Guideline
Deliberate Self Harm (DSH), Management of Patients presenting after an act of
Guideline Responsibilities and Authorisation
Department Responsible for Guideline
Guideline
Deliberate Self Harm (DSH), Management of Patients presenting after an act of
Guideline Responsibilities and Authorisation
Department Responsible for Guideline
Emergency Medicine – Administration
Document Facilitator Title
Emergency Physician
Document Facilitator Name
Tonia Nicholson & Anna Nienaber
Document Owner Title
Clinical Director
Document Owner Name
Ian Martin
Target Audience
Emergency Department Staff
Disclaimer: This document has been developed by Waikato District Health Board specifically for its
own use. Use of this document and any reliance on the information contained therein by any third party
is at their own risk and Waikato District Health Board assumes no responsibility whatsoever.
Guideline Review History
Version
Updated by
Date Updated
Summary of Changes
05
Victoria McLean
17/10/2017
Formatted into new template. Review and update of
and Anna
previous version
Nienaber
Doc ID:
3983
Version:
05
Issue Date:
19 JAN 2018
Review Date: 19 JAN 2021
Facilitator Title:
Emergency Physician
Department:
Emergency Medicine - Administration
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE DAY OF PRINTING
Page 1 of 4
 Guideline
Deliberate Self Harm (DSH), Management of Patients presenting after an act of
1. Purpose
Guideline
Deliberate Self Harm (DSH), Management of Patients presenting after an act of
1. Purpose
• To ensure safe observation, treatment and disposition from ED, of patients who have
attempted DSH.
• For people presenting at risk of suicide, the responsibilities of emergency staff are to:
o triage and plan for their safety
o diagnose and treat any concurrent non-psychiatric illness or injury
o perform a suicide risk assessment for all people who have suicidal thoughts or have
self-harmed, when they are deemed ready to interview
o assess for the presence of red flags for short-term risk
o identify those who require an immediate comprehensive mental health specialist
assessment within the emergency department
o identify those who can safely be discharged with a comprehensive mental health
assessment follow-up within 72 hours and who have good support systems
o identify those very-low-risk people with good support systems who can be safely
discharged to the community and referred to primary care management
o Engage with families to inform and support them.
2. Definitions
• People who present following an act of deliberate self harm (DSH) +/ or attempted suicide
are often in a state of extreme distress.
• The Ministry of Health has issued guidelines on how to assess and triage such patients.
These guidelines should be followed in Waikato
ED.
https://www.health.govt.nz/publication/preventing-suicide-guidance-
emergency-departments
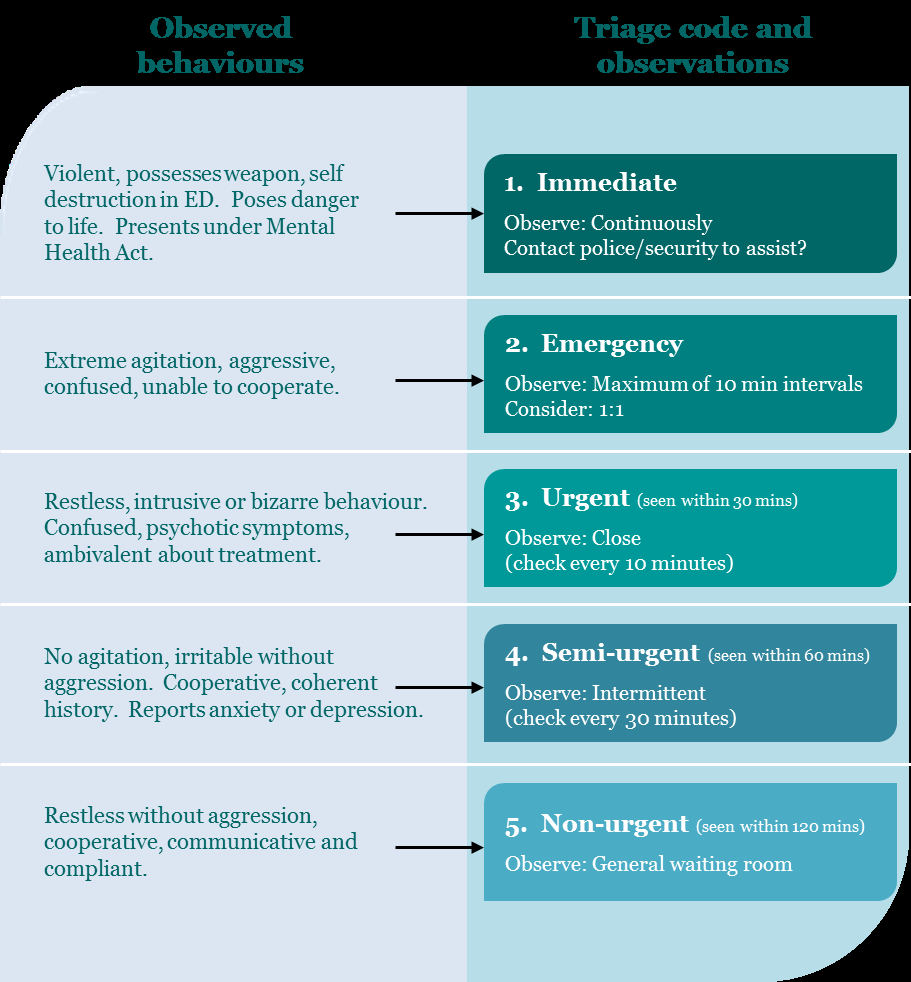
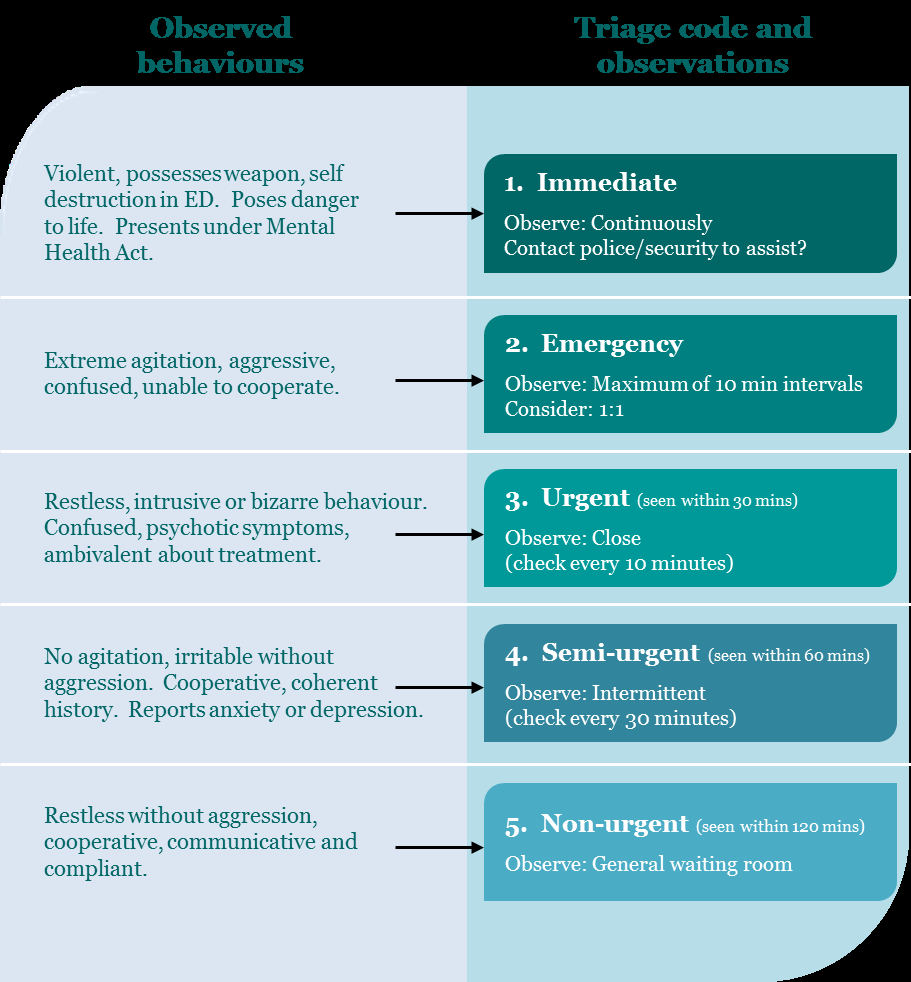
3. Triage
• Those patients who are assigned a mental triage score of 1, 2 or 3 will require 1 on 1
observation. Triage score 4 only need intermittent observation. Once it has been decided
that observation is necessary, the nurse in charge (NIC) should be notified. They will:
o Arrange an appropriate cubicle for the patient to go to
o Arrange an appropriate “patient watch” e.g. family member, carer, ED attendant,
hospital aid or security guard.
o Arrange with duty manager a “watch”
o Notify the ED consultant in charge of the shift
Doc ID:
3983
Version:
05
Issue Date:
19 JAN 2018
Review Date: 19 JAN 2021
Facilitator Title:
Emergency Physician
Department:
Emergency Medicine - Administration
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE DAY OF PRINTING
Page 2 of 4

 Guideline
Deliberate Self Harm (DSH), Management of Patients presenting after an act of
Guideline
Deliberate Self Harm (DSH), Management of Patients presenting after an act of
• Adapted version of the Australian Mental Health Triage Scale (AMHTS) as used
in
https://www.health.govt.nz/publication/preventing-suicide-guidance-emergency-
departments
4. Risk assessment
• The “
Mental Health Patients Risk Assessment Pathway” is available in triage and the
document bookshelf by the main desk. This allows a quick risk assessment of the patient
and stays in the patients notes.
5. Medical management
• Overdose, injuries and medical conditions should be dealt with appropriately
• Anxious, aggressive and uncooperative patients refer to t
he Violent Patients: Management
of Potentially guideline.
Doc ID:
3983
Version:
05
Issue Date:
19 JAN 2018
Review Date: 19 JAN 2021
Facilitator Title:
Emergency Physician
Department:
Emergency Medicine - Administration
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE DAY OF PRINTING
Page 3 of 4
 Guideline
Deliberate Self Harm (DSH), Management of Patients presenting after an act of
6. Mental health referral and Medical clearance/interviewable
Guideline
Deliberate Self Harm (DSH), Management of Patients presenting after an act of
6. Mental health referral and Medical clearance/interviewable
• Every patient who presents with DSH should generally be referred for psychiatric
assessment. Consult Liaison Psychiatry services are the service used during normal
business hours. The Crisis Team assess psychiatric patients during the evening and on
weekend and public holiday days. The on-call psychiatric registrar assesses psychiatric
patients overnight.
• Psych liaison, CAT team or the on call psychiatric registrar should be contacted – either by
the doctor responsible for the patient or the NIC, to let them know of the presence of the
patient in the department. The referral may be done by yourself or via the primary nurse or
nurse in charge
• Electronic referrals are made to Consult Liaison after you have spoken to them. This is
done via the clinical workstation on the patients’ health views. Steps are; MH forms, MH
referrals, click new and fill in required fields.
• The Crisis team can be contacted via the Operator and the on-call psychiatric registrar
through the Henry Bennet Coordinator via the Operator.
• These teams usually request a “medical clearance”. The intention is that the patient can be
interviewed and that acute medical problems, overdose or injuries has been attended to.
Psychiatric assessment should not wait for medical clearance if the person is interviewable.
Inform the appropriate mental health service as soon as the patient is interviewable even if
still need ongoing medical care but is awake and not sedated or intoxicated.
7. Disposition
• Some patients will be admitted by the mental health team to HBC
• After the mental health team has seen the patient and want to discharge them from ED an
ED discharge letter should be done.
• Very occasionally, patients may be discharged after a period of observation without
psychiatric assessment in the ED if the treating EM doctor feels that the person is at very
low risk of further self-harm in the near future. This should ideally be done in consultation
with mental health services to organise ongoing follow outpatient follow up
Doc ID:
3983
Version:
05
Issue Date:
19 JAN 2018
Review Date: 19 JAN 2021
Facilitator Title:
Emergency Physician
Department:
Emergency Medicine - Administration
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE DAY OF PRINTING
Page 4 of 4