping.
You will be on placement in a rural or provincial setting during Weeks 2 – 6.
We take your preferences and personal circumstances into account when assigning you to a pacement, as far
as possible given the limited number of practices available and other constraints. We are generally not able to
announce where you will be going more than 1 – 2 weeks in advance, as we need to procure places for the
whole group before informing individual students. Options often include Motueka, Golden Bay, Greymouth,
Central Otago, Oamaru, Kurow, Temuka, Geraldine, Waimate, Twizel, Tapanui, Winton, Te Anau, Tuatapere,
Gore and Mataura.
Most locations necessitate a driver licence and we strongly advise you to make the effort to get your full
licence before this module, if at all possible.
We send students to a variety of GP practices, and some of you will also spend time at a Rural Hospital
(e.g. Dunstan, Oamaru). Our clinical teachers are mostly GPs, but include Nurse Practitioners and Rural
Hospital Doctors. Where possible we encourage you to attend emergencies in the community with responders
such as St John.
While away from Dunedin you will learn from each other by sharing cases and experiences on our Moodle
discussion board.
In Week 7 you will be back at the GP Department for discussion and reflection on the preceding weeks to
maximise your learning, as well as assessments.
Assessments for the Module comprise
a feedback form from your clinical placement supervisors,
a clinical problem-solving assessment,
a small group presentation on an assigned topic,
a written multiple-choice question and short-answer question exam,
a five-station OSCE (history, examination x2, explanation and planning x2).
You are also required to demonstrate appropriate professionalism throughout the Module.
We look forward to supporting you in an enjoyable and stimulating programme, and hope that becoming a
clinician will start to be a tangible reality for you!
Out of hours requirements
We encourage you to make yourself available for up to five ‘on-call’ (after-hours weekdays, or on weekends)
shifts during the five week placement, where this is available. If it is possible to spend some time with the
Ambulance service during your placement, this is also a very valuable experience. It is your responsibility to
arrange your participation in after-hours shifts by liaising with your host GP, rural coordinator, hospital
doctors, St John Ambulance staff.
30
ALM5 Longitudinal Assignments
Paediatric Chronic Longitudinal Case
During your first 5th year Whole Class Learning Week you will be assigned in pairs, a child with a chronic
condition to follow until September that year.
A chronic condition in a child can affect their functioning and development into a competent adult. It also
affects the functioning of the whole family, and the community, and medical supports that revolve around
them. This assignment aimed to give you some insight into these issues, which you will not be able to
appreciate from your contact with acute hospital paediatrics alone.
To appreciate the impact of a chronic condition on the child, family/whānau you will be required to visit them
in their home a minimum of three times between February and September.
Summative assessment submission date is in September:
Family evaluation 30%
Essay or artistic expression with a write-up 70%
Clinical Ethics Case Analysis
Each member of the class is expected to write up and submit one ethics case analysis, due early in the second
semester of ALM5.
Submission of a satisfactory case analysis is a condition of successful completion of the module. It will be used
to evaluate your sensitivity to ethical features of practice and your reasoned application of ethical concepts.
You will be given feedback on your essay.
The case analysis can be about a patient (duly anonymised) from any of the rotations that you have done in
year five (or year four if you came across a situation then that you wish to analyse). It should be suitable for
ethical analysis, i.e. raise particular ethical, or demonstrate ethically challenging areas of practice. They do not
need to be insoluble dilemmas, and may demonstrate high ethical and legal standards as well as difficult
situations. The best ethics case write-ups are often ones where you have been moved to think about it at the
time or later on. So, if you saw a situation that made you think about ethics that’s probably a good one to pick.
Detailed information about this essay, including a marking rubric, are available on the Ethics Moodle page.
31
Overview of Vertical Modules
Clinical Pharmacology
The primary purpose of the clinical pharmacology module is to prepare students to be able to prescribe safely
and effectively. A secondary purpose is to enable students to participate in the processes of using medicines
safely, through reporting and recording of adverse drug reactions and adverse events.
Clinical pharmacology provides the science that underpins the use of medicines (therapeutics). Understanding
this science will improve your ability to prescribe, and to use medicines safely and effectively.
Clinical Pharmacology teaching occurs during Whole Class Learning weeks, Thursday afternoon teaching
sessions in 4th year, and in a number of block modules in ALM, including:
Medicine 1
Surgery
Child Health and Reproductive Medicine
Musculoskeletal, Anaesthesia, Intensive Care
The Clinical Pharmacology teaching is aligned with the essential learning medicines list, the core presentations
and the learning objectives.
Assessment
In the 3rd quarter of Year 5 there will be a MCQ test which is a terms requirement. You must achieve a mark
of 75% to pass, but you can have multiple attempts at the test and your best mark will be the accepted score.
You are expected to prepare for each tutorial in Years 4, 5 and 6 by watching the recorded mini-lecture, reading
the associated readings, answering the multiple choice questions for each session and by preparing answers
to the case-based tutorial questions which you will bring to each feedback session.
Questions relevant to the clinical pharmacology teaching may be included in the end-of run assessments and
in the common-component exams at the end of Year 5.
Clinical Skills
In ALM you will build on the foundational skills introduced in ELM. Competence in clinical skills is central
to becoming a capable clinician – able to communicate well with patients and colleagues, gather information
from history and examination, think critically, prioritise appropriately, formulate a coherent diagnosis and
management plan, and carry out the plan.
As clinicians who need to be able to work in challenging environments, sometimes with incomplete data and
limited resources, we must cultivate an awareness of our own thinking processes, including how we
approach uncertainty and the potential for biases and error.
We need to be competent at a broad range of procedural skills, e.g. effective hand washing, urine dipstick
analysis, safe disposal of sharps, suturing wounds, drawing up and checking intravenous drugs, controlling
external haemorrhage by direct pressure, and urethral catheterisation.
Clinical skills is an integral part of ALM, and you will have many opportunities to acquire and consolidate the
knowledge and abilities that you need to ‘think like a doctor’, and the associated procedural skill set.
Specific learning opportunities and resources available include the Communicating in Challenging Situations
module, simulated consultations (e.g. SECO Clinics in the 4th Year Urban General Practice Module and
5th Year Rural Health Module), procedural training at the Otago Clinical Skills Laboratories (Fraser
Building), clinical reasoning exercises, your 2nd and 3rd Year Clinical Skills workbooks and videos,
and the clinical skills app.
Please see our Moodle page for further information, and to download the app:
https://medschool.otago.ac.nz/course/view.php?id=1900
32
Communication Skills
The Communicating in Challenging Situations module runs through three of the four attachments in ALM 4.
We hope that your previous learning in ELM Clinical Skills will help you to make a smooth transition to this
module.
In this module you will have the opportunity to work individually with a tutor (and also in small groups) to
identify areas of communication that you would like to improve and also to apply your communication skills
to challenging clinical situations which are directly relevant to each of the following attachments: Medicine,
Surgery and Psychological Medicine.
By the completion of 4th year we hope you will have expanded your knowledge and skill base to have
confidence in situations that even experienced professionals can find difficult.
Course Requirements
1. Participation in three group tutorials over the year – one for each of the following attachments:
Medicine, Surgery and Psychological Medicine.
The tutorials in Medicine and Surgery are designed to help you prepare for your filmed interviews.
The tutorial related to the Psychological Medicine attachment is a 1.25 hour skills-based tutorial which
will require some pre-tutorial reading, followed by in-class skills practice.
Students who are on placement outside of Dunedin at the time of a tutorial will be provided with
tutorial notes and, in the case of the Psychological Medicine tutorial, catch-up work to complete.
2. Completion of two filmed interviews (one in Medicine and one in Surgery) with an actor playing the
patient role. Completion of pre-tutorial and in-class work related to the Psychological Medicine
attachment.
3. Completion of online reviews for both of your filmed interviews (using Bracken Learning - the online
reflection system) followed by attendance at the individual, face-to-face meetings with your
Communication Skills tutor for each of your filmed interviews. The times/dates of all tutorials, filmed
interviews and 1:1 reviews that you need to attend will be emailed to you in advance as the year
progresses.
Ethics and Law
The teaching on ethics and law in ALM builds upon the teaching you had in ELM. It aims to extend your
sensitivity to and understanding of the concepts introduced in ELM, and to develop your ability to apply them
in a range of areas of practice, particularly (though not exclusively) clinical situations. Through this you will
become able to make complex ethical decisions on the basis of sound ethical reasons, in accordance with New
Zealand law.
Most of the teaching occurs in tutorials placed within each rotation. They are led by teachers from the
Bioethics Centre, sometimes with clinicians from the current attachment. The ethical issues taken up in each
tutorial will reflect those typically encountered on that attachment. Some teaching also occurs during whole
class learning time.
In some tutorials, students will be expected to present cases that will be discussed and reflected on by the
class.
Lectures on medical law, prepared by a local health law specialist, will be available on Moodle, and time will
be allocated to view these during whole class learning time. Legal concepts are often raised and discussed
in the tutorials. This reflects the close relationship between ethics and law.
In year 5 you are required to complete a written ‘Clinical Ethics Case Analysis’. This is the only in course
assessment for this module – see the Moodle page for details. There will also be a short answer question
relating to ethics, law and professionalism in the end of year exam.
General supporting material is on Moodle. See in particular the 'Introduction to Clinical Ethics', and the
glossary of key concepts introduced in ELM.
33
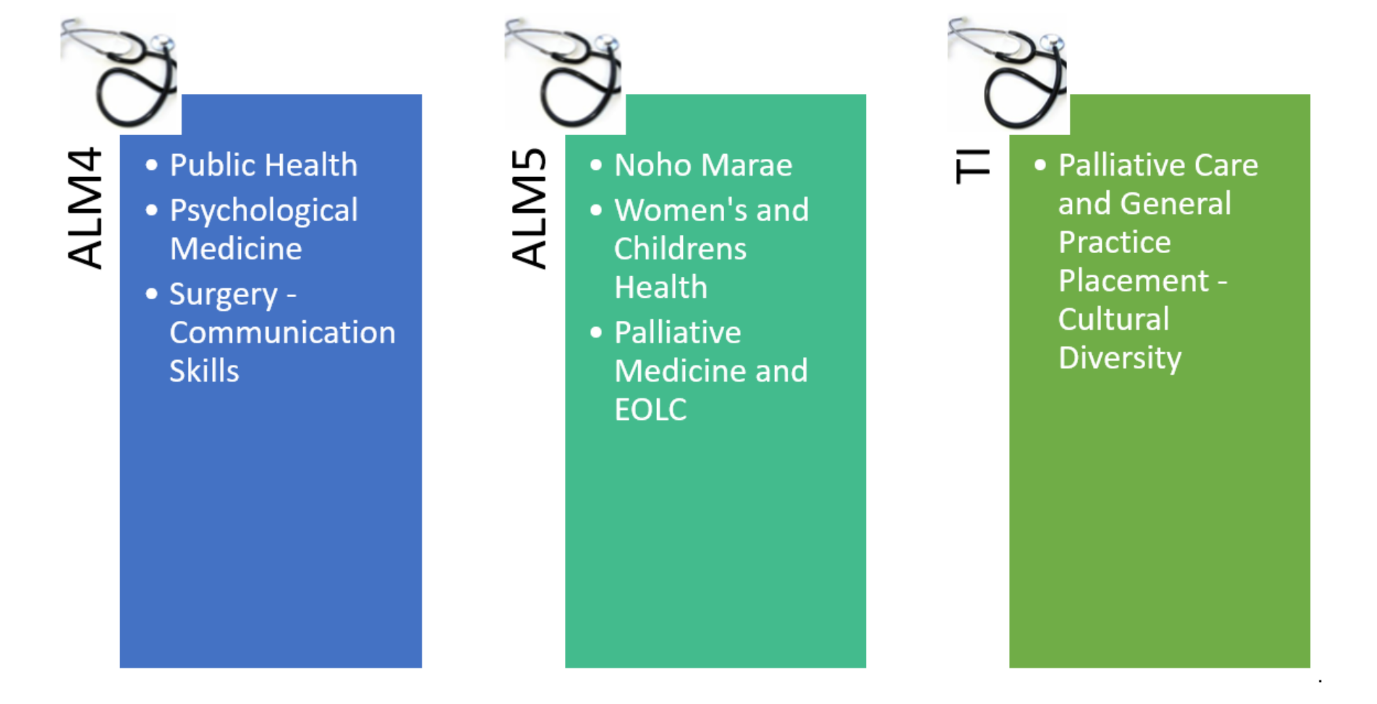
Hauora Māori
Hauora Māori/Māori Health
Tēnā koutou katoa.
Nau mai, piki mai, kake mai rā ki Te Whare Wānanga o Ōtākou. Koia nei te kāpui Hauora Māori mō ngā tauira
i eke mai nei i te pūtake. Kāore e ārikarika te whai whakaaro ki a koutou: anei kē mātou hei poutokomanawa,
hei pou whakawhirinaki i ngā tau kei te heke mai, ā haere ake nei.
Welcome to the University of Otago, Dunedin Hauora Māori vertical module for ALM students. We look
forward to supporting your learning in ALM Hauora Māori and your development as doctors throughout the
coming years.
Hei whakapā atu/Contact Information:
Kaituku/Convenor: Ahorangi/Professor Joanne Baxter Imeera/Email: [email address]
Kaiwhakahaere Tari/Adminstrator: Tui Kent Imeera/Email: [email address]
Our address is 71 Frederick Street. Our whare/building is on the corner of Malcolm and Frederick Streets,
alongside the Hunter Centre Annex. We welcome students who are needing support with regards to Hauora
Māori. We are accessible via email to make appointments.
Tiro Whānui/Module Overview:
Aims of the Hauora Māori Curriculum
To prepare graduates to work alongside Māori patients, whānau, providers and community to support Māori
health advancement, through:
Acknowledgement of Māori as the indigenous peoples of Aotearoa/New Zealand, and understanding
the ongoing impact of colonisation and racism on current Māori health status.
Demonstrating an ability to support Māori community initiatives and following Māori health
leadership/ guidance.
Demonstrating Hauora Māori competencies that identify and respond to individual patient/whānau/
community expectations e.g. use of te reo Māori, inclusion of tikanga within health service delivery,
inclusion of whānau within the health journey etc.
Delivery of health services that support equitable health outcomes for Māori patients/whānau/
community.
Advocating for health system and/or policy changes that support health equity that is tailored to
diverse needs within Māori communities.
34
5th Year Hauora Māori Immersion Week
The 5th year whole class learning immersion week in Hauora Māori, involves a four day programme. The first
day is on campus, and provides a platform for key learning for the rest of the week, followed by a half-day of
independent learning. The remainder of the week, involves a Noho Marae, staying at one of the local Ngāi
Tahu marae in Otago, experiencing a cultural immersion and engaging with a range of sessions aimed at
enhancing competence and confidence in Hauora Māori practice. Resources to enable you to prepare for this
event are available on our Moodle page.
The focus of Hauora Māori teaching and learning for this week is for you to participate in and experience
Hauora Māori in Action, exploring how to make a difference in Māori health, across a range of areas including
clinical, community and as 'agents of change'. The settings include on-campus and from within a marae and
community setting.
One key aim is to build on knowledge and skills in the practice of medicine in Māori health - working with
Māori individuals, whānau and communities. Marae are an important part of the lives of many Māori and
marae reflect and embody Māori relationships with health, wellbeing, and the past, present and
future. Gaining an understanding of Hauora Māori within a marae and community context provides an
opportunity for gaining further insights and understanding about Māori Health and ways of working with
Māori.
ALM Assessment for Hauora Māori vertical module
Attendance at all Hauora Māori teaching in ALM is a terms requirement, and absences will require catch-up
sessions to cover missed material
Hauora Māori in ALM in the Dunedin Campus is examined in 5th year in the end-of-year exam, and may be
assessed in any of the examination formats: OSCE, MCQ or SAQ.
The 5th year Noho Marae is also a terms requirement and students are expected to attend the full noho. A
reflective essay is part of the assessment from the noho.
35
Pacific Health
Pacific Health in ALM builds on what was taught in ELM to further broaden students’ knowledge and
understanding about the health of Pacific peoples in New Zealand and the Pacific region. It promotes the
importance of appreciating diversity in our pacific communities, understanding shared values, and includes
the strengthening of engagement with pacific patients to improve health outcomes.
The teaching of Pacific Health embraces community involvement and provides opportunities to learn within
non-traditional settings. In ALM 4, the Pacific Immersion Programme (PIP) provides the opportunity for
students to spend a weekend within the Pacific community. The Samoan, Cooks Islands, Tongan and a mixture
of minority ethnic communities have offered to host students. Prior to the weekend, students are fully briefed
and prepared for engagement and how best to learn within this environment, with a debrief session after the
weekend. Students are required to write a reflective essay about their experience. This has been a
transformative part of learning from many students, and our staff will prepare you well for engagement
through this learning opportunity.
In 2021 Groups B,C and A will have their PIP weekend during the Public Health Module, while Group D will do
this during the Urban GP Module.
In addition to learning about Pacific Health through engagement with local communities, students will have
an opportunity to learn about health in the international context through the Global Health Classroom. This is
peer-led case-based learning, organised with medical students at the National University of Samoa. This is an
interactive online class, where students from both medical schools share learning based around real cases in
each of their respective countries.
There is a whole day teaching in ALM4 on mental health involving whole class teaching with Pacific mental
health specialists, and small interactive group sessions utilising e-resources and the wealth of experiences
from members of our Pacific community.
In ALM5 our whole day teaching is on women’s health and engages relevant Pacific health specialists in
women’s health, and smaller interactive group sessions with members of our pacific community.
Handbooks for our whole day teaching and extra resources will be available on med moodle prior to each
teaching session.
Palliative Medicine and End-Of-Life Care
Palliative and end of life care (PEOLC) is an inherent part of clinical practice in most healthcare settings, so you
can expect to be directly involved in caring for patients and their family/whānau who have life-limiting and
life-threatening conditions in your learning and future practice as a doctor. This module aims to help you
develop the necessary knowledge, skills and attitudes to be able to provide a high standard of primary (non-
specialist) palliative care in a broad range of situations and healthcare settings by the time you qualify as a
medical doctor.
PEOLC is an integrated module that is embedded within the teaching provided by various departments,
progammes and modules from years 2-6. Essential principles and concepts which underpin the practice of
PEOLC are introduced in ELM (e.g. philosophy of palliative care, loss, grief and bereavement, ethical principles,
illness narratives and hospice care), while ALM focusses more on clinical issues such as symptom management,
ethical issues, end of life care and advanced communication skills. Much of your learning about PEOLC will also
occur informally on clinical attachments through your interactions with patients, families and the healthcare
team. You will learn a lot from these experiences and while it can be challenging, it is also enormously
rewarding, both personally and professionally.
PEOLC works closely with other modules and disciplines to coordinate your teaching and learning experiences.
The learning objectives, ppt presentations, readings and other resources are posted on Moodle. There is also
a palliative care student interest group (SIPmed) that meets monthly (look for it on facebook and join the
group so you receive notifications about meetings and other relevant information).
36
Pathology
Pathology teaching includes Anatomic/surgical pathology, haematology, chemical pathology, and
microbiology.
Anatomic pathology: You will get instructions to access online learning material (Kuracloud) during the 4th year
medical and surgical block modules. In addition, weekly tutorials will contribute to your teaching in anatomic
pathology. In addition, some pathology such as skin lesions and lymphoma is taught during whole class
time. During 5th year you will have pathology teaching during the musculoskeletal and gynaecology rotations.
Haematology: Haematology is mostly taught during the Thursday afternoon whole class sessions, in a mixture
of lectures, small group work and online resources.
Microbiology: Building on teaching from the last three years, practical skills in microbiology will be taught
during whole class time in 4th year, as well as during some of the Block Modules in both years (e.g. Urban GP,
Musculoskeletal, and Rural Health.
Chemical pathology: Selected aspects of chemical pathology will be taught in 4th year on Thursday afternoons
and in the Urban GP module. In addition, use your renal, respiratory, endocrine and other teaching within the
medicine module to learn chemical pathology.
Professional Development
Professional Development helps you become an effective and respectful doctor. The three clinical years will
provide you with learning opportunities and support so that the aims of the course are successfully met. You
will then be responsible for your own ongoing professional development throughout the rest of your career.
Our Professional Development program will provide you with an excellent base from which to continue as a
graduate. Important building blocks will be presented, and targeted sessions for skill development organised,
with an emphasis on the importance of effective collaboration with other students and healthcare colleagues,
as well as patients. The program in DSM features ongoing mentoring in peer groups throughout ALM 4, 5 and
6.
Thursday afternoon and WCLW sessions provide classroom learning opportunities throughout years 4 and
5. All clinical attachments provide the opportunities to experience doctors “at work” and to be developing
your own sense of what this means for you, and your own practice, as you progress through the course.
Whole Class Learning Week Program
Professional Development sessions are designed to be interactive and will build on on material available on
Moodle, as well as your own clinical experiences. Many of these sessions are not recorded, for obvious
reasons, so attendance is considered a professional duty. If you are unable to attend a session, please let our
Administrator Angela King know your reasons.
Mentoring
Early in the academic year you will be assigned to a mentor group and mentor, with whom you will be required
to meet on a number of occasions though the year. For ease of logistics and ongoing functioning these groups
will generally be aligned with your clinical attachment groups. Active engagement within this group is a
requirement for satisfactory completion of each ALM year, and will be documented by your small group
mentor. Any concerns regarding this will be dealt with by the Convenor Dr Nigel Thompson in conjunction
with your group Mentor. More information about this will be provided in the Introductory Whole Class
Learning weeks for both ALM4 and ALM5.
Active participation in a Mentoring group allows students to productively review clinical experiences together,
in a peer group facilitated by an experienced faculty member. These groups provide a confidential
environment for students to individually and collectively reflect on, and learn from, their clinical experiences.
This is a key format for ongoing professional development which is mandated at the post-graduate level by all
of the Medical Colleges in New Zealand and is required by the New Zealand Medical Council for ongoing re-
accreditation.
TPERs
37
Thought Provoking Event Reports (TPERs) provide a means for students to develop and display their capacity
for reflective practice in a confidential individual assignment. This will involve the submission of a short written
account to a secure section of Moodle, which will then be discussed privately with your Mentor in a 20 – 30
minute one-on-one session. It is a terms requirement to complete this TPER assignment to the expected
standard. One report will be required to be submitted and discussed with your mentor during each year of
your ALM study. In the event of scheduling difficulties the Convenor Dr Nigel Thompson will help complete
this task.
Radiology
(Information from Moodle. May be updated during the year.)
The overall purpose of the radiology vertical module is to ensure that you have the ability to function
effectively in clinical practice as a first year house officer.
Specific radiology teaching sessions are timetabled during your attachments. You will also encounter radiology
opportunistically as you work with patients in clinical settings. You should seek opportunities to increase your
understanding of radiology and practice interpretations with the support of your clinical teachers.
A number of useful support resources are provided on Moodle to assist you.
Assessment
Radiology as a discipline is not independently assessed, however it is embedded in many aspects of the
curriculum.
You can expect questions that require the interpretation of basic radiology, as defined in the objectives
(available on Moodle), to occur in end-of-run assessment and in your 5th year final examinations.
38
Rural Medicine Immersion Programme (RMIP) for ALM5
Each year twenty-five Otago Medical School students will get the opportunity to spend their ALM5 year in
rural New Zealand. This option has been available since 2007 and, as of 2020, two hundred and sixty-
four students have passed through this programme.
Students are placed for the whole academic year in groups of three or four students in one of seven regional
teaching centres based on Dannevirke, Masterton, Blenheim, Greymouth, Ashburton, Queenstown and
Balclutha. They spend half their time attached to the local small hospitals and the other half in the general
practices. They work in an apprentice-like model with the medical officers, general practitioners, nursing and
ancillary staff caring for patients in their facilities.
Learning is largely self-directed and occurs through the high level of patient contact provided in this
programme, as organised by local regional teaching centre coordinators. Students will see patients under the
supervision of experienced medical staff, take that experience away and, in self-directed learning time
research and learn about those conditions they have encountered. They also get time to study conditions they
have not yet encountered, to ensure they achieve good coverage of core curriculum conditions. The
experience of working under the supervision of professional personnel, observing procedures, doing the same
under supervision and when confident alone accumulates for the student a good repertoire of core
skills. Students are required to do four after-hours sessions a quarter to experience the emergency situations
in rural practice.
A half-day tutorial time each week is conducted by the local coordinator in their teaching centres and four
residential weeks provide some specialist based learning opportunities. Students are encouraged to become
immersed in the environment of the community, and take up opportunities to engage in cultural, sporting and
outdoor activities. The student experience is excellent, patient exposure is high and they experience the real
medical life they are training for.
Assessment occurs towards the end of each quarter with MCQs, SAQs, OSCEs, assignments of case studies, an
ethics essay, all checked and reported back to the student. Each student compiles a portfolio of prescriptions
and referral letters they have created. Students sit the Otago Medical School’s end of year assessment in
common with the students of the Dunedin, Christchurch and Wellington campus.
Students arrange to flat together in their groups of three or four and this forms the basis of their study groups.
Students apply by letter through SONIA and applications are accepted from June. Applications close August
(August 22nd in 2021) and all applicants will be interviewed early in September and, if successful will be invited
into the programme by mid-September (Friday 17th September in 2021). Applicants will indicate their order of
preference for regional teaching centres and allocations will be made by early October (Friday 1st October in
2021). It has been noted that even though students don’t always get their first preferences they still enjoy the
programme in the localities they are placed.
An ex RMIP student reported back
“I feel like I developed as a person and professionally immensely. While
studying/working in my RMIP year I always felt like a valued member of the team & dealt one on one with
senior staff members (consultants), house surgeons, GPs, nurses and other hospital staff a lot more than I
would have in a main centre. I was often asked about what I thought about a situation/patient & including in
decision making while at the same time being very well supported. We received multiple tutorials/on the spot
teaching from our senior colleagues however the majority of our study was self-directed”.
Dr Branko Sijnja, RMIP Director
Email
[email address]
RMIP Administrator
Email
[email address]
How to apply
https://www.otago.ac.nz/dsm-gprh/rmip/otago740077.pdf
39
Options for TI Year
Although most students continue on to TI year at the same campus where they were for ALM4/5,
there is the possibility of transferring to another campus within OMS, or even transferring to the
University of Auckland Medical School. Students can also opt to do their whole TI year in Invercargill or
Timaru.
An email is sent to all students early in ALM5 (usually Feb/March), inviting applications through
written submission to, and interview with the Associate Dean of Student Affairs. Students are
informed of the outcome of their application by mid-April.
Transfer between campuses of OMS is only possible if space is available in the campus you wish to transfer to.
For transfers between OMS and Auckland the following criteria need to be met:
a. a one to one exchange of students can be arranged
b. the student has achieved a standard of performance acceptable to the Academic Board;
c. the Academic Board is satisfied there are special reasons for the student to transfer
d. the University of Auckland has sufficient resources and facilities to accept the student.
Note: Students transferring from Otago to Auckland will graduate with the Otago MB ChB degrees.
Please feel free to contact the ADSA if you would like further information about this process.
TI Year Elective
For the foreseeable future, TI Electives will need to be NZ based (usually within the OMS region). If
you are in 1st Quarter for Elective, this will need to be planned during 5th Year.
Elective placements available are dependent upon resources and timetabling. These are published
on the SONIA database. You will receive further information about applying for Elective placements
during 5th year, including instruction on how to use the SONIA database.
40
Research Opportunities
Summer Studentships
The main objective of the Summer Studentship Programme is to give undergraduate Medical and
Science/Social Science students an introduction to research. The programme provides students with the
opportunity to work within an excellent research environment and to mix with researchers and post-graduate
students who are working at the forefront of their fields. Students become familiar with a complete research
experience, from project planning and data collection through to reporting results in a public forum.
Research is the fundamental cornerstone of all aspects of clinical medicine. Many summer students eventually
go on to take up a career in research (some senior researchers gain their first taste of research as a summer
student), whilst others acknowledge that their exposure to the rigors of research enriched their degree and
honed their critical thinking ability.
An educational grant of $5,000 is paid to students accepted into the summer studentship programme. The
programme is open to any Medical and Science/Social Science undergraduate student currently enrolled at
any New Zealand University. Projects with funding are supervised by staff members from all campuses and
associated institutions.
Our hope is that the experience will result in many students being sufficiently excited by research to make it
an important part of their careers.
If you are interested in applying for a Summer Studentship, contact:
Dr Manon Knapen
Health Sciences Division
PO Box 56
Dunedin 9054
Website
: https://www.otago.ac.nz/healthsciences/research/summerscholarships/dunedin/index.html
Bachelor of Medical Science with Honours (BMedSci(Hons))
If you would like to become more seriously involved in research you do not have to wait until you are
qualified. You can take a year out to do a Bachelor of Medical Science (Hons) – the details are in the University
Calendar and we can also put you in touch with other BMedSc students. This involves a thesis and there is a
good chance that you will be able to publish your results in an internationally recognised scientific journal. You
will also be in a strong position to follow on with an MMedSc or PhD at a later date. Research experience not
only looks good on your CV, but also will give you a more critical and informed approach to medicine. If you
might be interested in undertaking a BMedSc please make contact wi
th Mrs Jillian Tourelle (479 7700) o
r Ms
Jacqui Bradshaw (470 9776)
Further information available on the Otago Medical School website:
http://www.otago.ac.nz/courses/qualifications/bmedschons.html
Intercalated MB ChB/PhD
It is possible in exceptional circumstances for a medical student to upgrade from a BMedSc(Hons) into the
intercalated (combined) MB ChB / PhD. This involves taking further time out of the MB ChB programme to
complete a higher level research degree interspersed within the undergraduate medical qualification. This is
a highly demanding course of individual study available only to the most motivated students.
Approval to enrol for this option is granted on a case-by-case basis. For further information or to make an
appointment to discuss the possibility of undertaking an intercalated PhD, please email
[email address].
Please note: this PhD should not be confused with postgraduate doctoral degrees, the PhD and MD, which are
managed by the Graduate Research School.
41
Student welfare and services
Student Affairs
Location: Otago Medical School Adminstration, Sayers Building
The Student Affairs office is headed by two Associate Deans’ for Student Affairs (ADSAs), Dr Penny Eames and
Dr Tess Patterson. Although Dr Eames mainly sees ALM students, and Dr Patterson ELM students, there is
some cross-over. They are responsible for all student matters relating to your personal, academic or pastoral
care and are assisted by the Manager of Student Affairs, Jillian Tourelle. Jill is also able to assist and guide you
in these matters and refer on as appropriate. The responsibilities of the Student Affairs Office include matters
such as leave of absence, progress and assessment, final year electives, coordination of the sixth year
programme, OUMSA activities and coordination of timetables.
Appointments to see the ADSA can be made via Erin at
oms.studentaffairs@otago / 479 7420.
Medical Education Unit
Location: Otago Medical School Administration, Sayers Building
The Medical Education Unit (MEU) is involved in the planning and administration of the curriculum for
medicine, years 4 – 6 . You are welcome to contact members of the unit about curriculum/ education matters,
and general course information. You can do this either as an individual, or via your class reps.
Relevant staff you may contact include:
Associate Professor Ralph Pinnock (Director, Medical Education Group and Associate Dean,
Undergraduate Education)
Dr Kristin Kenrick (Deputy Associate Dean Medical Educatiion, Whole Class Learning Week Convenor,
Y4 Urban General Practice Module Convenor.)
Dr Steve Gallagher (eLearning Facilitator)
Dr Megan Anakin (Education Advisor)
Ms Angela King (Administrator Client Services, 4th & 5th year).
MEU provides:
Assistance to the Dunedin Campus with curriculum planning, development, and logistical support
Curriculum and educational support to 4th, 5th and 6th year students
Course evaluations
Invercargill and Timaru travel reimbursements (Years 4 and 5)
Teaching staff support and development
Input to OMS initiatives on course development
Reporting Concerns:
MEU staff are involved in regular meetings with student representatives. You can bring any concerns or
suggestions about curricular matters to us through them or directly.
Student Affairs, across the three campuses, has been working with our IT experts to get a new Moodle ‘Student
Support’ page up and running.
The page includes some brief information about Student Affairs, some wellbeing resources (at the moment
links to other sites), contact information, and a link to be able to report concerns about intimidating behaviour
in the learning environment.
We very much welcome any comment about suggested developments and resources that people have found
useful that we could link from the page.
42
The issues of reporting intimidating behaviour and implementing the informal reporting mechanism
recommended by a workshop of students and staff, were what drove this development initially. The document
endorsed by the Otago Medical School Executive is on the page, as is a link to a reporting form. When someone
submits a form, an email goes to Student Affairs who collate the forms and pass them on to the newly formed
Behavioural Assessment Team for discussion about action. We will email students regularly to remind them to
use the reporting form if incidents of concern have occurred. You may choose whether to put your name,
email, or student group on the page. These details would allow some feedback to you on what action was
taken.
The reporting form is housed outside of Moodle and is confidential and secure – it is not linked to your identity
in any way unless you decide to include your name or other details.
Support for students is always available from Student Affairs. Just get in touch using the contact details on the
page.
Also on the page is a link to announcements on student support and wellbeing. We hope as time goes on to
use this more and more to tell students about support and wellbeing initiatives and information.
Feedback is welcome!
Concerns can also be raised directly with your Module Convenor or through the Staff-Student Liaison
Committee (SSLiC) via your Class Rep or OUMSA Reps
Otago University Medical Students’ Association Inc (OUMSA)
In order to cater for ALM students’ needs, OUMSA’s structure has changed to include an ALM Exec:
President: Madison Hutton
[email address]
Vice President: Jack Forsythe
[email address]
Education Officer: Kelsey McNabb
[email address]
Social Officer: Emily Seddon
[email address]
Welfare Officer: Kate Saunders
[email address]
TI Education Rep: Harshith Kondakindi
[email address]
5th Year Education Rep: Jake Ward
[email address]
TI Social Rep: Marieke Kruiswijk
[email address]
5th Year Social Rep: Kate Emett
[email address]
TI Welfare Rep: Georgia Hoten-Walker
[email address]
5th Year Welfare Rep: Renne Ashton
[email address]
The New Zealand Medical Association (NZMA)
NZMA is the only doctors’ organization that represents you at every stage of your career, and in whatever
medical specialty you choose. The NZMA is a strong and effective voice in national health and social policy
issues. Our advocacy is heard and does make a different.
The NZMA is a strong supporter of medical students and works closely with the NZMSA. We sponsor student
events and activities including career evenings, conferences, workshops and projects. Most importantly, we
listen to and express issues such as education and training, the medical workforce pipeline and government
health policy. Our advocacy aims to ensure that the environment in which you learn, train and work benefits
you and the health system as a whole.
You are an NZMA member through your NZMSA and OUMSA membership. The NZMA represents the doctors
of tomorrow, today. As a member, you are helping to shape your future as a medical professional, project
your career investment and ensure your voice is heard. NZMA members are part of a professional community
of doctors. During your studies, through graduation and beyond, we are here to represent and support you.
Please refer to our website for further information:
nzma.org.nz.
43
Class representatives
It is the hope of the Faculty and OUMSA that you feel well represented and have multiple channels to give
feedback and be engaged with the medical school. Each year level has an Education representative who is
elected on an annual basis, and they (along with the Education officer) meet roughly fortnightly with the
faculty to discuss any issues and to ensure feedback makes it to the relevant parties. More importantly, as
each year a group of students is divided into four groups for administration purposes, each of these groups
should nominate 2 “SSLiC Representatives” (SSLiC = Staff-Student Liaison Committee). The main role of the
reps is to facilitate the flow of communication between the group, the rest of the class, the reps in the years
above and below, OMS and vice versa. SSLiC Reps meet with key faculty members monthly and the School
values their input. The quality of feedback to and from students is greatly influenced by the class reps and this
will become more important as curriculum and assessment changes are considered.
Students with impairments
If you have a permanent, recurring or temporary impairment that may affect your study please let the Student
Affairs Office know, as wherever possible they will try and meet your needs.
In addition, the staff at Disability Information and Support provide learning support, advice, advocacy and
information to students with permanent, recurrent or temporary impairments. More information is available
on request a
t [email address]
International student support
The University’s International office provides a wide range of support to international students. They can be
found in the Archway West Building or contact
[email address]
Māori Centre – Te Huka Mātauraka
https://www.otago.ac.nz/maoricentre/index.html
The Maori Centre is a support service for all students of iwi descent. The Centre also aims to encourage Iwi
Māori to participate and succeed in tertiary education. The Centre offers support for academic, cultural and
social needs from pre-enrolment through to graduation and operates from a kaupapa Māori base (Māori
philosophy).
Pacific Island Research & Student Support Unit
https://www.otago.ac.nz/pirssu/index.html
The Pacific Islands Research & Student Support Unit (PIRSSU) currently looks after approximately 500 Pacific
students from New Zealand and the Pacific region studying in the Division of Health Sciences. We offer
excellent training in health professional and allied health programmes, nurture successful research careers,
and offer quality pastoral care in an inclusive cultural environment. We look forward to welcoming you to our
Pacific community in Health Sciences.
Student Health Services
https://www.otago.ac.nz/studenthealth/index.html
Student Health is centrally located on campus in a purpose-built facility. We have approximately 50 staff,
comprising nurses, general practitioners, counsellors, psychiatrists and administrative staff.
We endeavour to provide the best health care possible in a manner that is competent, compassionate,
confidential, timely and in an atmosphere of mutual responsibility and respect.
We provide daily urgent and routine appointments. If patients need to be seen in our urgent daily clinic they
will always be triaged (phone call or face to face) by a nurse before being booked an appointment with a health
professional.
44
Consultation fees do apply (details are available on our website) and charges are reduced with a Community
Services Card (CSC).
The Dunedin Urgent Doctors and Accident Centre is available for after-hours emergencies. Higher consultation
fees apply for after-hours services.
Emergency Psychiatric Service at the Dunedin Public Hospital provides urgent mental health care 24 hours a
day.
Please refer to our website for services/charges
45
Working in a Clinical Setting
Chaperoning
It is necessary to consider the desirability of a chaperone when patients are being examined or interviewed.
This is especially true if the patient is of the opposite gender, a child or otherwise disadvantaged.
Chaperoning during consultations when a staff member is present is the responsibility of the member of staff.
A patient should always be asked if they would prefer the consultation to take place with a chaperone present.
Students should arrange with a colleague of the opposite gender in their group, to accompany them if they
wish to examine or interview a patient (to ensure protection of both student and patient).
More specific guidelines are as follows:
Adult Patients
In principle, chaperones should always be used when students are undertaking consultations on
members of the opposite sex.
If a chaperone is not readily available the patient should be asked whether they prefer a chaperone
to be present. If so, the consultation should not proceed until a chaperone is available.
In all circumstances, but particularly when a chaperone is not present, the nature of the examination
to be carried out should be explained to the patient and verbal consent obtained to proceed. It is also
useful to explain the steps in the examination process to the patient as the examination proceeds.
If a chaperone is not available for the whole examination it is useful to have a chaperone check
periodically that all is well.
Persons eligible as chaperones may include medical students, nursing staff of the opposite sex, or
some other appropriate person, if consented to by the patient.
Any problems which cause difficulty, concern or embarrassment during the consultation should be
reported to the Associate Dean for Student Affairs.
Children
Consultation with children of the same or opposite sex should in principle always be done with a
chaperone present.
In circumstances where a chaperone is completely unavailable the consultation should take place in a
relatively open setting (ie not behind completely-closed curtains).
If there is any suggestion from the patient that there may be a matter for complaint this should be carefully
recorded in the patient's notes, signed and witnessed. This should also be reported to the Associate Dean
Student Affairs.
Dress and appearance
It is appropriate here to reiterate the importance of suitable dress, not only in the School and on the wider
hospital campus, but particularly in the patient areas. At all times appearance is likely to be one of the ways
by which people in the hospital assess the School, and must meet the standards that your patients expect.
Appropriateness to clinical work must always be considered and is part of the requirement of your continued
honorary staff status with any District Health Board.
You reflect on dress expectations, whether your own dress fits the work of clinical students and the required
respect for patients. If in any doubt, please talk to your colleagues or the staff on your attachment. Members
of staff may expect conformity with particular standards within their departments and will discuss dress with
students should they deem it necessary.
46
Culturally-sensitive issues
Students are required to participate in all laboratory, practical and clinical activities, which includes activities
that may not be usual to your culture. In the professional classes, some aspects of the teaching will require
individuals to practice certain techniques on each other, which may require you to partly undress and may
involve body contact between students. Training is done under close supervision and all students are required
to participate, as it is essential for their acquisition of clinical skills. Assistance from students experiencing
difficulties in this area is available, on request, from the relevant Campus.
Dress requirements in theatre
Specifically, in disciplines such as surgery, medical students will be required to conform to standards
of dress that meet the high levels of hygiene in operating theatres. Personal garments, such as
headgear worn outside the theatre situation, must be replaced by alternative sterilised garments
provided by the hospital to meet accepted standards of infection control and asepsis. Students must
also adhere to the stringent protocols of scrubbing to involve hands and both forearms to at least
elbow level.
Professional behaviour: General
Remember, it is part of the requirement of your continued status with health providers that your
behaviour towards staff and patients is always of the highest standard. Please remember to show
consideration to others around the hospital, in lifts and other public places. You are easily recognised
as students, and people look to you to show a good example.
Professional etiquette and practical ethics for clinical education (teaching, learning & assessment)
The Medical School, hospital, and community providers aim to provide medical students with a
welcoming learning environment, and to encourage clinical staff who teach medical students
(supervising clinicians) to act as role models for professional behaviour and professional practice.
The following guidelines outline the general policy on the standards to be observed in clinical
education. They are to be read in conjunction with the policies and procedures of host institutions,
the University of Otago's Ethical Behaviour Policy, and the provisions of the Code of Health and
Disability Services Consumers' Rights as well as of the Health Information Privacy Code.
Patient rights in general
A patient has the right to be explicitly informed about the specific education activity in which the
patient may be participating. The supervising clinician is responsible for informing the patient about
education activities, in particular about any procedures in which a medical student may participate
under supervision.
Consent for clinical education
The patient's welfare and interests are always the overriding consideration. Patients are typically
generous in their willingness to support medical students' learning and often themselves benefit
from the process. Consent for clinical education obviously involves an element of permission but it
also extends to assisting patients to understand why a particular learning/ teaching activity is
valuable.
The following points address these aspects:
Patients must be informed that they may be involved in students' learning
Patients have the right to choose, or to decline, to be interviewed, examined or cared for by a medical
student, or to be involved in any other way in medical education
Patients have the right to know the name and professional standing of any person, staff or student,
who wishes, for teaching purposes, to interview them, examine them, or carry out any procedure
Patient consent for clinical education must be obtained by the supervising clinician (or other staff
member). This should be done in a setting out of sight of the student(s) to avoid placing undue
47
pressure on patients. Patients have the right to withdraw from the clinical education activity at any
stage and may change their mind between consent with the supervising clinician and subsequently
seeing the student.
In the case of children, their parent, guardian or other legal representative may, on their behalf, make
the decisions and receive the information summarised in the above four bullet points. Competent
children may consent or decline on their own behalf.
Patients of diminished capacity or children who have yet to attain full competence have the right to
be informed and to be involved, to the extent to which they are able, in any decision to participate or
not.
Where appropriate, an oral consent obtained should be recorded in the patient's notes; a written
consent should be documented in the notes.
If a patient is not competent to give a consent, consent for clinical education should be obtained from
the same person who gives consent for interventions on behalf of that patient.
Medical students should wear their name badge and carry their ID card in all clinical settings. When
introducing themselves to a patient by name, they should explain that they are a medical student,
confirm that the patient is willing to proceed, and seek an explicit permission on each occasion a
consultation is needed.
Medical students who are observers or who undertake examinations under supervision or who assist
with procedures under supervision while a patient is sedated or under general anaesthetic are
required to meet with the patient beforehand and, with assistance from the supervising clinician as
appropriate, obtain a written consent. Where a genital examination is performed by a student(s) while
the patient is under general anaesthetic, at most two students [who have obtained prior written
consent] may do so.
Medical students should be aware that the standard consent procedures may need to be abbreviated
or waived in emergency situations.
Clinical examination of patients
Most patients will have been advised that they should expect to be approached to assist in the clinical
education of medical students. However, students should note that they do not have an absolute right to
examine any patient. When you commence a new clinical attachment check with your tutor or supervisor on
the procedure to be followed in approaching patients. This may vary slightly according to the clinical discipline
involved.
In general, if you have been allocated a patient, or patients on one of the modules, you should:
Introduce yourself and obtain the patient's consent to interview and examination
Be cognisant of racial and cultural sensitivities
Sensitive examinations (includes breast, rectal, vaginal examinations, and those of the external genitalia) in
competent awake patients require explicit consent, which must be appropriately documented.
It is essential that there should be no possibility for the consent to have any element of coercion (e.g., it may be
harder for a patient to refuse if the patient is asked after undressing or in front of a student).
Sensitive examinations under anaesthesia require formal written consent obtained in advance and signed by
the patient. It is essential that there should be no possibility for the consent to have any element of coercion
(e.g., asking in front of a student may make it harder for a patient to refuse). Without such consent a student
cannot undertake such activity.
48
Professional behaviour: Supervision
A supervising clinician is expected to brief medical students about their role in patient care. Often this will
already be known (for example some issues are spelt out in this handbook), but if it is not clear, or the
requirements of a particular context are different from usual, medical students are encouraged to seek explicit
guidance about what is expected of them, paying particular attention to the following:
Dress code: Any requirements to be observed or avoided
Introductions: Any particular style, especially if the medical student's relationship to the team needs
to be made explicit
Accountability: Who is responsible for the medical student(s) and who is able to deal with queries and
concerns
Emergencies: Any procedures medical students are expected to observe in the event of an emergency
Standard precautions: Medical students will need to be warned of situations in which there are
particular infection control issues and advised of the appropriate precautions to observe
Risk of violence: Medical students should be given prior warning of patients with a known history of
violence with adequate briefing on protocols for ensuring personal safety
Chaperones/support persons: Medical students should be given guidance as to when a child or adult
should be offered a chaperone/support person and who may appropriately serve in that capacity
Boundary issues: Medical students should be advised of any clinical settings in which there is special
reason to maintain robust professional boundaries
Debriefing and reflection on clinical and professional development: Medical students should be
encouraged to seek, and be offered prompt opportunity for, debriefing after significant critical
episodes, and opportunities to reflect on what they have learned, how they are learning it, and their
development of professionalism.
Ethical issues: Medical students benefit from the opportunity, whether initiated by staff or students,
to discuss ethical issues generated by a specific case or experience.
Medical student rights
Medical students have the right to decline to participate in clinical teaching/or patient care if there are
concerns, ethical or otherwise about the activity; concern about their own competency, lack of knowledge, or
lack of understanding of the duties/tasks/responsibilities involved; or conscientiously believe there is a lack of
explanation or supervision.
49
Privacy and Confidentiality
Medical students are expected to observe the same high standards of confidentiality and respect for privacy
as govern the behaviour of all doctors and healthcare professionals. These standards are set in the Privacy
Act (2020) and the Health Information Privacy Code (2020) (The Privacy Code or HIPC).
The Privacy Code outlines specific rules regarding the collection, storage and disclosure of health information
in relation to identifiable patients. The basic rule is that no information about any patient should be given to
any other person without the permission of the patient concerned. This applies to all health information and
not only to that which the patient might regard as particularly sensitive. It applies to the simple fact that an
individual is a patient in the hospital or GP rooms as well as to details of their condition. It also includes
situations such as reports to lawyers, NZ Police, ACC and various other statutory bodies. There are some
limited and specific exceptions where disclosure of information without the consent of the patient is
permitted or authorized by law and you will learn about these over the next years of your training.
It is important to remember that patients share information with health professionals within a relationship of
trust and in order to assist the professional to help them with their health problem. Respecting that trust and
maintaining respect for privacy and confidentiality is fundamental to the doctor-patient relationship and
achieving the best outcome for the patient.
Access to notes and handling of written material
Students should only access patient notes with the consent of the patient and where the patient is under the
care of the team to which the student is attached. Notes of patients not under the care of the team should
not be accessed except where the student has an alternate legitimate reason to do so and has specific consent
from the patient.
Official patient hospital records must never be taken away from the clinical areas or out of the hospital.
Photocopying of patient notes by medical students is not permitted in any circumstances. Material written by
students which may contain patient-related information (eg case histories) should not have any ‘unique
identifiers’ (eg name, date of birth, address or national number). If these notes require work outside the
hospital (eg library) great care must be taken to ensure they remain secure and private. Once patient related
notes are no longer required they should be disposed of in a secure fashion in one of the bins provided by the
SDHB.
In addition to legal restraints around patient related health information, students are required to discuss any
matters referring to the Dunedin Campus and SDHB with the Dean BEFORE disclosing information to outside
agencies or bodies.
The following points should be also kept in mind:
Medical students should refrain from giving a patient a blanket guarantee of confidentiality, as this may
contravene their accountability to their supervising clinician. Whether information is acquired at interview or
from the clinical record, patients have a right to know the use(s) that will be made of the information [written
assignment, oral presentation to a tutorial group, one to one discussion with a tutor, etc], and what steps will
be taken to assure the privacy of the information [such as de-identifying]. Medical students should make sure
when, if at all, a copy of an assignment should be placed in the patient's notes, and patients should be informed
of this
Medical students should be meticulous in assuring the security of written assignments and other notes relating
to patients, even if de-identified, and should regularly dispose of material which has passed its use by date
through an approved destruction process.
Care should be taken to ensure that discussion of a patient for clinical education takes place in a secure setting
where what is said cannot be overheard by others and where there is thus no risk of what is discussed being
mis-interpreted.
Under no circumstances is a medical student permitted to take photographs of a patient or patient
information, or to make any video or audio recording of any interaction with or observation of a patient. If
50
photographs or recordings are needed for educational purposes, they will be sought by the supervising
clinician using current protocols.
Release of Information
Various pieces of legislation including the Health Information Privacy Code and Health Act, outlines
circumstances where personal details may be released without the consent of the patient or their
representatives. The Privacy Act does not apply if release of information is required under other legislation.
For example, the notification of infectious diseases is required under Section 74 of the Health Act.
Medical students must not release any information under these provisions without first consulting the senior
clinician working in this area. Students who make unauthorized disclosure of personal health information will
be subject to disciplinary action, and may also be in breach of the Privacy Act and the Health Information
Privacy Code.
Students are required to consult with the Associate Dean of Student Affairs BEFORE disclosing information
about the School or any of the DHB institutions to the news media.
51
School Buildings and Facilities
Fraser Building
You can use the Common Room, computer and study room and lockers available on the first floor of the Fraser
Building as well. This facility is open to all medical students from years 2–6.
Access to the Fraser Building will be via your hospital swipe card into that wing of the building, and then use
of the access code into the locker room and/or study area. The access code will be given to you at orientation.
This number must not be given out to anybody other than second-to-sixth-year medical students. This is for
your own security. Please ensure that this door is always locked behind you.
This common room has some lockers available, together with an adjoining room with tea and coffee making
facilities, a microwave and a fridge. Tea towels and washing up liquid will be provided. There is also a space
next door with chairs/space to study and a bathroom, complete with shower available for your use.
We recommend that you do not leave your valuables around, including stethoscopes etc, which tend to
disappear from time-to-time. Keys for the lockers will be available from Monday to Friday between the hours
of 9am–3.30pm, from OMS Reception, Sayers Building, at a cost of NZ$10 per key, on a first-come, first-served
basis. All keys must be returned to OMS Reception at the end of each academic year. There is no refund when
the key is returned.
I would be grateful if you would please ensure that you leave this room tidy at all times—this is your
responsibility. Please be aware that use of this facility is a privilege and not a right. Inappropriate behaviour or
abuse of the area will not be tolerated. Please advise the Student Affairs Office (03 470 7700) if you are
experiencing any problems with either of these common rooms.
Otago Clinical Skills Lab (OCSL)
The Skills Lab is situated on the top floor of the Fraser Building. It is funded by contributions from HealthCare
Otago, the Otago Medical School, and the Otago Polytechnic Department of Nursing and Midwifery. The Lab
is a venue split into four specific areas:
Clinical area
Hospital room
Clinic rooms (SECO and Ambulatory)
Tutorial room
All rooms are utilised by clinical students of the Otago Medical School and the Southern DHB for teaching and
practising of a variety of clinical skills and group simulation work. All areas are individually booked and booking
enquiries are made through the Medical Education Unit Administrator, or the OSCL Operations Manager, Paul
Medeiros.
The OSCL Operations Manager has the authority to actuate and confirm all bookings.
The operating hours of the Lab are Monday–Friday 8.30am – 4.30pm.
Contact Paul Mederios
: [email address]
General computing information
Moodle
Important information on your ALM4 and ALM5 years will be placed on Moodle. Please log on frequently:
[email address].
IT Help
Your first contact for assistance should be Ask Otago IT Support:
[email address]
Tel: 03 479 7000
ASK Otago IT will attempt to solve your problem over the phone.
52
Health Science Library
The Health Sciences Library, a branch of the University Library, is currently located on the first, second and
third floors of the Sayers Building (opposite Dunedin Hospital's main entrance in Great King Street). See
otago.ac.nz/library for information about the University Library.
Electronic resources
The University Library licenses access to a very large collection of databases, electronic journals and e-books.
These can all be searched from the Library's home page otago.ac.nz/library. If you are searching from off-
campus (including Dunedin and Invercargill Hospitals) you will need to authenticate with your university
username and password.
For access to key resources take a look at your Subject Guides: otago.libguides.com/medicine
Note that some resources are available via mobile devices. District Health Boards have their own library
services to which you will also have access.
Opening hours (note these may change in 2021 and with COVID)
Semester: 7am–11pm every day
Summer School: Monday–Friday 8.30am–10pm; Saturday 11am–5pm; Sunday 11am–9pm
Non-Semester: Monday–Friday 8.30am–5pm; Closed on weekends
See otago.ac.nz/library/hours/ or Library notice boards for variations and changes to opening hours.
Information and Research Skills
Through the Subject Librarian Service the library offers a range of support for individuals, small groups and
whole classes.
Contact your Subject Librarian to make an appointment (see otago.libguides.com/liaison/healthsciences).
When you are out of Dunedin for an attachment (e.g. in Invercargill), you are technically a Distance Student.
You still have access to the Library's electronic and print resources, and can have books and journal articles
sent to you through the Distance Library Service. See otago.libguides.com/distance for information on this
service.
Borrowing material
Loan Periods
Books and journals (print): 4 weeks with 3 renewals
o You can renew non-Reserve books through the My Library account link from the Library home
page otago.ac.nz/library
Reserve Collection: 2 hours during opening hours
o This material may be booked in advance and renewed if not required by another borrower.
Overdue fines (note that these may change in 2021):
Reserve Collection: NZ$0.10 per minute
Recalled Items: NZ$3.00 per day
Please note that we do not accept cash at the Library, you can pay fines using eftpos, or online.
Document Delivery Service
Items which are not held in the Library may be requested at no charge (except for loans from outside
Australasia). Apply through the ‘Get it’ Document Delivery Service.
See otago.ac.nz/library/interloan.html
Students with Impairments
There is a small study carrel – the Lee Gibson Room – available in the Health Sciences Library for students with
an impairment. Bookings must be made through the Disability and Information Support Office. Special
53
equipment can be made available to Health Sciences Library users through the Disability and Information
Support Office as required. See www.otago.ac.nz/disabilities/.
Please let Health Sciences Library staff know if there is any way that we can assist.
Health Sciences Library Contact details
Service Desk/Renewals [03] 479 7401
Document Delivery Service [03] 479
Health Sciences Librarian [03] 479 7403
Subject Librarians [03] 479 7407, [03] 479 7237, [03] 479 7459
Email [email address]
Twitter twitter.com/otagolibrary
Facebook facebook.com/UniversityofOtagoLibrary
54
Southland Hospital Invercargill
ALM4 Medicine, Surgery, Urban GP*
ALM5 Women’s and Children’s Health, Musculoskeletal Medicine
Arrival
On arrival, please come to the Main Entrance Public Car Park of Southland Hospital. Directly on your right after
entry into the Hospital is the Security Office where you will find your Welcome Pack. If there is no one at
Security please ask at the adjacent Emergency Department and they will contact security staff. Security staff
will issue you with your Doctor's Residence room keys and give you your Welcome Pack which will contain the
paperwork Southern District Health Board requires you to complete, a map of the hospital campus and details
for reporting for your first day. Free single accommodation is available to Trainee Interns at Southland Hospital
however, there is no married accommodation.
Download a printable copy of this map (PDF 140 KB)
Travel arrangements
You will need to liaise with the Module Administrator about travel arrangements to Invercargill. You will be
reimbursed for one return trip from Dunedin to Invercargill, unless you are required to return to Dunedin
during the module by the Module or OMS.
Please ensure you arrive in Invercargill on the evening before your attachment begins, and follow the
instructions in this document regarding obtaining and signing for your room key. If you are staying for the last
weekend of your attachment, please ensure you let Ms Karen Erdman, Accommodation Officer, know this.
You will then be responsible for ensuring the room has been left clean and tidy, and the bed made up with
fresh linen for the next person arriving on the day you leave. This is your responsibility.
Orientation
On the first morning of your attachment please report to Madge Storm, Study Hub, Research and Learning
Centre, at 8.45am for orientation. A map to her office is included in your welcome pack.
Students on the Urban GP module will have additional orientation arranged by Invercargill-based teaching
staff.
Contact details:
Madge Storm, Administrative Assistant
Study Hub, Research and Learning Centre
University of Otago, Southland Hospital, Kew Road, Invercargill PO Box 828
New Zealand
Tel: 64 (03) 218 1949 x 48212
Hours: Mon - Fri, 8.30 am - 12.15 pm Email
: [email address]
Instructions on how to get to the Study Hub will be in your Welcome Pack. After completion of paperwork
Madge will take you to orientation as required.
Library: Barry O’Callaghan
Infection Control: Jane Miedema
Medicine Department:To be advised
Surgery Department: To be advised
Obstetrics and Gynaecology: Lynley Pascoe / Annette Calder / Olwyn Thwaites
Paediatrics: Karen Anderson / Michelle Cools
RMO: Clair MacGregor
Accommodation Officer: Karen Erdman
55
Associate Dean (Southland)
Associate Professor Konrad Richter
Tel: 03 218 1949
Email:
[email address] OR [email address]
Should you need to see A/Prof Richter appointments can be made through the Administrative Assistant,
Madge Storm.
A/Prof Richter meets with the students at irregular times throughout the year. These meetings are usually
informal and with other students and are an opportunity to feed back any issues regarding your time in
Invercargill. These meetings are usually very productive and result in change where this can be achieved.
The Associate Dean's office is also in the Study Hub.
MRSA clearance
MRSA clearance is not required for students going to Invercargill unless:
You have a skin condition
You have had a previous positive MRSA test
ID / access cards
Southland Hospital has stringent access control measures in place across the campus.
It is important that you take your Southern District Health Board Identify Card with you; your Southern District
Health Board ID will be loaded onto the Southland Hospital security system on or before your arrival and will
be your means of identification and access during your placement.
Photocopier and Southern District Health Board computer use
The Southern District Health Board has no tracking on their copiers at present, so there are no copying charges
or restrictions on copying other than (1) those inherent in the Copyright Act 1994, and (2) an expectation that
only health study related copying will be done. Southern District Health Board computers are provided for
business purposes only, which includes study. Users must comply with the Southern District Health Board
policy Internet Use, copies of which can be found on Library notice boards.
Car parking
Parking is provided on the east side of the Doctors' Residence (gravel car park).
Students are not to park in the main public car park 8am–5pm Monday to Friday, or at any time in the Hospice
car park.
Library
The Library is situated across the car park from the main hospital in the Community Services Building. 24-hour
access to the Library is available with your swipe card. Entry is via the proxy card door / staff only entrance to
west side of Community Services Building. The Library is Reference Only at weekends, from 5pm at night to
8am the next morning, and very occasionally during normal working hours if the Library staff are absent.
Library users should present themselves at the Help Desk for assistance and to have books, etc, issued.
The loan period is three weeks and all loans must be returned to the Southern District Health Board Library
before students leave Southland Hospital. There are University of Otago PCs in the Library, one with a CD
burner and a University of Otago printer. The Library is a 'Quiet Zone'. It would be appreciated if phone calls
could be taken and made outside of the Library.
Barry O’Callaghan (Assistant Librarian) and Jeremy Andrews (Library Assistant) work in the Southern District
Health Board Library and look forward to meeting you. Please do not hesitate to seek their assistance if you
think they can be of help.
56
Dunedin Campus Computer Facility in Invercargill
Students will have access to computers in the Library, Clinical Services Building, Paediatric Department and
the Doctors' Residence. Please keep these areas tidy. Please take your pop numbers, passwords, etc, with you
regarding your own email to enable you to access and check it. Printing and scanning facilities are also available
in the library at no charge. Printing and scanning is also available in the Study Hub using your University ID
card.
Troubleshooting relating to the Dunedin Campus computers (apart from paper and toner resourcing) should
be through the University of Otago's Ask Otago IT Support
– [email address].
Madge Storm looks after paper and toner requirements in the Doctors Residence.
Computer help in Invercargill
For any further assistance the process is the same as if you were in Dunedin. The Invercargill computers are
remotely controlled by the Dunedin Campus ICT Support Group so we can often fix your problems quickly.
Doctors' Residence
An envelope containing your room keys and information about staying in the Doctors' Residence will be waiting
for you at Security with your Welcome Pack. The Doctors' Residence cannot be entered unless the correct
security code is used at the entrance door. This will be with your Room Key. Prior to leaving Dunedin you will
be asked to sign an agreement that you will abide by the rules of the Residence when you collect your key.
The Residence has three levels, each level with its own shared kitchen, ablutions and lounge areas. The ground
floor is generally used for on-call medical staff and fourth-year medical students. Trainee Interns are usually
on Level 2. DO NOT SWAP ROOMS DURING YOUR STAY, as rooms are planned out for the year. If there is a
problem with your assigned room please discuss with Karen Erdman. You room key must be returned to the
Security office when you leave. Failure to do so will incur a $25 replacement fee.
Each room contains:
Bed, mattress, and bed linen
4-drawer tallboy, wardrobe
Small study table, chair
Heating
Fresh bed linen and towels are available at all times; however all residents are responsible for cleaning their
own rooms. Vacuum cleaners are available. Residents are also responsible for keeping the kitchens, lounge /
TV areas clean and tidy. ISS clean the ablution areas four times per week. There is also a laundry and auto-
washers, tubs, and a drying room.
Kitchens are equipped with:
Electric range and microwaves
Fridge / freezer
Instant boiling water
Cooking utensils, cutlery, crockery, cupboards for food storage
No tea, coffee, milk, etc, is provided. Reasonably-priced meals and other snacks are available at the café in the
hospital. There is an expectation that you will keep the kitchens, lounge and your personal bedrooms clean
and tidy at all times. Cutlery and crockery must be returned to the kitchen areas and washed immediately
after use. Please also clean the ovens inside and out, microwaves and refrigerators, stovetops, inside and
outside microwave with cleaning products provided on a daily basis. When you leave throw out any unwanted
food items. Uncovered food items in the cupboards or on the bench will encourage mice.
Rules for the Residence
DO NOT CHANGE ROOMS, stick to your assigned room
Do not shift any furniture from the lounge, kitchen, or bedrooms
57
No bicycles are to be stored in the bedrooms
Turn off all taps
Wash, dry and put away all dishes immediately after use; do not leave them to "drip dry"
Clean out all refrigerators regularly
Wipe down benches, microwaves (inside and out), stove tops and ovens after each use.
Under no circumstances is cooking to take place in bedrooms or any other areas other than kitchens.
All bedrooms and corridors are fitted with smoke detectors, which are connected directly to the fire
brigade. Jug kettles are also not allowed in the bedrooms.
Please be considerate of other residents and keep the noise levels at a minimum between the hours
of 10 pm and 7 am.
At any time when the fire alarm sounds continuously all occupants are to evacuate the building. Failure
to leave a building when a fire alarm sounds may result in disciplinary action being taken. You are not
only endangering your own life but those of the response teams.
The Fire Service allow for two false alarm callouts every year; a NZ$1,000 invoice is sent to the Southern District
Health Board on the third. Should the cause of any callout be due to neglect then this invoice bill will be passed
onto the person responsible.
Evacuation board
When entering the Doctors Residence use status board to indicate your presence by sliding appropriate room
number to “IN”. When exiting Doctors Residence use status board to indicate your absence by sliding
appropriate room number to “OUT”. This is very important as if a Fire Alarm is activated Security and the Fire
Service know how many people are in the Residence.
Bike security
There are under cover bike stands available beside the Doctors' Residence. There is no enclosed locked area
available. Bikes left at any of the bike stands around the Hospital are at the owner's risk.
The Otago Medical School, Dunedin Campus and the Southern District Health Board have made a significant
joint investment in the provision of these facilities for your use. To ensure their continuing availability, the
Residence will be checked for cleanliness and damage on a regular basis. Failure to maintain the expected
standard of tidiness and basic hygiene will result in individual charges for cleaning and/or damage. You will be
required to sign a form indicating that you will abide by the rules of the residence.
Videoconferencing Room
The Study Hub has two AV rooms for your Zoom tutorials. Very occasionally these may have prior bookings
and you may have to do your Zoom session in one of the other rooms. If there are any problems with the link
to Dunedin please contact Madge or follow the help instructions nearby. It is important that you report any
problems or poor quality immediately. Dunedin Campus is committed to providing a good quality link so that
you continue to be involved in the Dunedin based teaching programme.
Zoom room
The zoom rooms and situated in the Study Hub. If there are any problems with the link to Dunedin please
contact Madge Storm, or follow the help instructions nearby. It is important that you report any problems or
poor quality immediately. The Dunedin Campus is committed to providing a good quality link so that you
continue to be involved in the Dunedin based teaching programme.
Contacts
Dunedin Lecture Theatre Technicians (Fraser Brown) - 03 479 7086 - or contact Fraser direct on 021 279 0740,
you may text during a presentation.
58
Complaints and/or concerns
If at any time during your stay in Invercargill you are concerned about anything in regards to the
course, personal or otherwise, please direct these issues to Madge Storm or contact the Student Affairs
Office at Dunedin Campus 03 479 7700/ emai
l [email address].
Timaru Hospital
Associate Dean (South Canterbury) and Administrator
The formal relationship between the South Canterbury District Health Board and the University of Otago
commenced in February 2013 with the appointment of the Regional Associate Dean & Administrator. The
scope of these positions includes all students from the Division of Health Sciences, University of Otago, who
are on clinical attachment in the South Canterbury region.
Maree Steel
Associate Dean South Canterbury
Associate Dean Student Experience
[email address]
027 2804846
Jehan Cunningham-Beynon
Administrator Client Services
South Canterbury
[email address]
03 687 2361
OTAGOHub
We have a dedicated University of Otago site “OTAGOHub” situated at 53 Edward St on the Timaru Hospital
Campus. This building is adjacent to our student accommodation on Queen Street. The site includes a study
room; teaching space; social space; University staff Offices; Networked computers to DHB clinical systems;
printing facilities, AV equipment; laptop; and hotdesk space.
Student Accommodation: 13A, B, C & D Queen Street, Timaru
The four flats at 13 Queens Street are leased by the University of Otago for students to use while in Timaru.
All flats are basic but fully furnished with linen provided, or you may wish to bring your own bedding. Each flat
has a sunny north facing courtyard and is opposite the botanical gardens and tennis court. They are also in
close proximity to the coastal walk. There are carparks available at the rear of the flats (one car park/flat). You
are also welcome to use the free parking facilities on Edward Street and High Street. With the issued staff
swipe ID you have 24/7 access to the Timaru Hospital Library just across the road and the OTAGOHub site next
door.
59
The West Coast
The West Coast District Health Board (DHB) serves 32,000 people. The region is 600km long (that’s about the
same as from Auckland to Wellington) and it takes 7 1⁄2 hours to drive from top to bottom.
What is the region like?
Website: www.wcdhb.health.nz
Some 84% of the land is national park or conservation reserve, containing such diverse features as palm
beaches, glacial landscapes, wild river gorges and thermal areas. It is also the sole source of precious pounamu
jade, prized by generations of Māori.
One of New Zealand's most beautiful, sparsely populated regions, the West Coast is known to Māori as Tai
Poutini.
Working and living on 'the Coast' offers a unique lifestyle. The spectacular native forests, mountain rivers,
lakes and sea coast offer outstanding recreational opportunities such as fishing, skiing, tramping, kayaking and
mountain biking.
Many West Coasters are engaged in primary industries such as mining, timber production and farming, while
the magnificent environment offers many outdoor recreational activities for locals and thousands of
international tourists.
Te Nikau, Grey Hospital and Health Centre
Contact Details
Postal: Te Nikau Hospital; P.O. Box 387 Greymouth
Phone: (03) 769 7400
Physical: Te Nikau Hospital; High St, Greymouth 7805
Special Reminder about Confidentiality:
It cannot be stressed enough how small the community is on the Coast. Most locals will know, or know of,
most other people and their family connections, hence confidentiality is of utmost importance. Remember
people are identifiable from their story NOT just their name.
Prior to travel to the West Coast
At least 10 working days before you are due to start your placement at Greymouth you must complete MRSA
testing (you will be working in another Hospital so need to be cleared before you can see patients).
You will also have completed a number of forms for the WCDHB: Immunisation History, a Personal Details
form, a Staff Appointment form, Health and Safety, IT Master form, and a Non-Disclosure form. These will
allow you to become a staff member at WCDHB for the period of your attachment, and give you access to
buildings, patients and information and computer systems.
A copy of your driver licence has also been sent to the WCDHB as you will need to drive to clinics and may also
be able to use a car in the weekend if one is available (you will need to pay for petrol though).
Transport to the West Coast
Your transport arrangements are made by the Department of Psychological Medicine well in advance of your
placement on the West Coast and you have been emailed your plane tickets and all details regarding transport.
You need to make your own transport arrangements to and from Dunedin Airport.
Tickets have been booked for you to fly Dunedin to Christchurch, then Christchurch to Hokitika on the day
prior to the start of your placement. There may be a period of waiting between flights at Christchurch airport.
It is your responsibility to ensure that you catch your connecting flight. Refer to flight tickets for details around
luggage.
60
On arrival at Hokitika you will take a shuttle to your accommodation.
Airport shuttle transfers have been booked for you with Greymouth Taxis. They will meet you off your inbound
flight.
The Department will be invoiced for the shuttle, so there is no cost to you.
Return to Dunedin is the reverse of travel to the Coast: shuttle to Hokitika airport, fly to Christchurch, connect
to flight to Dunedin airport. Please contact Greymouth Taxis (03 768 7078) the day before your departure
from Greymouth to check the pick-up time.
N.B. It is your responsibility to ensure you arrange the return shuttle, and catch your flights. You need to find
your own transport from Dunedin airport to your Dunedin accommodation.
Accommodation
Accommodation is in a single room at the Global Village Travellers Lodge. This is close to the Hospital (approx.
1km), and has a supermarket within walking distance. All bedding, towels and linen are provided and changed
regularly. The kitchen is large and fully equipped for either snacks, or a gourmet dinner. They have a large
modern laundry, and in the winter months, full central heating. There is also a fitness room, and lounge
areas/quiet spaces. You will be well looked after by Russell, Yuri and Simon.
You are not required to pay for your room but you will be responsible for any food or miscellaneous costs. You
can read http://www.globalvillagebackpackers.co.nz/
Contact Details
Global Village Travellers Lodge; 42 Cowper St, Greymouth
Phone: 03-768 7272
Clinical Placements
Dr Heather McPherson is the Clinical Director for Mental Health Services.
The medical secretary will arrange your timetable for your placement on the Coast.
You will meet Ingrid Dugand at the Mental Health Service reception for orientation to the service and to meet
staff members.
Contact Details
Ingrid Dugand, Management Secretary
Leeanne Hine, DAMHS Administrator and IPU Medical Secretary
Mental Health Services, WCDHB
P O Box 387, Greymouth 7840
Phone: (03) 769 7400 extn 2518 / 2629 [email address]
Dr Andrew Gin, Clinical Tutor
[email address]
Juliette Reese
Coordinator / Administrator Medical Training Programmes
Rural Learning Centre, WCDHB
PO Box 387, High Street, Greymouth Phone: (03) 769-7400 extn 2470 [email address]
Personal cell: 027 2332715
Julie Wallace
Clinical Nurse Manager [email address]
61
Facilities
The Rural Learning Centre (RLC)
The RLC is a suite of rooms located in the hospital grounds. The concept of the centre is to provide an
environment which fosters multidisciplinary learning.
The End Flat (closest to the old hospital) of the Rural Learning Centre consists of:
The Teaching Room
The office where Juliette Reese is located.
Nurse Manager - Workforce Development.
The Teaching Room facilities include:
TeleHealth/TeleMedicine (video conferencing system run by Vidyo).
Computer and large external screen (part of the Vidyo system and also able to act as a network
computer).
Speaker phone for teleconferences.
There is also a kitchen. You are welcome to join in with the RLC team for lunch at any time, but are asked to
ensure you keep on top of any dishes etc that you use. Code to get into this flat is CZ9615. The Office and the
Nurse Manager’s office are locked after hours.
The Study Space in the middle unit is both a drop in facility for all students use, as well as the RMIP students
allocated study space. This room is available on a 24 hour basis but is reserved on Fridays for the RMIP students
teaching schedule. A copy of ‘Foundations of Clinical Psychiatry’ is kept in this room for your use, a further
copy is also kept at the library. There are several networked computers there that you can log onto as well
and you can make use of this space to access Moodle.
Please let Juliette know if you’re running low on tea, coffee, sugar etc. Please make sure you keep up to date
with the dishes etc.
Local General Practices
If you need to see a General Practitioner during your time on the West Coast then you will need to organise
your own appointment and payment. Ensure you get a receipt, as otherwise you cannot be reimbursed.
Genuine medical attendances are reimbursed via Angela King at the Medical Education Unit.
Coastal Health 70-74 Cowper Street Greymouth
Ph: 03 768-5942
Integrated Family Health Centre Te Nikau Hospital
Greymouth
Ph: 03 769-9300
Family Planning Association (FPA) provides contraception phone 0800 372-546. Emergency contraception is
available at the above or from the community pharmacies.
Pharmacist
Unichem Olsens Pharmacy cnr Tainui & Guinness Sts Greymouth
Ph: 03 768-7470
62
SDHB Code of Conduct and Integrity (District)
This policy outlines the expected standards of behaviour and conduct of
Policy Purpose
all people involved in the operation of Southern District Health Board
(Southern DHB).
All employees of Southern DHB, Board and Commissioner Team
Policy Applies to
members, temporary employees and contractors, must comply with
this Code. It also applies to any person who is involved in the operation
of Southern DHB, including joint appointments, volunteers, those
people with honorary or unpaid staff status and prospective employees
applying for employment.
The Code of Conduct, ‘the Code’, should be read in conjunction with the
Code of Conduct and Integrity for the State Sector, and with relevant
organisational policies, which all employees must comply with.
Associated Documents
Disclosure of Interests Policy District (27894)
include:
Delegation of Authority Policy (District) (21584)
Disciplinary Policy (District) (55569)
Effective Working Relationships (District) (100004)
Email, Internet and Information Security Policy (District) (22497)
Fraud Policy (District) (25546)
Health and Safety and Welfare Policy (District) (15851)
Media Policy (District) (16106)
Private Practice Secondary Employment and Other Business Activities
Policy (District) (19707)
Private Practice Secondary Employment and other Business Activities
[Guidelines] (District) (81064)
Protected Disclosures / Whistle-blowing Policy (District) (19708)
Procurement and Purchasing Policy (District) (11400)
Sensitive Expenditure Policy (District) (48567)
Related
Legislation
Code of Conduct and Integrity for the State Sector
includes:
Employment Relations Act
Health and Safety at Work Act 2015
Human Rights Act
Protected Disclosures Act
Official Information Act
Privacy Act (2020)
Other:
WorkSafe New Zealand
63
Our obligations under the Crown Entities Act 2004 are to act as a ‘Good
Good
Employer
Employer’ as defined under section 118 of the Act.
Statement
The Act defines a good employer as an employer who operates a
personnel policy containing provisions generally accepted as necessary
for the fair and proper treatment of employees in all aspects of their
employment.
Southern DHB is committed to the principles of natural justice and
values all employees and treats them with respect.
Expectations
Southern DHB is committed to the highest level of integrity and ethical
standards in everything that we do. As employers and employees we
must be fair, honest, impartial, responsible and trustworthy at all times.
We must always conduct ourselves in a manner consistent with current
ethical, professional, community and organisational standards and in
compliance with all legislation.
This Code of Conduct does not cover:
every ethical issue that we might face; or
every law and policy that applies to the Southern DHB.
The objective of the Code of Conduct is to:
provide a benchmark and general standard for our behaviour.
provide clarity about expectations of honesty and integrity.
support the Southern DHBs’ reputation and image within the
community; and
make us all aware of the consequences if we breach this policy.
Responsibilities under the Code of Conduct
We are all responsible for implementing and upholding the Code in our
workplace, regardless of our position or role.
All employees are responsible for ensuring that their behaviour reflects
the standards of conduct in the Code and builds a positive workplace
culture. This is inclusive of all employees including clinical and non-
clinical.
All managers which includes clinical, nursing and allied health leaders
and directors have a special responsibility to support employees in
achieving those goals, by leading by example and assisting employees
to understand the Code. It is essential to maintain open communication
lines with organisations representing our employees regarding the
Code. In this Code, a
manager is any employee with supervisory responsibilities.
All of us must have a working knowledge of the laws and policies that
apply to our work, including the Code of Conduct.
64
Obligations under the Code of Conduct
Work to the Best of Your Perform your duties to the best of your ability with care, competence
Ability
and efficiency. Avoid behaviour which impairs your work
performance and/or undermines the integrity of your colleagues.
Maintain proper standards of integrity and conduct in the
performance of your duties. Be open about reporting potential
issues or mistakes.
Be present and actively engaged in your duties at Southern DHB as
required and be absent only with appropriate approval, taking leave
only for the purposes for which it is intended.
Carry out any lawful and reasonable instructions you are given and
work as directed. Implement policies and practices that apply to
your work. Work within appropriate delegations of authority.
Implicit in this is an obligation to obey the laws of New Zealand.
Avoid behaviour which endangers or causes distress to other people
or otherwise contributes to disruption in the workplace and/or avoid
behaviour which might impair their work performance.
Do not engage in alternative employment or self-employment
without appropriate authority, whether or not in a similar area of
work or your work for the Southern DHB. See the
Private Practice,
Secondary Employment and other Business Activities Policy (District)
(19707).
Avoid being a member of any organisation which may impinge on
the proper performance of your duties or be in conflict with the
interest of the Southern DHB.
Maintain a Safe Working Consider the safety of yourself and others in the workplace at all
Environment
times.
Comply with instructions given for workplace health and safety,
including using any personal protective equipment supplied.
Support and promote actions and initiatives in the workplace which
enable hazards and risks to be identified and isolated, eliminated or
reduced.
Ensure that your use of alcohol or other substances in your private
time, outside of work does not impair or impact on your work
performance or endanger the health and safety of others.
Accessing, transmitting, storing or downloading any form of
pornographic, sexually explicit, sexist, racist, demeaning or other
inappropriate material using Southern DHB resources is strictly
prohibited and serious penalties, which may include dismissal, will
apply.
Staff and contractors must wear Southern DHB formal identification
(ID) at all times.
65
Act Professionally
Act honesty and professionally and abide by any code, protocols or
set of standards relevant to the practice of your duties or profession.
For clinicians, this includes staying within your clinical scope of
practice and, where they exist, working within agreed practice
guidelines or research based protocols.
Southern DHB expects that all employees will act in a highly
professional, honest and ethical manner and in compliance with the
Code of Health and Disability Consumers’ Rights.
Maintain all qualifications/licences that are a requirement of your
position (including registration and annual practising certificates)
and provide evidence of these on an annual basis or when asked to
do so. Inform your manager immediately if there are any changes (if
your certificate is revoked or amended in anyway or you cease to
have a valid practising certificate) or restrictions placed on your
practice, including any professional disciplinary proceedings or
litigation that may impact on your employment or professional
registration.
Provide required information for police clearances such as VCA
checks when requested (on a 3 yearly basis).
Where applicable, ensure that your right to work in New Zealand is
maintained by ensuring relevant working or residence visas are valid
and maintained according to immigration requirements. You may
not undertake any work/duties on a visitor visa in New Zealand and
Southern DHB under any circumstances.
Advise Southern DHB in writing of any pending criminal or civil legal
action that may be taken against you and that may reflect on us.
Keep your appearance and presentation clean, tidy and appropriate
for your work role, and in line with relevant uniform and dress
policies and occupational safety/infection control and health
requirements.
Avoid Conflicts of
Avoid making any decision for the Southern DHB where you have any
Interest
interest in the matter other than the Southern DHB’s interests. See
the
Conflict of Interest Guidelines (District) (81067).
Disclose in writing any business activities outside the Southern DHB
and actual or perceived conflicts of interest. See the
Disclosure of
Interests Policy (District) (27894).
Do not use your role or position to gain an advantage in your private
life, for example by arranging jobs/ transfers/ benefits for family or
friends.
Do not let any outside interests adversely affect the performance of
work related duties.
Disclose any relationship you have or form with any person who
directly or indirectly reports to you.
Don’t Accept Gifts,
Never ask others for any reward other than what Southern DHB pays
Benefits or Rewards
you or any other entitlements you receive as an employee.
66
Gifts of money are not to be accepted under any circumstances.
No gift, regardless of monetary value, should be accepted if it could
potentially cause or be perceived by others as causing you to feel an
obligation to the gift giver. This is particularly relevant if you are
involved in current tendering/purchasing processes involving the
parties who may be offering the gift.
All gifts or benefits received must be reported to your manager, who
will advise on the correct course of action. All gifts are to be
recorded on the gift register as pe
r Delegation of Authority Policy
(District) (21584). Failure to do so may result in disciplinary action.
Show Respect for Others
Treat all people with respect, courtesy and honesty, and give
everyone a fair hearing.
Respect the dignity, rights and views of others, including different
values, beliefs, cultures and religions.
Don’t act or speak in a way that is likely to cause offence to others.
Do not discriminate against or harass members of the public, clients,
visitors, patients or colleagues because of their age, sex, marital
status, ethnicity, disability, religious or ethical beliefs, colour, race,
political opinion, employment status or sexual orientation.
Have zero tolerance for bullying and rudeness. Bullying behaviours
include attacks that are direct and personal as well as indirect and
task related. Examples of bullying can be found in the Worksafe New
Zealand ‘Bullying at Work: Advice for Workers’
quick guide.
Avoid behaviour which can be considered to be intimidating,
undermining or victimising.
Avoid any unwelcome or offensive sexual behaviour including:
banter or jokes of a suggestive/sexual nature, unwelcome touching,
patting or pinching, regular hassling for a date, sexually offensive
images or text or e-mail messages or other forms of media, intrusive
questions about personal sex life.
Maintain Confidentiality Treat all information about a person who is receiving or has received
of Information
a public health service with the strictest confidence. This
requirement for confidentiality continues to apply even after you
have ceased working for the Southern DHB.
Personal and sensitive information must be responsibly and
transparently collected and managed in accordance with the privacy
principles applicable to the Southern DHB.
Only access or release information about a patient, client or
employee when it is part of your job, it is lawful or when specific
consent is given.
Avoid Violent and
Southern DHB has zero tolerance to violence in our workplaces. This
Aggressive Behaviour
is not just limited to physical violence. To achieve this, violent and
aggressive behaviour will not be tolerated towards patients, clients,
other employees, students or members of the public.
67
Employees do not have to tolerate violent and aggressive behaviour
towards them, and have the right to expect to work in a safe and
healthy work environment.
Manage Time and
Manage your time and Southern DHB resources efficiently and with
Resources Efficiently
regard to relevant policies.
No private practice will take place during Southern DHB paid time,
or on, or using Southern DHB facilities, medical consumables or
equipment without a formal contractual arrangement approved by
the CEO.
Show reasonable care in using, or allowing the use of, Southern
DHB’s property, resources or funds.
Employees who make decisions involving financial resources on
behalf of the Southern DHB should ensure that they are doing so
within the scope of their delegated authority and within policies and
procedures for the acquisition, use and disposal of resources.
Don’t incur any liability on behalf of Southern DHB without proper
authorisation and within any approved limits specified in the
Delegation of Authority Policy (District) (21584).
All equipment, resources and consumable items are only to be used
for the work and business of Southern DHB unless prior written
authorisation has been obtained from your manager.
Limited, occasional and brief private use of local telephone calls,
personal cell phones, computers and the Southern DHB’s e-mail and
intranet systems are acceptable as long as it does not affect your
work, the work of others, or the reputation of Southern DHB and is
conducted in accordance with this Code and other relevant policies.
Standards of Behaviour and Performance
If you are unclear about the standard of behaviour and conduct that is
required of you as it relates to the Code you should discuss the
situation with your manager, Human Resources or senior
management.
As professional incompetence and/or misconduct are reported to
appropriate registration authorities, it may lead to disciplinary action
by the relevant professional body as well as disciplinary action under
this Code of Conduct.
The following are examples of ‘misconduct’ and not intended to be an
Misconduct
exhaustive list:
It should be noted that the examples listed below as misconduct may
also be considered as ‘serious misconduct’ depending on the nature
and severity of the breach.
Misconduct includes, but is not limited to:
a) failure to maintain an acceptable level of work performance.
68
b) failure to maintain an acceptable level of attendance at work.
c) refusal to perform duties or to follow a reasonable and lawful
instruction.
d) habitually arriving late for duty.
e) being absent from your assigned place of work during working
hours without authority or legitimate reason.
f) failure to provide your manager with timely notice of absences such
as sickness, or that you are unable to commence work at the normal
time.
g) sleeping while on duty (unless authorised by the employer).
h) failure to observe health and safety requirements, including the
requirement to proactively and promptly report personal injury,
injury to others, damage to Southern DHB or patient property or a
hazard that may cause harm.
i) improper use, wastage or damage of Southern DHB resources or
property including wasteful expenditure of Southern DHB
funds/time.
j) unauthorised use of fire protection or safety equipment.
k) reporting for work unsuitably dressed, or in such a condition that
you are unable to perform required duties in a safe and proper
manner.
l) inappropriate or disruptive behaviour in the workplace.
m) unreasonable behaviour towards other people, including abusive,
threatening or offensive language and any form of harassment
including sexual or racial.
n) posting offensive or inappropriate information on noticeboards or
electronic media. See
E-mail, Internet and Information Security
Policy (District) (22497).
o) smoking on Southern DHB premises.
p) failure to hold a current drivers licence and/or to carry a current
drivers licence on their person at all times whilst driving a motor
vehicle belonging to the employer on a public road.
q) failure to provide sufficient information and or respond to a request
to enable the renewal of a VCA check as required (core workers).
r) other breach of this or other policies.
Serious Misconduct
The following are examples of ‘serious misconduct’ and is not intended
to be an exhaustive list:
a) not being in possession of or eligible to hold a required annual
practising certificate.
b) working without a valid work visa.
c) breach of professional protocols or standards whether established
by the Southern DHB or the relevant professional body.
69
d) carrying out private patient work during Southern DHB paid time
and /or using Southern DHB premises or equipment or use of
Southern DHB time, facilities, premises or equipment to undertake
other employment.
e) inaccurate recording of leave, or failure to record leave taken.
f) failure to report to the appropriate manager or supervisor any
accident or incident at work involving actual, or risk of, personal
injury, or damage to property.
g) unauthorised possession of drugs (including alcohol) in the
workplace.
h) reporting for work under the influence of alcohol or drugs or driving
the employer’s vehicles under the influence of alcohol and/or
drugs.
i) violence of any form including assaulting or threatening to assault
anyone in the workplace.
j) possession of patient, client or Southern DHB property without
proper authorisation or possession of another person’s property
without that person’s consent.
k) any form of theft or fraudulent action.
l) being in possession of offensive weapons in the workplace.
m) the unauthorised disclosure of or access to confidential
information.
n) any attempt to mislead the Southern DHB, or any employee, or a
patient/client, or a member of the public in connection with the
Southern DHB’s business. This includes falsification of attendance
records or submitting false claims for expenses or reimbursement,
or providing incorrect information at any stage.
o) acting outside of your delegated authority.
p) exacting, attempting to exact, or accepting any fee, reward, gratuity
or remuneration, other than the salary or allowance pertaining to
the employee’s employment agreement, on account of anything
done in the execution of the duties.
q) deliberate or negligent behaviour adversely affecting the safety of
a patient, client, visitor or another employee.
r) using Southern DHB computers to make unauthorised copies of any
computer software, or for any other unauthorised purpose.
s) admitting to, or being convicted of, any offence which can
reasonably be considered as bringing the Southern DHB into
disrepute or, brings into question the employee’s suitability for
continued employment.
t) accessing, transmitting, storing, downloading or displaying any form
of pornographic, sexually explicit or inappropriate material using
Southern DHB equipment or resources.
70
u) implying or making actual threats of overlooking an employee or
potential candidate for future work opportunities or promotion as
a result of that employee or potential candidate declining the
sexual advances or similar actions of any person in a position of
authority.
v) victimising, intimidating or bullying any employee, or a
patient/client, or a member of the public.
As a general principle, personal behaviour outside of work is of no
Private Conduct
concern of Southern DHB, except where it interferes with work
performance, where the individual is identifiable as a representative of
the Southern DHB, or where the behaviour reflects on the standing or
integrity of the Southern DHB or the employee’s profession or trade,
or constitutes a breach of the law.
Employees should not bring the Southern DHB or their profession into
disrepute through their private activities.
An employee must make the Southern DHB aware of any such
instances as soon as possible.
Whether actions fall into the category of misconduct or serious
Consideration
misconduct will depend on the circumstances in each case. In making
judgements of this kind, regard should be given to the following
factors:
The nature and circumstances of the activity.
The position, duties and responsibilities of the employee.
The consequences of the activity on the employee to fulfil his/her
duties and responsibilities.
The effects of the activity or its consequences on working
relationships with colleagues, patients, outside contacts and the
general public.
Breaches of the Code of Conduct
We are all responsible for trying to avoid escalation of inappropriate
behaviour that may result in a breach of the Code, and for dealing with
workplace conflict through timely and appropriate communication that
addresses the behaviour in a constructive way. You are expected to
cooperate with any investigations being conducted in relation to an
alleged breach of the Code.
Managers must make fair, transparent and consistent decisions in
response to an allegation of a breach of the Code and the action to be
taken in response to a breach. In determining the action to be taken
the nature and seriousness of the breach will be considered.
Some possible consequences of a breach include:
informal or formal counselling.
disciplinary processes (including opportunities to improve, written
warnings, and summary dismissal).
71
referral to registration boards or other regulatory authorities
especially in the case of those employees providing direct patient
care.
referral to the Police (in cases of suspected criminal activity) or
relevant government department e.g. immigration.
If you are concerned about a possible breach of this Code, your manager
should be able to help you.
If you are concerned about approaching your manager to discuss the
issue, you can also talk to:
Human Resources.
Your professional leader.
Your union or employee representative.
A speak-up supporter, or
The State Services Commission's integrity and conduct help desk;
phone (04) 495 6722 or e-mail
: [email address]
Only those who need to know will be made aware of the situation.
Southern DHB is committed to protecting any person who raises
concerns or provides information about a breach of the Code or any
other organisational policy from retaliation or reprisals. In some
circumstances, an employee who makes a disclosure about serious
wrongdoing will be afforded anonymity as provided for in the
Protected Disclosures Act 2000. This Act makes it a criminal offence to
take a reprisal against any individual who makes a protected disclosure.
Please refer to the
Protected Disclosures and Whistle-blower Policy
(District) (19708) for full guidance.
I have read and understand the Code of Conduct and Integrity.
_________________________________________________
______________
(Name) (Date)
72
Key policies and regulations related to the MB ChB
These are available at
https://www.otago.ac.nz/medicine/current-students/resources/policies-
guides/index.html
The following list highlights some of these for your particular attention.
Code of Practice for Fitness to Practice Page
Code of Professional Conduct for Medical Students at the University of Otago Page
Medical Council of New Zealand Policies and Information for Medical Students Page
Harassment Policy Page
Privacy and Confidentiality Page
Academic Integrity Page
Copyright (Infringing File Sharing) Act 2011 Page
Drugs and Other Legal Offences Page
Ethical Behaviour Policy Page
Other Otago Medical School Policies of note Page
Policy and Procedure for Transfers Between Schools of the Otago Medical School Page
Policy and Procedure for Transfers Between Otago and Auckland Medical Schools Page
Policy on transmissible and blood-borne infections for medical students, based on Medical Council
guidelines
73
University of Otago Medical School Prizes and Dunedin Campus Prizes and
Awards
Otago Medical School
Prizes are awarded at the end of TI 6th) Year, however your studies during ALM4/5 can contribute to these
awards.
Batchelor Memorial Medal and Prize in Gynaecology and Obstetrics
Founded by members of the Otago Division of the British Medical Association, who, in 1916, subscribed the
sum of £119.14.6 to provide medals and prizes to perpetuate the memory of the late Dr Ferdinand Campion
Batchelor, Lecturer in Midwifery and Diseases of Women 1883–1909, and Professor in 1909. A medal and
prize are awarded annually by the University Council on the recommendation of the Pro-Vice-Chancellor
(Health Sciences), to the student who obtains the highest mark in oral assessments in the subjects of
Gynaecology and Obstetrics held in conjunction with the final-year examinations for the degrees of Bachelor
of Medicine and Bachelor of Surgery. The value of the Prize will be as set down in the current prize schedule
and an engraved medal.
Stanley Batchelor Memorial Prize in Surgery
The Stanley Batchelor Memorial Prize was founded by Mrs Stanley Batchelor, who, in 1942, donated the sum
of £150 to the University Council to perpetuate the memory of the late Dr F. Stanley Batchelor. The capital of
the fund was increased in 1960 when Mrs Batchelor's son, Mr L.C. Batchelor, donated £50 to the Council to
augment the fund. A further sum of NZ$100 was donated in 1973, both by Mr Batchelor and Mrs J.M. Elworthy
to increase the value of the prize. The prize is awarded annually by the University Council on the
recommendation of the Pro Vice-Chancellor (Health Sciences), to the Trainee Intern who has the highest
aggregate mark from assessments of performance on surgical attachments and a viva in Clinical Surgery. A
student who has not obtained passing assessments in all the subjects of the final year of the Medical course
shall not be eligible for the award of the prize. Any balance of income shall be added to the capital. The value
of the Prize will be as set down in the current prize schedule.
Colquhoun Memorial Medal in Clinical Medicine
This prize was founded in 1935 by the past students of Dr Daniel Colquhoun, who was Professor of Medicine
from 1883 to 1918 and Emeritus Professor from 1919 until his death in 1935. The medal is awarded annually
by the University Council on the recommendation of the Pro-Vice-Chancellor (Health Sciences), to the medical
student in the final year who gains the highest marks in Clinical Medicine in the end of year examination.
The Rita Gardner Travelling Scholarship in Medicine
Established in 1908 as the "Travelling Scholarship in Medicine", and amended in 1989 to its present title. The
Scholarship shall be awarded annually to the student in the graduating class who has gained the highest
aggregate of marks in the Second Year, Third Year, Fifth Year and Final Examinations for the degrees of
Bachelor of Medicine and Bachelor of Surgery. The holder of the Scholarship shall within eight years from the
date of the award proceed to some recognised school or schools of Medicine or other institution or institutions
approved by the Dean of OMS outside New Zealand and shall prosecute graduate studies there for a period of
at least one year. In exceptional circumstances, with the approval of the Dean, the Scholarship may be tenable
in New Zealand.
T W J Johnson Memorial Prize in Clinical Medicine
This prize was founded in 1958 when an anonymous donor gave the sum of £1000 to the Council to establish
a prize as a memorial to the late Dr T.W.J. Johnson, the first Medical Travelling Scholar. This prize is awarded
annually by the University Council on the recommendation of the Pro-Vice-Chancellor (Health Sciences), to
the medical student who in the final year of the course, gains the highest marks in Clinical Medicine in the end
of year examination. The value of the Prize will be as set down in the current prize schedule.
74
Emily Hancock Siedeberg Memorial for the Best Overall Woman Student
Established in 1996 on the 100th anniversary of the graduation from OMS of Emily Hancock Siedeberg. The
prize is funded from money contributed by the late great nephew of Dr Siedeberg. The prize shall be awarded
annually by the University Council on the recommendation of the Pro-Vice-Chancellor (Health Sciences) to the
female student in the graduating class who has gained the highest aggregate of marks in the second year,
third year, fifth year, and final examinations for the degrees of Bachelor of Medicine and Bachelor of Surgery.
The value of the prize is as set down in the current prize schedule.
Psychological Medicine Prize
A sum of money is available annually for the provision of a prize in Psychological Medicine. The award, which
is restricted to candidates completing the final examination for the degrees of Bachelor of Medicine and
Bachelor of Surgery, will be made by the University Council on the recommendation of the Pro-Vice- Chancellor
(Health Sciences), on the basis of performance in Psychological Medicine in the sixth year including an oral
examination. The prize is the sum set down in the current prize schedule for 'Distinction' in Psychological
Medicine.
J M Watt Prize in Paediatrics and Child Health
This prize was established in 1977 in honour of Professor James Michael Watt, the holder of the first Chair of
Paediatrics and Child Health established in New Zealand (1966). The prize will be awarded by the University
Council on the recommendation of the Pro-Vice-Chancellor (Health Sciences), for the first time in 1978, and
thereafter annually, to a final year student from one of the three Clinical Schools of the University of Otago.
The award will be made to the best candidate in the Paediatric distinction viva examination, taking into
consideration the student's interest and excellence throughout the preceding clinical years. The value of the
Prize will be as set down in the current prize schedule.
Dunedin Campus
Marjorie McCallum Medal in Medicine
This award was founded in 1923 by the Hon. Richard McCallum as a memorial to his daughter who died while
she was a medical student at the University of Otago. The medal is awarded annually by the University Council
on the recommendation of the Pro-Vice-Chancellor (Health Sciences), to the final year Medical student in
Dunedin who is awarded the highest marks in Clinical Medicine in a special end of year prize examination.
James Renfrew White Prize in Orthopaedic Surgery
The prize fund was established in 1976 by a bequest of NZ$3,000 from the late Miss Ida G. White in memory
of her brother, the late Mr James Renfrew White, a graduate of OMS who was Director of Orthopaedic Surgery
for the Otago Hospital Board and Lecturer in Orthopaedic Surgery from 1920 until 1948. The prize is awarded
annually by the University Council on the recommendation of the Pro- Vice-Chancellor (Health Sciences), to
the student who has served his or her clinical years in Dunedin and who while a sixth year student, in the
opinion of OMS on the recommendation of the Head of Section of Orthopaedic Surgery, has demonstrated
the most outstanding clinical ability and scholarship in the field of orthopaedic and trauma surgery. The prize
will be awarded only if there is a candidate of sufficient merit. The value of the Prize will be as set down in the
current prize schedule. Any surplus of income may be added to the capital of the fund or may be used at the
discretion of the Council for increasing the value of the prize or for awarding an additional prize. The Council
shall have the power to alter these regulations should changed circumstances render such action necessary,
provided that the name of the prize shall not be altered and that the wishes of the donor shall be observed to
the fullest possible extent.
Patricia Buckfield Prize in Paediatrics
Dr Patricia Buckfield MB ChB (NZ), MD Otago, MRCP, FRACP, DCH (FRP&S) was a senior lecturer in the
Department of Paediatrics and Child Health at the University of Otago in Dunedin between 1967 and 1981,
following postgraduate training in Neonatology in the UK. She introduced the new technique of neonatal
75
ventilation to the Special Care Baby Unit in Dunedin. She was a dedicated and caring paediatrician, who based
her MD thesis on the perinatal events of approximately 20,000 babies who were born in Dunedin City. A one-
year cohort of this sample formed the basis for the Dunedin Multidisciplinary Child Development Study, which
has achieved international recognition and is still ongoing. She also saw the need to provide extra assistance
for children and their families where there were concerns about the child's developmental progress. She was
instrumental in setting up the Vera Hayward Centre, which forms the base for the Dunedin Hospital Child
Development Service. During her time in Dunedin she was an enthusiastic and inspiring teacher of
undergraduate and postgraduate students from Health and many other disciplines. In her later professional
years she continued her interest in developmental paediatrics and worked as a Developmental Paediatrician
in the Puketiro Centre at Porirua. During her professional career she made an outstanding contribution both
to clinical and to academic paediatrics. The prize consists of books, instruments, or education aids to a value
of $600, and a book voucher to the value of NZ$100.
Sir Gordon Bell Prize in Surgery
This prize is named after the second Professor of Surgery at the University of Otago, who held the Chair from
1925–1952. Sir Gordon Bell was born in Marlborough, trained in Edinburgh and practised for most of his life
in Dunedin. He was a very eminent and practical surgeon, whose career spanned many of the important
developments in Surgery. The prize consists of books and instruments to a value to be advised.
Paediatric Artistic Expression
This prize was introduced in 2010 by Professor Barry Taylor. It is awarded to a Trainee Intern who chose to
submit an original artistic creation in their final assessment for their Paediatric Longitudinal Case: The Child
with the Chronic Condition, which is commenced in fourth year and completed in fifth year. This prize
recognises the Trainee Intern who showed outstanding artistic expression. The prize is a book voucher to the
value of NZ$50.
Mary Shaw Surgical Prize
Established in 1992 by a bequest of NZ$2,500 under the will of Mary Christiana Shaw (nee Manning) who was
born in Invercargill in 1912. In 1932 she married James Thomson Shaw, General Manager of the Southland
Savings Bank from 1952 to 1970. In 1964, while Mr Shaw was General Manager, the Board of the Bank
established the Southland Savings Bank Medical Foundation for the furtherance of medical education and
research in Southland. Mr and Mrs Shaw had two sons: John Donald Shaw, a mining engineer in Brazil, and
James Henry Farquhar Shaw BMedSc MD (Otago) FRACS, a surgeon in Auckland. Mrs Shaw died in Auckland in
1992. The prize of NZ$200 is awarded annually by the University Council, to the student undertaking the sixth
year of the course for the degree Bachelor of Medicine and Bachelor of Surgery, as a Trainee Intern in Dunedin
or Invercargill who, in the opinion of the clinical teachers concerned, displays the greatest industry and
competence in the Surgical attachment.
Stanley Wilson Prize
Established in 1982 by Dr Elizabeth Whitcombe, a graduate of OMS, for the purpose of furthering the study of
Medicine at the Dunedin Division of the OMS, and in particular to recognise the contribution made by a former
teacher, Mr Stanley Wilson, over many years, to the science and teaching of surgery at OMS. The prize consists
of books, instruments or education aids to the value of NZ$750, and is awarded by the University Council on
the recommendation of an Advisory Committee, comprising the Dean of OMS, the Professor of Surgery in the
OMS at Dunedin and the Chairman of the General Medical Staff of the Dunedin Hospital. The prize is awarded
annually to a medical undergraduate in OMS at Dunedin who best presents in his or her final year a clinical
presentation in the Department of Surgery having general medical interest and a reference to pathology.
Sir Bernard Dawson Prize in Clinical Obstetrics and Gynaecology
Sir Bernard Dawson held the Foundation Chair in Obstetrics and Gynaecology at the University of Otago in
Dunedin from 1932–1950. He was responsible for putting the academic discipline of obstetrics and
gynaecology firmly in place in New Zealand and he was knighted in 1948 for his services to Obstetrics and
Gynaecology in this country. The prize consists of educational material/aids to a value to be advised.
76
Professor Basil James Prize in Psychological Medicine
Professor Basil James was professor and head of the Department of Psychological Medicine from 1969–1981.
Professor James persuaded the general medical staff that psychiatry should also have a prize, as did medicine
and surgery, whose prizes had come from family bequests. These negotiations occurred in the late '60s. The
prize consists of books to a value to be advised.
RNZCGP Otago/JAD Iverach Prize in General Practice
Five prizes were awarded in Preventive and Social Medicine prior to 1974 by the New Zealand Faculty of the
Royal College of General Practitioners and from 1974 to 1977 by the Otago-Southland Faculty of the New
Zealand College of General Practitioners. These were replaced in 1978 by a single prize in the discipline in
General Practice. The Prize will be awarded at the annual Trainee Intern Prize giving and Farewell by the Head
of the Department of General Practice, Dunedin Campus, for the best student performance during the
undergraduate course in General Practice. This assessment will include the fourth, fifth and sixth years of the
course. The Prize consists of an engraved medal and $1,000. There is also a $500.00 prize awarded to the
runner-up, and two highly commended prizes of $250.00.
JAD Iverach Prize in Medicine
Captain Douglas Iverach was an infantry soldier at the First World War and received an MC. After the war he
went through OMS and went to Scotland on qualification, specialising in Medicine. He came back to Dunedin
and was appointed to the Honorary Staff of Dunedin Hospital, practicing as a general practitioner from the
Savoy. He was so thorough in his examination, so if GPs were worried, they would seek his opinion. There were
no full time specialists as such in those days. By the referrals to him, he became known as a specialist. In May
1965 the J A D Iverach Memorial Fund was started from which an annual prize would be awarded to the best
sixth year medical student in clinical medicine. There were some cash donations by grateful patients but most
of the contributions made by his family were made in shares. The prize consists of a presentation gift.
Inkster-Ross Memorial Prize
The Inkster-Ross Memorial Fund was established in 1946 by Lady Muriel Ross of Dunedin as a memorial to her
father Samuel Macaulay Inkster M.D. and to her mother Amy Inkster. The gift was established to further
medical research with an emphasis on the field of preventive medicine. The Inkster-Ross Memorial prize was
re-established in 2011 to recognize the research achievements of final year medical students as they complete
a health care evaluation project. Working in groups, students undertake research to address a problem in the
delivery of health care. The prize is awarded annually by the Department of Preventive and Social Medicine to
the group who undertake the highest quality research.
Elective Report Award
The Trainee Intern Elective Report Award was established in 1984 (by Professor Don Wilson) and sponsorship
was obtained in 1992 from Mr Russell Duff, Managing Director of VIP International Travel in appreciation of
the ongoing close links between VIP Travel and medical elective students. This sponsorship is continued today
by the School. The prize consists of a book voucher to the value of NZ$50 to the Trainee Intern who has
submitted the best elective report during the year, which has been chosen by our electives committee.
University Bookshop Prize for Best Student Contribution to Medical Education
Established in 1985 by the Directors of the University Book Shop Otago Ltd. The prize is awarded annually by
the University Council to the student who has made the most significant contribution to undergraduate
medical education in OMS during the past year. A nomination shall be made by the Dean after consultation
with the Staff/Student Curriculum Committee. The value of the Prize will be as set down in the current prize
schedule.
John Russell Ritchie Prize (to be confirmed if available in 2021)
John Russell Ritchie worked as an Anaesthetist at Dunedin Hospital from 1938 until his retirement in
1975. He was the Director of Anaesthesia at Dunedin Hospital for over 25 years and was appointed to the first
professorial position held by an Anaesthetist in New Zealand. During his time in Dunedin he was an enthusiastic
and inspiring teacher of undergraduate and postgraduate students from Health and many other disciplines.
77
He is famous for contributing to worldwide anaesthesia safety with his invention of the Ritchie oxygen failure
warning device which in either its original or a modified form became a standard part of all anaesthesia
machines. The prize for the best student performance in Anaesthesia and Intensive Care was first awarded in
1976. Following the 2002 reorganisation of the curriculum and departments the prize was held in abeyance.
It was decided to re-institute this prize from 2006 at Trainee Intern level. The criteria for this prize include:
That the prize be awarded, after an oral interview, to the top-placed candidate who has performed to
a level of excellence in the interview and during their attachment in Anaesthesia and/or Intensive Care
as a Trainee Intern.
Those to be interviewed are nominated by sub-groups of the Section of Anaesthesia and Intensive
Care. It is not a prize, which a trainee can apply for of one's own volition.
Trainee Interns have to have completed one or more Trainee Intern attachments in Anaesthesia or
Intensive Care in Dunedin to be nominated.
The areas assessed for the award of this prize now takes into account the candidates clinical work,
academic/research aptitude, professionalism and a Viva relating to topics in Anaesthesia, Pain
Management, Intensive Care and Resuscitation at the end of the Trainee Intern year.
Those to be interviewed are nominated by sub-groups of the Section of Anaesthesia and Intensive
Care. It is not a prize, which a trainee can apply for of one's own volition.
Trainee Interns have to have completed one or more Trainee Intern attachments in Anaesthesia or
Intensive Care in Dunedin to be nominated.
The areas assessed for the award of this prize now takes into account the candidates clinical work,
academic / research aptitude, professionalism and a Viva relating to topics in Anaesthesia, Pain
Management, Intensive Care and Resuscitation at the end of the Trainee Intern year. The prize consists
of books, instruments or education aids to the value of NZ$500.
Kōhatu – Centre for Hauora Māori Excellence Awards
The kete (baskets) of knowledge comes from ancient tauparapara (legend) which relates to the exploits of
Tane-nui-a-rangi in his pursuit of knowledge. Tane, the progenitor of mankind, of the forest, ascended from
earth to the heavens and obtained the three kete of knowledge. Tane returned to earth with the knowledge,
and there created humankind from the earth.
To many, this is a simple mythological story which seeks to explain how humankind gained its knowledge of
things both earthly and spiritual from the gods. The story is the beginning of the stories of the Whare Wananga,
which describe how this earthly realm came to be, and how everything in it came to be ordered as it is,
including how humankind was created by Tane.
To some it is a metaphor for the ideal life, a journey of striving for knowledge and education and
enlightenment, to become better people. In this context it graphically depicts three aspects of knowledge
achieved in the Hauora Māori medical curriculum within the Dunedin Campus, preparing students to make a
difference for Māori, whanau and communities.
Three kete will be offered annually – Dunedin TI Year:
Ko te kete Tuauri – Knowledge of Ritual, Memory, and Prayer (Cultural Connection) – For a student
that shows a commitment to enhancing Hauora Māori concepts such as culture, te reo, and
whakawhanaungatanga
Ko te kete Tuatea – Knowledge of Making a Difference (Addressing Equity) - For a student that shows
a commitment to improving health equity and challenging the status quo for Māori
Ko te kete Aronui – Knowledge to Help Others (Positive Solutions) – For a student that shows initiative
creating positive solutions for improving Māori Health
Awards funded, students nominated, and chosen by Kōhatu - Centre for Hauora Māori staff.
78