Lead Coordination Minister for the Government’s Response to the Royal Commission’s Report into the Terrorist Attack on the Christchurch Mosques
9 September 2021
Matthew Hooton
By email:
[FYI request #16400 email]
Ref:
ALOIA081
Dear Matthew
Response to your request for official information Thank you for your request under the Official Information Act 1982 (the Act) on 13 August
2021 for:
“the Briefing Note from the Ministry of Health dated 9 November 2020 referred to in
your letter to me of 2 August 2021. For your convenience, your letter of 2 August
2021 can be found at
https://scanmail.trustwave.com/?c=15517&d=0ZuZ4aM5ju1zc8GPXoF1ZKk60N7e-
koacEMbsJHaZA&u=https%3a%2f%2ffyi%2eorg%2enz%2frequest%2f15865%2fres
ponse%2f61183%2fattach%2f8%2fResponse%2520Letter%2520ALOIA057%2epdf”
The document you have requested is attached as Appendix 1 with some information
withheld under the following sections of the Act:
9(2)(a) to protect the privacy of natural persons
9(2)(f)(iv) to maintain the constitutional conventions that protect the confidentiality of
advice tendered by Ministers and officials.
I trust this information fulfils your request. Under section 28(3) of the Act, you have the right
to ask the Ombudsman to review any decisions made under this request. The Ombudsman
may be contacted by email at: [email address] or by calling 0800 802 602.
Yours sincerely
Hon Andrew Little
Minister of Health

Appendix 1
Briefing
Overview of work to transform New Zealand’s approach to mental
wellbeing
Date due to MO: 9 November 2020
Action required by:
N/A
Security level:
IN CONFIDENCE
Health Report number: 20201961 1982
To:
Hon Andrew Little, Minister of Health
Act
Contact for telephone discussion
Name
Position
Telephone
Information
Toni Gutschlag
Acting Deputy Director General, Mental
s 9(2)(a)
Health and Addiction
Kiri Richards
Group Manager, Mental Healt
Official h and
s 9(2)(a)
Addiction Strategy and Policy
the
under
Minister’s office to complete:
☐ Approved
☐ Decline
☐ Noted
☐ Needs change
☐ Seen
☐ Overtaken by events
Released
☐ See Minister’s Notes
☐ Withdrawn
Appendix 1
Overview of work to transform New
Zealand’s approach to mental wellbeing
Security level:
IN CONFIDENCE
Date:
9 November 2020
To:
Hon Andrew Little, Minister of Health
Purpose of report
1.
This report responds to your request for an overview of the implementation of the
1982
Government’s response to
He Ara Oranga: Report of the Government Inquiry into Mental
Health and Addiction (
He Ara Oranga). It also provides you with a summary of wider
Act
mental health and addiction work and your ministerial responsibilities under the Mental
Health (Compulsory Assessment and Treatment) Act 1992.
Summary
2.
Mental wellbeing impacts the lives of all people in New Zealand. Supporting people to
have good mental wellbeing is more important now than ever, given the wide-ranging
Information
impacts of COVID-19.
3.
A large programme of work is underway to implement the response to
He Ara Oranga.
He Ara Oranga called for the transformation of our approach to mental health and
addiction, underpinned by achieving equity and a collaborative approach with
Official
communities.
4.
This Government’s response to
He Ara Oranga is supported by the delivery of the
the
Budget 2019 investment of $1.9 billion in a cross-government mental wellbeing package.
A key focus of the Budget 2019 investment is the initiative to expand access and choice
of primary mental health and addiction support nationally ($455 million over four years).
under
This initiative is rolling out new services over five years, including in general practices
and kaupapa Māori, Pacific and youth settings.
5.
The Ministry of Health (the Ministry) is also leading the psychosocial response to COVID-
19, including the development of
Kia Kaha, Kia Māia, Kia Ora Aotearoa: Psychosocial and
Mental Wellbeing Plan (Kia Kaha).
Kia Kaha is a cross-sectoral plan that outlines a
national mental wellbeing framework to guide collective efforts to support mental
Released
wellbeing and sets out priority actions over the next 12–18 months.
6.
The development of a longer-term pathway to transform our approach to mental health
and addiction will build on
Kia Kaha and will outline the direction for our approach to
mental health and addiction over the next 10 years. The pathway will guide the actions
and investment needed to achieve the transformative change called for in
He Ara
Oranga.
7.
Alongside current work, the Ministry has also started planning for progressing Labour’s
manifesto commitments. These align strongly with the direction set by the Government’s
response to
He Ara Oranga and recent investments in mental wellbeing.
Appendix 1
Recommendations
This briefing has no recommendations and is for your noting only.
Toni Gutschlag
Hon Andrew Little
Acting Deputy Director-General
Minister of Health
Mental Health and Addiction
Date:
Date: 9/11/2020
1982
Act
Information
Official
the
under
Released
Appendix 1
Overview of work to transform New
Zealand’s approach to mental wellbeing
Context
1.
Mental wellbeing impacts the lives of all people in New Zealand. Approximately one in
five New Zealanders experience mental illness or addiction each year. Some population
groups are more at risk of poorer outcomes than others, including Māori, Pacific
peoples, younger people and people experiencing financial hardship.
2.
Mental wellbeing is not simply an absence of mental illness or addiction. It is a state of
wellbeing where people feel positive and are able to adapt and cope with life s
challenges. It is fostered in our homes, schools and communities and is influenced by
1982
wider determinants such as income, employment, housing, education, and freedom from
abuse, violence and discrimination.
Act
3.
The health and disability system plays a key role in supporting mental wellbeing through
the provision of a continuum of mental health and addiction supports to respond to
different levels of need. This ranges from wellbeing promotion activities; to primary and
community supports; to specialist services for those with higher needs, including crisis
responses and forensic services for people interacting with the justice system.
4.
Appendix One provides more information about New Zealanders’ mental wellbeing
Information
needs, outcomes and inequities, and the mental health and addiction system.
5.
COVID-19 has also had an impact on people’s mental wellbeing, including creating
heightened levels of distress, anxiety and a sense of ongoing uncertainty. This is a
normal response to such an event. Work to suppo
Official rt people’s mental wellbeing, and to
respond to people’s mental health and addiction needs, is therefore particularly
important now as it will help with both the immediate recovery from COVID-19 and will
the
lay the foundation for positive mental wellbeing in the longer term.
Inquiry into Mental Health and Addiction
under
6.
An independent Government Inquiry into Mental Health and Addiction was established
in 2018 to hear from people in New Zealand about the changes needed to address
mental health and addiction issues. Addressing inequities in outcomes was one of the
key drivers for the Inquiry.
7.
The Inquiry report –
He Ara Oranga – was presented to the then Government in
Released
November 2018 with 40 recommendations. Key shifts called for include:
a. ensuring our approach works for and meets the needs of Māori
b. moving to a holistic, whole-of-government approach grounded in wellbeing that
recognises the social, cultural and economic foundations of mental wellbeing and
looks across the life course
c. increasing access to and choice of mental wellbeing supports to ensure all people in
New Zealand receive the support they need, when and where they need it
d. designing supports collaboratively with communities, Māori and people with lived
experience of mental health and addiction issues.
Appendix 1
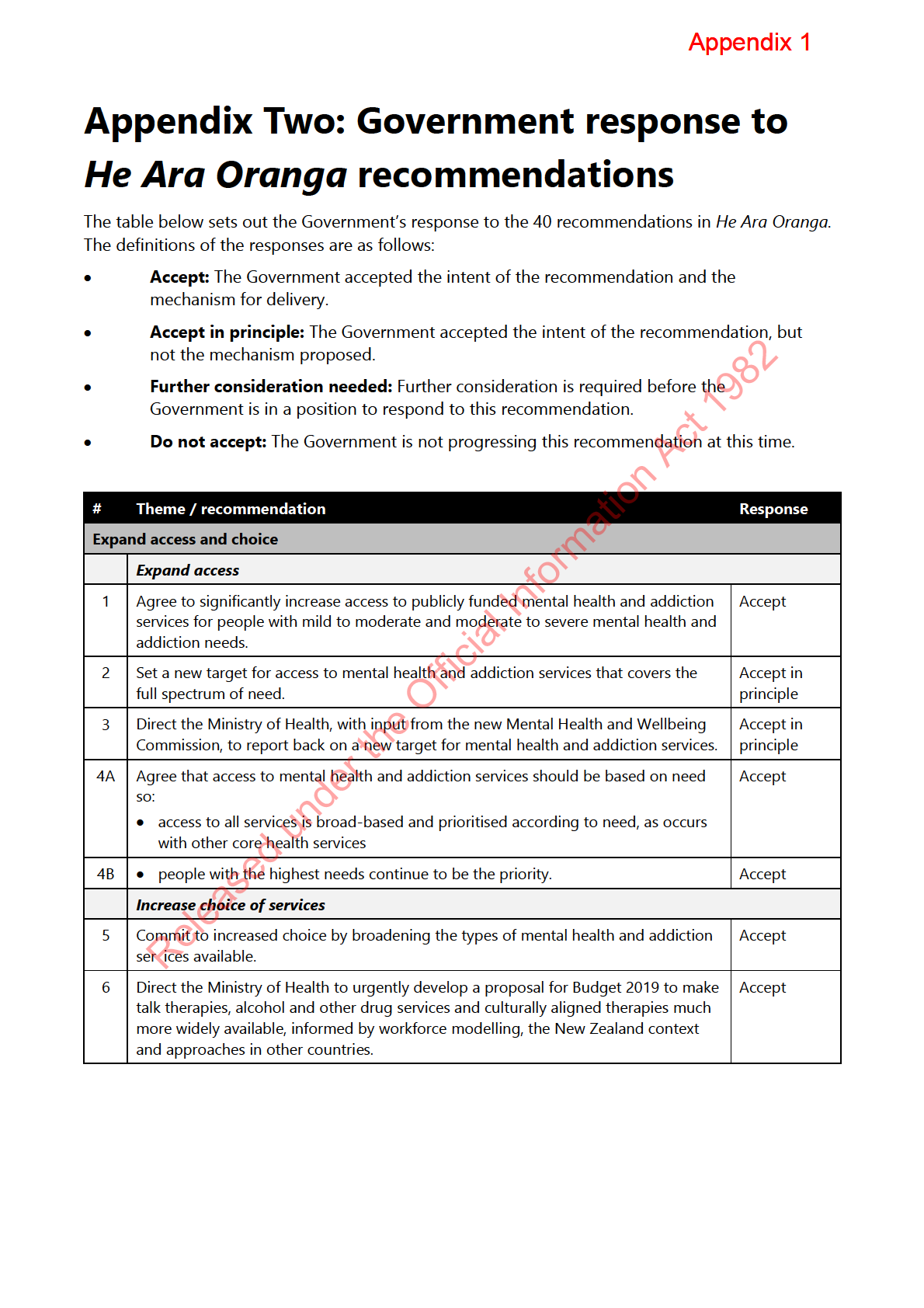
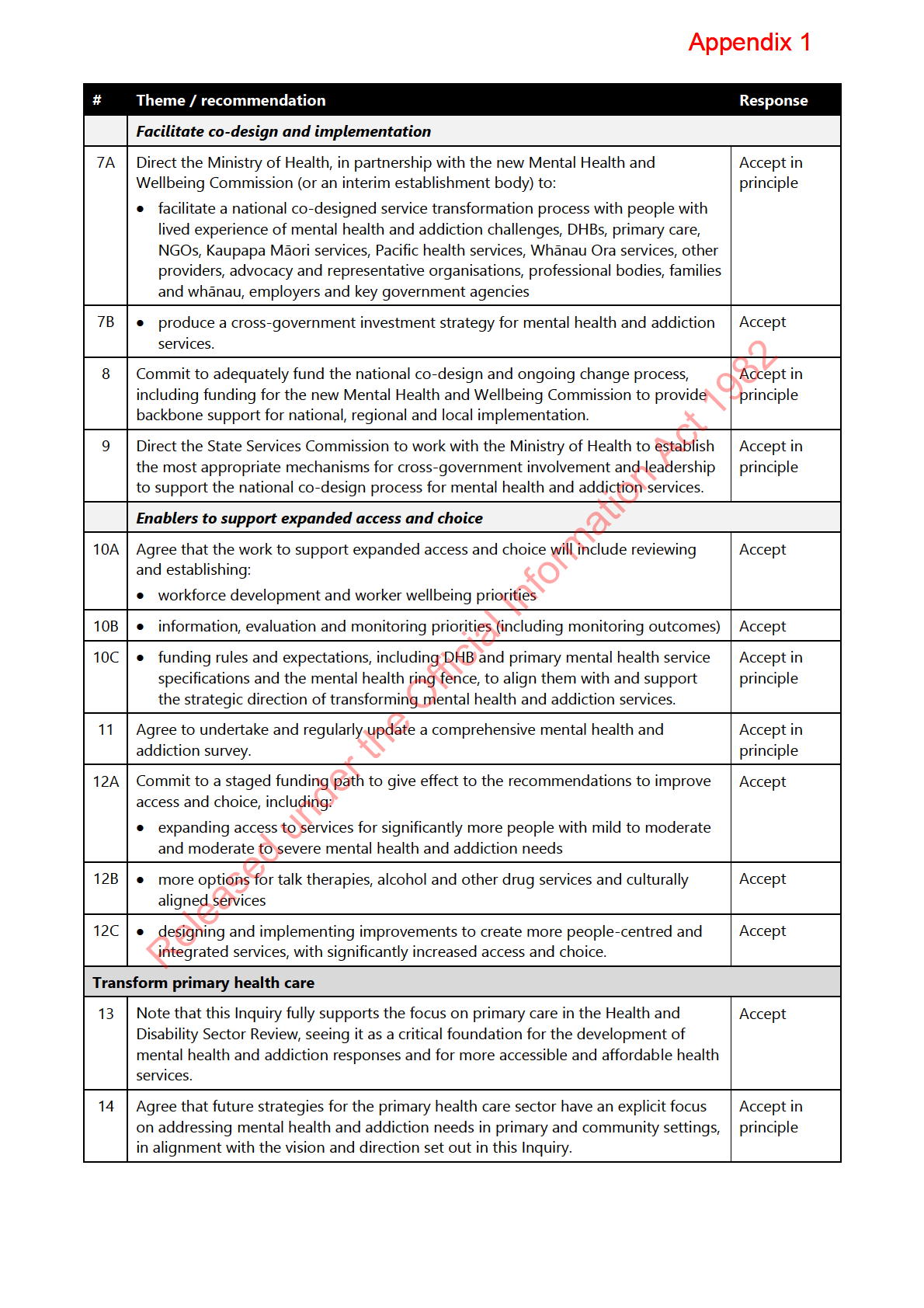
8.
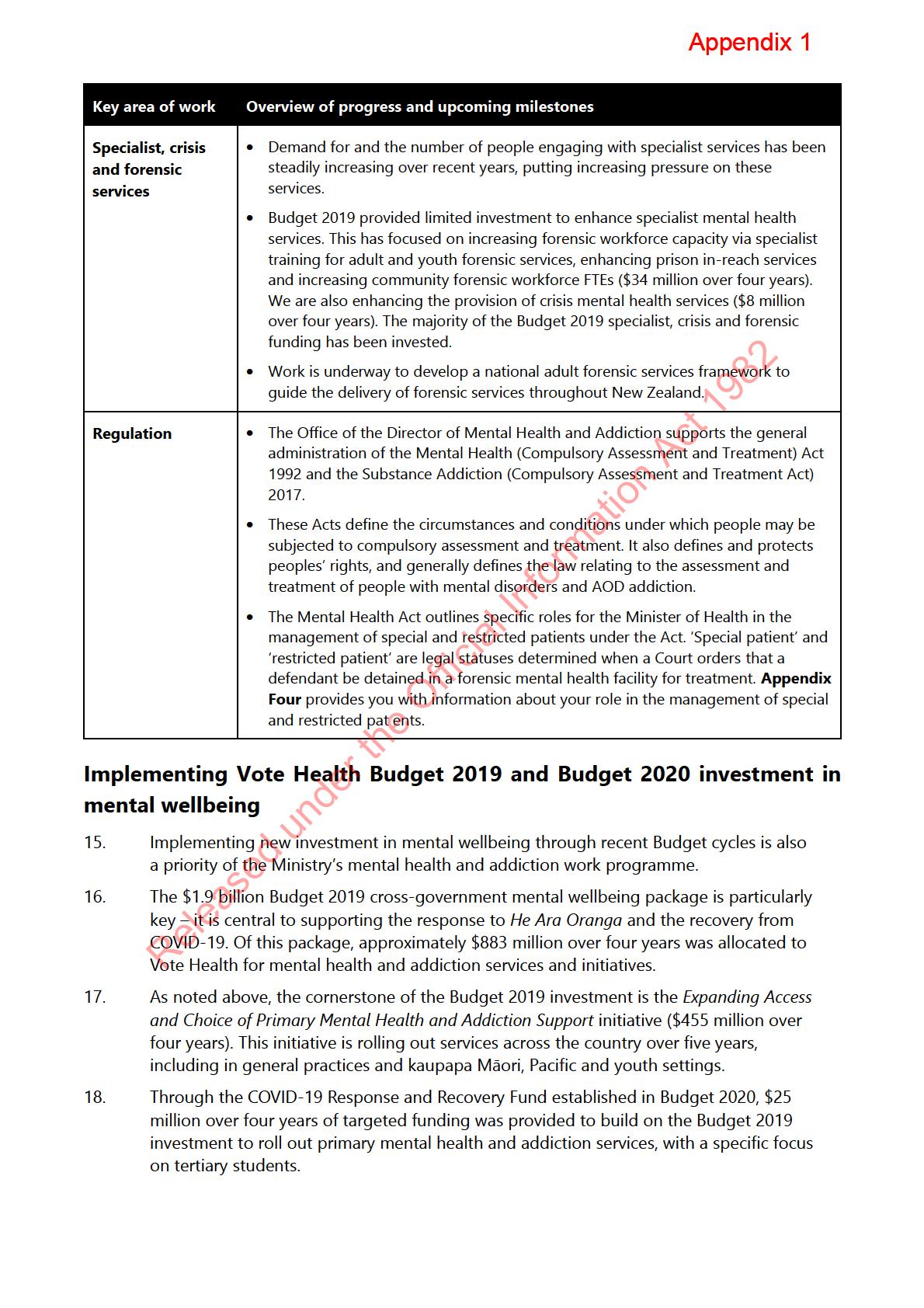
The then Government formally responded to
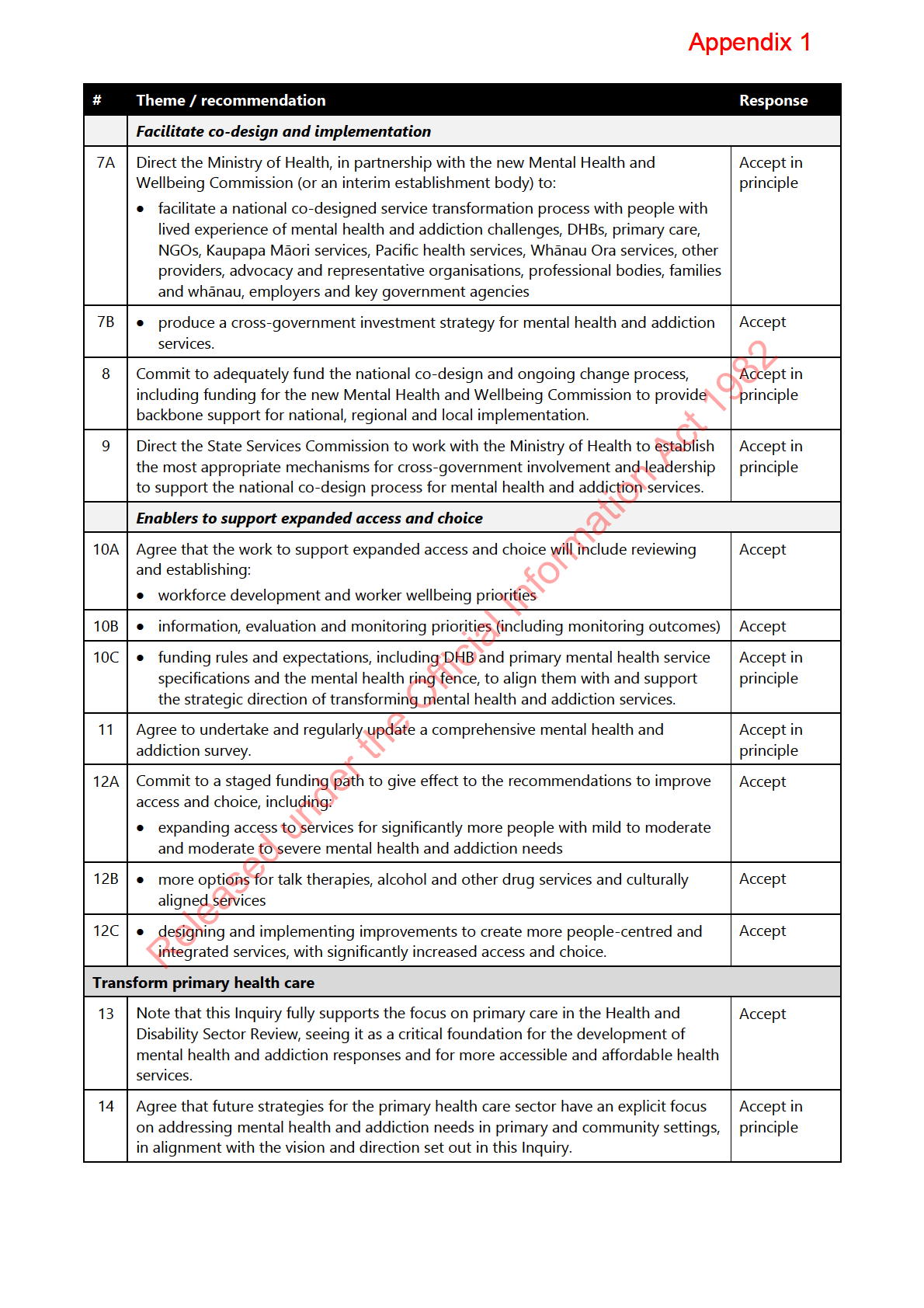
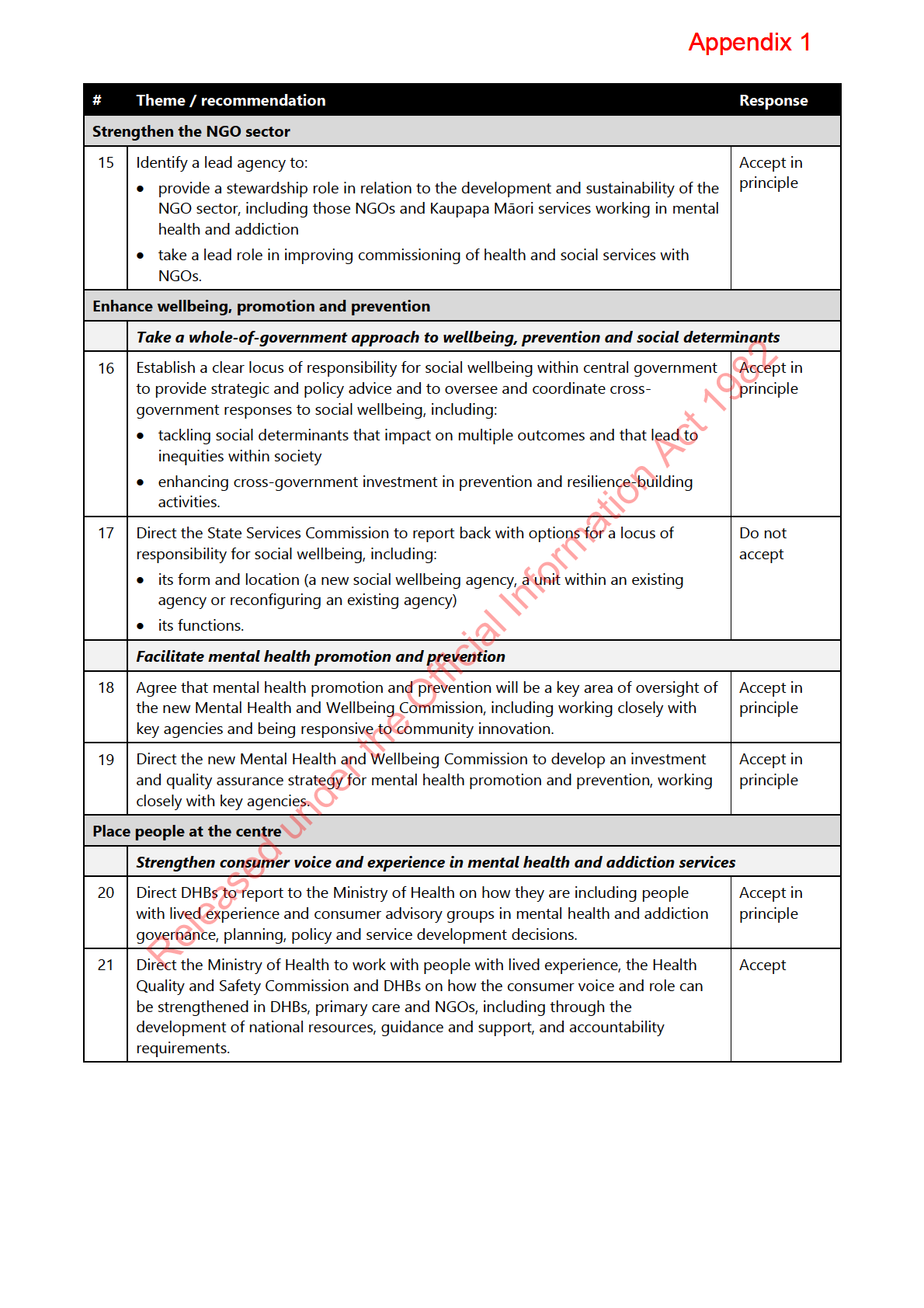
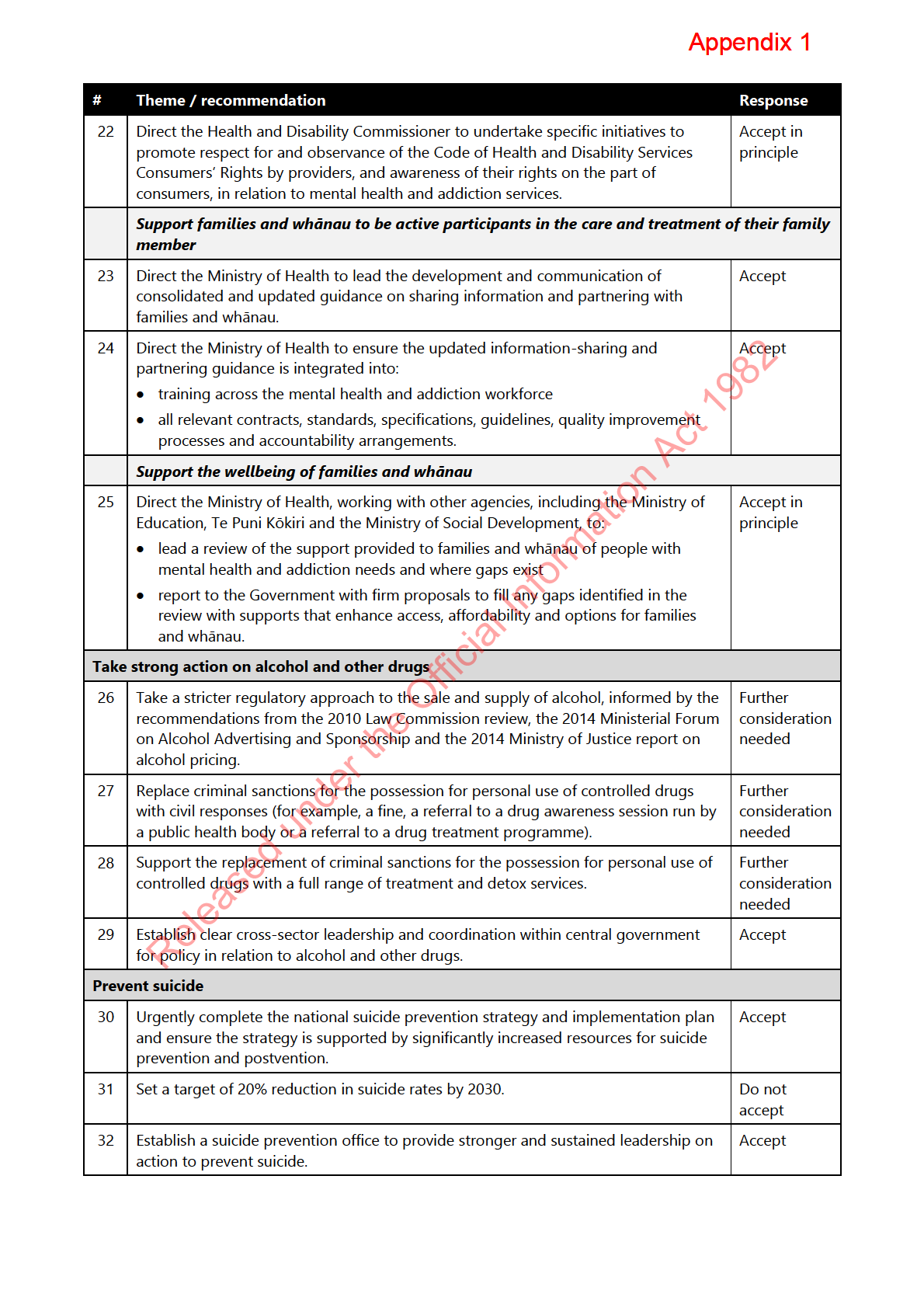
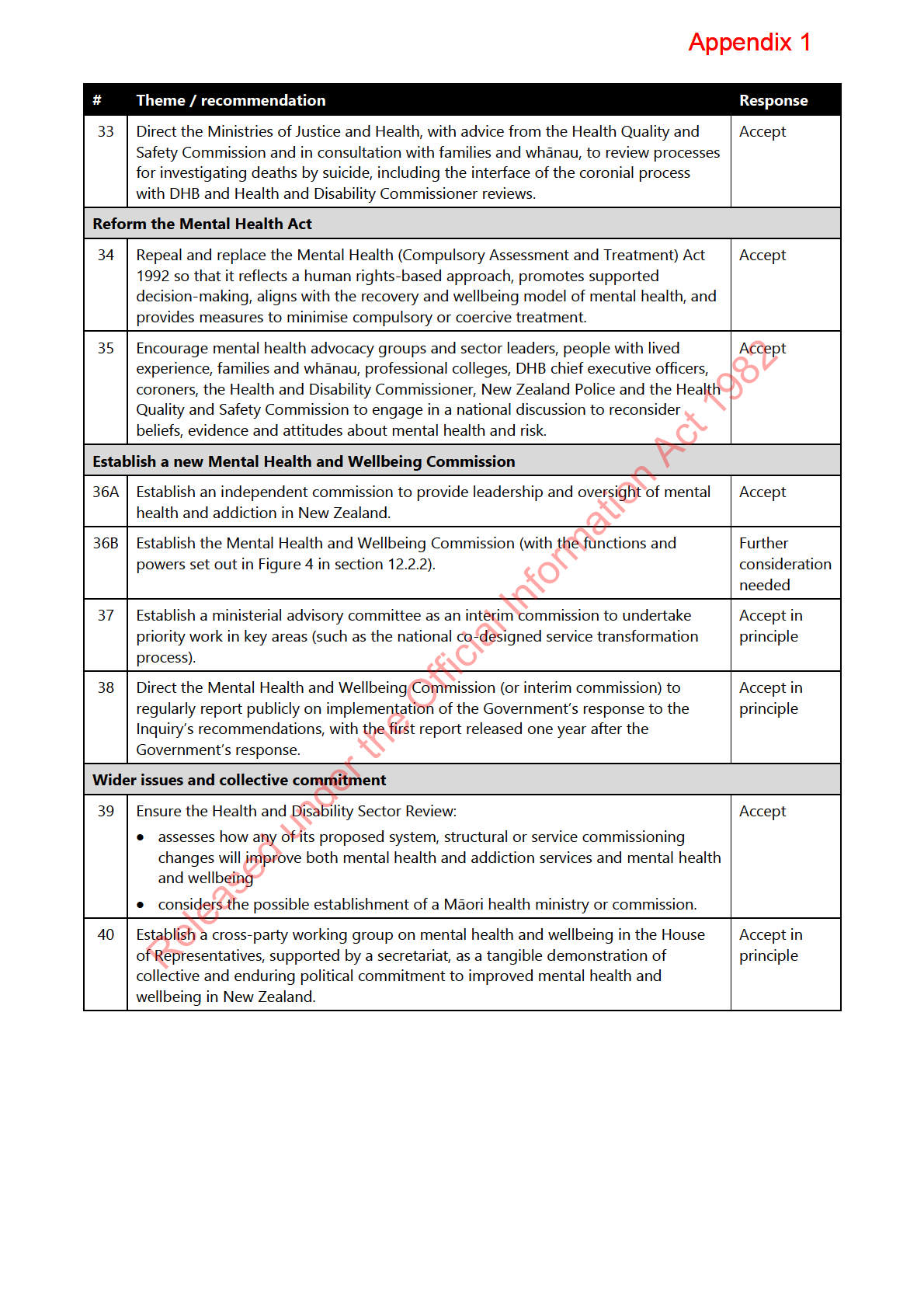
He Ara Oranga in May 2019,
accepting,
accepting in principle, or agreeing to further consider 38 of the 40 recommendations
[CAB-19-MIN-0182 refers].
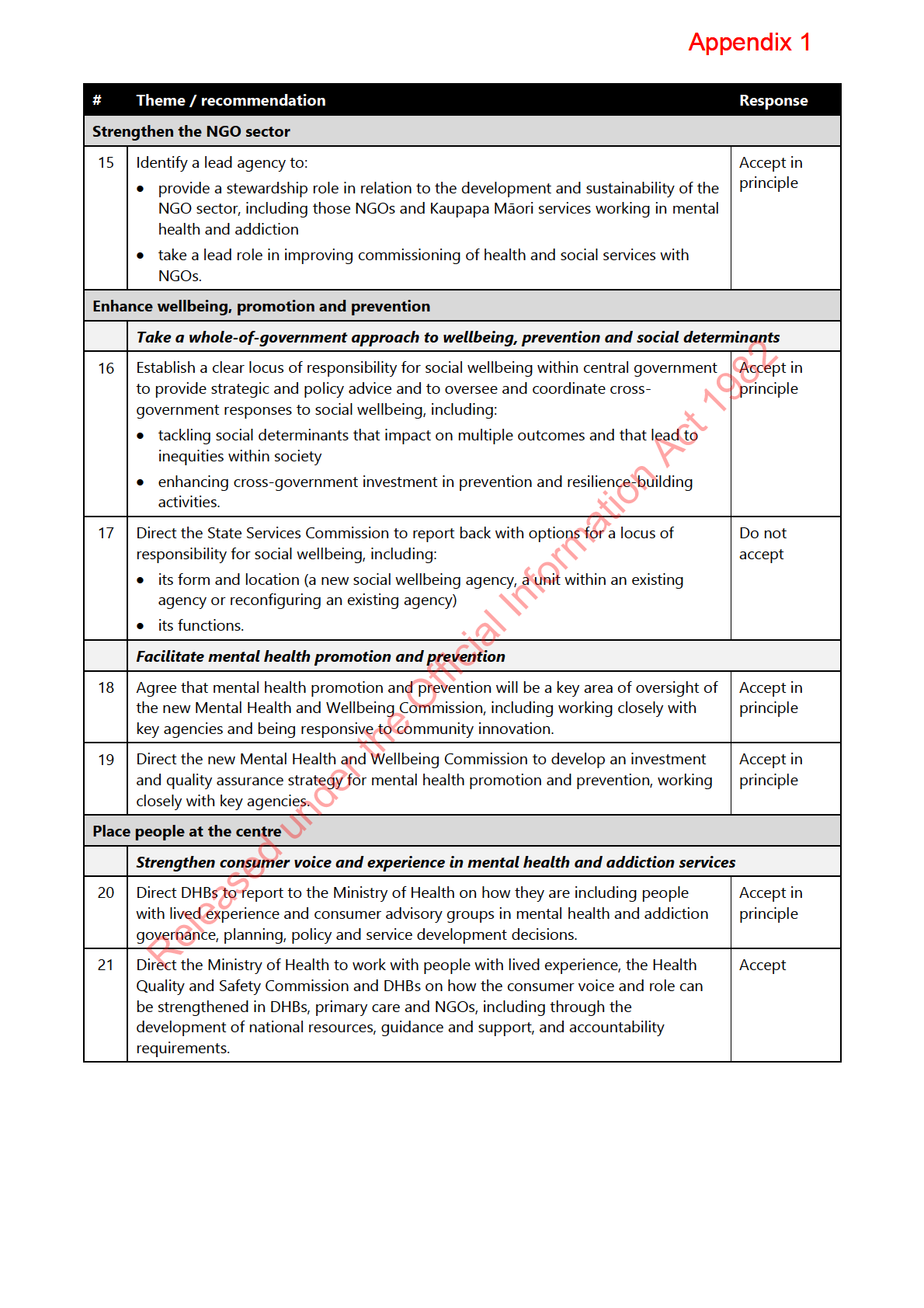
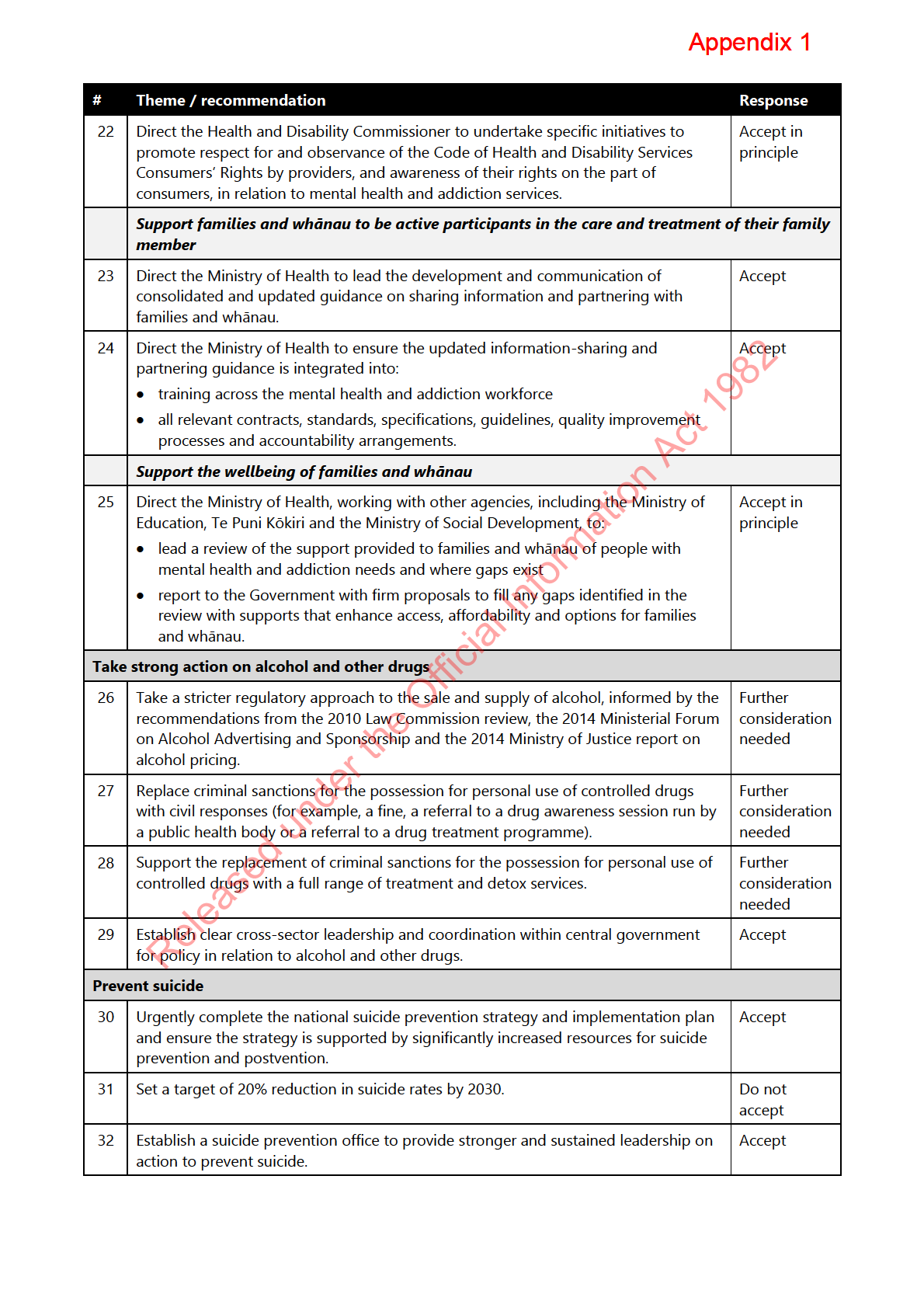
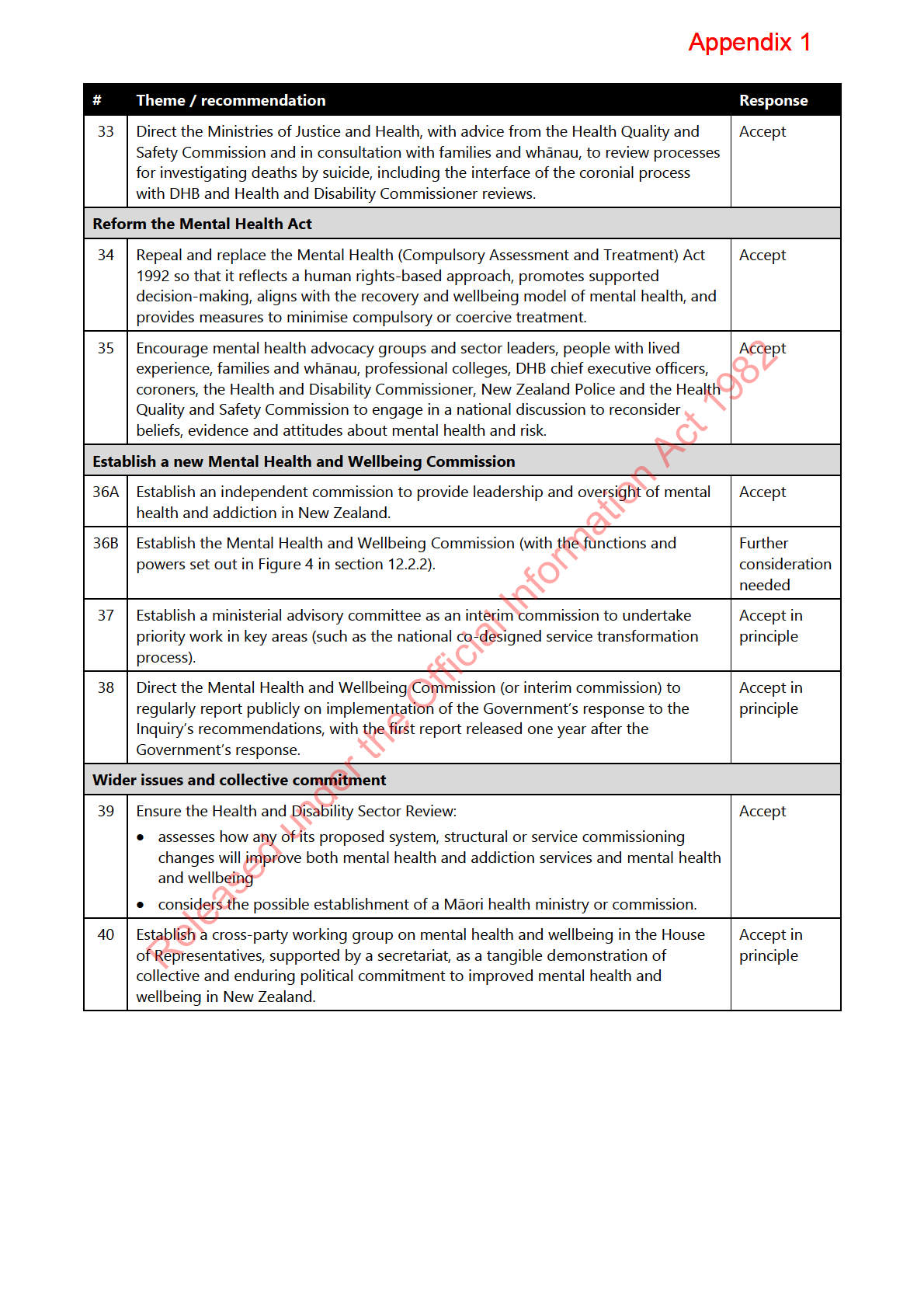
Appendix Two sets out the Government’s response to the
recommendations.
Implementing the Government’s response to He Ara Oranga
9.
Delivering on the Government’s response to
He Ara Oranga requires substantive system
shifts, actions and investment that will need to be prioritised and sequenced over the
short, medium and longer term. For this reason, the Ministry of Health’s (the Ministry’s)
mental health and addiction work programme is guided by the Government’s response
to
He Ara Oranga but has a focus on transforming the approach to mental health and
addiction that is broader than solely implementing the recommendations
.
10.
Operational matters such as oversight and administration of mental health and
addiction-related legislation, and work to support and monitor delivery of mental healt
1982 h
and addiction services, are also part of our work programme.
Act
A focus on achieving equity
11.
He Ara Oranga highlighted that there are significant inequities and unmet needs,
particularly for Māori, as well as for other population groups such as young people,
Pacific peoples, rainbow communities, disabled people, rural communities and people
interacting with the justice system. Further information about existing inequities is
included in
Appendix One.
Information
12.
Achieving equity underpins the Ministry’s mental health and addiction work. The
Ministry is beginning to address inequities through activities such as:
a. providing targeted funding for Māori and for population groups that experience
Official
inequitable mental health and addiction outcomes
b. collaboratively designing services with communities, and adopting new and
the
innovative procurement processes to support a broader range of kaupapa Māori,
Pacific and community providers to participate
c. expanding services in primary and community settings for people with mild to
under
moderate needs, who have historically had limited options for support
d. supporting increased access to services by Māori to reflect the fact that Māori have
higher rates of prevalence of mental health and addiction issues
e. improving the current application of the Mental Health (Compulsory Assessment
and Treatment) Act 1992 (the Mental Health Act) to reduce the use of compulsory
Released
treatment for Māori, while reforming the Act to embed a human rights approach.
Key areas of work underway
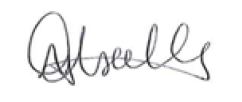
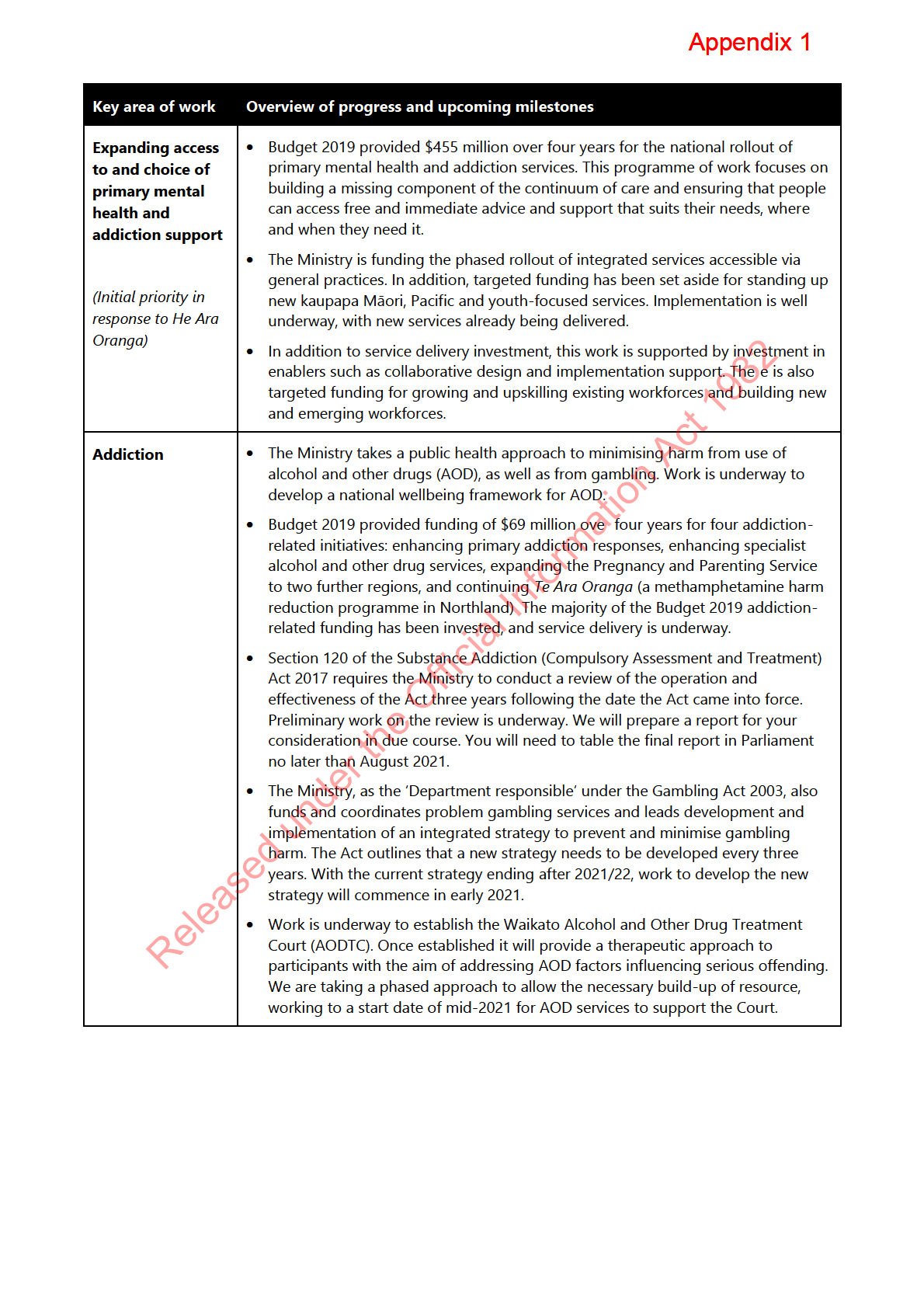
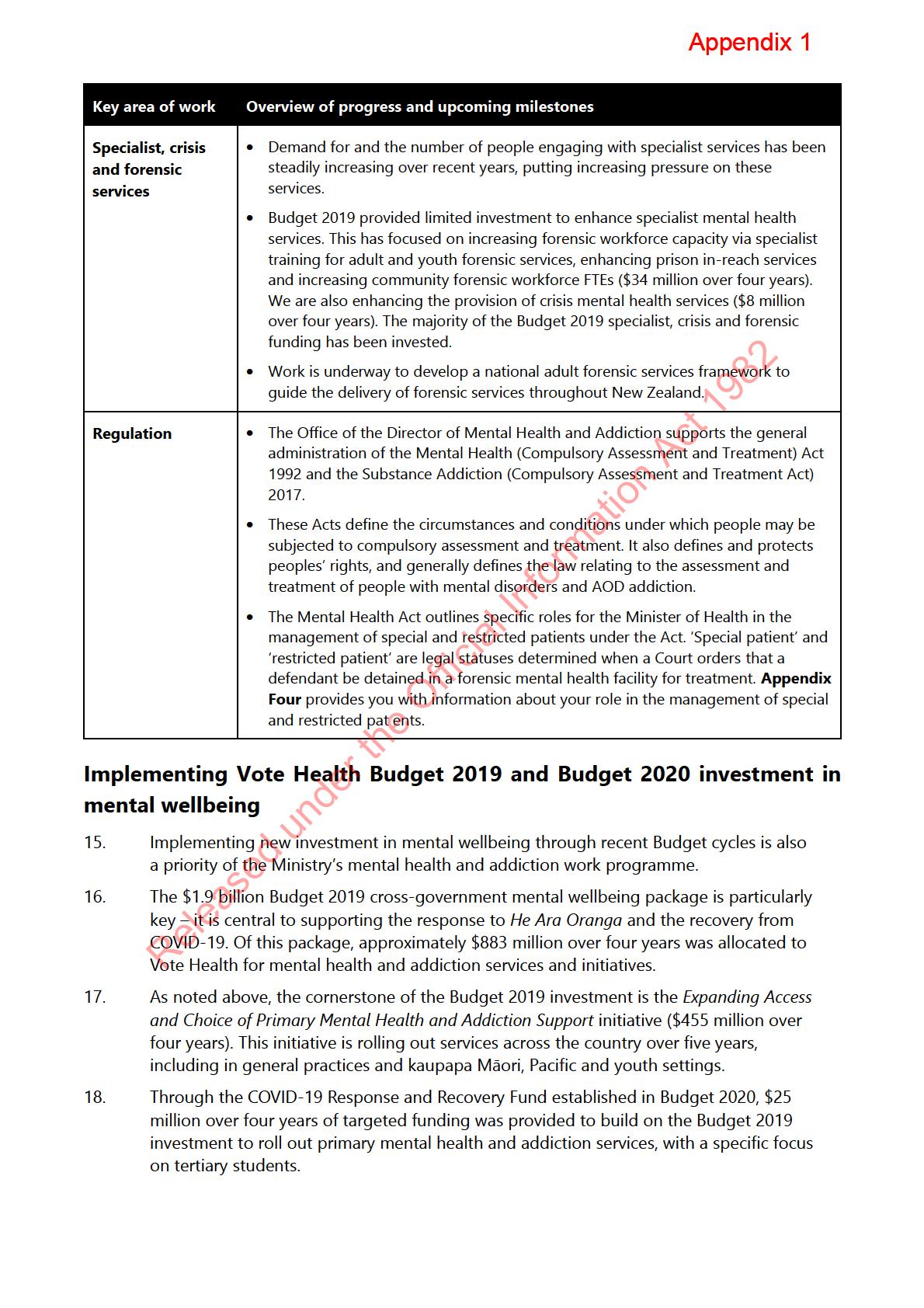
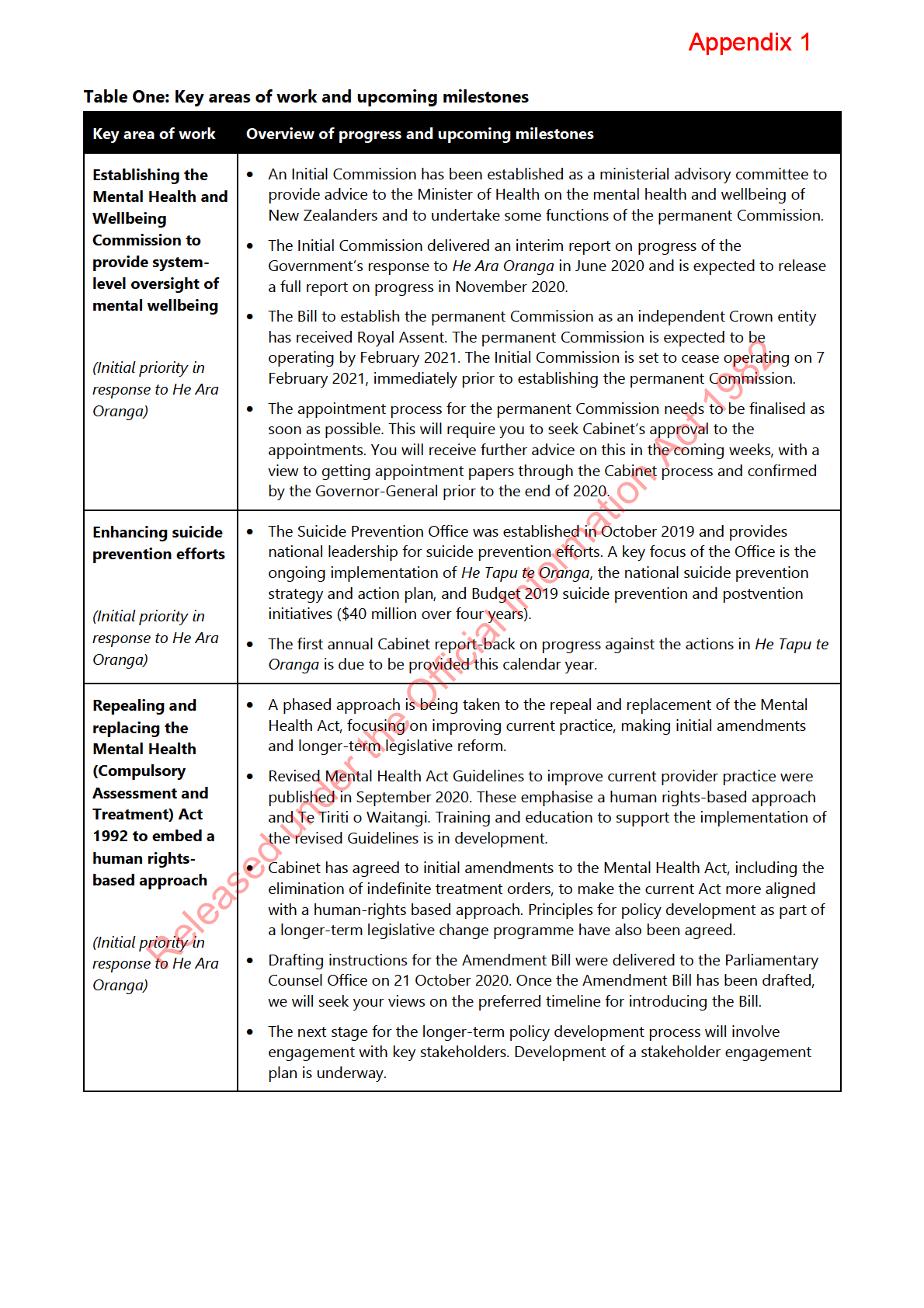
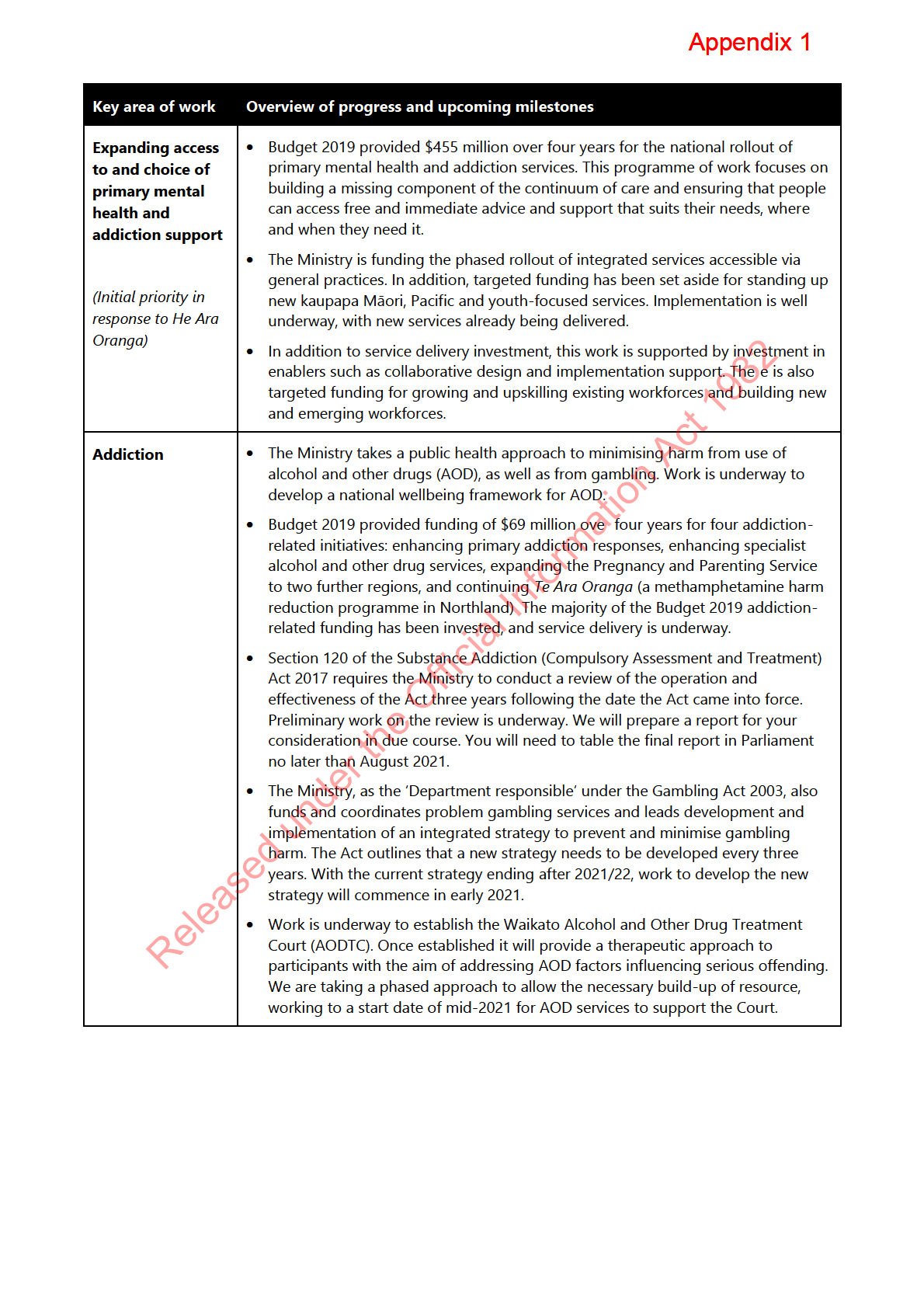
13.
Table One outlines key information about areas of work and upcoming milestones that
are underway to help transform our approach to mental health and addiction. This
includes work related to the initial priorities the then Government identified as part of its
response to
He Ara Oranga, as well as work to respond to specific recommendations in
He Ara Oranga.
14.
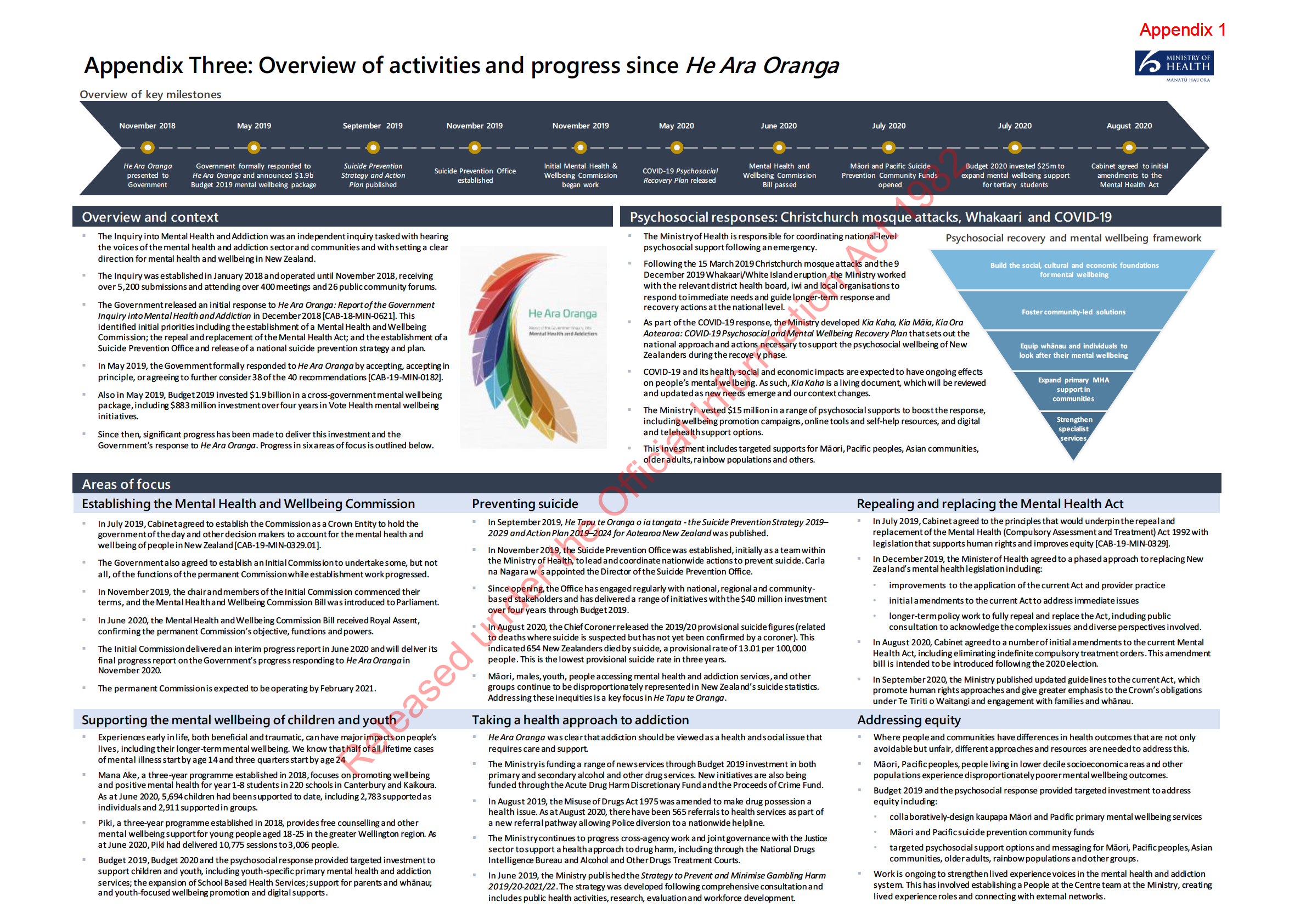
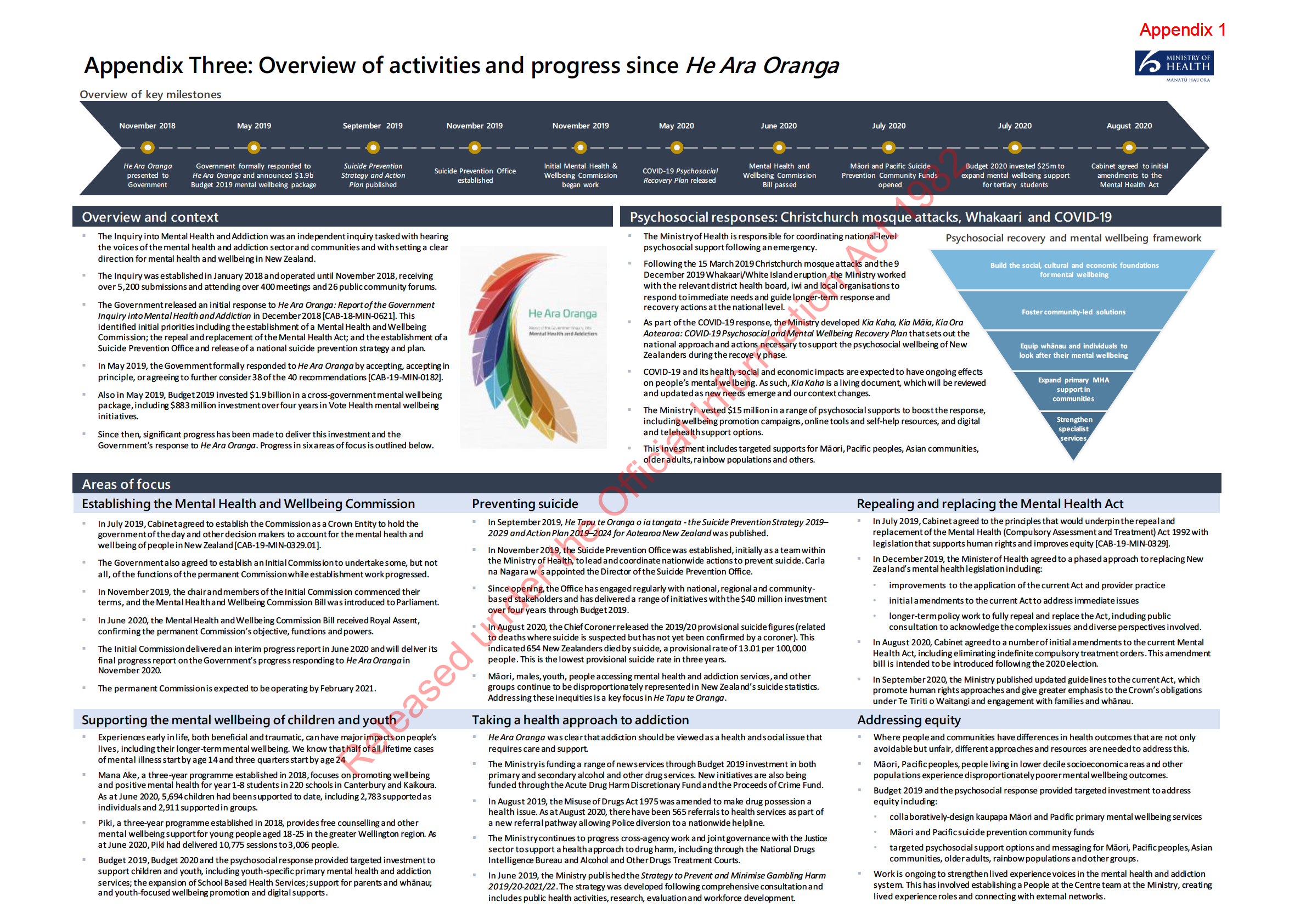
The A3 attached as
Appendix Three provides an overview of progress made since the
Government’s response to
He Ara Oranga.
1982
Act
Information
Official
the
under
Released
1982
Act
Information
Official
the
under
Released
1982
Act
Information
Official
the
under
Released
Appendix 1
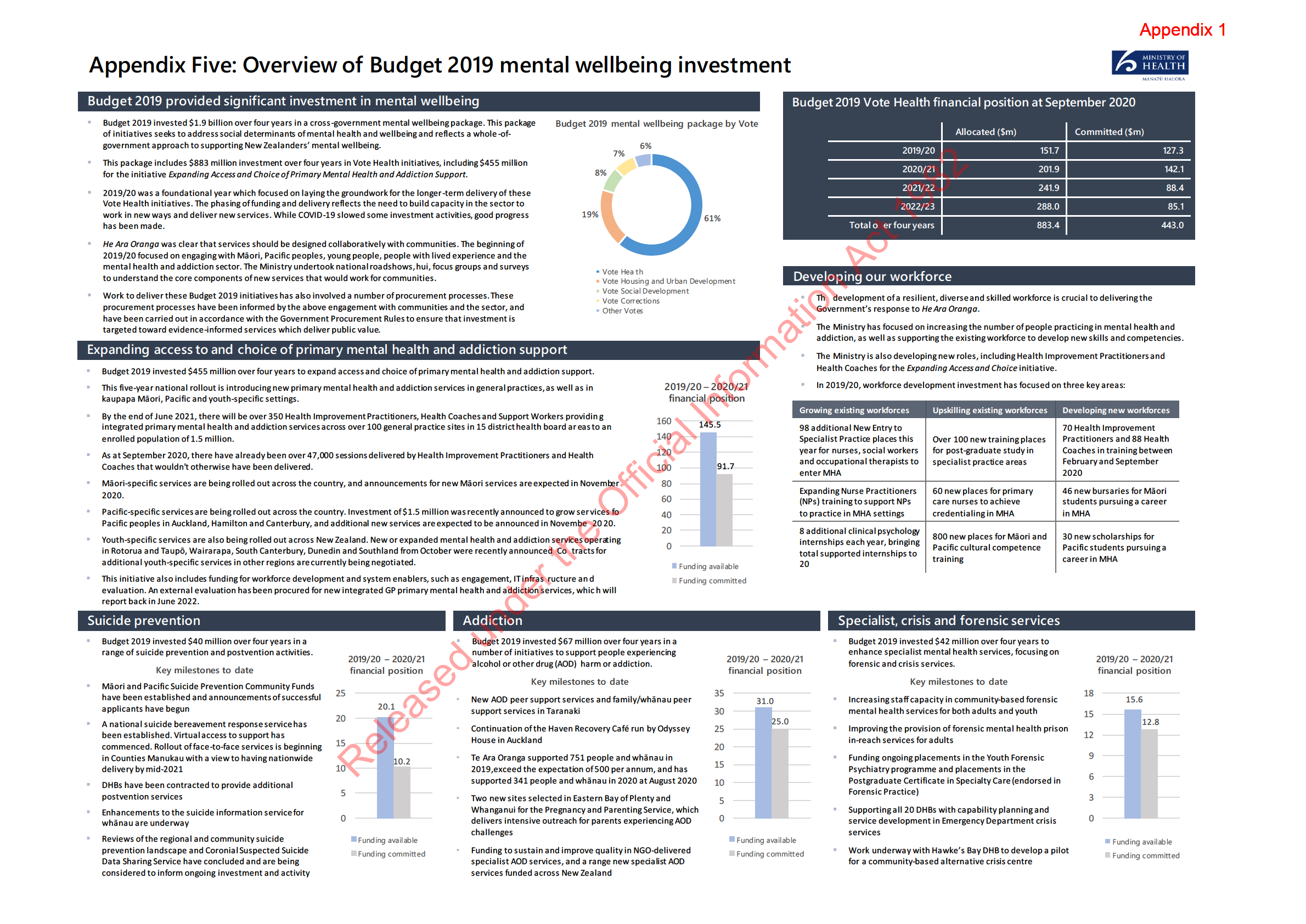
19.
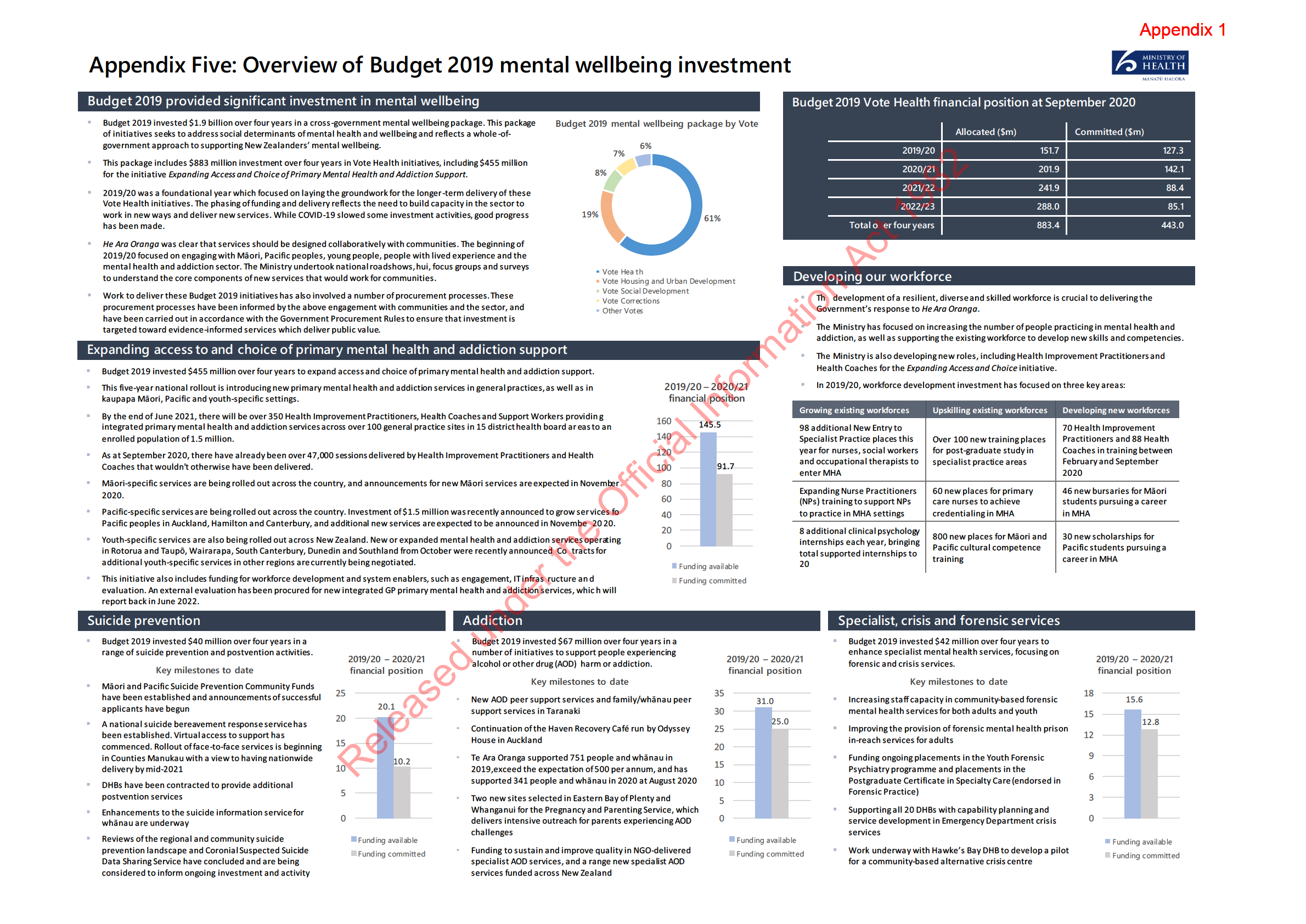
The remainder of Vote Health investment in the Budget 2019 mental wellbeing package
provided top-ups to support work in other areas such as suicide prevention, specialist
addiction treatment, school-based mental wellbeing and forensic mental health services.
20.
Delivery of Budget initiatives is well underway. The A3 attached as
Appendix Five provides an overview of progress made implementing Budget 2019 Vote Health mental
wellbeing investment.
21.
The previous Minister of Health reported monthly to the Cabinet Priorities Committee on
implementation of the Vote Health Budget 2019 mental wellbeing initiatives.
Progressing manifesto commitments
22.
The Ministry is actively planning to implement Labour’s 2020 election manifesto
commitments for new mental health and addiction initiatives once decisions are made
by you and Cabinet, including around new funding. These initiatives complement our
1982
current work programme for implementing the Government’s response to
He Ara
Oranga and recent investments in mental wellbeing
. They align strongly with our focus
Act
on supporting the mental wellbeing of children, young people and their parents and
whānau; taking a health approach to addressing AOD harm; and addressing inequitable
mental wellbeing outcomes.
23.
S9(2)(f)(iv)
Information
24.
Official
the
25.
under
26.
Released
Leading the psychosocial response to COVID-19
27.
The Ministry is leading the psychosocial response to COVID-19, including the
development of
Kia Kaha, Kia Māia, Kia Ora Aotearoa: Psychosocial and Mental
Wellbeing Plan (
Kia Kaha).
Kia Kaha is a cross-sectoral plan that sets out a national
mental wellbeing framework to guide collective efforts across national, regional and
local levels.
Appendix 1
28.
The first version of
Kia Kaha was released in May 2020. An updated version is expected
to be released before the end of the year. The updated version of
Kia Kaha represents
the first phase of a longer-term pathway to implement the response to
He Ara Oranga.
This updated version will include cross-government actions over the next 12–18 months,
including actions as part of the response to
He Ara Oranga.
29.
The Ministry is also implementing the $15 million one-off investment allocated to
support the psychosocial response. This investment has supported wellbeing promotion
campaigns, digital self-help tools, telehealth services and targeted supports for priority
populations such as Māori, Pacific peoples, Asian communities, older adults and rural
communities.
Long-term pathway for transformation
30.
The former Minister of Health was previously invited to report back to Cabinet with a
long-term pathway to transform New Zealand’s approach to mental health and
1982
addiction [CAB-19-MIN-0182 refers]. S9(2)(f)(iv)
Act
31.
The long-term pathway is intended to outline the direction for our approach to mental
health and addiction over the next ten years, and to guide the actions and investment
needed to achieve the transformative change called for in
He Ara Oranga.
32.
The long-term pathway will build on
Kia Kaha but will need to be flexible as work
progresses, including with any relevant changes in response to the Health and Disability
System Review, and as New Zealanders’ needs and aspirations change
Information . It will also need
to reflect ongoing engagement with Māori, people with lived experience of mental
health and addiction issues, whānau and communities.
33.
S9(2)(f)(iv)
Official
. The release
the
of an updated version of
Kia Kaha will help respond to public calls for a clear action plan
to implement
He Ara Oranga in the interim.
34.
Officials can provide you with further advice on next steps for progressing the long-term
pathway to help inform decisions about
under
the Cabinet report-back.
Priority areas for future investment
35.
The Government’s response to
He Ara Oranga acknowledged that multiple years of
significant and sustained effort and investment will be required to transform our
approach to mental
Released health and addiction.
36.
Moreover, while there has been a recent increase in investment in mental health and
addiction services, there is still significant pressure on some parts of the system.
37.
S9(2)(f)(iv)
Appendix 1
c. resource to support the implementation of the initial amendment to the Mental
Health Act to eliminate indefinite treatment orders
s 9(2)(f)(iv)
38.
Officials are able to provide further advice on these areas, as well as any immediate
manifesto commitments that require funding that you wish to progress.
Upcoming ministerial decisions
39.
Over the coming months there are a number of decisions that will likely need to be
sought from you or Cabinet, including the following:
a. appointments for the new Mental Health and Wellbeing Commission 1982
b. S9(2)(f)(iv)
Act
c. timing of and content for the Cabinet report-back on suicide prevention
d. progression of the Bill to implement initial amendments to the Mental Health Act
e. appointments to the Mental Health Review Tribunal and appointment of deputy
district inspectors (refer
Appendix Four for further information)
f. areas for focus of Budget 2021 mental wellbeing bids
Information
g. whether to continue providing monthly updates to the Cabinet Priorities Committee
on progress implementing the Vote Health Budget 2019 mental wellbeing initiatives.
40.
Information about indicative upcoming milestones and matters requiring ministerial or
Cabinet decisions is also outlined in
Appendix Six.
Official
Next steps
the
41.
Officials are available to discuss and can provide further information and advice on the
matters raised in this report.
under
ENDS.
Released
Appendix 1
Appendix One: Current state and system
overview
Mental wellbeing needs
1.
It is estimated that each year one in five people in New Zealand will experience mental
illness or significant mental distress, and over 50–80 percent of New Zealanders will
experience mental distress, addiction challenges or both in their lifetime. These
challenges have flow-on impacts for people’s whānau, families and communities.
2.
Suicide is a major issue in New Zealand, with persistently high suicide rates and a youth
suicide rate that is amongst the highest in the Organisation for Economic Co-operation
and Development (OECD). Every year over 550 people die by suicide. It is estimated that
1982
every year around 150,000 people will think about taking their own life; 50,000 will make
a plan to take their own life; and 20,000 will attempt to take their own life.
Act
3.
People’s mental wellbeing needs are strongly influenced by their experiences earlier in
life. Half of all lifetime cases of mental illness are thought to start by 14 years of age and
three quarters start by 24 years of age. Experiencing poor mental health early in life can
have lifelong impacts, including reduced participation in the future workforce, enduring
disability and/or poor family and social functioning Intervening early can however
significantly improve long-term outcomes and reduce future dependence on the health
Information
and social system.
Impact of COVID-19 on mental wellbeing needs
4.
COVID-19 and the measures taken to control it have affected the lives of all people in
Official
New Zealand. We have seen a direct impact on people’s mental wellbeing, including
higher levels of distress, anxiety, and a sense of uncertainty about the future.
the
5.
People’s mental wellbeing is also indirectly affected by the impacts of COVID-19 on
other areas such as education, income and employment, and family and community
relationships.
under
6.
Most people, whānau and communities can recover and adapt in challenging times, and
we have already seen positive examples of increased community cohesion, innovation
and resilience. However, we expect to see impacts on mental wellbeing and mental
health and addiction service demand continue to emerge in the coming months and
years, particularly associated with the potentially long-lasting economic impact of
COVID-19.
Released
Equity
7.
He Ara Oranga highlighted that there are significant inequities and unmet needs,
particularly for Māori, as well as for other population groups such as Pacific peoples,
refugees and migrants, rainbow communities, rural communities, disabled people,
veterans and people interacting with the justice system. People at certain stages of the
life course also experience inequitable outcomes, including young people, older people
and children experiencing adverse childhood events or in state care.
Appendix 1
8.
For example:
a. around 30 percent of Māori are estimated to have experienced mental health and
addiction challenges in the past 12 months, compared to around 20 percent of non-
Māori
b. Māori are approximately four times more likely than non-Māori to be subject to
compulsory treatment orders
c. the suicide rate among Māori is 2.1 times higher than among non-Māori
d. Māori and Pacific people are estimated to be more likely to have experienced
alcohol abuse or dependence in the past 12 months than people from other ethnic
groups (7.4, 4.2 and 2.2 percent respectively)
e. young people aged 15–24 years have the highest suicide rate of all life-stage age
groups (16.8 per 100,000 people compared to 11.3 per 100,000 people for the
general population), with Māori young people aged 15–24 years having a rate 2
1982.7
times higher than non-Māori young people
Act
f. males are more likely to experience alcohol abuse than females (16.3 percent
compared with 6.9 percent).
9.
People with mental health and addiction needs also experience disproportionately
higher levels of other health and social issues, such as poorer physical health outcomes,
homelessness, interaction with the justice system, unemployment and poverty. Poor
physical health and social outcomes are also associated with an increased likelihood of
people experiencing mental health and addiction needs.
Information
Mental health and addiction system overview
10.
Over the last few decades, the mental health and addiction sector has moved from an
Official
institutional base to a stronger focus on community-based services. There has been a
wide range of community services developed, as well as further development of
the
specialist and acute services.
11.
New Zealand’s health and disability system now provides a continuum of mental health
and addiction services. This includes:
under
a. wellbeing promotion for all New Zealanders
b. primary-level mental health, substance use and problem gambling services,
including support accessed through general practice and in the community
c. specialist services to support those with higher and more complex needs, including
crisis responses for people experiencing significant distress and forensic services for
Released
people interacting with the justice system.
12.
It is important to note that other sectors also contribute to mental wellbeing through
providing support for the social, economic and cultural foundations of mental wellbeing,
and through ensuring people’s mental wellbeing is supported through interactions with
the social, education and justice systems.
Appendix 1
Workforce
13.
The mental health and addiction workforce is diverse and includes a range of clinical
roles (eg, nurses, social workers, psychologists and doctors) and non-clinical roles (eg,
peer workers, employment support workers and cultural support workers). The
workforce in Vote Health-funded mental health and addiction services is estimated to be
around 12,500 full-time equivalent (FTE) staff and represents about 12 percent of the
total DHB workforce.
14.
In recent years, growth in the mental health and addiction workforce has been slower
than the increase in demand for mental health and addiction services. This is placing
increasing pressure on the workforce and services.
15.
He Ara Oranga called for new and different support options for New Zealanders, which
will require the development of a more diverse workforce and the use of workforces in
different ways. Workforce growth and development is a key focus of the Ministry’s work
1982
programme to implement the Government’s response to
He Ara Oranga (refer
Appendix Five for further information about workforce development)
Act
Mental health and addiction funding
16.
Historically, funding for mental health and addiction has focused on specialist mental
health and addiction services, which provided support to 3.7 percent of the population
in 2019/20.
17.
In 2018/19, of the approximately $1.53 billion of Vote Health funding spent on mental
Information
health and addiction (excluding pharmaceuticals and general medical services funded to
help treat or manage mental health matters):
a. around 95 percent was distributed via DHBs. Around 30 percent of this was used to
purchase services delivered by non-governmental organisations and primary health
Official
organisations
b. around 89 percent was spent on mental health services, and the remaining
the
approximately 11 percent was spent on addiction services.
18.
Mental health and addiction expenditure in DHBs is ‘ring-fenced’. This means that
although a DHB has discretion over where it allocates funding and can increase its
under
allocation to mental health and addiction, it cannot spend less than the previous year on
mental health and addiction.
19.
The Ministry of Health also contracts directly with NGOs and DHBs for some mental
health and addiction services. Additionally, some NGOs may receive funding from other
government agencies or through grants and philanthropic sources.
Released
1982
Act
Information
Official
the
under
Released
1982
Act
Information
Official
the
under
Released
1982
Act
Information
Official
the
under
Released
1982
Act
Information
Official
the
under
Released
1982
Act
Information
Official
the
under
Released
1982
Act
Information
Official
the
under
Released
Appendix 1
Appendix Four: Ministerial responsibilities
for decisions about special and restricted
patients
Purpose of appendix
1.
This appendix informs you of your role in the management of special patients and
restricted patients under the Mental Health (Compulsory Assessment and Treatment) Act
1992 (Mental Health Act).
Special and restricted patients
1982
2.
‘Special patient’ and ‘restricted patient’ are legal statuses determined when a Court
Act
orders that a defendant be detained in a forensic mental health facility for treatment.
3.
A defendant who is charged with an imprisonable offence and is suspected of being
mentally impaired can be assessed under the Criminal Procedure (Mentally Impaired
Persons) Act 2003 (Criminal Procedure Act). After an assessment, defendants can be
made a special patient if they meet the definition of ‘mental disorder’ in the Mental
Health Act.
Information
4.
The main categories of special patients are:
a. unfit to stand trial because of a mental disorder
b. not guilty by reason of insanity (as defined in the Crimes Act 1961)
Official
c. found guilty but the Court orders compulsory mental health treatment instead of, or
as well as, a prison sentence
the
d. people transferred from a Corrections facility (sentenced or on remand) to a forensic
mental health facility for treatment.
5.
Forensic mental health services provide treatment and rehabilitation services for
under
mentally disordered offenders, alleged offenders, or people who pose a high risk of
offending. Forensic mental health services provide inpatient treatment facilities (such as
secure units and step-down rehabilitation units) and community mental health services.
6.
When a person is made a special patient after being found not guilty by reason of
insanity, the order is for an indefinite period. A person found unfit to stand trial may be
Released
detained subject to a special patient order for up to half of the maximum sentence to
which they would otherwise be subject, to a maximum of 10 years, or until the person
becomes fit to stand trial.
7.
‘Restricted patients’ are compulsory mental health patients that present special
difficulties because of the danger they pose to themselves and others. The Court makes
decisions about restricted patient status based on an application from the Director of
Mental Health under the Mental Health Act.
Appendix 1
8.
The number of special patients is relatively small with about 130 people currently
detained under such provisions. There are currently only four people with restricted
patient status. Approximately 50 to 60 ministerial decisions are required for special and
restricted patients each year. Information on the nature and type of decisions you will be
required to make are outlined in the sections below.
Management of special and restricted patients
9.
The legal framework for managing special and restricted patients is set out in the
Criminal Procedure Act and the Mental Health Act.
10.
Special and restricted patients are detained for treatment in one of the five Regional
Forensic Psychiatric Services located in Auckland, Hamilton, Wellington (with a site in
Whanganui), Christchurch and Dunedin.
11.
Special and restricted patients are progressively reintegrated into the community by
1982
being granted leave from a secure forensic mental health facility. This approach enables
both the forensic mental health service and special patient to work towards planned
Act
treatment and recovery goals while giving due consideration to public safety.
12.
Each forensic mental health service conducts regular Special Patient Review Panels to
review the clinical progress of special patients and make recommendations for treatment
and rehabilitation. The Panels are made up of representatives from a multi-disciplinary
team that works with the special patient and may have a member external to the service.
13.
The Director of Mental Health may grant special and restricted patients up to six nights
Information
of leave per week (‘short leave’), requiring a return to hospital at least once per week
(section 52 of the Mental Health Act).
14.
Once a patient has demonstrated an ability to live safely and adaptively in the
community on unsupervised short leave, the responsible clinician can apply for longer
Official
periods of leave in the community, referred to as ‘ministerial long leave’ (section 50 of
the Mental Health Act).
the
15.
Once the responsible clinician is satisfied that the special/restricted patient no longer
requires management as a special/restricted patient, they may also apply for a change of
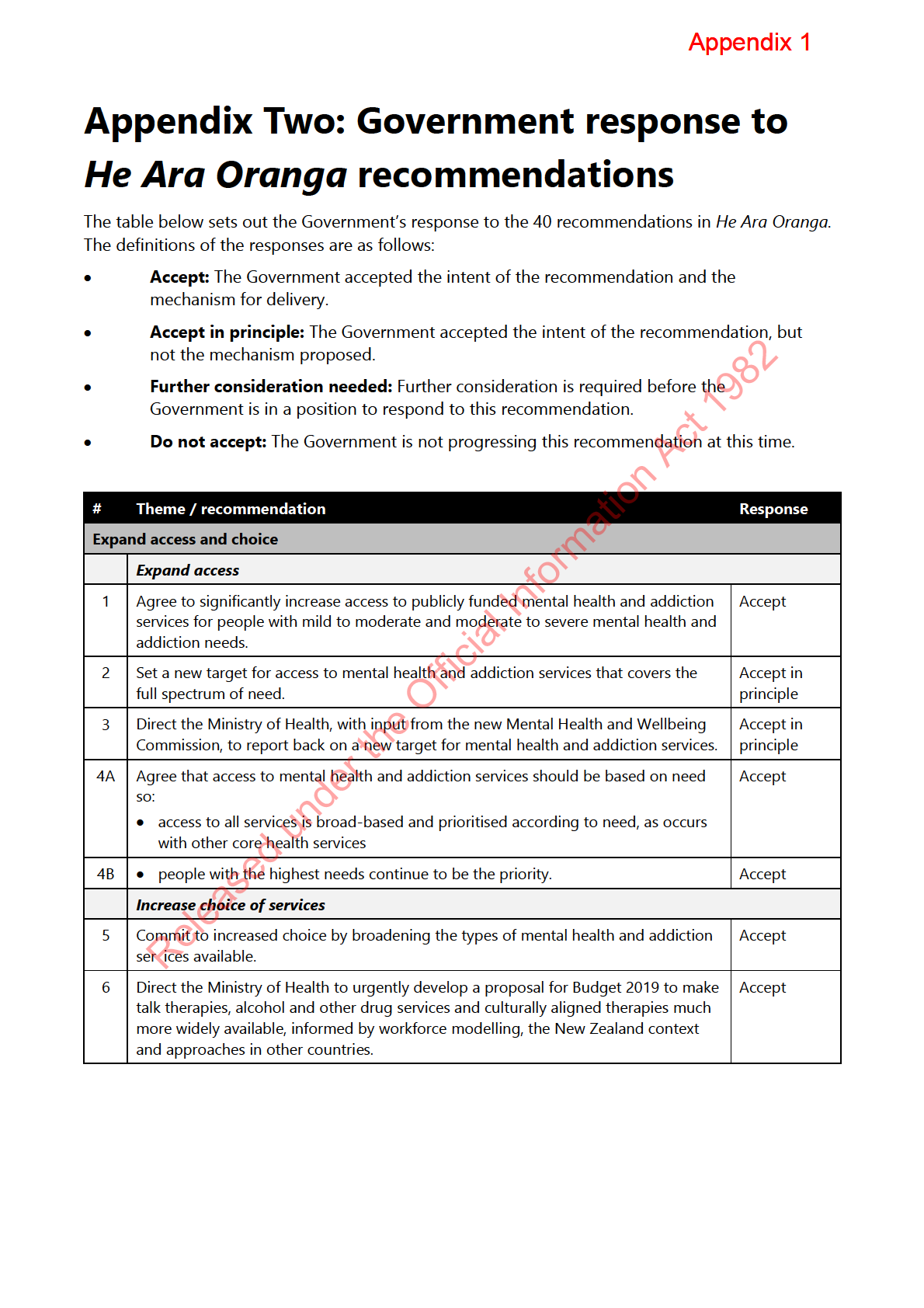
legal status. Figure 1 sets out the rehabilitative pathway for special and restricted
under
patients.
16.
The Minister of Health is responsible for making decisions on applications for long leave
and changes of legal status of certain special and restricted patients. These decisions
mark an important milestone in a person’s rehabilitation and reintegration into the
community. It can take years for a person to reach these milestones, and it is a
Released
meaningful occasion for them and their treating team.
Director of Mental Health
17.
The Director of Mental Health, Dr John Crawshaw, has oversight of the management of
special and restricted patients in New Zealand. The Director has specific powers in
relation to:
a. granting applications for short leave (section 52 of the Mental Health Act)
b. approving special patient transfers to another hospital (section 49)
Appendix 1
c. approving the return of certain inpatient special patients to prison, once their
mental health can be adequately managed in prison (section 47).
18.
The Director of Mental Health also considers applications for ministerial long leave and
changes of legal status and provides advice to assist the Minister of Health’s decision in
these matters. The Director is assisted by the Deputy Director of Mental Health and a
small team of advisors.
Ministerial decisions about special and restricted patients
19.
A special/restricted patient’s responsible clinician is accountable for the patient’s clinical
management in the forensic service. However, applications for long leave and changes of
legal status require a decision by the Minister of Health (and/or the Attorney-General for
certain categories of legal status).
20.
As Minister of Health you will be asked to make these decisions about special/restricted
1982
patients subject to orders under section 24(2)(a) of the Criminal Procedure Act, who have
been found not guilty of an offence by reason of insanity or deemed unfit to stand trial.
Act
21.
This level of decision-making reflects the seriousness of special and restricted patients’
status and the need to ensure that a wide range of factors are considered when making
decisions about such patients.
Ministerial long leave
22.
Under the Mental Health Act and the Criminal Procedure Act, you are responsible for
Information
granting long leave and approving changes of legal status for certain special and
restricted patients.
23.
When a responsible clinician assesses a special patient as fit to be absent from hospital,
an application will be submitted to the Director of Mental Health for consideration of
Official
long leave. The application must be supported by the Forensic Director of Area Mental
Health Services (DAMHS). The DAMHS is responsible for the operation of the Mental
the
Health Act in a district health board (DHB).
24.
Long leave applications will typically follow a sustained period of successful short leaves
in the community granted by the Director of Mental Health, up to a maximum of six
under
nights per week.
25.
The application contains supporting documents such as:
a. clinical progress notes and any notable incidents
b. a risk assessment and management plan for the patient while on leave
Released
c. the proposed conditions of leave
d. a certificate, signed by two medical practitioners, stating that the patient is fit to be
allowed to be absent from hospital (section 50(1) of the Mental Health Act).
25.
The Director of Mental Health will review all information provided, giving careful
consideration to the rights and rehabilitation needs of the patient and the protection of
the public. This cautious approach enables both the service and the patient to develop a
clear understanding of the course of treatment and future goals and gives due
consideration to public safety.
Appendix 1
26.
You would then be provided with a report setting out the Director’s advice and
requesting your decision. The report summarises the relevant aspects of the special
patient’s rehabilitative progress, risk and management plan. A glossary of terms used in
these health reports is enclosed for your information.
27.
If you choose to grant a period of long leave, a leave of absence is attached to the
health report for you to sign, giving effect to your decision. The leave of absence
includes standard conditions of leave and conditions that may be particular to certain
patients.
28.
It is convention to grant long leave for an initial period of six months, followed by
subsequent periods of 12 months if the initial leave is successful. If you choose to not
approve a period of long leave, no further action is required. The Director of Mental
Health will write to the patient’s responsible clinician about the reasons for refusing an
application.
1982
Revoking ministerial long leave
29.
Act
Occasionally the Minister is asked to revoke long leave under section 50(3) of the Mental
Health Act. This may be necessary if the conditions of leave are breached or if there are
concerns about the safety of the special patient or the public
30.
A revocation of long leave requires urgent attention, and the Minister is required to sign
the revocation within 72 hours of the patient’s return to hospital.
31.
While revoking leave is disappointing in terms of the patient’s progress, timely leave
Information
revocation demonstrates that the system in place for long leave is effective in terms of
identifying and managing risks to the patient and others.
Changes of legal status
Official
32.
Special patients acquitted on account of insanity may be considered for a change of
legal status. When a responsible clinician assesses that a special patient no longer
the
requires special patient status, an application will be submitted to the Director of Mental
Health for consideration. Applications must be supported by the Forensic DAMHS.
33.
The Director of Mental Health reviews the application, giving careful consideration to the
progress of the special patient
under and the protection of the public. The Director will provide
you with a health report summarising the special patient’s progress over time, their
treatment and rehabilitation activities, as well as any significant adverse events and risk
considerations, and a recommendation about the special patient’s legal status for your
consideration.
34.
Under section 33(3) of the Criminal Procedure Act you are required to decide whether
Released
continued detention for a special patient is necessary to safeguard the patient’s own
interests and the safety of the public. You will be assisted in your decision by advice and
a recommendation from the Director of Mental Health as noted above.
35.
In deciding whether a special patient status is no longer necessary for the safety of the
public or a person, considerations of risk are central. The Director’s advice will include
information on the special patient’s risk to self and others as assessed by the responsible
clinician using clinical tools. The range of protections and mitigations put in place by the
mental health service and the patient themselves will also be taken into account.
Appendix 1
36.
Considerations of risk are complex and multifactorial, but some key factors include:
a. the stability of the special patient’s mental state and abstinence from substance use
b. the special patient’s understanding of their mental health and how it links to their
offending
c. their level of engagement in treatment and rehabilitation plans and activities, and an
understanding of how treatment reduces their risk of future harmful behaviour
d. other protective factors such as relationship with family and meaningful
engagement in community life (such as work, learning and cultural activities)
e. the length of time living in the community without incident or recurrence of
behaviour mirroring the original offence
f. evidence of a robust management plan for the patient, should they be granted a
change of status
1982
g. whether they can be adequately managed as a compulsory patient under the
Mental Health Act.
Act
37.
If you find that the special patient’s continued detention is no longer necessary to
safeguard the interests of the person or the public, you may direct that the individual be
held as a patient subject to a compulsory treatment order under the Mental Health Act,
or that they be discharged.
38.
The reports append a direction for you to sign, should you choose to grant a change of
status.
Information
Change of status for special patients found unfit to stand trial
39.
Occasionally you will be required to make decisions about the status of special patients
who have been found unfit to stand trial. Most de
Official cisions about the legal status of this
group of patients are made by the Attorney-General, as set out in section 31 of the
Criminal Procedure Act.
the
40.
However, on rare occasions you will be required to make decisions about such patients
in concurrence with the Attorney-General. Clinicians can request a change of legal status
from the Minister of Health if the patient remains unfit to stand trial, but special patient
under
status is no longer required. This is unlikely to happen more than once a year.
Mental Health Review Tribunal findings
41.
The Mental Health Review Tribunal (the Tribunal) is appointed by the Minister of Health
under the Mental Health Act. The principal role of the Tribunal is to consider whether a
Released
patient is fit to be released from compulsory status. The Tribunal comprises of one
lawyer, one psychiatrist and one community member, and a number of deputy members.
42.
Every person subject to a compulsory treatment order is required to have their condition
reviewed at least every six months. Should a patient disagree with their responsible
clinician’s decision that they are not fit to be released from compulsory status, the
patient can apply to the Tribunal for a review of his or her condition.
43.
Applications for a change of legal status can arise when the Tribunal issues a certificate
stating that in their opinion, it is no longer necessary for a person to be held as a special
patient.
Appendix 1
44.
Section 80(5)(a) of the Mental Health Act requires the Tribunal to consider whether “the
patient’s condition still requires, either in the patient’s own interest or for the safety of
the public, that he or she should be subject to the order of detention as a special
patient.”
45.
The Tribunal describes the threshold for “requires” as high and falling between expedient
and desirable on one hand and essential on the other. The Tribunal will consider the
patient’s interest, the safety of the public and immediate and longer-term factors,
including what may happen if the patient is not a special patient.
46.
The Director of Mental Health will seek advice from the forensic mental health service on
their view of the patient’s condition and clarification of any aspects of the Tribunal’s
decision. The process for seeking a ministerial decision on a Tribunal finding is the same
as described in paragraphs 33 to 38.
Restricted patient leave and change of status
1982
47.
In relation to restricted patients, as the Minister of Health, you are also required to make
decisions about restricted patients’ detention where the:
Act
a. responsible clinician has applied for long leave
b. responsible clinician or Tribunal has found that a restricted patient remains mentally
disordered, but that it is not necessary for them to remain subject to restricted
patient status.
48.
Restricted patient long leave is handled the same way as special patients (see
Information
paragraphs 22 to 31). Change of legal status recommendations for restricted patients
must be agreed upon by you in concurrence with the Attorney-General.
Victims of special patients
Official
49.
Decisions around special patients are required to made within the current legislative
provisions; however, the notification and engagement with registered victims of special
the
patients has been problematic for the victims and the services and has led to adverse
media coverage on occasions.
50.
These challenges are due to how the legislation around victims’ rights is drafted and the
under
expectations and responsibilities for services arising from the Privacy Act, in particular
the Health Privacy Code with respect to the protection of the privacy of special patients.
51.
The Ministry is able to brief you separately on this issue and possible mechanisms to
address this.
Next steps
Released
52.
Dr John Crawshaw, Director of Mental Health and Addiction Services, is available to
assist you in making these decisions and to brief you further at your convenience.
Appendix 1
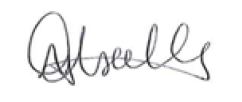
Figure 1: Special patient pathways
Special Patient found not guilty
Special Patient found unfit
Special Patient
by reason of insanity
to stand trial
transferred from Prison
s24(2)(a) CP(MIP) Act
s24(2)(a) CP(MIP) Act
s45 or s46 MHA
1982
Compulsory mental
Right to be treated as an
health treatment
ordinary patient subject to
Right to be treated as
cannot take place in
Mental Health Act (s44 MHA)
an ordinary patient
prison (s36 MHA)
Act
Detained in the hospital
until half maximum tariff
for most serious charge
Detained in a secure
If prisoner thought to be
Right to be treated in least
hospital
restrictive environment
mentally disordered, the prison
superintendent may apply for
MHA assessment
The special patient is carefully reintegrated back
into the community as their condition improves
Director can approve
leave up to six nights in
the community
Short Leave
Director can approve
(s52 MHA)
Information
leave up to six nights in
Clinical review at
DAMHS for
By Prisoner
the community
least every six
assessment
consent (s46
Short Leave
months
(s45 MHA)
MHA)
(s52 MHA)
Clinical review at
least every six
months
Ministerial Long Leave not available
Can approve leave
up to six nights in
the community
Official
Minister of Health can approve leave
Short Leave
for longer than six days on receipt of a
Joint ministerial decision with
Change of Legal
Certificate
(s52 MHA)
A-G if SP status considered
Ministerial Long Leave
medical certificate
received stating
Status
no longer necessary
Clinical review at
(s50 MHA)
no longer unfit
least every six
the
months
This leave can be revoked by
Minister (s51 MHA)
Attorney-General decision if
Ministerial Long Leave not available
no longer unfit
Certificate received indicating
under
Special patient status no
Change of Legal
longer necessary
Director of Mental Health
Status
can transfer Prisoner
Change to ordinary
Return to court
back to prison by
to face charges
MHA patient
DAMHS request
Minister of Health must
consider a change of legal
status to ordinary patient or
discharge
Released
Appendix 1
Glossary of terms used in special patient health reports
Criminal Procedure (Mentally Impaired Persons) Act 2003 (the Criminal Procedure Act)
The Criminal Procedure Act was the first significant revision of the law relating to mentally
impaired offenders in 50 years.
A defendant who is charged with an imprisonable offence and is suspected of being mentally
impaired can be assessed under the Criminal Procedure Act. At the conclusion of such an
assessment, the Court may find a defendant unfit to stand trial or acquit a defendant on account
of insanity.
The Criminal Procedure Act prescribes orders that the Court can make for the detention,
treatment and care of a defendant found unfit to stand trial or acquitted on account of insanity,
and for certain mentally impaired defendants who are convicted of an imprisonable offence.
1982
Director of Mental Health
The Director and Deputy Director of Mental Health have certain powers under the M
Act ental Health Act
in relation to special patients, including:
• the administration of matters relating to ‘special patients’, including approval of leave and
transfer
• the ability to apply to the Court for a ‘restricted patient’ order
• the ability to direct that patients be transferred between services
• the ability to instruct a district inspector to inquire into issues relating to the assessment and
Information
treatment of patients and proposed patients under the Mental Health Act
• the authority to inspect any aspect of a mental health service.
Directors of Area Mental Health Services (DAMHS)
Official
DAMHS are appointed to each DHB, as well as to the five regional forensic mental health services, by
the Director-General of Health. The forensic D
the AMHS have responsibilities in relation to special and
restricted patients, including:
• appointing health professionals to be responsible clinicians for each patient undergoing
compulsory assessment and treatment
under
• applying to the Director of Mental Health for the leave and transfer of ‘special patients’
• receiving applications for the compulsory assessment of a person detained in a penal institution
• deciding whether certain ‘special patients’ are fit to be returned to a penal institution
• directing the temporary return of certain ‘special patients’ to hospital
• receiving clinical reviews and Tribunal reviews of patients and special patients subject to a
compulsory treatment or
Released der.
District inspectors
District inspectors are lawyers appointed by the Minister of Health, with responsibilities to:
• make regular visits to hospitals and other services in the district of appointment
• conduct inquiries into any breach of legislation or breach of duty by persons employed in the
hospital or service
• monitor patients’ rights and investigate any complaints of breaches
Appendix 1
• ascertain views and wishes of patients during their course of treatment and assist where
appropriate with applications for review by a Judge or Tribunal
• prepare visitation reports for the DAMHS
• provide regular reports to DAMHS on the exercise of the district inspector’s responsibilities and
monthly reports to the Director of Mental Health.
Forensic mental health services
Regional forensic mental health services are responsible for the management of special patients and
restricted patients, within the legislative framework of the Mental Health Act and the Criminal
Procedure Act.
New Zealand legislation specifically allows for people who have been charged with or convicted of
an offence and who meet the definition of mental disorder in the Mental Health Act to be treated in
hospital for that illness. Treating the mental disorder is an important step in assisting an individual
to acknowledge and address the reasons for their offending and in doing so, can reduce the chances
1982
of future offending and significantly improve their wellbeing.
In managing special patients, forensic services are required to balance the treatment
Act and
rehabilitative needs of the individual with the safety of the public and the concerns of victims.
Index offence
The criminal offence that led to charges of which the special patient was found not guilty by reason
of insanity.
Information
Medical certificate
A certificate pursuant to section 50(1) of the Mental Health Act signed by two medical practitioners
stating that they have examined a special patient and found that they are fit to be absent from
hospital.
Official
Mental Health (Compulsory Assessment and Treatment) Act 1992 (the Mental Health Act)
the
The Mental Health Act provides the framework for the management of special patients, including
provisions for leave and transfer. The main sections of the Mental Health Act relating to the
management of special and restricted patients are:
under
• granting of ministerial long leave (section 50)
• granting of short leave by the Director of Mental Health (section 52)
• approving the transfer of special patients between facilities (section 49)
• enabling the transfer of prisoners into a forensic mental health facility for treatment (sections 45
and 46) Released
• approving the return of certain special patients to prison (section 47)
• enabling the Court to declare a patient to be a restricted patient (sections 54 to 56).
The key objectives of the Mental Health Act are to:
• define the circumstances in which compulsory assessment and treatment may occur
• ensure that both vulnerable individuals and the public are protected from harm
• identify the rights of patients and proposed patients and ensure those rights are protected
• ensure that assessment and treatment occur in the least restrictive manner consistent with safety
• provide a legal framework consistent with good clinical practice
• promote accountability for actions taken under the Mental Health Act.
Appendix 1
A ‘
patient’ under the Mental Health Act, means a person who is:
• required to undergo assessment under section 11 or section 13 of the Mental Health Act; or
• subject to a compulsory treatment order made under Part 2 of the Mental Health Act; or
• a special patient.
Mental Health Review Tribunal
The Minister of Health appoints members of the Tribunal pursuant to section 101 of the Mental
Health Act. One member must be a lawyer, one a psychiatrist, and the other a community member.
Key functions of the Tribunal in relation to special and restricted patients are:
• reviewing the condition of special patients found not guilty by reason of insanity, and reaching
an opinion as to whether “the patient’s condition still requires, either in the patient’s own
interest or for the safety of the public, that he or she should be subject to the order of detention
as a special patient” (section 80)
1982
• reviewing the condition of special patients found not unfit to stand trial, and reaching an opinion
as to whether they are no longer unfit to stand trial, and if so, whether they still require special
Act
patient status (section 80)
• reviewing the condition of patients who are subject to ‘restricted patient’ orders and reaching an
opinion as to whether the patient is fit to be released from restricted patient status (section 81)
• investigating complaints, including in relation to special and restricted patients (section 75).
Mental state
In clinical psychology and psychiatry, an indication of a person's mental health, as
Information determined by a
mental status examination.
Psychosis
Official
Psychosis occurs when a person loses contact with reality. The person may:
• have false beliefs about what is taking place, or who one is (delusions)
the
• see or hear things that are not there (hallucinations).
Responsible clinicians under
Key responsibilities of responsible clinicians include:
• determining whether or not a person is mentally disordered
• making applications to the Court for compulsory treatment orders (CTOs)
• overall management of the patient’s treatment
• regular clinical reviews of persons subject to CTOs and of ‘special patients’ and ‘restricted
patients’
Released
• ensuring consultation with the family or whānau of the patient or proposed patient unless there
are reasonable grounds not to do so.
Restricted patients
‘Restricted patients’ are compulsory mental health patients that present special difficulties because
of the danger they pose to themselves and others. The Court makes decisions about restricted
patient status based on an application from the Director of Mental Health under the Mental Health
Act. Restricted patient status is rare, with only eight people given this status since 1992. Restricted
patients have the same access to leave and change of legal status as special patients.
Appendix 1
Revoking ministerial long leave
Section 51 of the Mental Health Act permits the forensic DAMHS to direct that a patient on long
leave be admitted or readmitted to hospital if it is necessary ‘in the interests of the safety of that
patient or the public’.
Such an admission can only be for 72 hours, during which time the Director of Mental Health will
provide a health report to the Minister of Health seeking revocation of leave.
Special patients
‘Special patient’ is a legal status received when the Court orders that a defendant be detained in a
forensic mental health facility for treatment. Defendants can be made a special patient when they
meet certain criteria in terms of a mental disorder.
The main categories of special patients are:
1982
• unfit to stand trial because of a mental disorder
• found not guilty by reason of insanity (as defined in the Crimes Act 1961)
•
Act
found guilty but the Court orders compulsory mental health treatment instead of, or as well as, a
prison sentence.
Another category of special patient is where people in prison (sentenced or on remand) are
transferred under the Mental Health Act to a forensic mental health facility for treatment. The
person is transferred back to the Corrections facility when their responsible clinician considers their
mental health can be adequately managed in prison.
Information
When a person is made a special patient after being found not guilty by reason of insanity, the order
is for an indefinite period. A person found unfit to stand trial may be detained subject to a special
patient order for up to half of the maximum sentence to which they would otherwise be subject, to a
maximum of 10 years, or until the person becomes fit to stand trial.
Official
Special Patient Review Panel (SPRP)
the
Each forensic mental health service conducts regular SPRPs to review the clinical progress of special
patients. The Panels are made up of representatives from a multi-disciplinary team that works with
the special patient (e.g. psychiatrists, nurses, social workers), and may have a member external to the
service.
under
The special patient appears before the panel with support people (such as family and whānau) for a
discussion about their progress in the preceding period. The SPRP will then make comments and
recommendations for the patient’s treatment and management plan, including recommendations
about leave and change of status.
The SPRP s recommendations serve as a second multi-disciplinary team opinion for ministerial leave
Released
or change of legal status decisions and are referenced in the health reports to the Minister of Health.
Treating team
The treating team is a multi-disciplinary team that works with the special patient. Treating teams
may include psychiatrists, nurses, social workers, cultural support workers, kaumātua, addiction
practitioners, and peer support workers.
1982
Act
Information
Official
the
under
Released
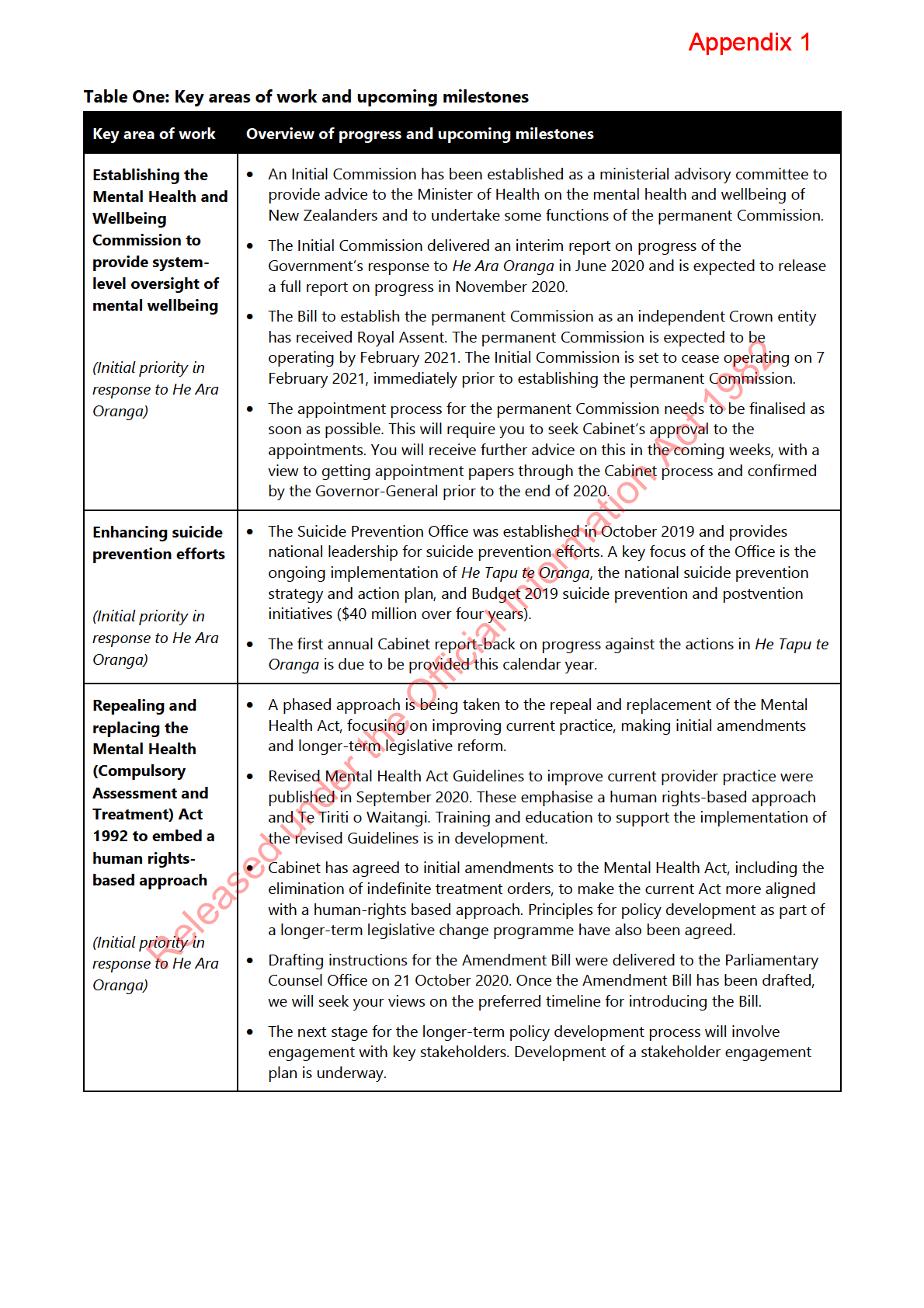
 Appendix Six: Indicative milestones through to 2023/24
Appendix Six: Indicative milestones through to 2023/24
Appendix 1
2020
2021
2021/22
2022/23
2023/24
2020/21 Q2
2020/21 Q3
2020/21 Q4
▪ Commence de ivery of expanded Māori services
▪ Commence phased delivery of new Māori services
▪ Integrated Primary Mental Hea th and Addiction Services
s
being delivered in over 100 general practice sites in 15 DHB
▪ Commence phased de ivery of expanded and new youth
▪ Commence phased delivery of new Pacific services
areas, providing coverage for around 1.5 mil ion people
services
Expanding
▪ Commence procurement for next tranche of youth services
▪ Commence delivery of new B20 services for tertiary students
Access and
▪ Commence procurement of new B20 services for tertiary
Choice
students
)
1982
▪ Commence estab ishment of Waikato Alcohol and Other
▪ Commence procurement processes for Waikato AOD
▪ New refined drug testing regime for Auckland AOD
▪
s
Drug (AOD) Treatment Court
treatment court
Treatment Court starts
▪ Sites identified for additional B19 primary AOD services
▪ Procurement of additional B19 primary AOD services
▪ Waikato AOD Treatment Court starts
underway
Addiction
▪ Contracts in place for additional B19 primary AOD services
Act
▪ Commence services of two additional Pregnancy and
)
Parenting Services sites (Whanganui and Eastern Bay of
Plenty)
▪ Report-back to Cabinet on progress implementing
He Tapu
▪ Additional LifeKeepers suicide prevention training
▪ Development of updated media guidelines and engagement
▪
s
te Oranga, the suicide prevention strategy (TBC pending
workshops and e-learning modules commence
with media completed
Ministerial decisions)
▪ Commence phased delivery of face-to-face bereavement
(
▪ First round of B19 Māori and Pacific Suicide Prevention
response service (note: national on ine services commenced
Suicide
Community Fund projects underway
in May 2020)
Prevention
▪ One year anniversary of Suicide Prevention Office
▪
s 9(2)(f)(iv)
s 9(2)(f)(iv)
Information
▪ Finalise updated
Kia Kaha, Kia Māia, Kia Ora Aotearoa:
▪
▪
s
COVID-19 Psychosocial and Mental Wel being Recovery Plan
s 9(2)(f)(iv)
s 9(2) f)(iv)
Psychosocial
(the Psychosocial Plan) to reflect stakeholder feedback
plan &
(
▪ Release updated Psychosocial Plan (TBC)
longer-term
pathway
Official
▪ Provide drafting instructions for initial amendments to
▪ Introduce initial amendment Bil (TBC pending Ministerial
▪ First reading and Select Committee consideration of initial
▪
▪
▪
Par iamentary Counsel Office (PCO)
decisions)
amendment Bil (TBC)
s 9(2)(f)(iv)
s 9(2)(f)(iv)
s 9(2)(f)(iv)
the
▪ Commence targeted stakeholder engagement to inform
Mental
policy development for repeal and replacement of the Act
Health Act
under
▪ Initial Commission delivers report on Government progress
▪ Permanent M ntal Hea th & Wel being Commission
▪ Monitoring and oversight of mental wel being activities
s
responding to
He Ara Oranga
established
Mental
Health and
▪ Finalise appointment process for permanent Mental Hea th
▪ Initial Commission term ends
(
& Wel being Commission (TBC pending Ministerial
Wellbeing
decisions)
2
Commission
▪ Commence procurement of additional B19 digital supports
▪ Commence service de ivery of Wel Child Tamariki Ora
▪ Commence delivery of additional B19 digital supports
s
Enhanced Support Pilots in Counties Manukau
▪ Commence service de ivery of B19 Wel Child Tamariki Ora
s
s 9(2)(f)(iv)
Released
Enhanced Support Pilot in Lakes
(
▪ Commence service delivery of pilot to improve transitions
Other
from acute mental hea th inpatient units (part of
priority MHA
Homelessness Action Plan)
)
initiatives
▪
s 9(2)(f)(iv)
Note: This is an indicative overview of potential activities to implement priority areas of the Government’s response to He A ra Oranga and the confirmed investment in mental health and addiction. Some activities are unconfirmed and subject to future Ministerial or Cabinet decisions. This is not intended to pre-empt or advise on those decisions.
Document Outline