OTAGO MEDICAL SCHOOL
Te Kura Hauora o Ōtākou
2021
University of Otago, Christchurch
Advanced Learning in Medicine
Fourth and Fifth Year
Handbook
ALM
4/
5
CC
YE
2015
C
University of Otago, Christchurch
Fourth and Fifth Year
Handbook
2021
Disclaimer: While al reasonable efforts have been made to ensure that the information
contained in this publication is correct at the time of printing, matters covered in this
publication are subject to change.
The University reserves the right to change courses and course requirements at any time.
1
2021 Year 4 & Year 5 Handbook Contents
COURSE INFORMATION
2021 Dates for Year 4 and Year 5 .............................................................................................. 5
Key Members of Staff and Contact Details ............................................................................... 6
Block and Vertical Module Convenors ...................................................................................... 7
Attendance ...................................................................................................................... 8
Communication / Changing Contact Details ................................................................... 8
Forms ............................................................................................................................... 8
Internet, Cel phone, iPad, Laptop Use............................................................................. 8
Social Media and the Medical Profession ....................................................................... 8
Remediation .................................................................................................................... 9
Remediation Timing ........................................................................................................ 9
Student Leave Policy ........................................................................................................ 10
Students on Placement – contact details on eVision ...................................................... 11
Trainee Intern Electives ................................................................................................... 11
UOC Gold Medal Teaching Awards ................................................................................. 11
Research Opportunities ................................................................................................... 11
Summer Studentships ..................................................................................................... 11
Bachelor of Medical Science (Hons) ................................................................................ 12
Year 4 Programme (green pages)
Welcome from the Dean ................................................................................................. 13
Course Overview ............................................................................................................. 14
Year 4 UOC ALM Block and Vertical Modules ................................................................. 15
2021 Year 4 Class Groups ................................................................................................ 16
2021 Block Module Rotations for Year 4 Groups ............................................................ 17
2021 Summary of Year 4 Clinical Modules ...................................................................... 18
Clinical Orientation .......................................................................................................... 21
Block Modules
Older Person’s Health Module ........................................................................................ 22
Public Health Medicine Module ...................................................................................... 24
Addiction Medicine Module ............................................................................................ 26
General Practice Module ................................................................................................. 28
Cardio-Respiratory Medicine Module ............................................................................. 29
Cardiology/Vascular Surgery/Plastic Surgery/Dermatology (CVPD) Module.................. 30
Surgery/Emergency Medicine/Gastroenterology/Oncology (SEGO) Module ................ 31
Vertical Modules
Clinical Skills ..................................................................................................................... 32
Ethics and Law ................................................................................................................. 33
Hauora Maori .................................................................................................................. 34
Palliative and End of Life Care (PEOLC) ........................................................................... 35
Pathology ......................................................................................................................... 36
Professional Development .............................................................................................. 37
Quality and Safety ........................................................................................................... 38
Radiology ......................................................................................................................... 39
Year 4 Awards .................................................................................................................. 40
Year 4 Scholarships on OMS website .............................................................................. 41
2
Year 5 Programme (pink pages)
Introduction from the Dean ............................................................................................ 43
Course Overview ............................................................................................................. 44
Year 5 UOC ALM Block and Vertical Modules ................................................................. 45
2021 Year 5 Class Groups ................................................................................................ 46
2021 Block Module Rotations for Year 5 Groups ............................................................ 47
2021 Year 5 Summary of Clinical Modules ...................................................................... 48
Block Modules
Women’s Health and Developmental Medicine ............................................................ 51
Paediatrics ...................................................................................................................... 53
Psychological Medicine ................................................................................................... 54
Orthopaedic and Advanced Surgery ............................................................................... 55
Advanced Medicine (Medicine/Neurosciences/Rheumatology) .................................... 57
Vertical Modules
Clinical Pharmacology ...................................................................................................... 59
Clinical Skills ..................................................................................................................... 61
Ethics and Law ................................................................................................................. 63
Hauora Maori................................................................................................................... 64
Pathology ........................................................................................................................ 65
Professional Development .............................................................................................. 66
Quality and Safety ........................................................................................................... 67
Radiology ......................................................................................................................... 68
Year 5 Prizes .................................................................................................................... 70
Year 5 Scholarships on OMS website .............................................................................. 70
University of Otago, Christchurch (UOC) Information
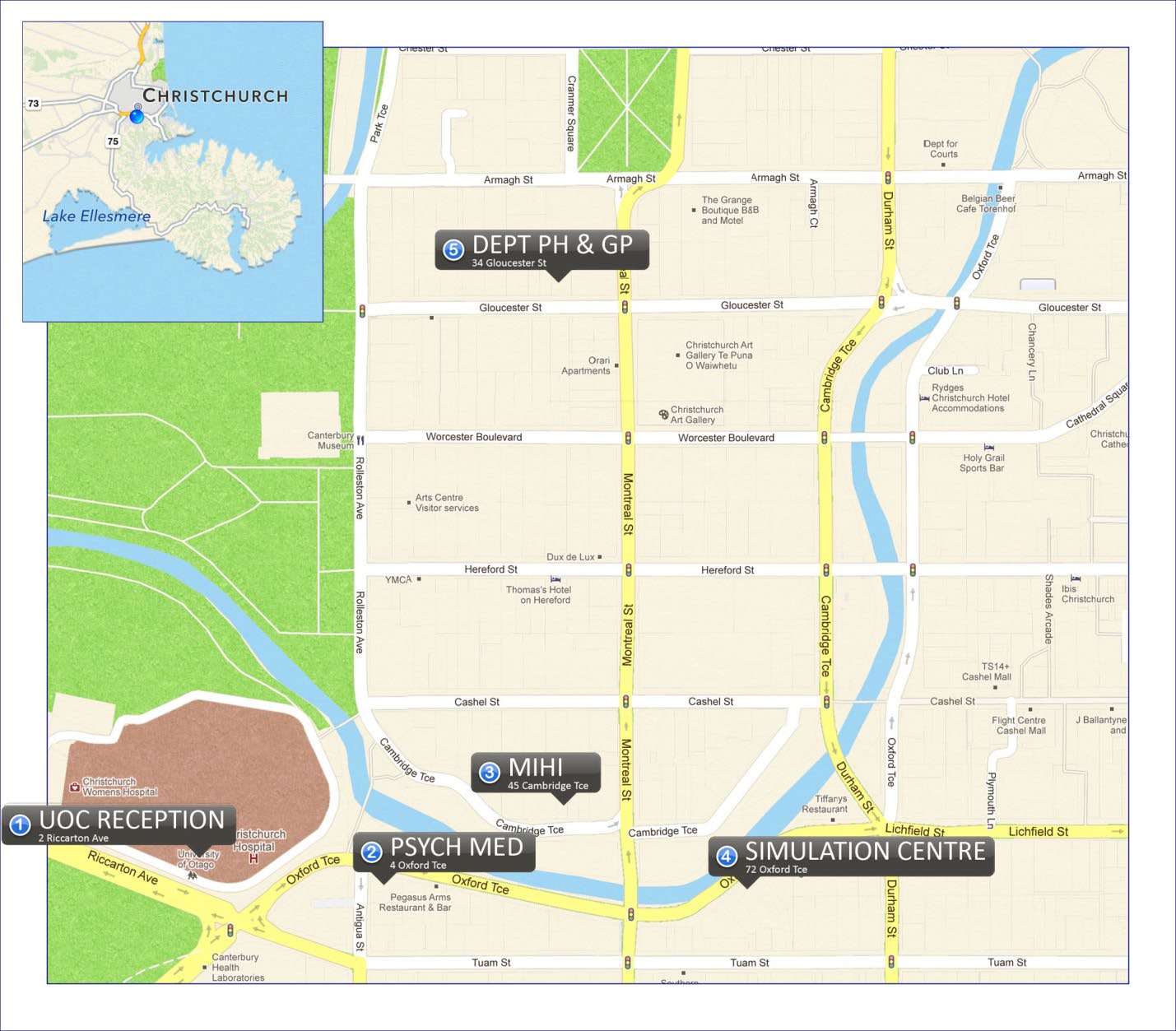
UOC Building and Facilities .............................................................................................. 72
Location Map for offsite UOC departments .................................................................... 75
Canterbury Medical Library ............................................................................................. 76
Student Computer Facilities ............................................................................................ 77
Medical Education Unit (MEU) ........................................................................................ 78
STUDENT WELFARE AND SERVICES
Module Convenor ................................................................................................................. 79
Student Staff Committee ...................................................................................................... 79
Associate Dean (Undergraduate Student Affairs) ................................................................. 79
Associate Dean (Medical Education) ..................................................................................... 79
Professional Development Group ......................................................................................... 79
Chaplain................................................................................................................................. 79
General Practitioner Service for Medical Students ............................................................... 80
School of Physiotherapy Clinic – 32 Oxford Tce .................................................................... 81
Disabilities Officer ................................................................................................................. 81
Maori Student Support ......................................................................................................... 81
Dean of the Campus .............................................................................................................. 81
International Student Support .............................................................................................. 81
International Student Advisers ........................................................................................ 82
Student Visa Service ......................................................................................................... 82
Insurance Support ............................................................................................................ 82
Code of Practice for Pastoral Care of International Students .......................................... 82
Christchurch Medical Students’ Association (CMSA) ............................................................ 83
Christchurch Postgraduate Students’ Association ................................................................ 83
New Zealand Medical Association (NZMA) ........................................................................... 83
New Zealand Medical Students Association (NZMSA) .......................................................... 83
3
OBJECTIVES, ASSESSMENT & EXAMINATION INFORMATION
Educational Objectives and Assessment ......................................................................... 85
University of Otago Medical Graduate Profile ................................................................ 85
MB ChB Programme Assessment Policies and Procedures ............................................. 87
Special Arrangements for End of Year Exams ................................................................. 88
Special Considerations in Assessments and Examinations ............................................. 88
Student Evaluation of Modules ....................................................................................... 91
WORKING IN A CLINICAL SETTING
Student Access to Canterbury District Health Board (CDHB) Premises .......................... 93
MedChart ......................................................................................................................... 93
Attendance at Clinical Ward Rounds while Unwell ......................................................... 93
Access to Clinical Records ................................................................................................ 93
Recording Lectures, Patient Interviews and Clinical Presentations ................................ 93
Taking and Sharing Images on personal devices: a guide for Otago Medical Students .. 93
Chaperoning .................................................................................................................... 96
Cultural y Sensitive Issues ............................................................................................... 96
Guidance on Dress ........................................................................................................... 96
Immunisation Guidelines on OMS website ..................................................................... 97
Emergency Response: Dealing with exposure to blood and/or body fluids ................... 97
Professional Behaviour: general ...................................................................................... 98
Professional Behaviour: the role of patients in clinical education .................................. 98
Consent for clinical education ............................................................................... 98
Clinical examination of patients ............................................................................ 98
Professional Behaviour: Supervision ............................................................................... 100
Appropriate supervision .................................................................................................. 100
Privacy and Confidentiality .................................................................................... 100
Medical Student Rights.................................................................................................... 102
Responding to Problems ................................................................................................. 102
UNIVERSITY, OTAGO MEDICAL SCHOOL AND OTHER RELEVANT POLICIES
A Guide to Academic Conduct ......................................................................................... 103
Ethical Behaviour Policy / Informal Conflict Resolution .................................................. 103
Otago Medical School (OMS) Policies available on Website ........................................... 104
Code of Practice for Fitness to Practise ........................................................................... 105
Policy and Procedure for Transfers between Schools of the Faculty of Medicine ......... 105
Policy and Procedure for Transfers between Otago and Auckland Med Schools ........... 106
Medical Council of New Zealand website ....................................................................... 106
4
COURSE INFORMATION
2021 Year 4 and Year 5 Dates
Year 4
1st Semester Monday, 1 February to Friday, 11 June 2021
Clinical Orientation/Hauora Maori Fortnight:
Monday, 1 February January to Friday, 12 February (compulsory)
Waitangi Day: Monday, 8 February (observed)
Mid-Semester Vacation: 2-11 April inclusive (includes Easter)
ANZAC Day: Monday, 26 April (observed)
Queen’s Birthday: Monday, 7 June
Mid-Year Vacation: 12-27 June inclusive (2 weeks)
2nd Semester Monday, 28 June to Friday, 29 October 2021
Whole Class Teaching Week (WCTW): 28 June-2 July (compulsory)
Mid-Semester Vacation: 21-29 August inclusive (1 week)
Labour Day: Monday, 25 October
Semester ends: Friday, 29 October 2021
Year 5
1st Semester
Tuesday, 9 February to Friday, 11 June 2021
Waitangi Day: Monday, 8 February (observed)
Mid-Semester Vacation: 2-11 April inclusive (includes Easter)
ANZAC Day: Monday, 26 April (observed)
Queen’s Birthday: Monday, 7 June
Whole Class Teaching Week (WCTW): 8-11 June (compulsory)
Mid-Year Vacation: 12-27 June inclusive (2 weeks)
2nd Semester Monday, 28 June to Friday, 5 November 2021
Mid-Semester Vacation: 21 August – 29 August inclusive (1 week)
Labour Day: Monday, 25 October
Study Week Tuesday, 26 October – Friday, 29 October
OSCE Saturday, 30 October
Written/MCQ exams Monday, 1 November – Friday, 5 November
TI Orientation Friday, 5 November
Semester ends: Friday, 5 November 2021
5
Key Members of Staff and Contact Details
Dean
Prof David Murdoch
[email address]
80522
Deputy Dean
Prof Vicky Cameron
[email address]
81210
Medical Education Unit & Reception (Ground Floor, UOC)
Assoc Dean (Medical Education) Prof Lutz Beckert
[email address]
Assoc Dean (Undergraduate
Student Affairs)
Tania Huria
[email address]
81080
Client Services administrator
Viv Hepburn
[email address]
81547
Medical Education Adviser
Anthony Ali
[email address]
86295
Coordinator Student Experience Amanda Clifford
[email address]
86161
Receptionist
Anna Groen
[email address]
80530
Key Administrative and Support Staff – 5th Floor
Senior Manager Client Services
Melissa Paton
[email address]
80554
Manager Client Services
Katrina Hogg
[email address]
81681
Dean’s Executive Assistant
Robyn Maguigan
[email address]
80522
IT Support Services team leader Tim Young
[email address]
81691
IT Support senior technician
Anna Young
[email address]
81685
IT Support senior technician
Jarren Nelson
[email address]
80632
IT Support senior technician media Dean Pester
[email address]
81007
IT Helpdesk
[email address] 0800 479 888
Research & Development Manager Rebecca Coombes
[email address]
80038
Research Manager, Maori
To be advised
81658
Heads of Academic Departments
Anaesthesia
Prof Ted Shipton
[email address]
81642
Population Health
Prof Gillian Abel
[email address]
364 3619
General Practice
Dr Ben Hudson
[email address]
364 3604
Medicine
Prof Richard Gearry
[email address]
81846
Obstetrics & Gynaecology
Dr Jo Gullam
[email address]
85638
Pathology & Biomedical Sciences Prof Martin Kennedy
[email address]
81530
Orthopaedics & MSM
Prof Gary Hooper
[email address]
80430
Paediatrics
Prof Andrew Day
[email address]
80735
Psychological Medicine
Prof Richard Porter
[email address]
86404
Surgery
A/Prof Tim Eglinton
[email address]
88174
Radiology
Prof Anthony Butler
[email address]
86359
Extension nos. starting with 80 can be direct dialled with prefix 3640 and last 3 digits of extension.
Extension nos. starting with 81 can be direct dialled with prefix 3641 and last 3 digits of extension.
6
Block Module Convenors
Year 4
SEGO
Mr Chris Wakeman - lead
[email address]
Prof Michael Ardagh
[email address]
Prof Bridget Robinson
[email address]
A/Prof Catherine Stedman
[email address]
Dr Matthew Strother
[email address]
Dr Tamara Glyn
[email address]
General Practice
Dr Lynette Murdoch
[email address]
Public Health
Rose Crossin
[email address]
Addiction Medicine
Dr James Foulds
[email address]
Prof Doug Sellman
[email address]
Cardio/Respiratory
Dr Geoffrey Clare
[email address]
CVPD
Mr Jeremy Simcock
[email address]
Year 5
Orthopaedics and Advanced
Prof Gary Hooper
[email address]
Surgery
Dr Ramez Ailabouni
[email address]
Advanced Medicine
A/Prof David Jardine
[email address]
Psychological Medicine
Dr Ben Beaglehole
[email address]
Paediatrics
A/Prof Tony Walls
[email address]
Women’s Health/ Developmental Dr Jo Gullam – lead
[email address]
Medicine
A/Prof Philip Pattemore
[email address]
Dr Stephanie Moor
[email address]
A/Prof Sue Luty
[email address]
Vertical Module Convenors
Year 4 & Year 5
Clinical Skills
Dr Niki Newman
[email address]
Ethics
Dr Simon Walker
[email address]
Dr Neil Pickering
[email address]
Hauora Maori – Y4
Maia Melbourne-Wilcox
[email address]
Hauora Maori – Y5
Prof Suzanne Pitama
[email address]
Pacific Health
Dr Allamanda Faatoese
[email address]
Palliative and End of Life
Dr Amanda Landers
[email address]
Pathology
Dr Andrew Miller - lead
[email address]
Anatomic Pathology
Dr Andrew Miller
Microbiology
Prof Steve Chambers
[email address]
Haematology
Dr Sean MacPherson
[email address]
Professional Development
Prof Bridget Robinson
[email address]
A/Prof Tony Walls
[email address]
Dr Martin de Bock
[email address]
Dr Philip Adamson
[email address]
Quality and Safety
Dr Phil Hider
[email address]
Radiology
Dr Mike Hurrell
mike.hurrel @cdhb.health.nz
Year 5
Addiction Medicine
Prof Doug Sellman
[email address]
Clinical Pharmacology
A/Prof Matt Doogue
[email address]
Dr Paul Chin
[email address]
7
Attendance
Students are expected to attend al (100%) learning opportunities to gain experience, and should
demonstrate enthusiasm, professionalism and commitment to learning. Individual block and
vertical modules wil clarify their expectations of attendance at the beginning of each module.
Unsatisfactory attendance may result in terms being deferred or denied. Please also refer to the
UOC policy on Student Leave in this handbook. In cases of absence due to il ness of more than 3
days, a medical certificate should be presented to the module administrator or Undergraduate
Administrator.
Communication
We cannot emphasise enough how important it is that you check and clear your student
email regularly, preferably on a daily basis as this is the best and fastest way that we wil get
information to you including important announcements. Please empty your mailboxes on a
regular basis so you don’t go over quota and miss important emails. If you have any problems
with your email please contact [email address] or 0800 479 888.
eVision Portal
o eVision is your online tool for applying to study, for accessing important study-related
information and for viewing your personal details and updating your contact details while
you study at Otago.
o eVision is your portal to other important University of Otago online applications. Access
timetable information, Blackboard, Student Webmail, the library catalogue and more
from one convenient place.
o Check ou
t http://www.otago.ac.nz/evision
Note: Please advise the Undergraduate Administrator of any changes to your contact
details.
It is also important that you check your pigeonhole and noticeboards on the LG floor
regularly.
Forms
All forms required by students, e.g., Exam Impairment, Withdrawal etc, are available from the
Undergraduate Administrator. Some forms are available on MedMoodle, e.g. leave requests.
Internet Use
For full details of the University of Otago regulations on Information and Communication
Technology see http://www.otago.ac.nz/administration/policies/otago081840.html. Students
are also reminded that the various Hospital Boards have policies in place regarding internet use.
Note:
• No user may use ICT for the purpose of accessing, sending or attempting to send:
Objectionable Material, or abusive, fraudulent, harassing, threatening, or illegal content.
Cel phones, Tablets and Laptops
Please use cellphones, tablets and laptops in a considerate manner. Receiving calls, texting,
tweeting, and/or updating your Facebook status during tutorials is NOT acceptable behaviour.
Social Media and the Medical Profession
Recent incidents involving University of Otago medical students make this a timely reminder of
our ethical obligations when using any form of online social networking.
The internet immediately connects us with the public domain and we must continue to avoid
making comments that could be interpreted as breeching the boundaries of patient-doctor
confidentiality.
8
While blogging, tweeting and other social networking avenues are, for the most part, well
intentioned, there is the potential for these activities to have future adverse consequences. As
members of a professional community with high ethical standards, any comments, images and
material you may leave on a personal page could embarrass you when seeking future
employment.
A copy of the excellent “Guide to online professionalism for medical practitioners and medical
students” can be found on moodle. This is a wel -articulated, informed reference.
Remediation
Module convenors and clinical teachers work hard to identify students who, for whatever reason,
are not up to sufficient standard to pass their clinical rotation. It is hoped that by identifying
students who are having problems early more can be done to help them progress. Students who
fail a module or who have a significant Conditional Pass on their PASAF are identified by the
module convenor, discussed at Academic Progress Meetings and interviewed by the Associate
Dean Student Affairs (ADSA).
The fol owing table outlines the most common presenting problems and the suggested
outcomes:
Issues which may contribute to a fail or
Possible Outcomes
conditional passes
• Health & Welfare Problems
→ADSA for assessment and referral
or
Direct to Student Health
• Problems in a specific area or specialty → ADSA for identification of problem and
which can be readily addressed (eg
discussion re how to address it. (eg buy
Lateness)
alarm clock)
Alerting next module convenor
• Personality Issues or breaches of
→ ADSA for discussion, identification of
professional behaviour
problem and ongoing
monitoring.
Alerting next module convenor
Referral to Fitness to Practice Committee
• Generic Problems across Specialties
English Difficulties
→ ADSA and referral for help with
Difficulties adjusting to NZ culture
language.
Clinical deficiencies across specialties
including problems with communication
→ ADSA and referral for Clinical
skills and difficulty synthesising clinical
Remediation
information and planning management
Remediation Timing
Students who are required to complete remediation or re-sit an assessment may be given the
opportunity to do this during their next holiday break or at the end of the year, rather than with
the next module’s assessment. You are strongly advised to be prepared for this eventuality when
booking travel for your holidays so that you have the flexibility to change your plans. We also
strongly recommend that 4th year students do not book any end of year travel until they know
that terms have been awarded in November (date to be confirmed). Some students may need
to remain in Christchurch for remediation and re-assessment if terms are deferred.
Fifth year students should be aware that if they fail one or more modules they could be denied
terms or have terms deferred until more work is set and passed.
9
Student Leave Policy
It is expected that all students will attend all scheduled learning experiences. This particularly applies to
all laboratories in ELM and all block and vertical modules in ALM. It is however acknowledged that a
student may wish to have leave from time to time to attend to personal or extracurricular matters.
The granting of leave is discretionary and considered case by case.
Application for Leave
Students are required to seek approval for all leave, and should request leave in advance from the
appropriate convenor, supervisor or tutor.
In ALM, when any leave is taken an on-line Leave Request needs to be completed on MedMoodle (located
on each year’s homepage) and approved by the appropriate
block and vertical convenor(s). If the leave
requested is longer than 3 days it also needs approval from the Associate Dean (Student Affairs).
Any
leave of 3 or more days should be planned and requested wel in advance. Consideration of leave application
When deciding on leave applications, the following points will be taken into consideration:
- Learning or professional development opportunities afforded by the activity
- The family, or community importance of the student attending the activity
- Whether the student has extenuating personal circumstances
- Whether the student is participating in a national or international sporting or cultural event
- Whether the student is presenting, organising or representing a group at a conference or
meeting
- The length of leave relative to the activity
- The reason the activity cannot be undertaken during scheduled holidays
- The importance of missed teaching or assessment and the student’s ability to catch up on
missed activities
- The student’s total leave in that year and any other leave in that module
If students wish to discuss the process of student leave the Client Services administrator in the Medical
Education Unit can provide information.
If the student’s application for leave is denied by the module convenor they may appeal to the Associate
Dean (Student Affairs). An ultimate appeal could be made to the Dean.
If students wish to discuss the process of student leave they can direct their concerns to either the Student
Staff Committee or the UOC Curriculum Sub-Committee.
Sick Leave, Bereavement Leave or other emergency
If a student is unable to attend learning sessions or their module due to il ness or other reasons the
appropriate tutor, module convenor and the student affairs office must be notified on the first day of the
absence and on any subsequent days. The sick leave must also be recorded in the on-line leave request
in MedMoodle when you have returned to study. This is the student’s responsibility. It is important not
only because of missed learning opportunities, but also because staff frequently arrange clinics and
patients to be available for students, so need to know if the student wil not be present.
A medical certificate is required for any student absent because of illness for more than 3 days in ALM.
Note: part of professional responsibility is to absent yourself from work if you are ill in order to avoid
infecting vulnerable patients.
The length of time taken for bereavement leave is considered on an individual basis.
Dealing with missed sessions
Please note it is the student’s responsibility to arrange any necessary catch up with the module convenors.
If missed content cannot be completed within the module this will lead to a module result of incomplete
and a plan made to al ow completion.
Failure to contact the tutor/module convenor if a session cannot be attended is considered
unprofessional behaviour and wil be brought to the attention of the Student Progress Committee.
10
Students on Placement – Contact Details in eVision
All students on placement through the University of Otago must fill in the ‘override address’
section in eVision to provide details of where the University can contact you during your
placement period. By filling in the ‘Override’ address the University will be able to quickly contact
you with regard to any issues that concern the area where you are on placement. The University
is always concerned with the safety and well-being of its students and being able to locate you
quickly in an emergency is the first step to ensuring you are safe and getting the support you
need. Emergency contact information (e.g. the name and number of your mother, father,
spouse) is used in the event the University needs to contact someone on your behalf should you
be involved in or experience a health or safety emergency.
Trainee Intern Electives
You wil be given the opportunity in 4th year to select your preferred elective quarter for trainee
intern year. More information on the trainee intern elective will be provided on Moodle and at
the 4th Year Elective evening.
UOC Gold Medal Teaching Awards
Awarded for excellence in teaching
1993 B M Colls 2009 AG Rothwell 2018 MW Ardagh
1994 R Fraser TJ Wilkinson 2019 S Chambers
2003 GD Abbott 2012 JM McKenzie D Jardine
R Sainsbury 2013 JB Morton
2004 PF Bagshaw MG Nicholls
PW Moller 2014 SG Pitama
PJ Parkin 2015 L Beckert
2007 EJ Begg 2016 MA Hurrell
AP Miller
Research Opportunities
Research is the cornerstone of our teaching and learning activities here at the Christchurch
Campus. The quality of research in Christchurch is renowned international y and is a vital factor
in maintaining the quality of health services in a tertiary teaching hospital and health service.
The Campus is very fortunate in that it hosts a number of very strong research programmes and
groups and amongst its staff has many researchers with an international reputation. The
Christchurch Campus hosts a number of programme grants funded by the Health Research
Council of New Zealand and enjoys research funding support from the Canterbury Medical
Research Foundation, Lottery Health, the Cancer Society, and other grant-funding bodies.
We encourage you to take an interest in research during your time here at Christchurch. The
campus is host to a large number of research meetings and seminars and these are advertised
via email and on our postgraduate noticeboards.
The Research Office, Level 5 of the main Campus building, co-ordinates all information about
research, research grants and funding opportunities. Please feel free to visit the Research Office
or visit the Campus’ Research web site,
www.uoc.otago.ac.nz/research for a list of researchers
and research groups and some of the projects that are presently underway.
Summer Studentships
If you would like to spend ten weeks over the summer vacation on a research project, email the
Christchurch Research Office
([email address]) for the Summer Studentship Project
List, available from early September. These Summer Studentships are a great introduction to
11
research and there are prizes for the best oral presentations of the research summaries. The
projects commence in October/November and students receive a scholarship of $5,000. The
Summer Studentship Handbook and al the information you wil need to apply for a Summer
Studentship is available on the School’s website at:
www.uoc.otago.ac.nz/research/summer.htm or from the Research Office on Level 5, University
of Otago, Christchurch building.
Bachelor of Medical Science (Hons)
If you would like to become more seriously involved in research you do not have to wait until you
are qualified. You can take a year out to do a Bachelor of Medical Science (Hons) – the details
are in the University Calendar and we can also put you in touch with other BMedSc students.
This involves a thesis and there is a good chance that you wil be able to publish your results in
an internationally recognised scientific journal. You will also be in a strong position to follow on
with an MMedSc or PhD at a later date. Research experience not only looks good on your CV,
but also will give you a more critical and informed approach to medicine. If you might be
interested in undertaking a BMedSc please make contact with Ruth Helms, Medical Education
Unit, ground floor, UOC building, to discuss this option.
Further information available on the Otago Medical School website:
http://www.otago.ac.nz/courses/qualifications/bmedschons.html
12
YEAR 4 PROGRAMME 2021
Welcome from the Dean
On behalf of the staff at the University of Otago, Christchurch, welcome to Advanced Learning in
Medicine.
Commencement of Year 4, with the shift to clinically based learning, is something of a "rite of
passage", a new stage in the progression to professional practice. The complexities of diagnosis
and management, and of the health care system, and the poignancy of the emotions and life
changes encountered by patients and their families, take on a new urgency and reality. We hope
the learning environment of the Christchurch campus and the Canterbury health care services
will provide a firm foundation for effective and empathic clinical practice in the years ahead.
In addition to its medical education role, the Christchurch campus has over 700 postgraduate
students enrolled in a variety of programmes to PhD level. The campus is also the primary centre
for health research in the Canterbury region, with a wide range of internationally recognised
research programmes. Your learning environment is enhanced by these postgraduate and
research activities.
Your Year 4 Course Handbook provides general information which you will need to know for your
clinical training in Christchurch's hospitals and other health services. It also outlines our
expectations of you as you become part of the clinical team, and gives details of specific modules.
Please read the Course Handbook carefully, to familiarise yourself with the School and your 4th
Year programme, and essential issues relating to patient care, ethics, confidentiality of
information, patient rights, and your own roles and responsibilities.
In the course of your clinical training you wil be encouraged to think for yourself, to become
comfortable with "self-directed learning", to move from theoretical to case-based learning, and
to engage with the lifelong task of becoming a responsible and competent health professional.
Your challenge, as you proceed from early to advanced learning in medicine, will be to acquire or
enhance the knowledge, skil s and attitudes through which you can best serve your patients and
the wider community in the years ahead.
Best wishes for a stimulating and satisfying year.
Professor David Murdoch
Dean
13
Course Overview
Years 4 and 5 have been designed to help you apply your knowledge to practical situations and
to help you develop from a student to an apprentice doctor.
The course has a series of block modules and vertical modules. In Year 4 there are 2 four week
modules and 3 eight week modules and you will rotate through each of them. Some topics are
better learnt over longer periods of time and are therefore organised as vertical modules that
run over the entire year.
The Pathology and Radiology vertical modules occur mostly on Thursday afternoons. Other
vertical modules wil be taught in dedicated teaching half days throughout the year. These are
Addiction Medicine (Y5 only), Clinical Pharmacology (Y5 only), Clinical Skills, Ethics and Law,
Hauora Maori, Palliative/End of Life Care, Professional Development, and Quality and Safety.
The best way to get the most of your year is to take as many opportunities as you can to meet
patients, to find out about their problems and then to synthesise this with your theoretical
knowledge. We encourage you to read about the conditions that your patients have. This is a
great way to help your theoretical knowledge “stick” in your mind. You will never know
everything so learning to identify important gaps and working out ways to fill them are important
lifelong skil s. Don’t expect therefore to be taught everything. Rather, by seeing the common
and important conditions in your patients we hope you wil be stimulated to identify and
prioritise your own learning.
14
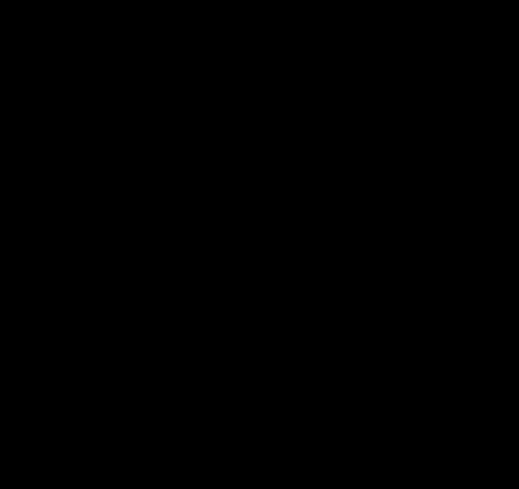
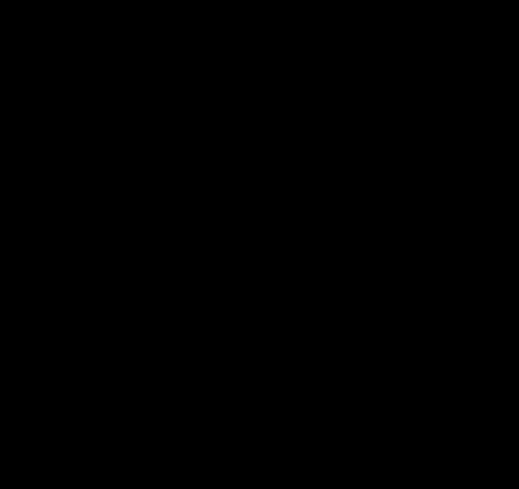
 University of Otago, Christchurch
Year 4 Advanced Learning in Medicine Modules
Public Health (3 wks)
Older Persons Health
Addiction Medicine (1wk)
(OPH)
(PHAM)
Surgery
Emergency/
University of Otago, Christchurch
Year 4 Advanced Learning in Medicine Modules
Public Health (3 wks)
Older Persons Health
Addiction Medicine (1wk)
(OPH)
(PHAM)
Surgery
Emergency/
•
Clinical Orientation
Gastroenterology/GI
•
Clinical Skills
Surgery
•
Ethics and Law
(SEGO1)
•
Hauora Maori
•
Pacific Health
General
•
Palliative and End of Life Care
•
Pathology (including Anatomical, Haematology, Clinical
Practice
Surgery
Chemistry and Microbiology)
(GP)
Oncology/
•
Professional Development
Haematology
•
Quality and Safety
(SEGO2)
•
Radiology
Cardiovascular
Cardio/Respiratory
Plastics, Dermatology
Medicine
(CVPD)
(CR)
Block Modules
- - - - - - - Vertical Modules
15
2021 Year 4 Groups – 15 January 2021
Group A
Group B
Group C
Group D
BOYCE Caitlin (Catey)
BARUGH Julia
BAJUNAID Mishal
BLAY Lucy
BROCHERIE Paris
BROWN Liam
BLAND Caitlin
FENG Yuyi (Jenna)
BURGESS Alice
CAO Helen
COATES Patrick (Paddy)
HALPIN Lewis
CAMERON-DUNN Samuel (Sam)
DHAKAL Rishav
DUNN Georgia
HU Gerald
CHUAH Joshua (Josh)
HAYES William (Jimmy)
HARTLEY Ella
LEADLEY Connor
FROELING Julia
HELU Tatila
HYNES John
MAYHEAD Anneke
KERSHAW Zachary (Zac)
HUNT Louise
JU William
MURRAY Cerianne
McCULLOUGH Benjamin
HUTCHINSON Joseph (Joe)
KAYES Julia
ORANGE Luke
PAGE Maya
LEE Justin
KEENAN Brydie
SOMERVELL Emma
PAIRMAN Lorna
McVICAR Nina
KUMAR Shiristi
THOMPSON Nasya
SEARLE Jordon (Jordan)
RICHARDSON Georgia
MacDONELL Nathan
van TURNHOUT Andrea
SHEPHEARD Tess
TAYLOR Millicent (Millie)
NICOLL Fiona
WHARTON Grace
SHERIDAN-ALEFOUNDER Ashlyn
van der LINDEN Jacinta
SWAN Meg
WILLIAMS Zoe
WILLIAMS Jasmyn
WILDING Susannah
TAIT Samantha
Group E
Group F
Group G
Group H
BAILIE-BELLEW Grania (Arni)
BOS Imogen (Imo)
BROWN Caitlin
ARNOLD Kate
BECKETT Olivia
CONNER David
DYSON Georgia
BARBAFIERA Bianca
DU Qingfeng
GOH Jerry
GOESSI Jacob
ENDERSBY Lara
HENDERSON Benjamin (Ben)
KRAUSS Robin
GOH Ashleigh
GENT Oliver
HONEYFIELD Zoe
LAY Rose
HOLDAWAY Mark
GUEST Megan
JORDAN Justin
McKEEMAN Alysha
HU Albert
KERSHAW Campbel
KAW Anu
MORETON Hannah
MAHER Hannah
KIM Ye Kyung
MANNING Bryony
NATHU Priyanka
MITCHELL-WITEHIRA Ariana
LAING Erica
McDONALD Kato
REYNEKE Josua (Bernard)
PETRIE Mack
LI Ruijian (Ritchie)
MILLS Sophie
ROXBURGH Erin
REAY Charlotte
McCALL Poppy
MILNE Lachlan (Lachie)
SHAJI Emmanuel
STEVENSON Elizabeth (Lizzie)
PERRY Adelaide
SHARP Samantha
TOMKINS Samuel
SU’A Taliah
WARD Joshua
WEHI-HOUGHTON Maia
WANG Analise
TAY Yan Hao
WILLIAMS Georgia
YOUNG Nicholas
WELSH Emma
16
2021 Year 4 Rotations
Module
Dates
GP
CR
CVPD
OPH
PHAM SEGO1 SEGO2
Semester 1
15/2-12/3
A
B
C
D
E
F
G
H
15/3-16/4
B
A
D
C
F
E
H
G
19/4-14/5
C
D
A
B
G
H
E
F
17/5-11/6
D
C
B
A
H
G
F
E
Semester 2
28/6-2/7
Y4 Whole Class Teaching Week
5/7-30/7
E
F
G
H
A
B
C
D
2/8-3/9
F
E
H
G
B
A
D
C
6/9-1/10
G
H
E
F
C
D
A
B
4/10-29/10
H
G
F
E
D
C
B
A
GP
General Practice
CR
Cardio/Respiratory
CVPD
CardioVascular, Plastics, Dermatology
OPH
Older Person’s Health
PHAM
Public Health (3 weeks) / Addiction Medicine (1 week)
SEGO 1 & 2 Surgery/Emergency Medicine/Gastroenterology/Oncology
17
Summary of Year 4 Modules 2021
Gr
1
1
1
1
5
2
6
4/
ou
5/
5/
9/
7/
/7
/8
/9
10
p
1
3
4
5
-30
-3/
-1/
-1
-
-
-
-
2/
16/
14/
11/
/
9
10
29/
3
7
4
5
6
10
ARNOLD Kate
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
BAILIE-BELLEW Grania (Arni)
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
BAJUNAID Mishal
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
BARBAFIERA Bianca
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
BARUGH Julia
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
BECKETT Olivia
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
BLAND Caitlin
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
BLAY Lucy
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
BOS Imogen
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
BOYCE Caitlin (Catey)
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
BROCHERIE Paris
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
BROWN Caitlin
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
BROWN Liam
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
BURGESS Alice
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
CAMERON-DUNN Samuel
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
CAO Helen
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
CHUAH Joshua
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
COATES Patrick (Paddy)
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
CONNER David
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
DHAKAL Rishav
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
DU Qingfeng
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
DUNN Georgia
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
DYSON Georgia
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
ENDERSBY Lara
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
FENG Yuyi (Jenna)
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
FROELING Julia
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
GENT Oliver
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
GOESSI Jacob
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
GOH Ashleigh
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
GOH Jerry
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
GUEST Megan
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
HALPIN Lewis
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
HARTLEY El a
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
HAYES Wil iam (Jimmy)
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
HELU Tatila
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
HENDERSON Benjamin
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
HOLDAWAY Mark
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
HONEYFIELD Zoe
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
HU Albert
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
HU Gerald
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
HUNT Louise
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
HUTCHINSON Joseph
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
HYNES John
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
JORDAN Justin
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
18
Summary of Year 4 Modules 2021
Gr
1
1
1
1
5
2
6
4/
ou
5/
5/
9/
7/
/7
/8
/9
10
p
1
3
4
5
-30
-3/
-1/
-1
-
-
-
-
2/
16/
14/
11/
/
9
10
29/
3
7
4
5
6
10
JU Wil iam
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
KAW Anu
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
KAYES Julia
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
KEENAN Brydie
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
KERSHAW Campbel
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
KERSHAW Zachary
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
KIM Ye Kyung
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
KRAUSS Robin
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
KUMAR Shiristi
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
LAING Erica
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
LAY Rose
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
LEADLEY Connor
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
LEE Justin
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
LI Ruijian (Ritchie)
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
MACDONELL Nathan
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
MAHER Hannah
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
MANNING Bryony
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
MAYHEAD Anneke
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
MCCALL Poppy
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
MCCULLOUGH Benjamin
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
MCDONALD Kato
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
MCKEEMAN Alysha
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
MCVICAR Nina
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
MILLS Sophie
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
MILNE Lachlan
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
MITCHELL-WITEHIRA Ariana
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
MORETON Hannah
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
MURRAY Cerianne
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
NATHU Priyanka
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
NICOLL Fiona
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
ORANGE Luke
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
PAGE Maya
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
PAIRMAN Lorna
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
PERRY Adelaide
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
PETRIE Mack
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
REAY Charlotte
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
REYNEKE Josua (Bernard)
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
RICHARDSON Georgia
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
ROXBURGH Erin
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
SEARLE Jordon
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
SHAJI Emmanuel
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
SHARP Samantha
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
SHEPHEARD Tess
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
SHERIDAN-ALEFOUNDER Ashlyn A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
19
Summary of Year 4 Modules 2021
Gr
1
1
1
1
5
2
6
4/
ou
5/
5/
9/
7/
/7
/8
/9
10
p
1
3
4
5
-30
-3/
-1/
-1
-
-
-
-
2/
16/
14/
11/
/
9
10
29/
3
7
4
5
6
10
SOMERVELL Emma
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
STEVENSON Elizabeth
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
SU’A Taliah
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
SWAN Meg
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
TAIT Samantha
C
CR
CVPD
GP
GP
SEGO
SEGO
OPH
PHAM
TAY Yan Hao
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
TAYLOR Mil icent
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
THOMPSON Nasya
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
TOMKINS Samuel
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
VAN DER LINDEN Jacinta
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
VAN TURNHOUT Andrea
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
WANG Analise
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
WARD Joshua
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
WEHI-HOUGHTON Maia
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
WELSH Emma
G
SEGO
SEGO
OPH
PHAM CR
CVPD
GP
GP
WHARTON Grace
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
WILDING Susannah
B
GP
GP
CVPD
CR
PHAM OPH
SEGO
SEGO
WILLIAMS Georgia
H
SEGO
SEGO
PHAM OPH
CVPD
CR
GP
GP
WILLIAMS Jasmyn
A
GP
GP
CR
CVPD
OPH
PHAM SEGO
SEGO
WILLIAMS Zoe
D
CVPD
CR
GP
GP
SEGO
SEGO
PHAM OPH
YOUNG Nicholas
E
OPH
PHAM SEGO
SEGO
GP
GP
CR
CVPD
20
Clinical Orientation
Module Convenors: Prof Lutz Beckert and Prof Suetonia Palmer
[email address]
[email address]
Module Coordinator: Claire Willis
Contact Details:
Email: [email address]
Phone:
364 1642
Department of Anaesthesia, Lower Ground floor, Parkside East
The aim of Clinical Orientation (which is in conjunction with the introduction to Hauora Māori) is
to familiarise you to your clinical environment and prepare you for your clinical work. At the end
of the two weeks of the Clinical Orientation and Hauora Māori you should be able to:
• Identify the physical support structure assisting your learning including the library, computer
lab, seminar rooms, lecture theatres and the hospital layout including teaching facilities on
the wards.
• Recognise organisational support networks aiding your learning, and meet the people
involved including the Dean (Prof David Murdoch) and Dean’s office staff, the Associate Dean
Māori (Prof Suzanne Pitama), Associate Dean Undergraduate Student Affairs (A/Prof Tania
Huria), Education Adviser (Anthony Ali), Associate Dean of Medical Education (Prof Lutz
Beckert), module convenors, mentors and peers (Trainee Interns).
• Experience a working hospital alongside a Doctor and Nurse.
• Revise, practice and interpret a patient’s presenting symptoms, history of presenting
complaint and past medical history.
• Revise and practise some of the clinical examination skills you have learnt in ELM 2 and 3.
• Appreciate collaborative work, small group work and peer support to achieve clinical learning
outcomes.
• Learn and practice a clinical model to work with Māori patients and whānau.
There will be no formal assessment at the end of Clinical Orientation (although there is an
assessment component for the clinical orientation to Hauora Māori).
If you have any questions about any of the Clinical Orientation module, please don’t hesitate to
contact us.
21
Older Persons Health Module
Module convenors:
Dr Hamish Jamieson / Dr Michaela Glanville / Dr Kate Eggleston
Module administrator: Anne Vernall
Contact details:
Shared Services Division / Department of Medicine
Portacom C
Burwood Hospital, 300 Burwood Road
Phone: 337 7918 – Burwood Office
Phone: 364 0825 – Christchurch Hospital Office
E-mail: [email address]
The focus of this module is the assessment, treatment and rehabilitation of older people to help
them to improve their functioning and quality of life. With the ageing of New Zealand’s
population this is everyone’s business rather than a purely specialist area of medicine or surgery.
You wil have opportunities to see patients in the wards and hopefully to accompany staff on
community visits into patients’ homes. You wil see how a range of health professionals work as
a team to enhance and promote independence with older people.
This module aims to help you improve your general clinical skills but you will also have particular
opportunities to learn how to examine the neurological system and a person’s mental state, to
conduct a psychiatric interview, and to learn about the particular needs of older people whose
independence is threatened.
Most patients stay longer at Burwood Hospital compared with the acute wards at Christchurch
Public Hospital, giving you good opportunities to get to know your patients and to see how the
team works alongside them and their care partners outside of hospital.
The objectives for this attachment are to:
1 Master a neurological examination
2 Obtain, collate and document a complete history and examination of an older person
3 Master the basic assessment and management of a person with dementia or delirium
Including:
• Taking a psychiatric history
• Performing a mental state examination, including bedside cognitive assessment
• Ordering appropriate tests
4 See and learn about common health problems for older people (in a variety of settings)
Including:
• Stroke
• Parkinson’s Disease
• Incontinence
• Falls
• Osteoporosis
• Frailty
• Appropriate prescribing
5 Display appropriate attitudes to older people and to col eagues
Seminar Room
There is a seminar room allocated for your use. This is located in Portacom C near Entrance 4 off
Mairehau Road at Burwood Hospital site.
22
Parking
You cannot park in front of Burwood Hospital. The car park is specifically for the use of members
of the public to use when attending the hospital as either a visitor or a patient.
The staff carpark is at the rear of the hospital through gate 5 off Mairehau Road.
The best parking is on Mairehau Road or the streets nearby
.
Computers
We have 3 University computers and a printer for your use connected to the School network and
2 DHB computers in Portacom C and 1 DHB computer located in the Librarian’s Office in Portacom
A. The CDHB network is available from ward computers in the hospital itself.
Lockers
Student lockers are available and also a key to Portacom C. You will be required to pay (in cash)
a $20 refundable deposit for these keys
on your first day. (We do not have Eftpos facilities). The
Portacom will be locked when unoccupied.
Medical Library
We have a medical library on site that has several text books on student reserve as well as a
number of journals and texts related to care of older people that are available for borrowing.
Textbooks and equipment
You don’t need to purchase any textbooks specifically for this attachment but a general medical
textbook is useful. Equipment to examine the neurological system is available but we encourage
you to bring your own tendon hammer and tuning fork. You should bring your stethoscope.
Revision
It is advised that you are familiar with the Cranial Nerve and Peripheral Nerve examination
techniques before the first day as we wil be building on the basic knowledge of these that you
gained prior to the rotation.
We look forward to meeting with you and we hope very much that you enjoy learning with us.
23
Public Health Medicine Module
Module Convenor: Dr Rose Crossin
Module Administrator: Shelley Morgan
Enquiries to: Department of Population Health
Email:
[email address]
[email address]
Orientation
On the first day of each attachment students should meet the module convenor on the 7th Floor
of the School at 9.00 am for the Public Health Introduction seminar. The room will be specified
in a welcome email sent the week before teaching begins.
Duration
The Public Health Medicine module is of three weeks duration, with the fourth week, Addiction
Medicine, being held at the National Addiction Centre. This module is part of the combined Older
Person’s Health and Public Health Medicine module.
Teaching
Objectives
The learning objectives for the Public Health Medicine module are grouped into ten areas:
• Burden of disease and injury among populations
• Cultural competence
• Determinants of health and their contributions to health outcomes and inequalities
• Global health
• Health systems
• Health advancement and reducing inequalities using frameworks of public health
including the Treaty of Waitangi
• Pacific health
• Population level thinking
• Research skills
• Statutory and clinical responsibilities in protecting populations and individuals
Learning objectives for the course are provided in the handbook, which will be distributed and
discussed with students at the beginning the module. Learning objectives are also described for
each session on Moodle.
Course Content
The course in Public Health Medicine will consist of seminars, case-studies, workshops, group
work (including a group project), and community visits. The main areas to be covered include:
•
Determinants of health and disease
•
Health promotion and disease prevention
•
Environmental health, including global climate change
•
Communicable disease surveillance and control
•
Public health research, including quantitative and qualitative research methods, study
design, and interpretation
•
Population health screening
•
Organisation and funding of health care, including the New Zealand health system and
health economics
•
The role of the community in the planning and delivery of health care
24
Seminars, case-studies, and workshops
A series of seminars, case-studies and workshops wil be held on the topics listed above and the
timetable and venues for these sessions wil be available at the beginning of the attachment.
Course Reading
All readings relevant to the public health attachment can be found on Moodle.
Student Assessment and Course Evaluation Terms:
The award of Terms will be dependent on satisfactory attendance and performance during the
module. Students are expected to attend al sessions unless prior permission has been granted.
Students wil be assessed on their contribution to the seminars, workshops and the group
presentation.
Formal Assessment:
Students will be required to participate in two formal assessment activities for the Public Health
Medicine module. These consist of a series of written assessment tasks and a group advocacy
project and presentation. Dates and other relevant details for these assessments will be
discussed on the first day of the attachment.
We look forward to meeting you and hope you wil find the Public Health Medicine module
interesting and enjoyable.
25
Addiction Medicine Module
4th Year Module Convenor: Prof Doug Sellman
Module Administrator: Lisa Andrews
Contact Details: National Addiction Centre
Department of Psychological Medicine
1st Floor, Terrace House, 4 Oxford Terrace
Phone: 372-6780
Email: [email address]
Introduction
We look forward to meeting you during the 4th year Addiction Medicine block course at the
University of Otago, Christchurch.
Addiction Medicine is a rapidly evolving medical specialty that has relevance to most other areas
of medicine. Addictive behaviours underpin many of the common conditions that people present
with in both primary and secondary care services, particularly mental health conditions and
gastrointestinal, cardiovascular and respiratory diseases.
The World Health Organisation estimates that tobacco, alcohol and illicit drugs are responsible
for
over 12% of deaths worldwide and
about 9% of disability (see
http://www.who.int/substance_abuse/facts/global_burden/en/). Over 90% of this morbidity
and mortality is from alcohol and tobacco rather than illicit drugs.
Alcohol and other substance use disorders are often undetected or undertreated. There are
several reasons for this, including patients’ denial, shame and stigma. However, clinicians’ lack of
knowledge or confidence in treating people with addiction problems also contributes to this
issue.
Therefore, our hope is that you will gain the skills to recognise these conditions whatever field of
medicine you are working in, as well as an awareness of treatments that are available and how
to access them. We find that most students experience a positive shift in their attitude and gain
confidence in interacting with people who are experiencing an addiction problem, as a result of
this course.
Course structure
Addiction Medicine is taught in a variety of ways across the three University of Otago campuses.
Here in Christchurch it is now split across 4th and 5th Year. The 4th Year course is a one-week
attachment which fol ows the three week course in Public Health, and forms part of the
combined Public Health and Addiction Medicine (PHAM) attachment.
Course materials
For the 4th Year module in 2021, a course booklet will be delivered into your pigeonhole by the
Friday before the commencement of the run. Please read the Introduction and bring this booklet
along with you on the first day of the Addiction Medicine attachment. The week long module
consists of a col ection of tutorials, discussion groups, clinical skills sessions, clinical interviewing
sessions and patient discussion groups. You wil also have a half-day clinical attachment at a
treatment programme.
You will also find a selection of course materials, including some of the powerpoint presentations
for the teaching sessions, on MedMoodle.
26
Assessment
The assessments for the 4th Year Addiction Medicine component of the PHAM module are:
1.
Formative assessment, includes three tasks:
a. A short report (300-500 words) of your attendance at a recovery group meeting (see
booklet for more detail on what to write about)
b. A brief, informal, oral presentation of your half-day clinical attachment. This can
involve visual materials (eg powerpoint) and is done together with any other
student(s) who attended the same attachment
c. A brief advocacy presentation (normally a brief letter to the editor – this will be
explained in class)
2. The
summative assessment for the course consists of an 8-minute OSCE on the final day
of the course, covering assessment and/or intervention skills (100%). The OSCE closely
fol ows the format of the end of 5th year OSCE exam, except that students will be given
brief direct feedback at the end of the exam. Students who do not pass the OSCE (score
above 60%) will be invited to resit, usual y within one week. If unsuccessful with the resit,
students will receive a conditional pass for the addiction medicine component of the
combined addiction / public health module, fol owing which a further resit or a viva exam
(or other remediative activities) will be organised.
It is a UOC requirement that you receive one final grade for the combined PHAM module. The
convenors of the two course components meet after every 2nd four week block to review marks
in the two components. The final outcome for the module (Distinction / Pass / CP / Fail) is
determined based on consensus between the module convenors. Students must receive a pass
grade for both components to pass the course, while it is possible to receive an overal distinction
based on outstanding performance in either component. Because of the requirement for the
public health and addiction medicine convenors to confer, we are typically unable to give you the
final grade until after this meeting has occurred.
27
General Practice Module
Module convenor: Dr Lynette Murdoch
Module administrator: Wendy Sincock
Contact details: Department of General Practice
14 Gloucester Street
Phone: 364 3613
Email:
[email address]
[email address]
On the first Monday morning of the module please report to the Department of General
Practice at 14 Gloucester Street. Half of you will be asked to come at 9.00am, the other half at
10.00am. We will e-mail you in advance so you know what time to arrive.
During the module you will participate in small group tutorials and gain clinical experience by
working with GPs. We wil contact you before the start of the module to al ow you to choose your
GP placements.
Details of the module, including most of the learning resources, are on Moodle and can be
accessed anytime. We will aim to have your timetable on Moodle the week before you start the
module.
We look forward to meeting you.
28
Cardio-Respiratory Medicine (CR) Module
Module Convenor:
Dr Geoff Clare
Department of Medicine
Module Coordinator: Fran Barrett
Department of Medicine
Ground floor, Parkside
Christchurch Hospital
Ph: 364 1116 (ext 81116)
[email address]
Please meet Dr Geoff Clare and Mr Jeremy Simcock at 9.00am on the first Monday morning of
the module in Room 704, 7th Floor, UOC Building for an introduction to the combined CR/ CVPD
modules.
The Cardio-Respiratory module and the Cardiology, Vascular, Plastics & Dermatology module are
integrated to al ow more patient centered learning. The two modules will be assessed as one and
results wil be finalised at the completion of the eight weeks. Students will receive a personalised
timetable at the beginning of the module.
For the four weeks of Cardio-Respiratory medicine, students will be allocated to ward based
clinical teams, have at least three bedside tutorials per week and have the opportunity to observe
cardiac catheterisation, cardiac exercise testing, echocardiography, bronchoscopies and lung
function testing. Whilst based on either Cardiology or Respiratory wards, students are
encouraged and expected to see patients from both specialties.
It is expected that students show a high degree of independent learning to cover the learning
objectives in Cardiology and Respiratory Medicine. We will support this with content related
lectures, small group tutorials (including topics such as systematic ECG analysis, smoking
cessation, GTN and asthma inhalers), a log book, practice MCQs (self-assessed), and weekly
‘signpost’ sessions to monitor progress. Preparation for teaching sessions from Moodle content
is vital for them to function efficiently and for full value to be gained.
The end of the module combined assessments will assess medical knowledge relevant to the
learning objectives via MCQs, assess the ability to take a history, perform a focused examination
and provide patient education via an OSCE, and assess the ability to gather, express and
synthesize clinical information through focused written case histories. In addition students will
have the opportunity to explore, in more depth, a topic that interests them via a short oral
presentation involving critical appraisal of a recent or landmark research paper.
Student engagement and feedback is essential for the success of this module.
29
CVPD Module
(Cardiology, Vascular Surgery, Plastic Surgery & Dermatology)
Module Convenor:
Mr Jeremy Simcock
Department of Plastic Surgery
Module Administrator:
Jane Marriner
Phone: 364 0640 Ext 80834
[email address]
Please meet Mr Simcock at 8.30am on the first Monday morning of the run in Room 704, 7th
Floor, UOC Building for an introduction to this module.
The Cardiology, Vascular Surgery, Plastic Surgery, Dermatology (CVPD) module and Cardio-
Respiratory (CR) module are integrated to allow more patient centered learning. Students wil
receive a personalised timetable at the beginning of the module.
Students on the CVPD module (4 weeks), in addition to whole group tutorials, will be allocated
to a range of clinical sessions in groups of 2 or 3. These include outpatient clinics and operating
lists at both Christchurch and Burwood Hospitals. These learning opportunities wil be scheduled
for all sessions except the two allocated to vertical module teaching (Tuesday pm and Thursday
pm). Students wil have the opportunity to complete self-directed study to cover the learning
objectives for the CVPD module at other times. A list of recommended reading will be provided
and preparation is expected prior to most sessions. A workbook will be provided to guide clinical
learning with a focus on student preparation, interaction and reflection. All other course
information and content are available on Moodle.
The end of module assessments will assess medical knowledge in the CVPD objectives via an MCQ
exam, assess the ability to take a history, perform a focused examination, interpret investigations
and provide patient education via an OSCE and assess the ability to synthesize clinical information
gained through focused case histories. In addition students wil have the ability to excel in a topic
of their choice through the preparation of an electronic poster presentation (e-Poster).
Student engagement and feedback is essential for the success of this module.
30
Surgery/Emergency Medicine/Gastroenterology/Oncology (SEGO) Module
Module Convenors: Mr Chris Wakeman (Overall SEGO Convenor and Surgery Convenor)
Ms Tamara Glyn (Surgery Co-Convenor)
Associate Professor Timothy Eglinton (Surgery HOD)
Professor Michael Ardagh (Emergency Medicine Convenor)
Associate Professor Catherine Stedman (Gastroenterology Convenor)
Professor Bridget Robinson (Oncology Convenor)
Dr Matthew Strother (Oncology Co-Convenor)
Module Administrator: Jennifer Van Dijk
Enquiries to: Ground Floor, 36 Cashel St
Telephone: 364 3634
Email:
[email address]
Please report at 7.55 am on the first Monday morning of the run to Room 706, 7th Floor, Main
University Building.
This eight week surgical module combines clinical areas that are closely aligned, namely
Oncology, Gastroenterology and Emergency Medicine. The surgical module is split into two parts,
Surgery & Gastroenterology, and Surgery & Oncology. Emergency Medicine is taught throughout
the eight weeks.
Your time will primarily be spent in Surgery. Your experiences in Oncology and Gastroenterology
are to extend and expand your comprehension of the diseases that may present to a surgeon
and to provide a more longitudinal appreciation of the clinical management of presenting
diseases.
Booklets including timetables and other course information for the module wil be handed to you
on your first morning.
All resources for the SEGO run (including learning objectives, assessment information,
31
Clinical Skills Vertical Module
Module Convenor: Dr Niki Newman
Module Convenor for 4th and 5th Year
Simulation Centre Director
Clinical Skills Director
Professional Practice Fellow
Em
ail: [email address]
Phone: (03) 364-3892
Module Administrator: Heather Reil y
Simulation Centre Administrator
Email: [email address]
Phone: (03) 364-3890
Simulation Centre |
Te Whare Whakataruna:
Level 1, 72 Oxford Terrace, Christchurch
Em
ail: [email address]
www.otago.ac.nz/christchurch/services/simulationcentre
Learning Outcomes:
Clinical Skills encompass all the skills used in the processes of consultation and management of patients. They
specifically include communication skills, consultation (includes communication, history, examination),
problem-solving (clinical reasoning), and procedural skills.
These skil s also contribute to the development of professional skil s and are not learned in isolation but
throughout al components of your programme, in particular during your block module clinical attachments.
During the three years of the Clinical Skills Vertical Module at UOC you will develop your professional and
clinical skills in a simulated clinical environment. By the end of the module you will be able to:
1. Demonstrate a range of professional behaviours and skills required of a newly graduated medical
practitioner.
2. Demonstrate the use of a systematic approach to the assessment and initial management of patients.
3. Demonstrate critical thinking and reasoning skil s during patient assessment, diagnosis (history,
examination, investigation) and initial management.
4. Perform procedural skills in a way which demonstrates safe, effective techniques and strategies to
minimise complications.
5. Be ready to apply clinical skills learned through simulation, to the real clinical learning environment.
Clinical Skills Programme
The Clinical Skills Vertical Module (CSVM) sessions are held on Monday afternoons and Tuesday afternoons in
4th year (and on one Wednesday afternoon), and Wednesday afternoons and Friday mornings in 5th year; at
the University of Otago Christchurch Simulation Centre, 72 Oxford Terrace, which is a scenic, seven minute
riverside walk from Christchurch Hospital.
MedMoodle
Please ensure you check the Clinical Skills MedMoodle pages regularly as they contain your timetable for the
year, the relevant resources to prepare you for each session, and other important information. Learning at the
Simulation Centre includes practical hands-on time and active participation, therefore we expect you to
prepare in advance of each session to help maximise your learning.
Assessment
Attendance and participation in all sessions of the Clinical Skills module is a ‘terms’ requirement. An absence
from any session without a satisfactory explanation and/or making up the missed session wil potential y
generate a conditional pass and may result in terms being denied. A register of attendance is maintained for
this module.
We look forward to seeing you at the Simulation Centre.
32
Ethics and Law Vertical Module
The ethics teaching in ALM is designed to build upon the ethics you did in ELM. It aims to extend
your sensitivity to and of understanding the concepts introduced in ELM, and to develop your
ability to apply them in a wide range of different areas of practice, particularly (though not
exclusively) in clinical situations. Through this you will become able to make complex ethical
decisions on the basis of sound ethical reasons.
Ethics is taught in tutorials which take place in each rotation. They are led by teachers from the
Bioethics Centre, sometimes with clinicians from the students’ current attachment. The ethical
issues taken up in each tutorial wil reflect those encountered on the attachment.
In some tutorials, students wil be expected to present cases for discussion and reflection by
tutors and class mates.
General supporting material is on Moodle. See the 'Introduction to Clinical Ethics', and the
glossary of key concepts introduced in ELM 2 & 3. Material for each class is also to be found on
Moodle.
Medical law is taught in ALM 5 during the mid-year whole class learning week. Legal concepts
are often raised and discussed in ethics classes. This reflects the close relationship between
ethics and law.
The overarching learning goals for ALM ethics are as follows:
To develop an understanding of and respect for the values that underpin medical practice
To be able to recognize ethical problems as they arise in medical practice
To develop the ability to apply ethical concepts to specific medical situations and programs
To be able to critically reflect on and participate in ethical discussion relevant to medical
practice
To develop the ability to make complex ethical decisions and to explain the reasons for
those decisions
In each year, students are expected to attend al four classes or to provide an explanation for
non-attendance. Non-attendance at two or more tutorials, even with an explanation, will be
referred to the Student Progress Committee.
In year 5 you will required to complete two assessments: a clinical ethics case analysis (as part
of a group), and a written clinical ethics case analysis. See the Moodle page for details. There
will also be a short answer question relating to ethics, law and professionalism in the end of
year exam.
33
Hauora Māori Vertical Module
Course Convenor: Maia Melbourne-Wilcox ([email address])
45 Cambridge Terrace
MIHI, Christchurch
Teaching Fel ow: Amber Philpott ([email address])
45 Cambridge Terrace
MIHI, Christchurch
The Māori/Indigenous Health Institute (MIHI) represents a major milestone in the development
of Māori focussed clinical teaching and health research at the University of Otago, Christchurch.
This Hauora Māori vertical module is hosted by MIHI and is carried out in accordance with our
mission statement:
To contribute to Māori health gain and capacity building through health research, training and
teaching.
The purpose of the Hauora Māori vertical module is to further develop your clinical competencies
in understanding the fol owing:
- Developing competencies in the application of Hauora Māori clinical models to clinical
practice.
- Understanding the role of clinicians in contributing to Māori health gains.
- Factors that contribute to continued health disparities between Māori and non-Māori in
New Zealand.
We know that you will enjoy the Hauora Māori vertical module and find it useful in your
professional development.
This year the Hauora Māori vertical module involves:
1. A combination of Immersed Integrated and Independent learning blocks.
2. The immersed teaching block for 2021 is at Ōnuku Marae, Banks Peninsula and occurs during
the first week of February.
3. Scheduled integrated (during block modules) Hauora Māori teaching sessions.
4. Immersed and Integrated teaching blocks wil build your knowledge and understanding of how
to apply key principles of Hauora Māori to your clinical practice.
5. All students will be required to complete two summative assessment and two formative
assessments within the Hauora Māori vertical module.
6. Your summative assessment within the vertical module will be matched to Immersed,
Integrated and Independent learning opportunities throughout the year.
7. Hauora Māori completes a PASAF of your overall performance, including attendance and
professionalism throughout the year.
34
Palliative and End of Life Care (PEOLC) Vertical Module
Module Convenor: Dr Amanda Landers
Nurse Maude Hospice Palliative Care Service
Module Administrator: Fran Barrett
Department of Medicine
Ground Floor, Parkside
Email: [email address]
Enquiries: [email address]
The PEOLC Module is new and evolving this year in its current format. The University of Otago
recognises the importance of caring for people with life-limiting illnesses and the need for all
medical professionals to have effective teaching in this area.
The purpose of this module is to equip you with the knowledge and skil s to provide quality care
to people facing the end of their lives, in a wide range of settings and including malignant and
chronic illnesses.
Essential skills will be taught in collaboration with other specialities such as Pharmacology, Ethics,
Anaesthetics/Pain Management, Hauora Maori and General Practice throughout 4th and 5th year.
It is a complex area of medicine and requires complementary experiences from many parts of
the curriculum. There is also dedicated teaching time in 4th and 5th year vertical sessions which
will focus on the four major principles: understanding palliative care, communicating effectively
with patients and their families/whanau, symptom management and the legal aspects of end-of-
life care.
Moodle
The PEOLC Moodle site will have important information and extra resources about each session.
It is important to read the site as it gives a step-by-step guide of any preparation you may need
to do before the session. It also links to other relevant parts of the curriculum/modules.
Assessment
Assessment is based on attendance and participation to make ‘terms’. An absence from any
session without a satisfactory explanation and/or making up the missed session will potentially
cause a conditional pass to be given and terms may be denied. A register of attendance is kept
and uploaded onto Moodle. Unsatisfactory attendance and participation may require an extra
small group tutorial at the discretion of the convenor.
In ALM4 there wil a short MCQ test in the last session requiring a 60% pass mark.
In ALM5 a presentation to the class will be part of the assessment for the year. It will not require
extra time outside of the session as all preparation will happen within the allocated module time.
Students will be required to have shown reasonable effort to pass.
35
Pathology Vertical Module
Head of Department:
Professor Martin Kennedy ([email address])
Module Convenors:
Anatomical Pathology:
Dr Andrew Miller ([email address])
Clinical Chemistry:
Dr Chris Florkowski ([email address])
Haematology:
Dr Sean MacPherson ([email address])
Microbiology:
Professor Steve Chambers ([email address])
Administration Team:
Enquiries to:
Alice Milnes (Administrator Client Services) or
Fran Cox (Administrator Client Services)
Level 2, School of Medicine building
Tel: 378 6381 (internal 86381)
E-mail: [email address]
Moodle
The Pathology Vertical Module has an active student resource in MedMoodle. Please note that
this site also has Radiology material related to the integrated Pathology-Radiology tutorials.
Please ensure that you check MedMoodle regularly as it will have up-to-date information on
weekly and semester timetables, lectures, handouts, images and other material relevant for your
course work.
If you find that a link doesn’t work or some information you require is not available on the
Pathology pages, please send an e-mail to [email address].
Teaching Programme
The Pathology programme is run over two years (Year 4 and Year 5). The formal component of
the programme comprises small and large group tutorials and lectures based around the major
subspecialties of pathology (Anatomical Pathology, Clinical Chemistry, Haematology and
Microbiology). All of these are assessed and contribute to terms and Potential Distinction.
Y4 Pathology teaching wil be on Thursday afternoon. Some of this teaching wil be combined
with the Y5 class. For many sessions there will be preparatory material which you wil be expected
to have completed before the session. Each Y4 student has the opportunity to attend an autopsy
on a Tuesday morning on a designated date - see the Autopsy roster on MedMoodle. If you wish
to attend the autopsy, please ensure that the time does not clash with your other commitments
on your rostered Tuesday morning. Attendance is not compulsory and you do not have to attend
if you do not wish to.
Details of each week’s programme are posted on MedMoodle and will be emailed to you. You
should consult the weekly timetable as this wil have the most current information on
venues/topics. Please note that the timetable may change at short notice.
There are in-course assessments in each of the pathology sub-disciplines: Anatomical Pathology,
Clinical Chemistry, Haematology and Microbiology. Satisfactory performance in the assessments
is a Pathology Terms requirement. Passes (or Passes after Conditions Met – PACM) are required
in at least THREE of the FOUR pathology sub-disciplines to obtain Terms in Pathology. The
Department provides ample opportunities for remediation for each assessment for any who fail
– our objective is to get you through al the assessments with a solid core of pathology learning.
We hope that you enjoy the Y4 Pathology course and look forward to meeting you. We
welcome you and your feedback.
36
Professional Development Vertical Module
Module Convenors:
Prof Bridget Robinson
Email:
[email address]
Dr Martin de Bock
Email: [email address]
A/Prof Tony Walls
Email:
[email address]
Dr Phil Adamson
Email:
[email address]
Welcome to Professional Development.
We will focus on the wider social contexts of medical practice that are not always encountered
during routine clinical care but are necessary for the future challenges you will face as a doctor.
Teaching sessions will be on Monday or Tuesday afternoon in fourth year and Wednesday
afternoon or Friday morning in fifth year. These sessions will be mostly small group interactive
learning opportunities with input from a variety of people from other professional
organisations and within the wider health team.
Assessment
Assessment and Terms is based on attendance at al four sessions during the year. If you are
unable to attend the session, you must email the administrator (as per Moodle information)
with your reason for not attending,
before the session takes place.
Making the transition from medical student to doctor is a huge challenge. We are sure you will
enjoy the professional development sessions and find them useful for developing your own
personal and professional attitudes needed for sound medical practice.
37
Quality and Safety Vertical Module
Module Convenor:
Dr Phil Hider
Department of Population Health
Email:
[email address]
Patient safety and quality improvement are becoming increasingly important in healthcare.
The ELM course introduced quality and safety as an important area for student learning and this
vertical module aims to build on that foundation. The programme allows discussion of a range of
factors related to patient safety, systems causation of adverse events both in medicine and other
industries, and various quality improvement methods and techniques. Improving the quality and
safety of patient care incorporates evidenced-based medicine, communication, patient-
centeredness, cultural competency and teamwork.
The module teaching sessions occur within the vertical module teaching times of Monday
afternoons in 4th year and Wednesday afternoons in 5th year. The sessions will involve a mixture
of exercises, presentations, discussions and self-directed work with a focus on prescribing and
medication safety. Some sessions will include opportunities for inter-professional learning.
There will be opportunities to consider issues related to the quality of patient care and patient
safety that students observe during their block modules.
• During the 4th year you will be asked to reflect on where patient harm may occur.
• During the 5th year you will be asked to consider an area where you think improvement is
necessary and suggest solutions.
Assessment
There is no PASAF for this Module. Assessment wil be based on attendance.
Contacts
If you have any questions about the course, please contact:
[email address]
38
Radiology Vertical Module
Module Convenor:
Dr Mike Hurrell
Radiology Department, Christchurch Hospital
This module is run in conjunction with the Pathology Department and is a weekly combined
Radiology-Pathology teaching session. Module documentation wil be handed out as part of the
Pathology materials, and this will direct you to websites for additional Radiology information.
A brief and excellent student-orientated textbook, David Lisle’s
Medical Imaging for Students, is
available on-line via the Canterbury Medical Library.
Four of the seven concurrent pathology tutorials held each week will include radiology questions
to be worked on. These topics can be discussed with a radiologist or radiology registrar when
they visit your group at 1600 hrs.
Each tutorial group must split into two small subgroups to facilitate constructive col egial
discussion and to get enhanced radiologist-student interaction. By discussing the radiology and
pathology findings with other members of your subgroup, it is hoped that these interactions wil
help you gain insights into the disease processes themselves, understand how the pathology is
reflected in the imaging, and encourage mutual professional cooperation and support
(collegiality).
Formal assessment is at the end of the year as part of the RadPath OSPE. This wil test three of
the tutorial topics worked on during the term using questions from the modules themselves.
Additional short MCQ self-tests are available on Moodle to check your understanding of module
topics. Although these tests do not contribute to your final grade, the results wil be useful to
guide your pre-OSPE revision, and encourage you to seek help if you need to. If you do not
understand something, ask the tutor during the tutorial, ask a knowledgeable classmate, or email
me (mike.hurrel @cdhb.health.nz) for assistance. I real y do want you to understand this core
material and pass the OSPE!
39
Awards for 4th Year Students
There are a number of Otago Medical School and UOC awards made at the end of the 4th, 5th
and 6th Year. The full awards list is available in the Dean's office. Several of these awards,
although presented at the end of the 5th Year, are given on the basis of achievement in the 4th
Year as well as in the 5th Year of the course.
The University of Otago, Christchurch Awards are:
Denis Stewart Award in Pathology
The Denis Stewart Award in Pathology was established by the New Zealand Society of
Pathologists to commemorate the outstanding contribution which Dr Denis Tiffin Stewart made
to pathology in al its aspects. The award is funded from a capital sum contributed by pathologists
throughout New Zealand and by members of the Christchurch medical staff. This sum is invested
by the Society.
The award is made annual y to the student achieving the highest standard in Pathology
throughout the 4th and 5th Years of the MB ChB degree course in the Christchurch School of
Medicine. It wil be awarded on the recommendation of the Dean and the Professor of Pathology
of the School.
Robin Carrell Award in Pathology
Established in 2006, this award is presented to the student achieving the highest standard in
Research Essays.
Ian Town Award for Excellence in Respiratory Medicine
Established in 2006, this award is presented for the best presentation on a respiratory topic at
the end of the Cardio-Respiratory module.
The Neil Columbus Award in Cardiology
This award was instituted in 1992 and shal be presented annually by the University Council on
the recommendation of the academic staff concerned to the 4th Year student enrol ed at the
University of Otago, Christchurch whose project presentation in the broad area of cardiology is
judged best of the year.
Plastic Surgery Award
Established in 2012, this award is presented to the 4th year student for the best e-poster
presentation on a Plastic Surgery topic at the end of the CVPD module.
Graham Riley Award in Health Care of the Elderly
Awarded annual y by the Health Care of the Elderly Education Trust to the top 4th Year student
in Health Care of the Elderly. It is to reflect Dr Graham Riley's interest in continuing the
advancement of teaching in Health Care of the Elderly.
ANZSGM Australia New Zealand Society of Geriatric Medicine Award
This award shall be presented to a person who in the year of the award is the best performing
4th Year medical student enrolled in the ‘Care of the Elderly’ clinical attachment in Dunedin,
Wellington and Christchurch campus (total of 3 awards).
AMI Award in Public Health
Established in 1994 by donation from the AMI Insurance Company. The award shall be presented
annual y on the recommendation of the Professor of Public Health in Christchurch to the 4th Year
student at UOC who has the best achievement in the Public Health module as determined by
consideration of results from the final examination and assessment of module work.
40
SEGO Award for Best Overall OSCE Mark in the Surgery/Oncology/Gastroenterology/
Emergency Medicine attachment
This award was instituted in 2001.
Department of Surgery Awards for Clinical Excellence in Surgery
There are four awards presented annually – one for each of the four groups for the best overall
OSCE mark on that module.
Chirnside-Morton Award in Emergency Medicine
Named after Mr Alan Chirnside and Mr John Morton, who established the first academic position
in Emergency Medicine in Australasia.
This award is presented annual y to the student who
achieves the best overall performance in Emergency medicine during the 4th Year of the MB ChB
degree course at UOC.
Maori/Indigenous Health Institute (MIHI) Hauora Maori Award
Established in 2016, this award is presented annually for general excellence in the ability to learn,
apply and engage in Hauora Maori in 4th Year.
4th Year Scholarships – Otago Medical School
These are available at http://micn.otago.ac.nz/current-students/scholarships/alm-years-4-6
41
42
FIFTH YEAR PROGRAMME 2021
Introduction from the Dean
Welcome to 5th Year - may the year be a rewarding and productive one for you.
The resources of Christchurch's hospitals and other health services wil provide you with an
excellent opportunity, through your 5th Year programme, to encounter the major areas of clinical
specialisation. The challenge of acquiring increasingly specialised knowledge and skills relating
to particular conditions must be complemented by an appreciation of and respect for the
individuality of each patient. Sir William Osler's advice to clinicians in 1899 was to "care more
particularly for the individual patient than for the special features of the disease." Osler's
challenge is still relevant today, perhaps more so given the complexities of modern medical
specialisation and sub-specialisation. It will be important also for you to grapple with the ethical
and societal issues which provide the wider context for clinical practice, at a time in medical
history when the demand for health care increasingly exceeds available resources.
Our campus is dependent not only on the excel ence of our clinical teachers, but also on the
world class research undertaken in Christchurch. Some familiarity with the School's research
activities will broaden your understanding of the close relationship between research and clinical
effectiveness, so take advantage of opportunities to attend research presentations. The School
has an international reputation for research across the clinical disciplines.
The examination at the end of 5th Year is generally seen as a major assessment hurdle, but for
those who have been conscientious through the year, the main challenges will be to integrate
and demonstrate what has been learned. Local and common components of 5th Year assessment
are directed toward the clinical and practical experience you will have had on the wards, in clinics,
and in the community. You should check carefully the requirements and objectives for each of
your clinical modules, and then make the most of the learning opportunities available to you.
The 5th Year programme offers an excel ent opportunity to extend your knowledge and skil s,
and enhance the attitudes and values central to your care of patients and their families. Best
wishes for a thoroughly productive and enjoyable year.
Professor David Murdoch
Dean
43
Course Overview
Years 4 and 5 have been designed to help you apply your knowledge to practical situations and
to help you develop from a student to an apprentice doctor.
The course has a series of block and vertical modules. There are 2 four week modules and 3 eight
week module in Year 5 and you will rotate through each of them. Some topics are better learnt
over longer periods of time and are therefore organised as vertical modules that run over the
entire year. The Pathology vertical module teaching occurs on Thursday afternoons. Other
vertical modules wil be taught in dedicated teaching half days throughout the year. These are
Addiction Medicine, Clinical Pharmacology, Clinical Skills, Ethics and Law, Hauora Maori, Palliative
and End of Life Care, Professional Development, and Quality and Safety.
The best way to get the most of your year is to take as many opportunities as you can to meet
patients, to find out about their problems and then to synthesise this with your theoretical
knowledge. We encourage you to read about the conditions that your patients have. This is a
great way to help your theoretical knowledge “stick” in your mind. You will never know
everything so learning to identify important gaps and working out ways to fil them are important
lifelong skil s. Don’t expect therefore to be taught everything. Rather, by seeing the common
and important conditions in your patients we hope you wil be stimulated to identify and
prioritise your own learning.
44
 University of Otago, Christchurch
Year 5 Advanced Learning in Medicine Modules
Women’s Health and
Developmental Medicine
University of Otago, Christchurch
Year 5 Advanced Learning in Medicine Modules
Women’s Health and
Developmental Medicine
•
Addiction Medicine
Paediatrics
•
Clinical Pharmacology
•
Clinical Skills
Advanced
•
Ethics and Law
Medicine
•
Hauora Maori
(
incl Neurology
•
Pathology (including Anatomical, Clinical
& Rheumatology)
Chemistry, Haematology, and Microbiology)
•
Palliative and End of Life Care
•
Professional Development
•
Quality and Safety
Psychological
•
Radiology
Medicine
Orthopaedics and Advanced Surgery
(Orthopaedics, Urology, Ophthalmology,
Otorhinolaryngology)
_____ Block Modules
-------- Vertical Modules
45
2021 Y5 Student Groups - 23 December 2020
Group A
Group B
Group C
Group D
BIDDLE Sarah
BLACKMORE Samuel (Sam)
BARNETT Isabella
BOWEN Emily
CHIM Michael
CARNEGIE Abigail (Abby)
BOTTING Tom
DAVEY Regan
FISHER Calum
DAVEY Drew
CAHILL Charlotte
DELPACHITRA Shenyll
FOOKES Victoria
DUTHIE Cassian
FRATER Jordan
JOHNSTON Phoebe
GWYNNE JONES Julia
KIM Jamin
ISAACS Rosie
MOOLENAAR Marcella
HARTLEY Rachael
LI Shelley
JONES Gavin
NOSA Jonathan
HILL Callum
MATTINGLY Ben
KIBBLEWHITE Christopher (Chris)
O’BYRNE Ellen
HOWARD Charlotte
McNAUGHTON Grant
LIU Yizhuo (Valery)
ROBERTSON Ella
KLADNITSKI Sergey
MOORE Amy
MORIARTY Samantha (Sam)
SCIASCIA Harris
MURRAY Toriana (Tori) semester 2 only SCHAFER Josephine
THOMAS Emily
SOWTER Daniela
SCHULZ Ailsa-Rose (Rosie)
SULLIVAN Grace
WOLYNCEWICZ Benjamin
SUTCLIFFE Oliver
TOWERS Sarina
WU Ruiqi (Rachel)
WOOTTON Alexandra (Alex)
Group E
Group F
Group G
Group H
BAIN Caroline
ADDY Kaleb
BEATTIE Harriet
APPLETON Jasmine
BANKIER Shane
APRECIO Merk
EASON Josephine (Josie)
CLARK Elinor
CHAND Raksheel
BATTY Anna
HUNTER Greer
GELL Billie
DE GRAAF Steven
CHUA Aquila
KATIPA-MAIKUKU Jacqueline (Jackie) HARTLEY Molly
ELPHICK-IAVETA Amelia
CLARK Rosa
MAKIN Mark
HAY Immanuel
LEWIS Claudia
DELPACHITRA Navodhi
MARTIN Gemma
KELLAND Scott
LISLE Stella
DONALDSON Jack
PAIN Daniel
LIM Angela
PEAT Samuel (Sam)
HUGHES Emilie
PHILLIPS Jazmin
MASTERS Luke
RIDGEN Michael
KAHU Hineari (Hine)
SEIDELIN Jasmine
MIDDELBERG Jessica (Jess)
RUDDLE Caitlin
MELLIS Isabella
WATSON Lachlan (Lachie)
PATERSON Jaimee
STANNERS Jessica
RUSSELL Kaden
WILLIAMS Nicola
WANG Dongfan (Mark)
THWAITES Julia
URQUHART Anna
YEE-GOH Anthony
RMIP
CLARKE Isabel
DELL Ceri
EVISON Isla
LINSCOTT Oliver
MEURILLON Lys
ON Sebastian
SOMERFIELD Amanda SONI Rutvi
TAYLOR William
WESTGARTH Sophie
WHEELER Annaliese
WHITCOMBE Hazel
46
UOC 2021 Year 5 Block Module Rotations
Dates
WHDM
PAED PSYC
OAS
ADV MED
Semester 1
9/2-5/3
A
B
C
D
E
F
G
H
8/3-1/4
B
A
D
C
F
E
H
G
12/4-7/5
C
D
A
B
G
H
E
F
10/5-4/6
D
C
B
A
H
G
F
E
8-11 /6
Y5 Whole Class Teaching Week
Semester 2
28/6-23/7
E
F
G
H
A
B
C
D
26/7-20/8
F
E
H
G
B
A
D
C
30/8-24/9
G
H
E
F
C
D
A
B
27/9-2210
H
G
F
E
D
C
B
A
26-29/10
Study Week
30/10-5/11
Exam Week
WHDM Women’s Health and Developmental Medicine (8 weeks)
PAED Paediatrics (4 weeks)
PSYC Psychological Medicine (4 weeks)
OAS Orthopaedics and Advanced Surgery (8 weeks)
ADV MED Advanced Medicine (including Neurology and Rheumatology) (8 weeks)
47
Summary of Year 5 Block Modules 2021
Gr
9/
8/
12/
10/
28/
26/
30/
27/
ou
2
3
p
-5/
-1/
4
5
6
7
8
9
-
-
-
-
-
-
3
7
4
2
2
2
22
4
/5
/6
3/
0/
4/
7
/
8
9
10
ADDY Kaleb
F
OAS
OAS
ADVM
ADVM
WHDM WHDM PSYC
PAED
APPLETON Jasmine
H ADVM
ADVM
OAS
OAS
PSYC
PAED
WHDM
WHDM
APRECIO Merk
F
OAS
OAS
ADVM
ADVM
WHDM WHDM PSYC
PAED
BAIN Caroline
E
OAS
OAS
ADVM
ADVM
WHDM WHDM PAED
PSYC
BANKIER Shane
E
OAS
OAS
ADVM
ADVM
WHDM WHDM PAED
PSYC
BARNETT Isabel a
C
PAED
PSYC
WHDM WHDM ADVM
ADVM
OAS
OAS
BATTY Anna
F
OAS
OAS
ADVM
ADVM
WHDM WHDM PSYC
PAED
BEATTIE Harriet
G ADVM
ADVM
OAS
OAS
PAED
PSYC
WHDM
WHDM
BIDDLE Sarah
A
WHDM WHDM
PAED
PSYC
OAS
OAS
ADVM
ADVM
BLACKMORE Samuel
B
WHDM WHDM
PSYC
PAED
OAS
OAS
ADVM
ADVM
BOTTING Tom
C
PAED
PSYC
WHDM WHDM ADVM
ADVM
OAS
OAS
BOWEN Emily (Mil y)
D PSYC
PAED
WHDM WHDM ADVM
ADVM
OAS
OAS
CAHILL Charlotte
C
PAED
PSYC
WHDM WHDM ADVM
ADVM
OAS
OAS
CARNEGIE Abigail (Abby) B
WHDM WHDM
PSYC
PAED
OAS
OAS
ADVM
ADVM
CHAND Raksheel
E
OAS
OAS
ADVM
ADVM
WHDM WHDM PAED
PSYC
CHIM Michael
A
WHDM WHDM
PAED
PSYC
OAS
OAS
ADVM
ADVM
CHUA Aquila
F
OAS
OAS
ADVM
ADVM
WHDM WHDM PSYC
PAED
CLARK Elinor
H ADVM
ADVM
OAS
OAS
PSYC
PAED
WHDM
WHDM
CLARK Rosa
F
OAS
OAS
ADVM
ADVM
WHDM WHDM PSYC
PAED
CLARKE Isabel
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
DAVEY Drew
B
WHDM WHDM
PSYC
PAED
OAS
OAS
ADVM
ADVM
DAVEY Regan
D PSYC
PAED
WHDM WHDM ADVM
ADVM
OAS
OAS
de GRAAF Steven
E
OAS
OAS
ADVM
ADVM
WHDM WHDM PAED
PSYC
DELL Ceri
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
DELPACHITRA Navodhi
F
OAS
OAS
ADVM
ADVM
WHDM WHDM PSYC
PAED
DELPACHITRA Shenyl
D PSYC
PAED
WHDM WHDM ADVM
ADVM
OAS
OAS
DONALDSON Jack
F
OAS
OAS
ADVM
ADVM
WHDM WHDM PSYC
PAED
DUTHIE Cassian
B
WHDM WHDM
PSYC
PAED
OAS
OAS
ADVM
ADVM
EASON Josephine (Josie) G ADVM
ADVM
OAS
OAS
PAED
PSYC
WHDM
WHDM
ELPHICK-IAVETA Amelia
E
OAS
OAS
ADVM
ADVM
WHDM WHDM PAED
PSYC
EVISON Isla
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
FISHER Calum
A
WHDM WHDM
PAED
PSYC
OAS
OAS
ADVM
ADVM
FOOKES Victoria
A
WHDM WHDM
PAED
PSYC
OAS
OAS
ADVM
ADVM
FRATER Jordan
C
PAED
PSYC
WHDM WHDM ADVM
ADVM
OAS
OAS
GELL Bil ie
H ADVM
ADVM
OAS
OAS
PSYC
PAED
WHDM
WHDM
GWYNNE JONES Julia
A
WHDM WHDM
PAED
PSYC
OAS
OAS
ADVM
ADVM
HARTLEY Mol y
H ADVM
ADVM
OAS
OAS
PSYC
PAED
WHDM
WHDM
HARTLEY Rachael
A
WHDM WHDM
PAED
PSYC
OAS
OAS
ADVM
ADVM
HAY Immanuel
H ADVM
ADVM
OAS
OAS
PSYC
PAED
WHDM
WHDM
HILL Cal um
A
WHDM WHDM
PAED
PSYC
OAS
OAS
ADVM
ADVM
HOWARD Charlotte
A
WHDM WHDM
PAED
PSYC
OAS
OAS
ADVM
ADVM
HUGHES Emilie
F
OAS
OAS
ADVM
ADVM
WHDM WHDM PSYC
PAED
HUNTER Greer
G ADVM
ADVM
OAS
OAS
PAED
PSYC
WHDM
WHDM
ISAACS Rosie
C
PAED
PSYC
WHDM WHDM ADVM
ADVM
OAS
OAS
JOHNSTON Phoebe
D PSYC
PAED
WHDM WHDM ADVM
ADVM
OAS
OAS
WHDM Women’s Health and
PSYC
Psychological Medicine
Developmental Medicine
PAED
Paediatrics
OAS
Orthopaedics and Advanced Surgery
ADVM
Advanced Medicine
RMIP
Rural Medical Immersion Programme students
48
Summary of Fifth Year Block Modules 2021
Gr
9/
8/
12/
10/
28/
26/
30/
27/
ou
2
3
p
-5/
-1/
4
5
6
7
8
9
-
-
-
-
-
-
3
7
4
2
2
2
22
4
/5
/6
3/
0/
4/
7
/
8
9
10
JONES Gavin
C
PAED
PSYC
WHDM WHDM ADVM
ADVM
OAS
OAS
KAHU Hineari (Hine)
F
OAS
OAS
ADVM
ADVM
WHDM WHDM PSYC
PAED
KATIPA-MAIKUKU Jacqueline G ADVM
ADVM
OAS
OAS
PAED
PSYC
WHDM
WHDM
KELLAND Scott
H ADVM
ADVM
OAS
OAS
PSYC
PAED
WHDM
WHDM
KIBBLEWHITE Christopher C
PAED
PSYC
WHDM WHDM ADVM
ADVM
OAS
OAS
KIM Jamin
B
WHDM WHDM
PSYC
PAED
OAS
OAS
ADVM
ADVM
KLADNITSKI Sergey
A
WHDM WHDM
PAED
PSYC
OAS
OAS
ADVM
ADVM
LEWIS Claudia
E
OAS
OAS
ADVM
ADVM
WHDM WHDM PAED
PSYC
LI Shelley
B
WHDM WHDM
PSYC
PAED
OAS
OAS
ADVM
ADVM
LIM Angela
H ADVM
ADVM
OAS
OAS
PSYC
PAED
WHDM
WHDM
LINSCOTT Oliver
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
LISLE Stel a
E
OAS
OAS
ADVM
ADVM
WHDM WHDM PAED
PSYC
LIU Yizhuo (Valery)
C
PAED
PSYC
WHDM WHDM ADVM
ADVM
OAS
OAS
MAKIN Mark
G ADVM
ADVM
OAS
OAS
PAED
PSYC
WHDM
WHDM
MARTIN Gemma
G ADVM
ADVM
OAS
OAS
PAED
PSYC
WHDM
WHDM
MASTERS Luke
H ADVM
ADVM
OAS
OAS
PSYC
PAED
WHDM
WHDM
MATTINGLY Benjamin
B
WHDM WHDM
PSYC
PAED
OAS
OAS
ADVM
ADVM
McNAUGHTON Grant
B
WHDM WHDM
PSYC
PAED
OAS
OAS
ADVM
ADVM
MELLIS Isabel a
F
OAS
OAS
ADVM
ADVM
WHDM WHDM PSYC
PAED
MEURILLON Lys
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
MIDDELBERG Jessica
H ADVM
ADVM
OAS
OAS
PSYC
PAED
WHDM
WHDM
MOOLENAAR Marcella
D PSYC
PAED
WHDM WHDM ADVM
ADVM
OAS
OAS
MOORE Amy
B
WHDM WHDM
PSYC
PAED
OAS
OAS
ADVM
ADVM
MORIARTY Samantha
C
PAED
PSYC
WHDM WHDM ADVM
ADVM
OAS
OAS
MURRAY Toriana -2nd sem A
OAS
OAS
ADVM
ADVM
NOSA Jonathan
D PSYC
PAED
WHDM WHDM ADVM
ADVM
OAS
OAS
O’BYRNE El en
D PSYC
PAED
WHDM WHDM ADVM
ADVM
OAS
OAS
ON Sebastian (Seb)
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
PAIN Daniel
G ADVM
ADVM
OAS
OAS
PAED
PSYC
WHDM
WHDM
PATERSON Jaimee
H ADVM
ADVM
OAS
OAS
PSYC
PAED
WHDM
WHDM
PEAT Samuel
E
OAS
OAS
ADVM
ADVM
WHDM WHDM PAED
PSYC
PHILLIPS Jazmin
G ADVM
ADVM
OAS
OAS
PAED
PSYC
WHDM
WHDM
RIDGEN Michael
E
OAS
OAS
ADVM
ADVM
WHDM WHDM PAED
PSYC
ROBERTSON El a
D PSYC
PAED
WHDM WHDM ADVM
ADVM
OAS
OAS
RUDDLE Caitlin
E
OAS
OAS
ADVM
ADVM
WHDM WHDM PAED
PSYC
RUSSELL Kaden
F
OAS
OAS
ADVM
ADVM
WHDM WHDM PSYC
PAED
SCHAFER Josephine
B
WHDM WHDM
PSYC
PAED
OAS
OAS
ADVM
ADVM
SCHULZ Ailsa-Rose (Rosie) A
WHDM WHDM
PAED
PSYC
OAS
OAS
ADVM
ADVM
SCIASCIA Harris
D PSYC
PAED
WHDM WHDM ADVM
ADVM
OAS
OAS
SEIDELIN Jasmine
G ADVM
ADVM
OAS
OAS
PAED
PSYC
WHDM
WHDM
SOMERFIELD Amanda
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
SONI Rutvi
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
SOWTER Daniela
D PSYC
PAED
WHDM WHDM ADVM
ADVM
OAS
OAS
WHDM Women’s Health and
PSYC
Psychological Medicine
Developmental Medicine
PAED
Paediatrics
OAS
Orthopaedics and Advanced Surgery
ADVM
Advanced Medicine
RMIP
Rural Medical Immersion Programme students
49
Summary of Fifth Year Block Modules 2021
Gr
9/
8/
12/
10/
28/
26/
30/
27/
ou
2
3
p
-5/
-1/
4
5
6
7
8
9
-
-
-
-
-
-
3
7
4
2
2
2
22
4
/5
/6
3/
0/
4/
7
/
8
9
10
STANNERS Jessica
E
OAS
OAS
ADVM
ADVM
WHDM WHDM PAED
PSYC
SULLIVAN Grace
B
WHDM WHDM
PSYC
PAED
OAS
OAS
ADVM
ADVM
SUTCLIFFE Oliver
D PSYC
PAED
WHDM WHDM ADVM
ADVM
OAS
OAS
TAYLOR Wil iam
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
THOMAS Emily
C
PAED
PSYC
WHDM WHDM ADVM
ADVM
OAS
OAS
THWAITES Julia
E
OAS
OAS
ADVM
ADVM
WHDM WHDM PAED
PSYC
TOWERS Sarina
A
WHDM WHDM
PAED
PSYC
OAS
OAS
ADVM
ADVM
URQUHART Anna
F
OAS
OAS
ADVM
ADVM
WHDM WHDM PSYC
PAED
WANG Dongfan (Mark)
H ADVM
ADVM
OAS
OAS
PSYC
PAED
WHDM
WHDM
WATSON Lachlan (Lachie) G ADVM
ADVM
OAS
OAS
PAED
PSYC
WHDM
WHDM
WESTGARTH Sophie
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
WHEELER Annaliese
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
WHITCOMBE Hazel
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
RMIP
WILLIAMS Nicola
G ADVM
ADVM
OAS
OAS
PAED
PSYC
WHDM
WHDM
WOLYNCEWICZ Benjamin C
PAED
PSYC
WHDM WHDM ADVM
ADVM
OAS
OAS
WOOTTON Alexandra
C
PAED
PSYC
WHDM WHDM ADVM
ADVM
OAS
OAS
WU Ruiqi (Rachel)
B
WHDM WHDM
PSYC
PAED
OAS
OAS
ADVM
ADVM
YEE-GOH Anthony
G ADVM
ADVM
OAS
OAS
PAED
PSYC
WHDM
WHDM
WHDM Women’s Health and
PSYC
Psychological Medicine
Developmental Medicine
PAED
Paediatrics
OAS
Orthopaedics and Advanced Surgery
ADVM
Advanced Medicine
RMIP
Rural Medical Immersion Programme students
50
Women’s Health and Developmental Medicine Module
Departments of Obstetrics & Gynaecology / Paediatrics / Psychiatry
Head of Department:
Dr Jo Gullam
Module Convenor:
Dr Jo Gullam
Paediatric Liaison: A/Prof Philip Pattemore
Child Psychiatry Liaison: Dr Katherine Donovan
Adult Psychiatry Liaison:
A/Prof Sue Luty
Module Administrator:
Francoise Hurt
Link Admin for Paediatrics:
Michele Armstrong
Link Admin for Psychiatry:
Lisa Andrews
Enquiries to:
University Department of O & G,
Level 3, Christchurch Women’s Hospital
Ph: 364 4630 (internal extn 85630)
E-mail: [email address]
Students should report to the University Department of Obstetrics and Gynaecology at 0830h
on the first day of the attachment.
Introduction
The current course was developed for 2011 and combines material from the disciplines of
Obstetrics and Gynaecology, Midwifery, Adult and Child Psychiatry, Adolescent Health, Neonatal
and General Paediatrics. This is an interactive and multidisciplinary approach to reproductive
and women’s health focussing on biopsychosocial development from conception to adulthood.
The run is intended to provide a basic introduction to women’s health and to the journey of
development from conception through childhood and adolescence to adulthood and beyond
menopause.
As well as comprehensive teaching from the individual specialities, there will be regular
multidisciplinary sessions with an emphasis on problem solving, communication and evidence
based practice.
The run is administered jointly by the above departments, with central coordination by the
Department of Obstetrics and Gynaecology.
Objectives
To attain proficiency in history taking and examination in Obstetrics and Gynaecology, Neonatal
Paediatrics and Adolescent Health.
To attain proficiency in history taking and examination in Adult Psychiatry relevant to pregnancy
and the Puerperium.
To gain an understanding of the principles of history taking and examination in Child and
Adolescent Psychiatry
To consolidate previous learning and acquire a sound knowledge of the curriculum relating to
above specialities.
To develop sound consultation and communication skills.
To use this knowledge base and clinical skill to formulate differential diagnosis and management
plans.
To understand critical appraisal of evidence and to use evidence to inform practice.
51
Teaching Programme
1. The introductory week comprises tutorials on essential topics and skills including history
taking and examination, informed consent, and communication. There will be no rostered
clinical duties during this week to enable al students to attend the sessions.
2. There follows a comprehensive six week programme of clinical work. This will include
sessions in Birthing Suite, Ante-Natal Clinics, Gynaecology Clinics and Theatre, Acute
Gynaecology Assessment Unit, Neonatal Paediatrics, Child and Adolescent Psychiatry,
Maternal Mental Health, Family Planning and Sexual Health. A supporting tutorial
programme will run simultaneously with material from all the clinical disciplines, Hauora
Māori and Ethics. Reference material and resources will also be available on Moodle. Some
of this teaching will take the form of long case scenarios and multidisciplinary case scenarios.
The students are expected to contribute actively to all sessions.
3. Week eight of the module is Case Presentations, MCQ and OSCE.
Details of these sessions can be found in the Module Handbook.
Assessment
Assessments will include:
1. Continuous assessment including feedback from clinical attachments.
2. Case presentation
3. Topic presentation
4. Logbook
5. Clinical Reflection fol owing the Youth In-Patient session
6. MCQ and OSCE examination modelled on the end of year assessments.
The module has been designed to offer a solid grounding in the various disciplines, whilst
encouraging a holistic approach to the problems encountered in day to day practice.
Please also refer to documents located under Module Info on MedMoodle. We look forward to
welcoming you to the module.
52
Paediatrics Module
Module Convenor: Assoc Prof Tony Walls
Module Administrator: Michele Armstrong
Contact Details: Department of Paediatrics
3rd Floor, Terrace House, 4 Oxford Terrace
Phone: 372 6718
Email:
[email address]
[email address]
Students are to report to the Department of Paediatrics at 0845 on the first day of the module for
an introductory session with A/Prof Tony Walls in the Paediatric Seminar Room (opposite
Paediatrics Outpatient Dept, Lower Ground Floor, Riverside).
Paediatric experience in Christchurch consists of four weeks in 5th year and four weeks in 6th year, as
wel as neonatology, child development and behaviour during the 5th year Women’s Health &
Development module.
Tutorials are held in the morning/early afternoon in the paediatric department seminar room or at
Terrace House. These provide an introduction to Paediatrics, covering child assessment and common
paediatric conditions. Pre-tutorial preparation tasks and tutorial notes are available on Moodle. Each
run has a Global Health Classroom session – a group tutorial where we link with medical students in
either Samoa or Fiji to discuss cases.
Afternoons allow students to pursue self-directed learning and clinical experience. Students are
rostered to attend the Children’s Acute Assessment (CAA) unit and clerk acute admissions under
supervision. There are weekly bedside examination tutorials and smal group Mentor Sessions.
Visits to Plunket rooms, kindergartens, and either Ferndale or Al envale Special School have been
arranged to encounter normal and impaired development, and different child-learning
environments. You wil need to make your own way to these visits.
Assessments: You are required to obtain a pass in each of these components to gain terms:
1. Online learning modules: These need to be completed in the first 2 weeks of the run. Students
must obtain a pass mark for al of the tutorials combined and al learning modules must be
completed to obtain terms.
2. Logbook: Students list the age, sex, and diagnosis/problem list of all cases they have seen, write
a short discharge letter and brief discussion notes for one case. Students wil reflect on their
extramural visits (format to be discussed). The completed logbook is uploaded to Moodle.
3. Clinical Skills Checklist and Mini CEX: Students are expected to develop confidence in handling
babies, and interacting with toddlers, older children and adolescents, along with their parents.
Students carry a checklist of bedside clinical skills to be observed during the attachment. Students
are also required to have two mini Clinical Exams (Mini CEX) rated by Registrars or Consultants.
The checklist and Mini CEX are uploaded to Moodle.
4. MCQ: A Moodle-based MCQ, based on common clinical paediatric issues, is held in the last week.
A pass requires 60% correct answers. Most issues are covered in the coursework, but some topics
such as rheumatology, pharmacology/poisoning, dermatology are not, so some general reading
in the recommended textbooks and articles is required. The MCQ bank is available on Moodle.
5. A communication skills test (OSCE) with two stations is held in the final week.
6. Module tutors will comment on your attitudes, attendance and participation – including your
completion of pre-tutorial on-line exercises.
Module resources are available on Moodle. A clinical examination techniques booklet and a clinical
experience checklist wil be given to you during your orientation session on the first day. We look
forward to seeing you then.
53
Psychological Medicine Module
Module Convenor: Dr Ben Beaglehole
[email address]
Module Administrator: Lisa Andrews
1st Floor, Terrace House, 4 Oxford Terrace
372 6780
[email address]
Students should report to the reception area of Te Awakura, Hil morton Hospital (Annex Road)
on the first Monday of their four week module for their orientation. You wil be advised by
email of the reporting time the week prior to the start of the run.
Each student will be attached to a clinical team and be expected to participate as a member of
this team. Students wil review patients with the consultant psychiatrist and psychiatric registrar
from each team and be expected to see patients on their own to gain experience in taking
psychiatric histories. Possible attachments include acute inpatient psychiatry, rehabilitation
psychiatry, old age psychiatry, youth inpatient psychiatry and mothers and babies psychiatry.
For interested students, arrangements can be made to attend outpatient clinics and spend time
with junior doctors on call.
Detailed information on the run can be found on Moodle.
54
Orthopaedic and Advanced Surgery Module
Orthopaedic and Advanced Surgery Module
Orthopaedic Surgery
Module Convenor: Mr Ramez Ailabouni and Professor Gary Hooper
Module Administrator: Jane Marriner
Department of Orthopaedic Surgery and MSM
Lower Ground Floor, Parkside West
Phone 364 0640 (Extension 80834)
Students wil be emailed the week before the start attachment advising where and when the
introduction to the module wil be held.
The Orthopaedic Surgery side of the module combines attachments to orthopaedic surgery,
musculoskeletal medicine, spinal injuries and rehabilitation. There is teaching input from clinical
pharmacology, pathology and radiology. The aim is for you to gain understanding and
competence in the following general objectives.
The Objectives of the Course are to:
1.
Become competent in the clinical interview of patients with musculoskeletal disorders
2.
Become competent in the examination of the musculoskeletal system especially of the
hand, shoulder, hip, knee and spine
3.
Gain a sound knowledge of common musculoskeletal conditions
4.
Learn the principles of management of acute and established musculoskeletal conditions
5.
Understand the impact of musculoskeletal disorders on the individual, the family and the
community.
Teaching Programme
Orthopaedic clinics, tutorials and surgery
Pharmacology tutorials
Radiology and Pathology tutorials
Topic Presentations
Assessment
Assessments of knowledge, skills and attitudes are largely based on the following items:
• Structured Clinical Examination (OSCE) at the end of the run
• MCQ
• Pain Assessment
• satisfactory completion of patient Case Studies
• Patient based Topic Presentation – as allocated
The marking of the structured clinical examination is carried out after the exam to give immediate
feedback on performance.
We look forward to welcoming you to our programme.
Prof Gary Hooper
Convenor
Head of Department
55
Advanced Surgery
Module Convenors:
Ophthalmology: Associate Professor Mark Elder
Otolaryngology: Associate Professor Phil Bird
Urology: Mr Stephen Mark and
Dr Jane McDonald
Module Administrator: Jane Marriner
E
mail: [email address]
This eight week module combines Orthopaedic Surgery and the Advanced Surgery module
(Otolaryngology, Ophthalmology and Urology) which will be assessed as one. The results wil be
finalised at the completion of the eight weeks.
During the Advanced Surgery module you will participate in tutorials, undertake self-directed
learning from resources on Moodle and textbooks, and gain clinical experience by attending clinic
and theatre opportunities in Ophthalmology, Otolaryngology and Urology. There is teaching
input from Clinical Pharmacology, Pathology and Radiology.
All readings and resources relevant to the Advanced Surgery module wil be uploaded to Moodle.
You will receive a handbook which outlines the Orthopaedics and Advanced Surgery learning
objectives, timetable and module assessments at the orientation session on the first Monday of
the attachment.
Assessment
Assessments of knowledge, skills and attitudes are largely based on the following items:
• Patient based Topic Presentation – as allocated
• Clinical Scenario Assessment (Ophthalmology only)
• MCQ
We look forward to welcoming you to our programme.
56
Advanced Medicine Module
(General Medicine/ Neurology/ Rheumatology)
Module convenor: Assoc Prof David Jardine
Module coordinator: Fran Barrett
Department of Medicine
Ground floor, Parkside
Phone: 364 1116 ext: 81116
Email: [email address]
Students wil be divided into two groups at the start of the combined attachment. Those doing
General Medicine for the first four weeks wil report to the General Medicine morning
handover meeting at 8.00am in the Great Escape Café annex and al be joined by the second
group at 8.30am for an introduction to Neurology and Rheumatology.
You will attend clinics and tutorials in Endocrinology, Diabetes, Nephrology, Neurology,
Rheumatology and Clinical Pharmacology. Skills will be assessed in a combined OSCE (General
Medicine/ Neurology/ Rheumatology) and combined MCQ assessment, based on ward teaching,
clinics and tutorials, during the final week of the combined eight week module.
General Medicine
Each student is attached to a General Medicine team at Christchurch Public Hospital and will see
acute admissions under their teams. They will also be able to follow these patients on the wards.
Most of the teaching in General Medicine is ward based. You will be taught history taking,
physical examination and differential diagnosis. These skills will be assessed in a combined OSCE
(General Medicine/ Neurology/ Rheumatology) on the last Wednesday of the run.
Textbooks to buy before starting:
Clinical examination: A guide to systematic physical diagnosis - Tally and O’Connor
We also recommend that you buy either the Oxford Textbook of Medicine or Harrison’s
Principles and Practice of Internal Medicine
Equipment required:
stethoscope
reflex hammer
watch with a second hand
tape measure
small torch
Neurology
To provide proficiency in the basic clinical skills of interviewing and examining patients with
neurological and neurosurgical disorders.
To introduce the student to the methods of problem solving used in diseases of the nervous
system.
To introduce the student to the commonest and most important neurological disorders.
Detailed Skills Objectives
Students will acquire and demonstrate their proficiency in the following skills:
Take a neurological history
Examine higher mental function
Examine the peripheral nervous system
Examine the cranial nerves
Write up neurological and neurosurgical cases
Interpret neuroradiological investigations
Understand the principles and purpose of electrophysiological studies
57
Rheumatology
History: Become competent in the clinical interview of patients with rheumatological
disorders.
Examination: Become competent in the examination of the musculoskeletal system especially
of the hand, hip, knee and spine, GALS screening examination.
Investigations: To understand the characteristics that make a diagnostic test useful and to
demonstrate appropriate use and interpretation of commonly used laboratory tests in
musculoskeletal disorders.
Attitudes: Understand the impact of musculoskeletal disorders on the individual, the family
and the community.
Knowledge: Gain a sound knowledge of common musculoskeletal conditions including their
management.
58
Clinical Pharmacology Vertical Module
Module Convenors:
A/Prof Matt Doogue 364 1055 (81055)
Dr Paul Chin 364 9671 (89671)
Module/Departmental Secretary:
Jasmin Metcalf 364 1858 (81858)
Department of Clinical Pharmacology
Department of Medicine, Ground Floor, Parkside
Overview
Clinical pharmacology is about the principles underpinning the use of medicines. Therapeutics is
the application of those principles in the care of patients, i.e. using medicines. This module
focuses on clinical pharmacology in 5th year and therapeutics in the trainee intern year.
Therapeutics is an important component of all modules. Information and course material are
provided on Moodle.
Details of course
In 5th year there are weekly lecture/workshops on major topics in clinical pharmacology. There
are tutorials in the Advanced Medicine and Advanced Surgery modules. In the TI year there are
therapeutics tutorials in the Medicine module.
Therapeutics is part of each speciality attachment. Therapeutics is underpinned by your personal
formulary of medicines you encounter throughout the course. You are expected to learn about
medical management of core conditions and core presentation during each attachment.
Objectives: Please refer to the curriculum map for more detail.
• To understand and apply the principles underpinning the use of medicines.
For example: pharmacokinetics, pharmacodynamics, individualisation of doses,
monitoring and adjusting treatment, regulation and the place of medicines in
health systems
• To understand factors affecting the use of medicines.
For example: adverse drug reactions, drug interactions, age and diseases,
pregnancy and lactation, prescribing and decision support systems.
• To be able to find, evaluate and use information about medicines.
• To understand the processes of medicines use (including prescribing) and medicines
regulation
Drug profiles
Seek and understand the properties of the medicines you encounter:
• generic name and drug class
• pharmacokinetic properties – bioavailability, clearance, distribution, half-life
• pharmacodynamic properties – physiological and molecular actions
• indications – when the drug is likely to be beneficial (these are uses of the drug)
• contraindications – when the drug is likely to be harmful
• adverse effects - serious adverse effects and common minor adverse effects
• overdose – effects of overdose and how to manage
• potential drug interactions
• dosage regimen/s - route, dose amount and dose interval, duration
• monitoring – clinical effects (beneficial and harmful), biomarkers, drug concentrations
Core medicines list
The Otago Medical School list of medicines to be learnt in detail, as important examples. You are
expected to have “drug profiles” for the core medicines list and are encouraged to profile new
59
medicines you encounter – particularly commonly used medicines. You will be assigned
medicines from the core medicines list to profile to prepare in detail for a class set of drug
profiles.
Module assessment
There is a 1½ hour written test at the end of the lecture-workshop series in 5th year. This
contains short answer questions and extended matching multiple-choice questions. This is the
majority of the module assessment. Students who fail the test wil be required to sit a
supplementary test. Students excelling will be offered an oral viva for potential distinction.
Participation in the lecture-workshops is a terms requirement. Participation will be recorded
by student use (or not) of Pol Everywhere in each lecture-workshop. Answering one or more
questions that week will be taken as the record of participation.
Attendance and quality of participation in tutorials is recorded and may influence module
assessment. Formative assessment will be provided.
The top student in 5th year Clinical Pharmacology will be awarded the E G McQueen prize.
Other clinical pharmacology assessment
As part of the advanced medicine assessment at the end of the attachment, there are
questions in Clinical Pharmacology and an OSCE station.
As part of the advanced surgery assessment at the end of the attachment, there are questions
in Clinical Pharmacology.
The end of year exam and OSCE includes Clinical Pharmacology questions and stations.
The Prescribing Skil s Assessment (PSA) is part of the end of fifth year assessment
The PSA is common across all medical schools in NZ and most in Australia. It is the Australasian
version of an internationally recognised exam.
In 2021 the PSA is compulsory at Otago Medical
School as a terms requirement. See
https://prescribingskil sassessment.com, including two
practice exams you can try. Note, there are only two practice exams available so use them
carefully.
Evaluation of the course
At the end of the lecture/workshop course, an HEDC survey may be provided for you to give
feedback on the course/teachers.
We welcome informal feedback and questions, please email Ma
tt, [email address]
or Paul,
[email address]
60
Clinical Skills Vertical Module
Module Convenor: Dr Niki Newman
Lead Module Convenor for 4th and 5th Years
Simulation Centre Director, Clinical Skills
Director, Professional Practice Fellow
Email:
[email address]
Phone: (03) 364-3892
Module Administrator: Heather Reilly
Simulation Centre Administrator
Email:
[email address]
Phone: (03) 364-3890
Simulation Centre | Te Whare Whakataruna
Level 1, 72 Oxford Terrace, Christchurch
Email:
[email address]
www.otago.ac.nz/christchurch/services/simulationcentre
Learning Outcomes:
Clinical Skills encompass all the skills used in the processes of consultation and management of
patients. They specifical y include communication skil s, consultation (includes communication,
history, examination), problem-solving (clinical reasoning), and procedural skills.
These skills also contribute to the development of professional skills and are not learned in
isolation but throughout all components of your programme, in particular during your block
module clinical attachments.
During the three years of the Clinical Skills Vertical Module at UOC you will develop your
professional and clinical skills in a simulated clinical environment. By the end of the module you
will be able to:
1. Demonstrate a range of professional behaviours and skills required of a newly graduated
medical practitioner.
2. Demonstrate the use of a systematic approach to the assessment and initial management
of patients.
3. Demonstrate critical thinking and reasoning skills during patient assessment, diagnosis
(history, examination, investigation) and initial management.
4. Perform procedural skil s in a way which demonstrates safe, effective techniques and
strategies to minimise complications.
5. Be ready to apply clinical skills learned through simulation to the real clinical learning
environment.
Clinical Skills Programme
The Clinical Skills Vertical Module (CSVM) sessions are held on Monday afternoons and Thursday
mornings in 4th year (and on one Wednesday afternoon), and Wednesday afternoons and Friday
mornings in 5th year; at the University of Otago, Christchurch Simulation Centre which is a scenic
seven minute walk from Christchurch Hospital.
MedMoodle
Please ensure you check the Clinical Skills MedMoodle pages regularly as they contain your
timetable for the year, the relevant resources to prepare you for each session and other
important information. Learning at the Simulation Centre includes practical hands-on time and
active participation, therefore we expect you to prepare in advance of each session to help
maximise your learning.
61
Assessment
Attendance and participation in all sessions of the Clinical Skills module is a ‘terms’ requirement.
An absence from any session without a satisfactory explanation and/or making up the missed
session will potentially generate a conditional pass and may result in terms being denied. A
register of attendance is maintained for this module.
We look forward to seeing you at the Simulation Centre.
62
Ethics and Law Vertical Module
The ethics teaching in ALM is designed to build upon the ethics you did in ELM. It aims to extend
your sensitivity to and of understanding the concepts introduced in ELM, and to develop your
ability to apply them in a wide range of different areas of practice, particularly (though not
exclusively) in clinical situations. Through this you will become able to make complex ethical
decisions on the basis of sound ethical reasons.
Ethics is taught in tutorials which take place in each rotation. They are led by teachers from the
Bioethics Centre, sometimes with clinicians from the students’ current attachment. The ethical
issues taken up in each tutorial wil reflect those encountered on the attachment.
In some tutorials, students wil be expected to present cases for discussion and reflection by
tutors and class mates.
General supporting material is on Moodle. See the 'Introduction to Clinical Ethics', and the
glossary of key concepts introduced in ELM 2 & 3. Material for each class is also to be found on
Moodle.
Medical law is taught in ALM 5 during the mid-year whole class learning week. Legal concepts
are often raised and discussed in ethics classes. This reflects the close relationship between
ethics and law.
The overarching learning goals for ALM ethics are as follows:
To develop an understanding of and respect for the values that underpin medical practice
To be able to recognize ethical problems as they arise in medical practice
To develop the ability to apply ethical concepts to specific medical situations and programs
To be able to critically reflect on and participate in ethical discussion relevant to medical
practice
To develop the ability to make complex ethical decisions and to explain the reasons for
those decisions
In each year, students are expected to attend al four classes or to provide an explanation for
non-attendance. Non-attendance at two or more tutorials, even with an explanation, will be
referred to the Student Progress Committee.
In year 5 you will required to complete two assessments: a clinical ethics case analysis (as part
of a group), and a written clinical ethics case analysis. See the Moodle page for details. There
will also be a short answer question relating to ethics, law and professionalism in the end of
year exam.
63
Hauora Māori Vertical Module
Course Convenor: Suzanne Pitama ([email address])
Teaching Fel ow: Amber Philpott ([email address])
MIHI
45 Cambridge Terrace, Christchurch
The Māori Indigenous Health Institute (MIHI) is the centre for Hauora Māori teaching and
research at the University of Otago, Christchurch (UOC).
The Hauora Māori 2021 vertical module involves the following:
1. This year utilises a ‘flipped classroom’ learning method. This means that it is expected
that each student wil have completed al online learning modules before attending
scheduled classes. These online learning modules allow for more interactive and
simulated based learning activities during classes, and comprise the formative
assessment for Hauora Māori.
2. Please also ensure you have reviewed the session requirements, including group
allocations and reporting times (as they vary for each teaching session).
3. At UOC the HMVM utilises a combination of immersed, integrated and independent
learning approaches.
• The immersed learning times are scheduled for 6 hours per 8-week rotation.
a) The Hauora Māori Moodle site will specifically outline the content
and learning methods for each session.
b) One of the key highlights for this year is a community Māori health
screening day (Tamariki ora) which is a joint venture between the
MIHI team and the Department of Paediatrics. This is timetabled
during the Whole Class Teaching Week, June 2021.
• Your Independent learning for 2021 includes:
a) Completing all online learning modules (formative assessment).
b) Undertaking an interview for your Hauora Māori Case Presentation.
• Your integrated learning will take two forms:
a) Hauora Māori hosts a joint session with Clinical Skills and Palliative
Care.
b) Hauora Māori content is included in an online learning module
within the Psych Med attachment (Māori and Schizophrenia).
• The Immersed, Integrated and Independent Learning opportunities provide a
pathway to attaining the Hauora Māori learning outcomes.
4. Al students wil be required to complete two summative assessments within the Hauora
Māori 2021 thread.
a) The Hauora 2021 OSCE
b) The Hauora 2021 Case Presentation (HMCP)
• All summative assessment results will be posted directly to Moodle.
5. Your professional behaviors will be measured through:
• Your attendance at learning sessions, and
• Your engagement within online and face to face learning sessions.
6. Hauora Māori 2021 completes a PASAF on the HMVM Moodle page.
64
Pathology Vertical Module
Head of Department:
Professor Martin Kennedy ([email address])
Module Convenors:
Anatomical Pathology:
Dr Andrew Miller ([email address])
Clinical Chemistry:
Dr Chris Florkowski ([email address])
Haematology:
Dr Sean MacPherson ([email address])
Microbiology:
Professor Steve Chambers ([email address])
Administration Team:
Enquiries to:
Alice Milnes (Administrator Client Services) or
Fran Cox (Administrator Client Services)
Level 2, School of Medicine building
Tel: 378 6381 (internal 86381)
E-mail: [email address]
Moodle
The Pathology Vertical Module has an active student resource on MedMoodle. Please ensure
that you check this regularly as it will have up-to-date information on weekly and semester
timetables, lectures, handouts, images and other material relevant for your course work.
If you find that a link doesn’t work or some information you require is not available on the
Pathology pages, please send an e-mail to [email address].
Teaching Programme
The Pathology programme is run over two years (Year 4 and Year 5). The formal component of
the programme comprises small and large group tutorials and lectures based around the major
subspecialties of pathology (Anatomical Pathology, Clinical Chemistry, Haematology and
Microbiology). All of these are assessed and contribute to terms and Potential Distinction.
Y5 Pathology teaching will be on Thursday afternoons. Some of this teaching will be combined
with the Y4 class. You will be expected to have completed your preparation prior to attending
these classes. Details of each week’s programme are posted on MedMoodle and will be emailed
to you. You should consult the weekly timetable as this will have the most current information
on venues/topics. Please note that the timetable may change at short notice.
The Department’s
Guide to Pathology booklet contains details of the course objectives,
timetable, assessments, recommended textbooks and location of tutorials and lectures.
There are in-course assessments in the fol owing pathology sub-disciplines: Clinical Chemistry,
Haematology and Microbiology. Satisfactory performance in the assessments is a Pathology
Terms requirement. Passes (or Passes after Conditions Met – PACM) are required in at least TWO
of the THREE pathology sub-disciplines to obtain Terms in Pathology. The Department provides
ample opportunities for remediation for each assessment for any who fail – our objective is to
get you through al the assessments with a solid core of pathology learning.
We hope that you enjoy the Y5 Pathology module and we welcome you and your feedback.
65
Professional Development Vertical Module
Module Convenors:
Prof Bridget Robinson
Email:
[email address]
Dr Martin de Bock
Email: [email address]
A/Prof Tony Walls
Email:
[email address]
Dr Phil Adamson
Email:
[email address]
Welcome to Professional Development.
We will focus on the wider social contexts of medical practice that are not always encountered
during routine clinical care but are necessary for the future challenges you will face as a doctor.
Teaching sessions will be on Monday or Tuesday afternoon in fourth year and Wednesday
afternoon or Friday morning in fifth year. These sessions will be mostly small group interactive
learning opportunities with input from a variety of people from other professional
organisations and within the wider health team.
Assessment
Assessment and Terms is based on attendance at al four sessions during the year. If you are
unable to attend the session, you must email the administrator (as per Moodle information)
with your reason for not attending,
before the session takes place.
Making the transition from medical student to doctor is a huge chal enge. We are sure you will
enjoy the professional development sessions and find them useful for developing your own
personal and professional attitudes needed for sound medical practice.
66
Quality and Safety Vertical Module
Module Convenor:
Dr Phil Hider
Department of Population Health
Email:
[email address]
Patient safety and quality improvement are becoming increasingly important in healthcare.
The ELM course introduced quality and safety as an important area for student learning and this
vertical module aims to build on that foundation. The programme allows discussion of a range of
factors related to patient safety, systems causation of adverse events both in medicine and other
industries, and various quality improvement methods and techniques. Improving the quality and
safety of patient care incorporates evidenced-based medicine, communication, patient-
centeredness, cultural competency and teamwork.
The module teaching sessions occur within the vertical module teaching times of Monday
afternoons in 4th year and Wednesday afternoons in 5th year. The sessions will involve a mixture
of exercises, presentations, discussions and self-directed work with a focus on prescribing and
medication safety. Some sessions will include opportunities for inter-professional learning.
There will be opportunities to consider issues related to the quality of patient care and patient
safety that students observe during their block modules.
• During the 4th year you will be asked to reflect on where patient harm may occur.
• During the 5th year you wil be asked to consider an area where you think improvement
is necessary and suggest solutions.
Assessment
There is no PASAF for this Module. Assessment wil be based on attendance.
Contacts
If you have any questions about the course, please contact:
[email address]
67
Radiology Vertical Module
Module Convenor: Dr Mike Hurrell,
[email address]
Departmental Secretary:
Extension 80913
Enquiries to:
First Floor, Parkside, Christchurch Hospital
Since the discovery of x-rays more than 100 years ago, radiology has developed a wide range of
imaging techniques. Now, standard CT and US imaging have expanded to include 3D and
endocavitary techniques. MRI and nuclear medicine studies have given us dramatical y different
physical viewpoints of the human body and its pathology, and interventional radiology has
al owed us to treat conditions with reduced patient morbidity and mortality.
These developments have given clinicians an increasing array of possible investigations, and one
of your learning tasks is to develop a basic feel for which examinations are appropriate for which
indications, and to know when you need to ask for help when choosing an investigation.
Your radiology teaching has been integrated into the teaching of musculoskeletal, neuroscience,
paediatrics and O&G. As well as tutorials in radiology during the block modules, you will also have
opportunity to attend working multi-disciplinary meetings where images are reviewed and
clinical decisions are made in conjunction with radiological input. You may also find it useful to
come to the department to see examinations performed on your patients. In particular you
should observe the fol owing studies:
US (Ultrasound)
CT (Computerised Tomography)
MRI (Magnetic Resonance Imaging)
DSA (Digital Subtraction Angiography)
Interventional Radiology (e.g. abscess drainage, nephrostomy, stenting, clot retrieval)
For each of these examinations, feel free to discuss the procedure with the radiologist, the
radiology registrar, or the medical imaging technologist.
By now you should be comfortable using PACS, and you should be reviewing imaging on your
patients to identify abnormalities described in the radiologist’s report.
Evaluation
Radiological questions will be included in the students’ examinations conducted by individual
departments. Radiological teaching wil be assessed by the students at the completion of their
clinical modules.
Resources
All radiologists participate in the teaching of medical students, and we all welcome you to
observe procedures and reporting in the Radiology Department. In addition, Dr Mike Hurrel is
available for students who need specific help.
Books on Reserve at the Canterbury Medical Library
Imaging for Students (Lisle) also available from the library website as a downloadable e-
book
Felson’s Principles of Chest Roentgenology (Goodman)
Radiology 101 (Erkonen)
Squire’s Fundamentals of Radiology (Novelline)
On-Line Resources
1. There are various PowerPoints on
Moodle under Radiology in the Advanced Medicine or
Advanced Surgery courses (Click the Radiology button at the top of the
Moodle page).
68
2. Websites:
https://www.dartmouth.edu/~anatomy/HAE/Radiology_Intro/rad_index.html – good
for revision at the start
https://www.radiologymasterclass.co.uk/tutorials/tutorials – tutorials for med students
and junior docs
www.radquiz.com – cases by area e.g. neuro, and also covers anatomy topics and
pathology e.g. brain tumours
https://drive.google.com/open?id=0B4nWyToNPRoRemdZMmFOcFRYU2s – How to
approach a chest x-ray
3. Major radiology journals are available on-line within the hospital or medical school (via
Ezproxy). These include:
Radiology
http://radiology.rsnajnls.org/
Radiographics
http://radiographics.rsnajnls.org/
American Journal of Roentgenology
http://www.ajronline.org/
European Journal of Radiolog
y http://www.sciencedirect.com/science/journal/0720048X
European Radiology
http://link.springer.com/journal/volumesAndIssues/330
69
Awards for 5th year students
At the end of the 5th Year there are nine awards which could be presented to students in the
Christchurch class. Two of these are Otago Medical School awards open to competition between 5th
Year students in the three Schools. The other seven are University of Otago, Christchurch awards.
The Otago Medical School awards available are:
Fowler Scholarships in Medicine
Established in 1924 by Miss L E Fowler. Three Scholarships shal be awarded annual y to the three
students gaining the highest aggregates of marks in the 5th Year examination, MB ChB. The
Scholarships may be held concurrently with any other scholarship.
The Rita Gills Gardener Memorial Prize
Founded in 1969 by a gift from Dr E Deny Gil s in memory of her late sister, Dr Rita Gardener (nee
Gil s), a graduate in Medicine of the University of Otago. The prize is awarded to the student gaining
the highest aggregate of marks in the 5th Year Examination. The prize consists of books to the value
set down in the current prize schedule. (Note: No entry required).
The University of Otago, Christchurch Awards are:
The Denis Stewart Award in Pathology
The Denis Stewart Award in Pathology was established by the New Zealand Society of Pathologists to
commemorate the outstanding contribution which Dr Denis Tiffin Stewart made to pathology in al
its aspects. The award is funded from a capital sum contributed by pathologists throughout New
Zealand and by members of the Christchurch medical staff. This sum is invested by the Society. The
award is presented annual y to the student achieving the highest standard in pathology throughout
the 4th and 5th Years of the MB ChB degree course in the Christchurch School of Medicine. It will be
awarded on the recommendation of the Dean and the Professor of Pathology of the School.
EG McQueen Award in Clinical Pharmacology
This award will be presented to the student who achieves the best overal performance in a clinical
pharmacology examination at the end of the fifth year
B M Colls Award in Medicine
This award, established in 1992, is for the student who scores highest overal during his/her medical
modules during the year.
Bone Marrow Cancer Trust Haematology Award
Established in 2002, this award is presented by the South Island Bone Marrow Transplant Trust and
is awarded for high achievement in aptitude in Haematology.
Maori/Indigenous Health Institute (MIHI) Hauora Maori Award
Established in 2006, this award is presented annually for general excellence in the ability to learn,
apply and engage in Hauora Maori in the 5th Year.
George Abbott Award in Paediatrics
Established in 2009, this award is presented for the best overal performance in Paediatrics in fifth
year.
Fifth Year Scholarships
These are available at:
https://www.otago.ac.nz/medicine/current-students/support/financial/index.html#scholarships
70
71
UNIVERSITY OF OTAGO, CHRISTCHURCH (UOC) INFORMATION
University of Otago, Christchurch Building & Facilities
The fol owing are located within the building:
Lower ground floor: Student common room, lockers and pigeonholes.
Ground floor:
Reception / Medical Education Unit / Rolleston Lecture Theatre and
foyer / Ground Floor meeting room
1st Floor:
Research Laboratories / Department of Anatomical Pathology / Stewart
Museum / Café Medici
2nd Floor:
Research laboratories / Department of Pathology & Biomedical Science
3rd Floor:
Research laboratories
4th Floor:
Research laboratories
5th Floor:
Department of the Dean / Research Office / Technology Services and
Student Computer Lab
6th Floor:
Canterbury Medical Library
7th Floor:
Beaven Lecture Theatre and foyer / Tutorial rooms / Sick Bay (key
available from reception)
Access to the floors / 7th floor rooms
Research Laboratories are on the 1st, 2nd and 4th floors. For security reasons these floors have
restricted entry so check with Reception first. Your UOC ID/security card will give you access to
the Pathology Department (2nd Floor) during working hours of 9.00am to 5.00pm, after hours
access to the UOC building, student computer lab, library, and 24 hour access to the lower ground
floor student common room and lockers.
All 7th floor rooms and lecture theatres have restricted access and, except for Rooms 706, 708
and 710, should be booked by completing a booking form which should be emailed or handed to
ground floor reception staff. The booking form is available from reception or the School’s
intranet (accessed from the
www.uoc.otago.ac.nz homepage). Rooms 706, 708 and 710 are
available for study use when not otherwise booked for teaching and meetings. Students wil stil
be required to use their access cards to gain entry but these specific rooms wil not require
booking through reception unless you want to book a specific time in advance. The 7th floor
notice board displays a daily booking sheet notifying readers when these rooms have been pre-
booked and therefore unavailable. Students should not use any computers on the 7th floor other
than the student designated computer in Room 710. Access to this computer is by usual student
login and password. Rooms should be left tidy after use and the furniture should not be re-
arranged. Appropriate use and care of these rooms and their facilities is monitored.
Bicycles
Bicycles may not be brought into the University of Otago, Christchurch building due to fire
regulations. There is a secure bicycle park available within the grounds of Christchurch Hospital
and you have access to this with your ID/security card.
Carparking
There is no parking available on the Christchurch Hospital site. Use the designated roadside al -
day parking in Hagley and Riccarton Avenues or pay to use one of the car park sites near the
hospital.
Parking at Night: You are advised to use the Hospital Security staff for out of hours escort to your
car or bike (within reason). The Hospital Security Office is located at the Emergency Department
reception. If possible, bring your car close to the hospital at dusk.
72
Fire Procedure
If you discover or suspect a fire:
• Break glass and operate alarm to get the Fire Department on its way and to evacuate the
building
• Dial 777 on nearest telephone and tel the operator the location and extent of fire; the
operator will take a 777 call immediately
Action to be taken when fire alarm sounds:
• Check your immediate area, you may find someone needs assistance
• Comply immediately with any instructions
• Vacate building via nearest exit stairway -
DO NOT USE LIFTS
• Assemble outside the building at the west end of Christchurch Hospital (Main Hospital Door).
The state of alarm exists until the fire brigade has given the all clear. Stoppage of the alarm bells
is not an all clear.
ID/Security Cards
ID/Security cards indicating you are a medical student will be issued at the start of fourth year.
This card is to be used during your time in Christchurch. You must display your ID clearly at all
times when in CDHB and university buildings. If you lose your card, please advise Reception as
soon as possible.
Lockers
Student lockers are located on the lower ground floor. Locker keys are available from Reception
for a deposit of $20, which is refundable when the key is returned at the end of your Trainee
Intern year. Please report lost keys to Reception and arrangements will be made for you to have
a new key cut. Try to keep track of your key - replacements are costly and pose a security
problem.
Mail Delivery
Your mail is delivered to your pigeonholes (lower ground floor) daily. Deliveries are welcome at
reception and we will hold any parcels there until you collect them.
Notice board
The official student notice boards are in the pigeonhole area, lower ground floor, UOC building.
You may put personal notices and meeting dates on this notice board. Please date these notices.
There is also a notice board in the Café Medici on which you may place personal notices.
Prayer Room
The Hospital Chapel, ground floor of Christchurch Hospital, is available to all denominations for
prayer. There is a Muslim prayer room located on the 7th floor, opposite Room 711.
Security
In the past the campus has suffered more than its fair share of security problems. One of the
most serious problems we still have is “stair-dancers”; people who use the back stairs to gain
unauthorised access onto the floors. These people have stolen handbags, items of clothing,
sports equipment, chemicals from the laboratories and even a laptop computer.
You can help. Use your lockers - if you bring valuables to the campus, secure them in your locker
and keep it locked AT ALL TIMES. Keep your key with you and report to reception at once if you
lose it. Do not leave your bags or backpacks unattended, particularly in corridors during lectures
or in the common room.
If you see anyone in the building who you are concerned about, report it to Reception and we
wil alert security. Do not approach the person yourself. If Reception is
unattended after hours,
go to the Orderlies office near the hospital main entrance and they will alert security for you.
73
Keep door codes a secret and if anyone asks you for the code tel them you don’t know what it
is.
Sports Facilities
There are no University of Otago sports facilities at the Christchurch campus
. The University of Canterbury Recreation Centre, 22 Kirkwood Avenue, has a University of Otago
student rate. See
www.reccentre.canterbury.ac.nz or phone 364 2433.
The YMCA, 12 Hereford Street, has student membership rates which you need to ask them about.
When you apply for membership please present your student ID Card.
The Christchurch Hospital Squash Club has two courts situated in St Asaph Street. Membership
is open to medical students. For further details please phone extension 80322.
Student Common Room
The Student Common Room is located on the lower ground floor of the University of Otago,
Christchurch building. Students have 24 hour access to this area. It would be appreciated if
students kept this area tidy, particularly taking responsibility for washing their own dishes and
putting their rubbish in the bin provided. Recycling bins for paper and plastics, along with a bin
for disposal of confidential material are located in the lift lobby area.
Please do not leave food
to go rotten in the fridge. Telephones and Beeps
Reception and Departmental phones are not to be used for personal cal s. There is a phone for
student use located outside the Student Common Room. Internal telephones are located in all
areas. The automatic paging system in use throughout the Christchurch hospitals works as
follows:
Paging Access Code
22
Number being called 4 digit number
Your extension - …. fol owed by #
e.g. if you are on extension 89237 and are calling pager 8431, dial 22 8431 89237#
CDHB Hospital Maps
Site maps for Christchurch Hospital, Burwood Hospital and Hillmorton Hospital are available on
the CDHB website – www.cdhb.health.nz
74
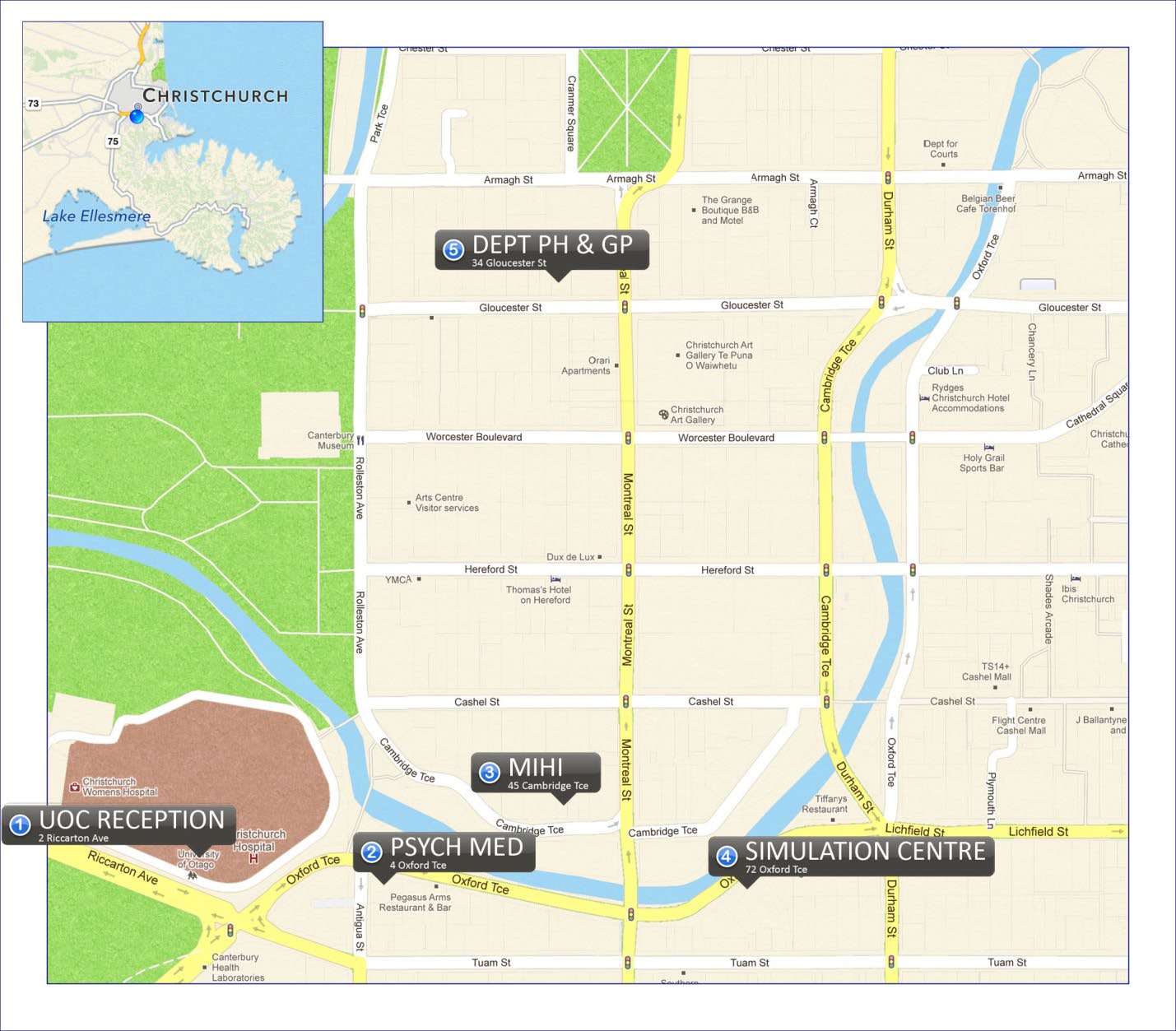 University of Otago, Christchurch - Department locations in close
proximity to the School
University of Otago, Christchurch - Department locations in close
proximity to the School
75
Canterbury Medical Library
Health Sciences Librarian:
Marg Walker
Enquiries:
Ph.: 03 364 0500
Website:
https://www.otago.ac.nz/christchurch/library/
Canterbury
Medical
Library (
CML) supports the educational, patient care and research activities of the
staff and students of the
University of
Otago,
Christchurch (
UOC), the Canterbury District Health Board
and health professionals in the Canterbury region.
Location: The Canterbury Medical Library is on the 6th floor of the UOC, School of Medicine building.
Library Help: For assistance or for any queries, contact CML staff in person or by phone, 03-364-0500,
chat online using the
LibChat link from our library homepage or simply email us at
[email address]. Library Hours and access: Basic hours of opening are Monday to Friday: 0830 to 1700, when the library
can be accessed directly. A security card and PIN is required to access the library during scheduled evening
and weekend hours of opening. Full details of the library’s hours are available at
https://www.otago.ac.nz/christchurch/library/otago011601.html Any changes to these hours are
publicised by email and on our library website.
Membership: Library membership for all 4th, 5th and 6th year medical students is rolled over at the
beginning of each academic year. As with the other University of Otago libraries in Dunedin and
Wellington, your current university student ID card is also your library card, please bring it with you when
visiting this library.
The standard loan period for material is 28 days, with automatic renewal of any loan items, as long as an
item is not required by anyone else. If an item you have out is requested by another person, you’ll be
notified through your
student email address that the item has been recal ed and given a new due date.
Please return any recalled items on or before this new date to avoid being charged overdue fines of $3.00
per day.
Student Reserve Col ection: This col ection contains student texts in heavy demand. Reserve items are
issued for two-hours, but can be renewed online through the library catalogue or check with Lending Desk
staff. Otherwise return reserve books promptly to the Lending Desk to avoid fines (of 10c per minute).
Online Library Resources: A range of online resources, from medical & health databases to online books
and journals, are all available through the CML website
https://www.otago.ac.nz/christchurch/library/.
The CML website is quite distinct and quite separate from the University Library (Dunedin) website and
to access CML online resources directly, remember to login through the ‘Off-campus Access’ link (on the
blue navigation bar) using your student username and password.
Group study rooms: CML has two group study rooms available for up to two hours at a time. Book one of
these rooms on the day or up to a week ahead, by contacting library staff at the Lending Desk in person,
or by phone or email.
Photocopying/printing & scanning: The library has one multifunctional machine for copying/printing and
scanning and a kiosk machine for adding funds to your account. As these are all part of the University’s
UniPrint system, Christchurch-based students are advised to select the correct print queue:
https://blogs.otago.ac.nz/studentit/printing/printing-outside-dunedin/
Recommending texts: Please talk to CML staff if there is a textbook you would like to recommend for
purchase for the collection, particularly if you feel it is a key text, or is one that would be of broad interest
to and likely to be wel used by other students and staff.
Request and Interloan Services: Use your student username & password to sign into the CML catalogue
for access to all the available request options. A ‘callslip’ request will allow you to borrow textbooks from
other Otago University libraries, these are generally supplied within 2-3 working days. Any ‘scan request’
for a book chapter or article from a print journal will be sent directly to your student email as a pdf
attachment.
The Interloan Service is a way to obtain material for your coursework that is not held in the Otago Library
76
system, but is available from another library. Interloan requests are also placed through the CML
catalogue.
Branch Libraries: If based at Burwood or Hillmorton Hospital, you may use the respective Burwood and
Hillmorton Hospital Libraries while you are on placement at either hospital.
Computer Facilities
Technology Services
Location: 5th Floor, Main UOC Building (2 Riccarton Ave)
Helpdesk Phone: 0800 479 888
Helpdesk Email: [email address]
Technology Services staff
Tim Young Team Leader, IT Support Services
Jarren Nelson IT Support Services Senior Technician
Anna Young IT Support Services Senior Technician
Dean Pester IT Support Services Senior Technician – AV/Lecture Theatre support)
Computer Lab
The student lab at the University of Otago, Christchurch is located on 5th floor of main UOC
building. There are 50 similar workstations running the same University desktop as the labs in
Dunedin. There is one multifunction device (MFD) which acts as a printer, photocopier & scanner.
There are also 10 CDHB computers available for student use split between the 5th floor student
lab and the 6th floor Library.
There are two more MFD's in the 6th floor Library, along with an EFTPOS Kiosk where you can
load money onto your printing account.
The student lab is a quiet study area and no food or drink is allowed inside. No-spill water bottles
can be used with caution.
Students are not permitted to copy any software from or onto the machines in the lab. If additional
programmes are required please contact the Team Leader IT Support Services.
Access to the computer system
Access to the computer system requires a user id and a password. These details have been sent
to you by the University administration.
If you have problems with logging into the computers please contact the helpdesk phone 0800
479 888.
When you leave the Christchurch campus your accounts wil stay alive for 3 months, after which
we delete your data. If you want to archive data or forward your email temporarily to somewhere
else, please contact the helpdesk (email:
[email address]).
Physical Access to the lab
To gain entry to the lab, you first need to arrange for security access which is part of the
University of Otago, Christchurch ID card process,
You have to use an ID Card to enter the Lab. Al ID cards include access to the lab but if
you have access problems please UOC reception staff.
77
• To access the lab, take the main (east) lifts to the 5th floor, turn left exiting the lifts then turn
right just past the photocopier (before you get to the sliding glass door). You wil need to use
your ID card on the door sensor to enter the computer lab.
• You do not need a card to exit the lab.
Printing
Printing or photocopying is charged at 10 cents per page for black & white or 50 cents per page
for colour. Double sided printing counts as two pages. This cost is based on total cost recovery.
The account wil have the unused balance from last year. The account can be topped up using
the EFTPOS kiosk in the Library on 6th floor. Please manage this account tightly (not too much
money on it, but stil enough to print that assignment on the Sunday night!) as refunds are
generally not given.
More information on student printing is available from the ITS website:
Student IT > Printing:
https://blogs.otago.ac.nz/studentit/printing/
Getting Help
If you need help with the computer lab, please phone the helpdesk on 0800 479 888 and inform
them you are a student in Christchurch. Alternatively feel free to visit the Technology Services
offices in the north-west corner of 5th floor (just past the rear lifts). If problems can be dealt with
later, you can send an email ([email address]).
More help is available on the web:
ITS Services > Information for Students:
http://www.otago.ac.nz/its/services/otago033765.html
Student IT Help:
http://www.otago.ac.nz/studentit
Medical Education Unit (MEU)
The MEU is located on the ground floor of the UOC building, via Reception. It is the first port of
call for students for all matters related to their medical education in Christchurch. Staff located
in the Christchurch MEU are:
Prof Tim Wilkinson
Prof Lutz Beckert Associate Dean (Medical Education)
Tania Huria Associate Dean (Undergraduate Student Affairs)
Assoc Prof Margaret Currie Associate Dean (Postgraduate Student Affairs)
Anthony Ali Education Adviser
Amanda Clifford Student Coordinator, Student Experience
Viv Hepburn Client Services Administrator
78
STUDENT WELFARE AND SERVICES
At the University of Otago, Christchurch we aim to provide an environment in which you enjoy
your learning and which enables you to perform to the best of your ability. At times, however,
problems can arise that hinder this. These may be problems in your personal life or problems
with the course. If this happens, there are several avenues of help available to you.
Module Convenor
If there are problems specific to a particular block module or vertical module you are strongly
encouraged, in the first instance, to discuss these with the module convenor.
Contact details for module convenors are listed in the first section of this handbook.
Student-Staff Committee
The Student-Staff Committee is another place to take any concerns about the course. Student
representatives from each year sit on the committee with members of staff. The committee works
very wel and has a proven record as an effective means of airing student and staff concerns and
initiating change.
You should approach one of your student education representatives to raise any problems at a
meeting of this committee.
Associate Dean (Undergraduate Student Affairs)
If you are having problems that are impacting on your performance at the School, the Associate
Dean (Undergraduate Student Affairs) is an appropriate person to talk to.
Tania Huria is the Associate Dean (Undergraduate Student Affairs). As this is a part-time position,
if you wish to make an appointment with the ADSA it is preferable that you contact Tania initially
by email:
[email address]. Associate Dean (Medical Education)
The ADME, Prof Lutz Beckert, has responsibility for the whole curriculum delivered to medical
students at UOC. He is also available if you have concerns about any aspects of the course,
particularly if you have suggestions for improvement.
Professional Development Group
As part of the professional development vertical module you will be in a small group of other
students from your class that meets regularly throughout the next two to three years with a staff
member mentor. These meetings provide opportunities to discuss any problems or concerns you
have (if you so choose) that relate to your developing professional role – that is, becoming a doctor.
79
General Practitioner Service for Medical Students
The Christchurch Doctors, Level 1, 148 Hereford Street, Christchurch, phone 366 3391, provide
a General Practice service to medical students at the University of Otago, Christchurch. Their
website is: http//www.thechristchurchdoctors.co.nz.
The Christchurch Doctors hours are 8am – 5pm daily, Monday to Friday. UOC pays $27 per
consult or there is no charge if the student has a community services card.
When making an
appointment, it is important that you indicate that you are a medical student patient and also
which doctor you wish to see. The arrangements with The Christchurch Doctors fol ow
negotiation with CMSA and are covered in the Student Services Fee. We would all appreciate
constructive feedback on this service which is continually reviewed.
Other General Practitioners may be used on a case by case basis with approval by the Associate
Dean (Student Affairs), Assoc Prof Jan McKenzie. An example would be where a student already
has a family GP in another practice. In these situations the first $30 will be paid by the School.
The balance wil need to be paid by the student.
• RMIP (Rural Medical Immersion Programme) students, from UOC 5th year. The first $28 is
paid by UOC, the same as the above, however the balance is paid by the RMIP budget.
The first $28 is only paid by UOC if the Student Welfare Levy is paid by the student along
with their fees, and this is credited to UOC.
• Nelson and Timaru students. UOC will cover the cost of treatment similar to the
arrangements for Christchurch students. See your Nelson or Timaru TI Handbook for
medical practice details.
International students are not eligible for a community services card and should request a receipt
and lodge a claim with their health insurer.
The following services will not be subsidised by the UOC but are available from the health centre:
diving medical assessment, insurance report, immigration medical, insurance medical, well
person checks, Depo Provera injection, IUD insertion, and wart removal.
House calls are available if you are too unwell to travel to the practice. There is a charge for
community services cardholders with a larger charge for non-cardholders. We are unable to
subsidise visits to the After Hours Surgery in Bealey Avenue.
Free flu vaccinations are available from the CDHB Occupational Health. They run a vaccination
programme in March/April – times/venues are advertised around the hospitals.
Counsel ing or clinical psychologist input is also available and is accessed via:
o The Christchurch Doctors and is subsidised up to $600 per annum. This
counselling is confidential, i.e. we are not notified of students accessing
counsel ing, or
o Associate Dean (Student Affairs)
o
Please ensure you cancel any appointments you are not going to attend.
Most counsel ors charge full rates for missed appointments and require
24 hours notice of cancel ations. Students wil be required to pay for any
appointments they do not attend.
Note: Other private specialist referrals are not covered under the levy. However, if a student is
struggling to pay for health costs they can discuss funding with the Associate Dean Student
Affairs.
80
School of Physiotherapy Clinic
Located on the ground floor, 32 Oxford Terrace on Tuam Street side. Offers:
• Full and comprehensive physiotherapy services
• Reduced rates for Otago University Students and Staff
• Referrals are not required
For further information or to make an appointment:
Telephone 332 2627
Email
[email address]
Web otago.ac.nz/physio-clinic/christchurch
Maori student support at UOC
The University of Otago, Christchurch has a number of resources to support Maori students
within our medical school.
Specifically these resources include:
Professional mentoring and networking support: Please contact Dr Maia Melbourne-
Wilcox,
[email address] (Professional Practice Fel ow based at MIHI).
Access to Maori language and tikanga development opportunities: Please contact Clara-ann Paul
who is the administrator for the Maori Strategic Framework at UOC. (Clara-ann is based at MIHI)
clara-ann.pa
[email address]. Research advice and guidance: Please contact the Kaitohutohu Maori health research adviser
who is based in the Research office on the 5th floor of the UOC building.
Student support to undertake extension in Maori health opportunities
The University of Otago, Christchurch is committed to provide al students the opportunity to
further their professional development opportunities in Hauora Maori. Specifically these
resources include:
Placements within providers who work with Maori patients: Please contact Suzanne Pitama,
[email address]. Suzanne is the TI Hauora Maori convenor and is based at MIHI.
Access to Maori language and tikanga development opportunities: Please contact Clara-ann Paul
who is the administrator for the Maori Strategic Framework at UOC. (Clara-ann is based at MIHI)
clara-ann.pa
[email address]
Research advice and guidance: Please contact Karen Keelan who is the Kaitohutohu Maori health
research.
[email address]. Karen is based in the Research office on the 5th floor of
the UOC building.
Dean of the Campus
Finally, it has been a long-standing policy of successive Deans of the School to listen to any concern
that any student may have and to assist in any way possible. Professor David Murdoch is available
for discussion in confidence with any student. To make an appointment with Prof Murdoch contact
his EA, Robyn Maguigan, by phone 364–0522 or e-mail [email address]
81
Student Support for International Students University of Otago, Christchurch
The University of Otago’s International Office offers support in the fol owing ways to
international students based at the
University of Otago Christchurch campus:
International Student Advisers
International Student Advisers (located in Dunedin) are available on a confidential basis to help
students cope with the difficulties that arise when adapting to a new culture; such as the stress
and unhappiness brought on by culture shock, homesickness, difficulties with making new
friendships, financial arrangements or family difficulties. You can contact a Student Adviser in
one of the fol owing ways:
Email: [email address]
Phone: 03 479 5777/5921 (between the hours of 9.00-4.30)
In addition, an adviser will visit the Christchurch campus during the year. The adviser will be
available to meet with international students to discuss any concerns or problems they may have.
Please refer to the Undergraduate Administrator for the schedule of visits and information on
how to make an appointment, or feel free to contact the advisers directly.
Student Visa Service
The Student Visa Coordinator or a Student Adviser from the University of Otago’s International
Office in Dunedin will visit the Christchurch campus in March (actual day to be confirmed) and
wil be available to accept your application provided that you are eligible to apply through the
Visa-on-Campus service (for more information refer to
www.otago.ac.nz/international/visas)
The International Office will contact you earlier in the year with details of their visit and to
arrange appointments for students to submit their applications.
International students can only make applications through the Visa-on-Campus service
in person
during the visit listed above; otherwise all other applications will have to be made directly to
Immigration New Zealand.
For more information please refer to the website
www.otago.ac.nz/international/visas or
contact the Student Visa Coordinator at
[email address]
Insurance Support
The International Office provides an insurance support service. For more information on your
policy or advice in making a claim please refer to the website
www.otago.ac.nz/international/healthcare
or contact us by
email:
[email address], or Phone: 03 479 8344 (between the hours of 9.00am-
4.30pm)
Code of Practice for the Pastoral Care of International Students
The University of Otago is a signatory to th
e Code of Practice for the Pastoral Care of International
Students published by the Ministry of Education and has agreed to observe and be bound by the
Code.
The Code is a document which provides a framework for service delivery by education providers
and their agents to international students. The Code sets out the minimum standards of advice
and care that are expected of educational providers with respect to international students. The
Code applies to pastoral care and provision of information only, and not to academic standards.
Copies of the Code are available on request from this institution or from the New Zealand
Ministry of Education website at
www.minedu.govt.nz/goto/international
International Office Complaints Procedure
Below is the process available to all international students should they wish to make a complaint
against the University concerning information provided, the standard of advice given or pastoral
care received under the Code of Practice for the Pastoral Care of International Students
82
1. Talk to an International Student Advisor about your complaint. Together you will discuss
the issue and try to reach an agreeable outcome. If the complaint is regarding an
International Student Advisor, talk directly to the Manager, Student International
Services.
2. If you are not satisfied with the proposed outcome, you wil be asked to put your complaint
in writing to the Manager, Student International Services.
3. The Manager, Student International Services, will discuss the complaint with you and
inform the person (if there is one) against whom the complaint is being made.
4. The Manager, Student International Services, will decide upon an outcome and action to
be taken and discuss this with you.
5. If you are unhappy with the outcome, you should put your complaint in writing to the Pro-
Vice-Chancellor (International).
6. If you stil have any concerns with the decision of the University, you can contact the
International Education Appeal Authority (IEAA). This is an independent organisation that
deals with complaints from international students. The IEAA enforces the standards in
the Code of Practice for the Pastoral Care of International Students.
For further information, email:
[email address]
Student Representation – Christchurch Medical Students’ Association (CMSA)
The Christchurch Medical Students’ Association (CMSA) represents medical students at the
University of Otago, Christchurch (UOC). The CMSA consists of a President, a Vice-President, a
Treasurer, a Secretary, two NZMSA Reps, six Class Reps, four Social Reps, and one Cultural Rep.
These positions are filled by election at the AGM, which occurs at the start of each academic year.
The overall functions of the CMSA are as follows:
• Provision of student representation on the Student/Staff Committee and the Curriculum Sub-
Committee UOC. These committees provide the official interface between staff and students
at the UOC, and enable students to provide staff with feedback about aspects of the course,
teaching, facilities, student welfare, etc.
• Organisation of social events, including ‘Steins’, the Medical Student Ball, Class Dinners and
various other activities.
• Organisation of forums for student information, for example the ‘Electives Evening’, and
various other annual events, including the Cultural Evening and the ACE Evening.
• Liaison with the New Zealand Medical Students’ Association (NZMSA) to provide national
representation for Christchurch medical students.
• Liaison with the Otago University Students’ Association (OUSA) to provide representation of
Christchurch medical students within the University of Otago.
• Liaison with the Postgraduates Society (PSOC) on issues common to studying at the
Christchurch Campus. This includes issues around computer services, study space and the
library.
• Cultivation of a positive experience for all medical students studying at the UOC.
If you want to become involved in the activities of the CMSA, or if you have a problem with any
aspect of life at the UOC, feel free to contact the CMSA President or any other member of the
CMSA.
The 2020 CMSA President is Dali Fan
Email:
[email address]
Website
: https://cmsa.org.nz
83
Association for Postgraduate Students of Otago, Christchurch (Inc.) (PSOC)
PSOC represents and promotes the needs of postgraduate students studying at the University of
Otago, Christchurch. As a charitable organisation, some of PSOC’s main objectives include:
fostering a higher education and research ethic; promoting cultural and recreational welfare; and
organising recreational activities for its members. One of PSOC’s goals is to encourage a close
relationship with CMSA (Christchurch Medical Student’s Association), thereby linking all
Christchurch students and maximising the diversity and scale of services offered.
Please direct all inquiries and suggestions to:
[email address]. The New Zealand Medical Association (NZMA)
NZMA is the only doctors’ organisation that represents you at every stage of your career, and in
whatever medical specialty you choose. The NZMA is a strong and effective voice in national
health and social policy issues. Our advocacy is heard and does make a difference.
The NZMA is a strong supporter of medical students, and has a close relationship with the New
Zealand Medical Students’ Association. They sponsor events and activities including career
evenings, workshops and projects. Most importantly they listen to and express your views to
training providers, regulatory bodies and the government, tackling issues such as education and
training, funding and government health policy to make positive gains on training and working.
Join the NZMA and NZMSA, become a part of your future in medicine, protect your career
investment and have your voice heard. As a member you are part of a professional community
of doctors. During your studies, through graduation and beyond, we are here to represent and
support you.
Visit the websit
e: www.nzma.org.nz
The New Zealand Medical Students Association (NZMSA) The New Zealand Medical Students' Association (NZMSA) is the peak representative body for
New Zealand medical students. Our nationwide volunteer executive advocates on your behalf on
any issue pertinent to medical students - a lot of our work focuses on education, welfare, and
political advocacy. Essentially we aim to inform and be informed by all medical students.
Our flagship event each year is Conference, which brings together medical students from across
New Zealand to hear from top speakers. Go to
http://conference.nzmsa.org.nz to find out about
what is in store this year. Other events we run on campus include
Beyond the Med School Gates
- a guide to life in the real world,
ACE Information Evenings and a nationwide blood drive during
which each school competes for the
Vampire Cup.
If you want to find out more information about the Association or stay in touch with what we are
doing, please visit our website. You can email us at any time with questions, concerns or
suggestions. We always want to hear from our members so that we can improve the advocacy
and service we provide.
We wish you al the very best for your year to come, and look forward to seeing you at some of
the Association's events throughout the year.
The New Zealand Medical Students' Association
[email address]
www.nzmsa.org.nz
84
OBJECTIVES, ASSESSMENT & EXAMINATION INFORMATION
Educational Objectives and Assessment
All block modules and vertical modules of the course have associated learning objectives. These
can help guide your study.
The Graduate Profile provides an overview of the attributes expected on an Otago medical
graduate.
University of Otago Medical Graduate Profile
On completion of the Otago University MB ChB programme, the graduate should be competent
to practise safely and effectively as a first year doctor (intern) and have an appropriate
foundation for further training in any branch of medicine. Specifical y, the graduate should have
the fol owing skil s and attributes;
1. Personal Attributes
1.1
The capacity to be a critical thinker, capable of weighing, evaluating and integrating new
information into his or her understanding of issues.
1.2 The ability to evaluate his or her own professional functioning and to act to remedy
limitations of knowledge, skills and attitudes throughout his or her career.
1.3 The ability to extrapolate from knowledge and principles to solve new problems.
1.4
An awareness of his or her professional limitations, and a willingness to seek help when
these limitations are met.
1.5
The ability and wil ingness to learn and to appreciate that learning continues throughout
life.
1.6
The ability and willingness to facilitate the learning experience of individuals, groups and
communities, both within and beyond the health sector.
1.7 Information literacy, including the ability to locate, evaluate and use information in a
range of contexts.
1.8 The ability to be organised and the skills for time management, so that time and resources
are used effectively and efficiently.
1.9 A dedication to appropriate ethical behaviour, based on a well developed awareness of
his or her own moral values, and knowledge and application of principles of medical
ethics.
1.10 An awareness of his or her own needs as a person, how health needs might impact on
competence to practice and an ability to access appropriate support or healthcare for him
or her self.
1.11 A commitment to the fundamental importance of the interdependence between
research, medical knowledge and professional practice.
1.12 A commitment to advocate for the health needs of individuals and communities.
2. Interactive Attributes
2.1 A caring and empathetic attitude to others.
2.2 Respect for, and an ability to co-operate with colleagues, competence in teamwork and an
understanding of the roles of other health professionals and healthcare teams.
85
2.3 A respect for patients and a dedication to work with patients to optimise their health and
wellbeing.
2.4 Respect for, and an ability to respond to the cultural context and aspirations of patients,
colleagues, other health care workers and communities.
2.5 An understanding of and an ability to respond to the obligations of the Treaty of Waitangi.
2.6 Oral and written communication skills, including an ability to communicate effectively with
individuals, groups and communities, both within and beyond the health sector.
3. Disciplinary Attributes
3.1 A sound knowledge of the philosophical, scientific and ethical principles underlying the
practice of medicine and an ability to apply this knowledge as part of competent medical
practice.
3.2 A sound understanding of the legal framework surrounding medical practice in New
Zealand.
3.3 A sense of social responsibility and an understanding of the contribution of doctor, health
services, society and political influences to the health outcomes of patients.
3.4 A commitment to the principles of patient-centred medicine.
3.5 Knowledge of factors impacting on inequalities in health outcomes.
3.6 Knowledge of factors impacting on the health status of Maori and other cultures.
3.7 Skil s in eliciting, documenting and presenting the history of a patient's problems and the
relevant physical examination findings.
3.8 Skills in problem solving and formulation of differential diagnoses.
3.9 Skills in the management of common medical conditions, including; informing and
negotiating, the performance of relevant clinical procedures, assessment of prognosis,
prescribing skil s, knowledge of drug therapy and care of the dying patient.
3.10 Skills in the management of emergencies and other serious medical conditions.
3.11 An awareness of, and the skills to manage, uncertainty in medical interpretation and
decision making.
3.12 An ability to maintain proper boundaries between personal and professional roles.
3.13 An understanding of the role played by individuals and society in the development of
disease and the maintenance of well-being.
3.14 A sense of social responsibility and an understanding of the roles and functions of
healthcare institutions in the social and political environment.
3.15 An appreciation of the global perspective of medicine, and an informed sense of the impact
of the international community on New Zealand and New Zealand's contribution to the
international community.
86
Advanced Learning in Medicine: Assessment in Years 4 and 5
The MB ChB Programme of Assessment Policies and Procedures can be found on MedMoodle
ALM4 and ALM5 homepages under the Assessment heading. Please consult this document
regarding assessment in Y4 and Y5. It is updated each year around March with any changes
to assessment procedures for the year.
87
Procedure for Special Arrangements for Saturday Examinations Due to Religious Beliefs
Fourth, Fifth & Sixth Year Medical Courses
Dunedin, Christchurch and Wel ington Schools
If a student requires special arrangements for Saturday examinations, due to religious beliefs,
the student must make an appointment with their respective Associate Dean for Undergraduate
Student Affairs (DSM, UOC or UOW) requesting exemption from the Saturday Examination
(OSCE) and applying for special alternative arrangement. This must be done as early in the year
as possible. The process of applying for this special arrangement wil be explained to the student
at this time.
Procedure for special arrangements for end of year examinations due to religious or cultural
beliefs
If a student requires special arrangements for end of year examinations, due to religious or
cultural beliefs, the student must make an appointment with their respective Associate Dean for
Student Affairs requesting exemption or special arrangements. This must be done as early on in
the year as possible, in writing, and six months before the examination, at the latest. The process
of applying for this special arrangement will be explained to the student at this time.
Procedure for arrangements for students to sit end of year examinations away from their home
campus
If due to exceptional circumstances a student requires arrangements to sit their end of 5th year
examinations at a campus that is not their home campus, the student must apply in writing and
provide details of the exceptional circumstances to the ADSA or RMIP Administrator as early on in
the year as possible, and six months before the examination, at the latest. This application will then
be sent to the MB ChB Assessment Manager. The Assessment Manager wil consult with the staff
responsible for organising the OSCE and written examinations, regarding logistics and capacity, at
the centre in which the student wishes to attend. The application and response from the
Assessment Manager wil then be submitted to the Board of Censors 4/5 Year for approval.
Al owances and assistance in assessments and examinations
Special consideration for students with temporary conditions affecting performance
Refer also: University of Otago, Special Consideration in Final Examinations policy
One purpose of assessments and examinations is to inform progress decisions, whether students
have achieved a standard equivalent to a fail, conditional pass, pass, potential distinction or
distinction in in-course assessment or a Fail, Pass, or Distinction for the year.
A student may have some temporary impairment at the time of an assessment that may affect
their performance and hence the result.
Special consideration regulations are intended to apply in cases where a student’s performance
is seriously impaired or absence is due to events beyond a student’s control. Students and staff
should be aware that the OMS has its own processes in relation to applications for special
consideration in module assessments and final examinations.
In general, if a student is unable to sit an assessment or examination on a particular day because
of acute il ness or other exceptional circumstances at the time of the module assessment or final
examination OR considers that their performance in any assessment or examination has been
seriously impaired due to illness or other exceptional circumstances, they should notify their
ADSA and/or the OMS of their intention to submit a Special Consideration application preferably
before, but always within 1 business day of the assessment.
88
Applications should be completed and submitted as soon as possible after the last examination
for which you are seeking special consideration, preferably within 1 business day, but always
within 5 calendar days, e.g. if your last exam is on the 20th, your application is due no later than
the 25th. As BOCs meet very soon after the completion of exams, students applying for Special
Consideration should understand that there may be significant delays in receiving their final
grade should the completed application postdate the BOC meeting.
The application (and any supporting documentation) will be considered by an advisory group
consisting of the ADSAs. To preserve the confidentiality of each claim the advisory group report
only the degree of impairment of each claimant to the relevant BOC.
At the discretion of the relevant BOC, a student whose application for special consideration is
accepted will either be offered the opportunity to sit an alternative assessment (mandatory in
the case of missed end of year examinations) or the level of impairment to be considered in
making a decision about the student’s performance. The BOC would have to ensure that any
alternative assessment that may be arranged for a student that has missed, rather than failed,
an assessment is added to the col ective evidence and was just as robust.
If the student’s result is close to a decision-making (fail/conditional pass/pass/potential
distinction/distinction) threshold then the impairment and any other relevant information wil
be taken into account by the BOC. The BOC wil make their decision based not only on the result,
but also on the degree of impairment and other relevant information. The outcome decision
might be different to that of the result alone.
As stated in the “Examination Regulations” section of the “General Regulations” in the University
of Otago Calendar, aegrotat passes are not offered in the MB ChB programme.
The OMS Special Consideration application form is available from the office of the ADSA in
Dunedin, Christchurch and Wel ington.
Alternative arrangements for students with permanent conditions affecting performance
A student who has a disability, impairment, medical condition or injury that they believe
significantly impacts on their performance in such a way as to prevent them from demonstrating
their ability may request alternative arrangements for that assessment. Alternatively, a student
who has a disability, impairment, medical condition or injury that they believe could interfere
with the standard running of an assessment for themselves and/or others may request
alternative arrangements for that assessment.
Where the assistance and/or allowances are of a nature that might reasonably be accommodated
in the normal workplace of a practicing doctor, particularly in the normal workplace of a PGY1
doctor in New Zealand, alternative arrangements will generally be approved.
Where a component of an examination assesses competence in a clinical setting and/or where
the appropriate timeframe for recognition of clinical material is included in the examination
development, e.g. MICN OSCEs and OSPEs, applications for extra time will generally not be
approved.
The student wil suggest the assistance that he or she considers appropriate for the impairment.
Application would have to be made
at least three months prior to any assessment. If the Board
agrees then this assistance wil be provided and the student wil sit the assessment/examination.
If the Board does not feel this assistance will be appropriate the student can reconsider. Late
applications wil only be considered in exceptional circumstances.
From the MoU between OMS and MCNZ:
89
“The Health Practitioners Competence Assurance Act (2003) (HPCA Act) creates a
statutory duty on any health practitioner or employer of health practitioners to notify
the medical council if any graduating student has a health problem that would not
enable them to perform the functions required for practice.” The OMS must therefore
notify, at graduation, the Medical Council of New Zealand (MCNZ) of any students who
fall into this category. The MCNZ Health Committee functions to support and monitor
doctors with health issues and helps them practise within their capacity.”
The MCNZ have confirmed that any concern regarding a graduating student should be raised with
them and that they will review all the information. A disability, impairment, medical condition or
injury that a student has, that required alternative arrangements and/or special consideration in
assessments, may affect their level of performance in practice and wil be notified to the MCNZ.
Decisions about which graduands should be notified to the MCNZ should be made by The Fitness
to Practice Committee (FtPC) who will consider al the evidence and advise the Dean of the
Medical School as to whom to refer. Given MCNZ policy, it is envisaged that alternative
arrangements and special assistance for a disability, impairment, medical condition or injury
would be included.
Students granted alternative arrangements in assessments for permanent conditions will be
expected to report these to the MCNZ themselves when completing their application for
registration with MCNZ.
The OMS application forms for Special Consideration and Alternative Arrangements are available
from the Student Affairs Office at each campus.
90
Student Evaluation of Modules
The primary purpose of students evaluating modules in the programme is to gather feedback to develop
and improve the teaching and learning environment. There are primarily two formal methods by which
we obtain student feedback: questionnaires and focus groups.
A Questionnaire is an online evaluation method that has a wide ranging scope of rating scales and free
text questions. Questions are decided by the Module Convenor (MC) with support from the Education
Adviser (EA), Anthony Ali. You will be sent a link via email, from the University’s Quality Advancement Unit
(QUA), to complete the questionnaire. The final response set will be provided to the MC, HoD, and EA.
The online method has been recently adopted by the University as the preferred method for
questionnaires. Since inception the online method has had a lower student response rate compared to
the previous method of having students complete the questionnaire on paper in a room usual y associated
with some learning opportunity they were doing concurrently. We want to increase this response rate so
encourage al students to help modules improve through completing these online questionnaires.
A Focus Group is an evaluation method that can elicit slightly different information compared to
questionnaires, usually more detail about fewer aspects of a module. They tend to range from 30-60
minutes and facilitated by the EA. Focus group discussion points are noted by the EA with a summary
report sent to the MC and HoD
without any student identifying information.
Students are reminded that, regardless of whether or not a convenor chooses to formal y conduct an
evaluation (as described above) of the module, they can at any time approach the convenor to offer
feedback. This method is preferred for incremental on-going improvements to the student experience.
Another avenue for students to provide feedback is through your education representative who is a
member of the UOC Student Staff Committee, which facilitates collaborative discussions to improve the
MB ChB programme.
Module Convenors are required to formally report to the UOC Curriculum Sub-committee (UOC-CSC) on
their module evaluation activities every three years using a digest*. However, module evaluation in most
instances can and wil occur in between reporting years in a more continuous manner.
The formal process of module evaluation, and MC reporting of evaluation activity, is diagrammed below.
Module Convenor & Education Adviser discuss
aspects to evaluate and method
QUA online questionnaire
Focus Group
QUA sends response set to
EA report sent to MC and HoD
MC, HoD, and EA
MC completes " Summary of Module
Evaluations " digest*
Summary of Module Evaluations presented to the UOC-CSC
Summary report including module digests sent to the Otago
Medical School Evaluation and Research Sub-committee
91
* Summary of Module Evaluations digest – this is formal y completed by module convenors and submitted
to the UOC Curriculum Sub-committee once every three years and asks convenors to comment on their
module evaluation activities, specifically:
• Method(s) used to gather data on the quality of the module, including who you approached for
feedback.
• Overall feedback and observations
• How the module has responded to previous evaluation comments
• How the stated learning objectives, teaching strategies, and assessments (if any) are aligned with
each other.
• Summary of the findings from the compulsory questions asked to students about how the
learning environment supported student learning.
• What’s working for them that others could learn from?
• Area(s) identified for, and strategies to address improvement
• Requests for support (resources: physical, human, other)
• Head of Department response
• CSC discussion points, (to be completed at meeting)
The Summary of Module Evaluations digest encompasses all aspects of evaluation the convenor has
chosen to conduct in the past three years, and may include not only student feedback methods described
above but other sources, for example, feedback from other staff involved in the module, assessment
results, and convenor reflections.
Your feedback does matter and without it we lose a valid source of information to enhance the overall
student learning experience. Many changes in the curriculum have been a direct result of such feedback,
just ask your fellow students! However, please keep in mind that student feedback, while valuable, is one
of many factors convenors consider when developing and improving modules. Your feedback may not
result in immediate change (or any change at al ) but it does prompt the module convenor to reflect on
what students are telling them.
If you need further information or have any questions, comments, or concerns about the module
evaluation process contact the EA, Anthony Ali ([email address]).
92
WORKING IN A CLINICAL SETTING
Student Access to Canterbury District Health Board Premises
The University of Otago has entered into a Memorandum of Agreement with the Canterbury
District Health Board which grants University Staff and students access to Canterbury District
Health Board facilities for the purposes of clinical instruction, clinical assessment and research.
Access to Canterbury District Health Board’s Hospitals and other facilities is on the following terms:
1.
University staff performing clinical services must hold a current annual Practising Certificate
issued by the relevant statutory certificates of authority.
2.
University staff and students must comply with al legislation including the Health
Information Privacy Code 1994, the Health Act 1956 and the Code of Health and Disability
Services Consumer Rights.
3.
Each undergraduate student in a clinical setting must be under the supervision of an
appropriately qualified member of either the professional Canterbury District Health Board
staff or the academic staff of the University.
4.
All University staff and students must comply with the policies, procedures and clinical
standards of the Canterbury District Health Board.
5.
That the University will ensure that all students will immediately leave the Canterbury
District Health Board’s facilities if instructed to do so by the Chief Executive (or his nominee)
of the Canterbury District Health Board, who wil advise the Registrar of the University of the
event.
The Dean of the University shal then take the appropriate action in accordance with the
regulations of the University governing disciplinary matters.
6.
The penalty of exclusion from classes if imposed shal be deemed to include exclusion from
all Canterbury District Health Board premises.
7.
That no student is placed in a clinical situation which is reasonably likely to develop beyond
the student’s capability and that the University wil ensure that a student is withdrawn from
such a clinical situation if instructed to do so by a Service Manager of the Canterbury District
Health Board.
8.
Access to Canterbury District Health Board premises shall be restricted to those students
required to undertake medical or other studies in the course of their tuition which require
them to have access to Canterbury District Health Board premises.
9.
That students are identified on al Canterbury District Health Board premises by the
wearing of an identification badge.
MedChart
MedChart is now live across CDHB and you should revise your MedChart training and use
MedChart with your teams. Participating in patient care (with supervision) is an important part
of learning to use medicines safely and effectively.
There have been a couple of occasions when students have inadvertently signed prescriptions in
MedChart. If this happens to you: if you notice immediately cease the prescription immediately;
If you realise later contact your supervising prescriber (RMO or SMO) immediately and ask them
to check the patients medication chart and make any adjustments necessary AND record the
event in the clinical notes. The “Update” step is the electronic signature that activates a
prescription. All electronic health systems record who does what and when. If you make a
mistake let someone know.
93
Attendance at Clinical Rounds While Unwell
It is unprofessional to expose patients to risk of infection. Students scheduled for a clinical round
whilst unwel should consider the welfare of those with whom they wil be in contact, both
patients and col eagues. If in doubt, seek the advice of staff.
If you are absent due to il ness you must advise your module convenor/administrator, your team
or Undergraduate Administrator.
Access to Clinical Records
To access a patient’s notes from the Clinical Records Department, year 4 and 5 students are
required to obtain consent from the patient. This wil not apply to patients who are stil in the
ward or patients that students are seeing in outpatients from whom consent has already been
obtained to be involved for education purposes.
Recording Lectures, Patient Interviews and Clinical Presentations
Please remember that recording of lectures should only occur if you have personally asked the
lecturer whether this is permissible. Recording of patient interviews or clinical demonstrations
by students is NOT permitted under any circumstances. Patients have not been asked for
permission and it is inappropriate for students or others to request permission at the time of the
demonstration. Please ensure that you respect the confidentiality implicit in all clinical
demonstrations.
Taking and Sharing Images: a guide for Otago Medical Students
1. Identifiable images
Images, pictures and any other visual representation of a patient or their record (including
notes and investigation results) that can identify that person is
health information under the
terms of the Health Information Privacy Code. Normally, consent from the patient is required
for the col ection, storage and use of a patient’s
health information. Although you have access
to health information for your training, such as patient notes and what patients tel you,
because of the ease with which images can be copied and transferred, the risks of breaching
patient confidentiality usual y outweighs the benefits of medical students taking such images.
For these reasons, the following rules are in place:
• Otago Medical Students must not take identifiable images on personal devices.
• Otago Medical Students must not store or share identifiable or potentially identifiable images on
personal devices.
• If requested by the clinical team to obtain an image of a patient for treatment related purposes,
even if the image itself is non-identifiable, students must not use personal devices to do so. It is
general y not recommended that students obtain images for treatment purposes, but if doing so
under clinical supervision the student shares the responsibility for ensuring the image is securely
transferred to the patient record and deleted from the imaging device.
Patient records/notes:
• Otago Medical Students must not take images of or make copies of identifiable patient
records/notes and must not take official records away from the clinical environment/hospital
• Material created by students (paper-based and electronic) which contains patient-related
information, either from a student-patient interaction or from existing patient records/notes,
must have basic de-identification efforts made including exclusion of any “unique identifiers” (e.g.
name, birth date, address or national number)
• It should be remembered however that if there is sufficient detail in the notes to be an accurate
and meaningful representation of the case, e.g. for “case history” purposes, then these are
potentially still identifiable and should be regarded as
health information under the HIPC
• If these materials/notes require work outside the clinical environment/hospital (e.g. library) great
care must be taken to ensure they remain secure and private
94
• Work on such records/materials should preferentially be done on University devices/student
desktop and not on personal devices and patient-related records should also be password
protected
• Once student created reproductions of patient notes are no longer required they should be
disposed of in a secure fashion – in a “confidential paper disposal bin” or deletion from the
electronic device/server.
2. Non-identifiable images for education related purposes
Images which do not, and cannot, identify patients do not count as
health information for the
purposes of the
Health Information Privacy Code. For example, this might include a photo of
a relatively common rash showing only a small area of skin. If you wish to create a non-
identifiable image that is in some way of, or relevant to, a patient, or if you are asked to do
so, you should ask the patient if they are happy for you to do this. The Code of Rights requires
you to treat the patient with respect and you can do this by explaining why you would like to
create an image and how you intend to use it.
• Even with patient consent, the creation, storage and use of non-identifiable images has a number
of risks, which is why the Otago Medical School encourages you think carefully about the benefits
and risks of doing so, and discourages you from using personal devices to create and store images.
You should create and store non-identifiable images of patients’ health information only for
legitimate education-related purposes. You should NOT publicly display the images, except in
formal teaching sessions, or otherwise share the images, especially via social media.
• If you wish to create or use a non-identifiable image of a patient or part of their record, seek their
agreement and explain the reason for creating the image, how it wil be used, and how and when
the image wil be deleted.
• You must have a legitimate and compelling training purpose for the creation and use of such an
image
• You must be able to delete that image
• Once the educational purpose has been met the image should be destroyed.
3. Ensuring an image is non-identifiable
Great care must be exercised to ensure that an image you create does not and cannot identify
the patient.
• Digital imaging devices often collect the date, time and GPS location of images. That information
could identify the patient. You must ensure that such information is deleted from the image file.
• Some conditions or injuries are rare and an image that identifies such a condition could identify
the patient and bring the information within the scope of the HIPC. Similarly, some bodies have
distinctive features that may make the person more easily identifiable. Students should avoid
using such images.
4. The difficulty of deleting images
Mobile devices tend to back up data to a cloud and share it with other applications. This can
make it very hard to delete an image once you have created it.
• You must ensure that any non-identifiable-image you do take is not backed up to a cloud or
another location where it might be hard for you to keep track of and delete the image.
Contexts where special care is required
Particular care must be taken in the creation of non-identifiable images in clinical contexts
where consent is compromised or not possible. For example, it would be inappropriate to
create a non-identifiable image of a child without the assent or consent of the child
(developmental age permitting), and the agreement of their parents and those supervising you
in that clinical environment. You should also be mindful that in the event that there is an
95
investigation under the Vulnerable Children’s Act, any image you create could be used as
evidence in that investigation.
Other situations where cultural and language influences preclude the usual patient consent,
including for example some Trainee Intern electives, may mean that images cannot be obtained
and used.
Chaperoning
It is necessary to consider the desirability of a chaperone when patients are being examined or
interviewed. This is especial y true if the patient is of the opposite gender, a child or otherwise
vulnerable. A patient should always be asked if they would prefer the consultation to take place
with a chaperone present.
It is also appropriate to consider the desirability of a chaperone if the student feels
uncomfortable with the patient, as the intent of chaperoning is to provide an environment for
consultation in which both parties feel safe. Students should never feel obliged to proceed with
an unsupervised interview or examination where they feel uncomfortable or concerned without
first seeking advice and assistance from a senior member of staff. Staff members should also
provide guidance to students in relation to chaperoning of specific patient interviews and
examinations.
Chaperoning during consultation when a staff member is present is the responsibility of the
member of staff.
There are a range of persons suitable to function as chaperones depending on the individual
circumstances, but usually another health professional, in particular a member of the nursing
staff, would be the first choice.
Cultural y Sensitive Issues
Health Sciences students are required to participate in all laboratory, practical and clinical
activities, which include activities that may not be usual in your culture. In the professional
classes, some aspects of teaching will require individuals to practice certain techniques on each
other, which may require you to partly undress and may involve body contact between students.
Training is done under close supervision and all students are required to participate, as it is
essential for their acquisition of clinical skills. Assistance for students experiencing difficulties in
this area is available, on request, from the relevant School.
Guidance on dress
Patients will judge you initially by your appearance – it is important that you dress appropriately
and in a respectful way. Use your common sense and note how doctors dress and present
themselves in the different clinical areas you work in. You are expected to dress like a doctor not
a student. You are usual y not expected to wear a white coat. Some teachers have specific
expectations about how you should dress (for example some prefer you to wear a white coat
and/or expect the men to wear ties) – you should respect their wishes.
Over the summer of 2003/2004 one of your col eagues conducted a survey of 451 patients at
Christchurch Hospital (inpatients and outpatients) to ascertain what styles of dress patients felt
comfortable or uncomfortable with in their doctors. She found that a tidy, semi-formal style of
dress is least likely to offend patients.
Items of clothing that, on average, patients were uncomfortable with for male doctors were:
facial piercings, earrings, rings on several fingers, brightly dyed hair, long hair, T-shirts, shorts,
sandals and sneakers.
Items of clothing that, on average, patients were uncomfortable with for female doctors were:
facial piercings, heavy make-up, short tops exposing the midriff (this can be extrapolated to low
96
cut tops and low riding trousers that expose the midriff), brightly dyed hair, T-shirts, shorts,
sandals and sneakers.
Younger patients were more tolerant of casual and alternative items than older patients. It was
generally acceptable for male doctors to opt for no tie.
When participants were presented with several photos of doctors in different styles of dress, a
friendly smile on the doctor’s face had an overwhelmingly positive impact – this is definitely
worth keeping in mind!
Immunisation Guidelines
Please refer to http://micn.otago.ac.nz/faculty-policies.
Emergency Response: Dealing with Exposure to Blood and/or Body Fluids
Actions Required by Staff Member/Student/Individual exposed to blood and/or body fluids:
1. If skin is splashed or penetrated, wash the area well with soap and water.
2. If the eyes are contaminated, rinse the eyes using the emergency eye wash facility.
3. If there is a splash into the mouth spit it out and rinse thoroughly.
4. Contact your supervisor or manager immediately.
5. Document the date and time of exposure, how the incident occurred and the name of the
source if known.
Actions Required by Supervisor / Manager / Other Responsible Person:
1.
Ensure area has been washed.
2.
Assess the type of exposure and need for testing and intervention. For the fol owing types
of exposure, consultation within 24 hours is mandatory:
• A needle stick injury or other sharp instrument injury when the needle or sharp
instrument is contaminated with blood or body fluids from another person.
• Mucous membrane contact with, or ingestion of blood or body fluids of another person.
• Contamination of fresh unhealed cut or broken skin surface with blood or body fluids
from another person.
• Bites where the skin surface is broken, or scratches where blood or body fluid
contamination from another person is likely.
3.
Contact:
Dunedin: Emergency Department, Dunedin Hospital (474 0999) for staff members,
Student Health for Students (479 8212) during working hours and Emergency Department,
Dunedin Hospital after working hours. Inform of the nature of the incident.
Christchurch: contact Infection Control or the Microbiologist on call at Christchurch
Hospital (364 0640).
Wellington: ring the Occupational Health Nurse at Wel ington Hospital (385 5999 ext. 6331
- pager 6331) or After Hours Manager if outside normal working hours, please ring the
Wellington Hospital operator.
For incidents that occur in other hospitals or other health care environments: immediate
notification of the local hospital staff member responsible for blood and /or body fluids
exposure is essential.
The Associate Dean for Student Affairs, Head of Department, Dean or other senior staff
member should also be contacted.
4.
Arrange for 10 mL blood to be taken from the exposed individual as soon as possible. The
screening must include HIV, HBsAg, HBsAb and HCV.
5.
If the source is known, contact and arrange for 10 mL blood sample to be taken.
6.
Provide support for the student or staff member involved.
7.
Complete the accident/incident form and forward to the HOD, Office of the Dean, and the
(Occupational) Health & Safety Team. Contact details for Health & Safety staff and the
97
accident/incident form are available on the Health & Safety website:
http://www.otago.ac.nz/healthandsafety/
IMMEDIATE ASSESSMENT
It is important that the individual is medical y assessed by an expert immediately so that
treatment can be commenced if deemed necessary.
It is important to arrange fol ow up with the emergency contacts provided.
Issues for the medical services to consider include:
Action wil depend on the status of the individual and the status of the source
Is there a need for immediate antiretroviral treatment?
Is there a need for hepatitis B immunoglobulin?
Is there a need for hepatitis B vaccination?
Has follow up been arranged?
98
Professional behaviour: general
Remember, it is part of the requirement of your continued status with health providers that your
behaviour towards staff and patients is always of the highest standard. Please remember to
show consideration to others around the hospital, in lifts and other public places. You are easily
recognised as students, and people look to you to show a good example.
The medical school, hospital and community providers aim to provide medical students with a
welcoming learning environment, and to encourage clinical staff who teach medical students
(supervising clinicians) to act as role models for professional behaviour and professional practice.
Professional behaviour: The role of patients in clinical education
Consent for clinical education
The patient’s welfare and interests are always the overriding consideration. Patients are typically
generous in their wil ingness to support medical students’ learning and often themselves benefit
from the process. Consent for clinical education obviously involves an element of permission but
it also extends to assisting patients to understand why a particular learning/ teaching activity is
valuable.
The following points address these aspects:
• Patients must be informed that they may be involved in students’ learning
• Patients have the right to choose, or to decline, to be interviewed, examined or cared for
by a medical student, or to be involved in any other way in medical education. Students
have no right to learn on patients.
• Patients have the right to know the name and professional standing of any person, staff
or student, who wishes, for teaching purposes, to interview them, examine them or carry
out any procedure
• Patient consent for clinical education must be obtained by the supervising clinician (or
other staff member). This should be done in a setting out of sight of the student(s) to
avoid placing undue pressure on patients. Patients have the right to withdraw from the
clinical education activity at any stage and may change their mind between consent with
the supervising clinician and subsequently seeing the student.
Medical students should wear their name badge and carry their ID card in all clinical settings.
When introducing themselves to a patient by name, they should explain that they are a medical
student, confirm that the patient is wil ing to proceed, and seek an explicit permission on each
occasion a consultation is needed.
Clinical Examination of Patients
Rectal, vaginal and genital examinations should not be considered routine examination
procedures for students. They require prior specific consent. For procedures undertaken on
patients under sedation or anaesthesia the prior consent must be written. Where a genital
examination is performed by a student(s) while the patient is under general anaesthetic, at most
two students [who have obtained prior written consent] may do so.
Medical students should be aware that the standard consent procedures may need to be
abbreviated or waived in emergency situations. In these circumstances responsibility rests with
the supervising clinician.
99
Professional behaviour: supervision
Appropriate Supervision
A supervising clinician is expected to brief medical students about their role in patient care. Often
this wil already be known (for example some issues are spelt out in this handbook), but if it is
not clear, or the requirements of a particular context are different from usual, medical students
are encouraged to seek explicit guidance about what is expected of them, paying particular
attention to the fol owing:
• Dress code: any requirements to be observed or avoided
• Introductions: any particular style, especial y if the medical student’s relationship to the
team needs to be made explicit
• Accountability: who is responsible for the medical student(s) and who is able to deal with
queries and concerns
• Emergencies: any procedures medical students are expected to observe in the event of
an emergency
• Standard precautions: medical students will need to be warned of situations in which
there are particular infection control issues and advised of the appropriate precautions
to observe
• Risk of violence: medical students should be given prior warning of patients with a known
history of violence with adequate briefing on protocols for ensuring personal safety
• Chaperones/support persons: medical students should be given guidance as to when a
child or adult should be offered a chaperone/support person and who may appropriately
serve in that capacity
• Boundary issues: medical students should be advised of any clinical settings in which
there is special reason to maintain robust professional boundaries
• Debriefing and reflection on clinical and professional development: medical students
should be encouraged to seek, and be offered prompt opportunity for, debriefing after
significant critical episodes, and opportunities to reflect on what they have learned, how
they are learning it, and their development of professionalism
• Ethical issues: medical students benefit from the opportunity, whether initiated by staff
or students, to discuss ethical issues generated by a specific case or experience.
Privacy and Confidentiality
Medical students are expected to observe the same high standards of confidentiality and respect
for privacy as govern the behaviour of al doctors and healthcare professionals. These standards
are set in the Privacy Act (1993) and the Health Information Privacy Code (The Privacy Code or
HIPC) (1994).
The Privacy Act 1993 and Privacy Code 1994 lay down specific rules regarding the collection,
storage and disclosure of health information in relation to identifiable patients. The basic rule is
that no information about any patient should be given to any other person without the
permission of the patient concerned. This applies to al health information and not only to that
which the patient might regard as particularly sensitive. It also includes situations such as reports
to lawyers, NZ Police, ACC and various other statutory bodies. There are some limited and specific
exceptions where disclosure of information without the consent of the patient is permitted or
authorised by law and you will learn about these over the next years of your training.
100
It is important to remember that patients share information with health professionals within a
relationship of trust and in order to assist the professional to help them with their health
problem. Respecting that trust and maintaining respect for privacy and confidentiality is
fundamental to the doctor-patient relationship and achieving the best outcome for the patient.
Access to notes and handling of written material:
Students should only access patient notes with the consent of the patient and where the patient
is under the care of the team to which the student is attached. Notes of patients not under the
care of the team should not be accessed except where the student has an alternate legitimate
reason to do so and also has specific consent from the patient.
Official patient hospital records must never be taken away from the clinical areas or out of the
hospital. Photocopying of patient notes by medical students is not permitted in any
circumstances. Material written by students which may contain patient-related information (e.g.
case histories) should not have any "unique identifiers" (e.g. name, birth date, address or national
number). If these notes require work outside the hospital (e.g. library) great care must be taken
to ensure they remain secure and private. Once patient related notes are no longer required they
should be disposed of in a secure fashion in one of the bins provided by the CDHB.
In addition to the legal restraints around patient related health information, students are
required to discuss any matters referring to the University of Otago, Christchurch and CDHB with
the Dean BEFORE disclosing information to outside agencies or bodies.
The fol owing points should also be kept in mind:
Medical students should avoid giving a patient a blanket guarantee of confidentiality and keep in
mind their position as trainees, the responsibility to always act in the patient’s best interests and
their accountability to their supervising clinician.
Whether information is acquired at interview or from the clinical record, patients have a right to
know the use(s) that wil be made of the information (written assignment, oral presentation to a
tutorial group, one to one discussion with a tutor, etc), and what steps will be taken to assure
the privacy of the information (such as de-identifying).
Medical students should make sure when, if at al , a copy of an assignment should be placed the
patient’s notes, and patients should be informed of this.
Care should be taken to ensure that discussion of a patient for clinical education takes place in a
secure setting where what is said cannot be overheard by others.
Under no circumstances is a medical student permitted to take photographs of a patient or
patient information, or to make a video or audio recording of any interaction with or observation
of a patient. If photographs or recordings are needed for educational purposes, they wil be
sought by the supervising clinician using current protocols.
Release of Information
Various pieces of legislation including the Health Information Privacy Code and the Health Act,
outlines circumstances where personal details may be released without the consent of the
patients or their representatives. The Privacy Act does not apply if release of information is
required under other legislation. For example, the notification of infectious diseases is required
under Section 74 of the Health Act.
Medical students must not release any information under these provisions without first
consulting the senior clinician working in the area. Students who make unauthorised disclosure
of personal health information will be subject to disciplinary action.
Students are required to consult with the Associate Dean of Student Affairs BEFORE disclosing
information about the School or any of the DHB institutions to the news media.
101
Medical student rights
Medical students have the right to decline to participate in clinical teaching and/or patient care
if there are concerns, ethical or otherwise about the activity; concern about their own
competency, lack of knowledge, or lack of understanding of the duties/tasks/responsibilities
involved; or conscientiously believe there is a lack of explanation or supervision.
Responding to problems
You may have concerns about a staff member or another student in particular concerning:
Unethical behaviour
Unprofessional behaviour
Poor role modelling
Threat to safety of self or others
Failure to meet ordinary teaching / learning Gratuitous belittling
obligations
In such situations contact one of the fol owing:
Module convenor
Head of Department
Associate Dean (Student Affairs)
Associate Dean (Medical Education)
University of Otago Mediator
Education Adviser
Student/Staff Committee
Class representative
102
UNIVERSITY OF OTAGO POLICIES
University Policies
A Guide to Academic Conduct
Over the course of your studies you wil be required to submit a wide variety of work in a range
of styles and formats. The purpose of this guide is to introduce you to good practice and help
you avoid poor or unacceptable academic practice.
What do we mean by academic misconduct?
In simple terms we mean ‘not cheating’, but academic conduct is much more than that. Gaining
a university degree indicates that you have achieved certain knowledge and skil s in your chosen
subject. The academic integrity of the awarding institution adds considerable kudos to the value
of your degree, hence the concern about buying degrees over the internet. Academic conduct
means playing by the rules, demonstrating a high level of personal integrity in your academic
work.
Academic misconduct is a very serious offence and can lead to a range of penalties from reduced
grade to expulsion. These are described in the University Calendar and University policies on the
OMS website
http://www.otago.ac.nz/medical-school/otago614508.pdf
Ethical Behaviour Policy
The University's Ethical Behaviour Policy sets out expected standards of behaviour for all
members of the University community and commits itself to providing you with an environment
of safety, respect and dignity. If you believe that you are being harassed or discriminated against,
or otherwise treated unacceptably, you can talk about this with a contact person - see the posters
on campus or visit the website or contact the University Mediator on 03 479 5679
([email address]). The policy and more information are on the website at
www.otago.ac.nz/mediation.
Informal Conflict Resolution
The University is committed to providing an environment of safety, respect and dignity for al
members of the University community while they participate in University life. The Ethical
Behaviour Policy outlines unacceptable behaviours (including sexual harassment, racial
harassment and personal harassment or bullying, discrimination and abuse of authority), ensures
that people can raise issues without fear of reprisal, and promotes the informal resolution of
complaints. You can read more about the Policy, which outlines the processes for both informal
conflict resolution and formal complaints,
at www.otago.ac.nz/mediation
If you are angry or unhappy about a situation, try:
instant resolution: if you make your feelings known to the person most directly involved,
you may be able to resolve the issue straight away. Most people do not intend to be
unjust, unkind or threatening. If they have made inappropriate comments or decisions,
they usual y want to know about it and have the chance to put it right. If you feel
uncomfortable doing this alone, you may want to take someone with you for support.
peer discussion: talk to friends to find out if you are overreacting and how they might
handle similar situations, get advice as to your options but think about their
consequences. You can approach one of the Ethical Behaviour Network contact people
(their names are on posters and on the website) who are trained to listen, in confidence,
to your problem, help you clarify it and outline the options available to you.
assistance from a staff member or the Head of Department to discuss these issues in
confidence.
103
mediation assistance: if the first three steps don't work or seem inappropriate, you can
contact the University Mediator (telephone 479-5679, email [email address]) to
informally discuss any concerns. Everything is confidential and YOU remain in control. You
may decide to choose mediation - where the mediator assists you and the other person
to talk through your problem and come up with a mutual y acceptable solution.
OTAGO MEDICAL SCHOOL (OMS) POLICIES AND GUIDELINES
The official policies, guidelines and codes of conduct applicable to the Bachelor of Medicine and
Bachelor of Surgery (MB ChB) medical degree programme, its staff, and students are listed below
and available at
https://www.otago.ac.nz/medicine/current-students/resources/policies-guides/index.html.
These are both the authoritative and most recent versions of these documents.
Please contact the OMS Manager if you have any queries about these documents:
Assessment
• MB ChB Programme of Assessment Policies and Procedures
• MB ChB Standards for Assessment in the MB ChB Programme
• MB ChB Assessment Incident Reporting Form
• Academic Misconduct in OMS-run assessments that inform progress decisions
• Otago Medical School prize list
•
Procedures on the retention, release and disposal of records related to student
assessment
• Writing conditions to Pass for students awarded a Conditional Pass
Codes of Conduct
•
Code of Professional Conduct for Medical Students
•
A Guide to Academic Conduct
• Medical Council of NZ and OMS Memorandum of Understanding
• Medical Students and Informed Consent – a national consensus statement 2015
• Code of Practice for Fitness to Practise
• Guidelines on Maintaining Confidentiality of Clinical Material
• Guide to online professionalism for medical practitioners and medical students
• Taking and sharing images – a guide for Otago medical students
• Student Leave Policy
• Students Viewing Patients’ Health Information Policy
Options
•
BMedSc(Hons) Degree Policy
•
Exit Options after 3rd Yr Policy •
MB ChB & PhD Protocol
•
Other Study Opportunities for Medical Students
•
Research Opportunities for Medical Students
•
Transfer Policy •
Withdrawal Policy & Procedures
Safety and well-being
•
Emergency Response blood and body fluids • Infectious Diseases and
Immunisation Policy link (to Division of Health Sciences policy)
• Safe Travel for TI students on their electives
• Processes for confidential y reporting events of concern in the learning environment
(University access only via Moodle)
• Trainee Intern Working Hours Guidelines
• OMS Support for Student Parents
104
Code of Practice for Fitness to Practise
Medical students are part of the medical profession. Whilst students do not yet enjoy the
privileges accorded to qualified practitioners, and are not yet bound by the full professional
constraints imposed upon practising doctors, it is vital that issues that may affect their current or
future fitness to practise are fairly and transparently addressed by the Faculty of Medicine and
its Schools.
The Code of Practice for Fitness to Practise outlines the policy and mechanisms of the University
of Otago Faculty of Medicine to assess and act on issues fairly and equitably concerning a
student’s Fitness to Practise.
It is expected that, at graduation, our students wil meet the expectations of the University of
Otago Medical Graduate Profile, through their personal attributes, teaching and learning during
the course, and support from staff.
Throughout the undergraduate programme, the assessment processes wil include steps to
identify and monitor any students who might not meet the graduate profile standards through
problems with health, or with professional attitudes and behaviour both within and outside the
teaching environment. In the normal course of events, the assessment wil be conducted by the
relevant Student Progress and Assessment Committee (SPAC). But in cases of particular concern,
referral is made to the Fitness to Practice Committee. The Committee provides support,
remediation and monitoring of potential or actual Fitness to Practise needs of students who do
not meet graduate profile standards. The FtPC has the power to recommend the granting or
withholding of terms where ongoing issues are unresolved.
A copy of the policy can be found on the Otago Medical School website:
https://www.otago.ac.nz/medicine/current-students/resources/policies-guides/index.html
POLICY FOR TRANSFERS BETWEEN SCHOOLS OF THE OTAGO MEDICAL SCHOOL
• Once a student is placed in a Campus School of Medicine (DSM, UOC or UOW) the student is
expected to remain at that School until completion of sixth year.
• A student who wishes to transfer to another Campus School of Medicine after being placed in a
School for fourth year, but fourth Year has yet to commence, will address his/her request to
change Schools directly to the Associate Dean of Student Affairs, Dunedin School of Medicine.
This will be dealt with as an allocation of school in third year, as opposed to transfer.
• Transfers wil not normal y be considered during, or between, fourth and fifth year, but may be
considered for sixth year. Applications are to be submitted to the Campus School Associate
Deans of Student Affairs/Undergraduate Education by 5 pm 6 March 2020 (please note, this is an
earlier closing date than in previous years) in the year prior to transfer.
• The Dean of the Otago Medical School, will only approve transfers if places are available and the
Deans of the respective Schools support the transfer (principles contained in the MB ChB
regulation Division of Class after Third Year in the University of Otago Calendar will be taken into
account).
• Transfers between DSM, UOC and UOW are not necessarily on a one-to-one basis but the total
numbers at each school will be considered with a view to maintaining the agreed numbers of
places for each school (eg 80 – DSM, 110 – UOC, 110 – UOW).
• Criteria for assessing eligibility and priority for transfer shall be determined by the Deans and
Associate Deans of Student Affairs/Undergraduate Education – DSM, UOC and UOW
• Elective quarters in 6th Year cannot be guaranteed for transferring students. The School to which
the student is transferring shall make the final decision on Elective quarters.
105
POLICY FOR TRANSFERS BETWEEN OTAGO AND
THE MEDICAL PROGRAMME AT UNVERSITY OF AUCKLAND
• A student who wishes to transfer to the Medical Programme, University of Auckland, for Year 6
will apply in writing to the Associate Dean of Student Affairs/Undergraduate Education at the
Campus School of Medicine they are currently attending. The application is to be received
by 5
pm 6 March in the year prior to transfer, i.e. when a student is in Year 5 of the medical course.
• Transfers will only be approved on a one-to-one swap with a student from the Medical
Programme, University of Auckland.
• Students must have an acceptable standard of performance in the course.
• The home institution wil notify current Vulnerable Children Act 2014 compliance and clearance
to the host institution prior to the transfer commencing.
• Students must provide evidence of special reasons for transfer and the Associate Deans for
Student Affairs at Otago and the relevant staff at Auckland shall determine the criteria and assess
applications against this criteria.
• As Year 6 of the programme in Auckland commences in early January each year, trainee interns
from Otago who transfer to Auckland, will be required to commence the year in mid-November
with a 4-week elective. Following completion of this in early January, they then join the Auckland
programme. Elective attachments in Auckland are for a period of 8 weeks and if undertaken
overseas, must be undertaken under one institution.
• The Elective quarter cannot be guaranteed for Otago students transferring to Auckland. The
Auckland Programme staff shall make the final decision on Elective quarters. Auckland students
transferring to Otago will be allocated 4th Quarter Electives. This enables the Auckland student
to complete the programme and meet the earlier graduation deadlines for the Auckland
programme.
• Auckland students transferring to Otago will undertake the full Otago sixth year programme, i.e.
from November – November.
• Otago students at Auckland are not enrol ed students so will have academic visitor status
associated with their ID cards, this may restrict access to some student facilities andservices as
wel as public transport discounts. They may use the library but if borrowing is needed, it wil be
Note:
Deans of Dunedin, Christchurch, Wel ington and the University of Auckland delegate to their
Associate Deans of Student Affairs/Undergraduate Education (ADSA) and relevant staff at
Auckland the authority to recommend transfers out of and into their School. Al transfers are
monitored by the ADSA (Dunedin) on behalf of the Otago Medical School to ensure applicants
from all Schools have equal opportunity to transfer.
Medical Council of New Zealand Policies and Information for Medical Students
The Medical Council of New Zealand websit
e: http://www.mcnz.org.nz provides information on
Medical Registration requirements and other information for medical students.
106
ALM
4/
5
University of Otago, Christchurch
Advanced Learning in Medicine
Fourth and Fifth Year Handbook
2021
For further information:
University of Otago, Christchurch
PO Box 4345
Christchurch 8140
New Zealand
Tel 64 3 364 0530
Document Outline