Private Bag 911, Timaru
New Zealand
Telephone 03 687 2100
Facsimile 03 688 0238
23 December 2021
Andrew McGregor
By email:
[email address]; fyi-request-17708-
[email address]; [FYI request #17709 email]; fyi-request-17710-
[email address];
Dear Andrew,
Re:
Official Information Act Request
I refer to your Official Information Act request received on 8th December 2021 in which you
specifically requested the fol owing:
1. Please provide Guidelines/Procedures for the management of postoperative Urinary
Retention (POUR).
SCDHB’s response: Please refer to appendix A as attached.
2. Please provide Guidelines/procedures for the management/prevention of persistent
Postsurgical Pain.
SCDHB’s response: Please refer to appendix B & C as attached.
3. Please provide Guidelines/procedures in the treatment of patients after a suicide
attempt and/or suicidal ideation.
SCDHB’s response: Please refer to appendix D as attached.
4. Please provide Guidelines/procedures differentiating subtypes of primary (idiopathic)
constipation.
SCDHB’s response: South Canterbury DHB does not have guidelines/procedures
differentiating subtypes of primary (idiopathic) constipation; therefore, we decline your
request under section 18(g) of the OIA because the information is not held.
You have the right to seek an investigation and review of our decision by the Ombudsman. The
Ombudsman's Office can be contacted on 0800 802 602 or on-line at
http://www.ombudsman.parliament.nz/
If you wish to discuss this decision with us, please feel free to get in touch.
Kind regards
Sophie Lyons
SLT Administrator
South Canterbury DHB
 Appendix A
Appendix A:
UROLOGY SERVICES
PROTOCOL
Urinary Retention
Introduction:
Patients requiring catheterisation do not always require urological follow-up.
Urinary retention associated with renal failure can lead to a post-obstructive diuresis, a potentially
life-threatening scenario.
1.
Initial diagnosis of urinary retention
1.1 Confirm diagnosis (palpation of distended bladder or bladder scan).
1.2 Collect blood for creatinine.
2.
Management of urinary retention
2.1 If retention has been preceded by gross haematuria, manage as per SCDHB Urology
Protocol Number 2: Haematuria Management.
2.2 Place 16 G Fr urethral catheter.
2.3 Allow bladder to empty and record volume drained.
2.4 Send urine for microscopy, culture and sensitivities.
2.5 If creatinine is less than 200, discharge (see below).
2.6 If creatinine is >200, observe patient for two hours:
2.6.1 if urine output, after initial drainage, is > 200 mL per hour, commence treatment
for post-obstructive diuresis – see 3 below
2.6.2 if urine output, after initial drainage, is < 200 mL per hour, encourage oral fluid
intake, discharge patient and arrange repeat creatinine in 2 to 3 days with GP
3.
Management of post-obstructive diuresis
3.1 Prescribe intravenous fluid replacement at a rate of 50% of urine output per hour.
3.2 Urine needs hourly measurement and the iv fluid rate adjusted accordingly by nursing
staff.
3.3 Use alternate one litre bags of Normal Saline and Dextrose 4% Saline.
3.4 The patient will require admission to hospital.
4.
Admission
4.1 Patients in urinary retention can usually be discharged, unless they develop a post-
obstructive diuresis.
4.2 Discussions around acute management and admission are to be discussed with the on
call Urologist in Christchurch.
4.3 Patient to be admitted under the On Call SCDHB General Surgeon.
4.4 If patient haemodynamically unstable, consider ICU involvement.
4.5 On week days Urology Nurse to be notified of admission, and in weekend, the on call
house surgeon.
4.6 On the week days Urology Nurse (and in weekends the house surgeon) to discuss patient
with the Christchurch on call Urologist, after daily ward round.
5.
Discharging a patient who is catheterised
5.1 Supply patient with night bag and give catheter education.
5.2 Prescribe doxazosin 4 mg daily for male patients if they are likely to tolerate this and are
not currently on any therapy for benign prostatic hyperplasia.
5.3 Complete District Nursing referral: a District Nurse should attend the next day.
5.4 Refer to Urology Nurse for outpatient review: a decision will be made and the patient
contacted regarding a trial of void if that is thought appropriate.
AUTHOR: Urology Nurse
FILE NUMBER: UP7
AUTHORISED: Feb 2021
REVIEW DUE: Feb 2023
This is a controlled document. The electronic version is the most up-to-date. Printed versions are valid on the day of printing only.
Page
1 of
2
 UROLOGY SERVICES
PROTOCOL
Protocol:
UROLOGY SERVICES
PROTOCOL
Protocol:
1.
Initial diagnosis and management as per 1 and 2 above.
2.
The vast majority of patients will be discharged home.
3.
Complete referrals and prescribe doxazosin as outlined in 5 above.
4.
Patients who develop a post-obstructive diuresis will need admission and discussion with the on
call Urologist in Christchurch, or if it has not been possible to place a catheter.
TERTIARY REFERRAL TO CDHB:
No improvement after 3 days should prompt tertiary referral to the CDHB. This should be done through
the Christchurch Urologist on-call.
AUTHOR: Urology Nurse
FILE NUMBER: UP7
AUTHORISED: Feb 2021
REVIEW DUE: Feb 2023
This is a controlled document. The electronic version is the most up-to-date. Printed versions are valid on the day of printing only.
Page
2 of
2
 Appendix B:
Patient Label
ACUTE PAIN SERVICE REFERRAL FORM
Appendix B:
Patient Label
ACUTE PAIN SERVICE REFERRAL FORM
Email and scan referral t
o [email address]
File form in ward referal clear file
Referral Date:
Patient Location:
Referrer:
Ward
Name Designation Contact Number
Room Number
Admission Date:
Planned Discharge Date:
Indication for Referral
□ Pain not responding to standard treatment ** □ Caesarean Section (day one)
□ Uncontrolled Nausea / Vomitting **
□ In-situ Intervention (eg PCA, Pain Buster, T34)
□ Complex Pain Past History
□ Other _____________________________________
□ Trauma _____________________________
** Call Acute Pain CNS and complete Referral Form
_____________________________
□
After hours: House Officer to contact Duty Anaesthetist
Surgery ______________________________
______________________________
Current Interventions - tick all which apply
Co-morbidities
□ PO /IV Analgesia - charted and given?
Y / N
□ IHD / Cardiac Failure
□ History of PONV
□ PCA
□ Intrathecal
□ Respiratory Issue
□ Gastric Ulcer
□ Epidural
□ Regional Infusion
□ Renal Impairment
□ Chronic Pain
□ On-Q Pain Buster □ Local Anaesthetic
□ Liver Impairment
□ Anxiety
□ Opioid infusion
□ Ketamine infusion
□ Diabetes
□ Substance Abuse
□ IV Sedation
□ T34 Niki Pump
□ Other _____________
1. Patients with invasive pain adjuncts or complex analgesic medication needs will be seen daily
2. Please ensure charted analgesia has been given prior to submitting Acute Pain Service Referral
3. Please ensure Antiemetics, Break through analgesia and Constipation medications are charted
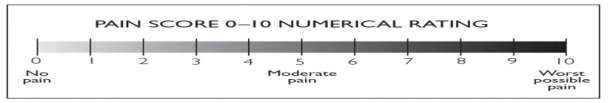
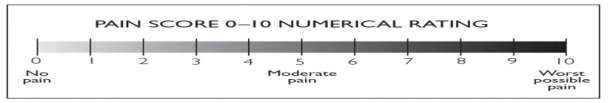
Pain Score 1-10: ______ rest:
_____ activity
Function Activity Score:
A □ B □ C □
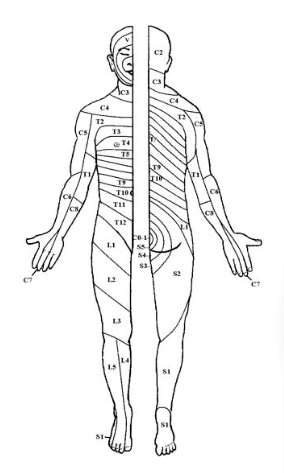
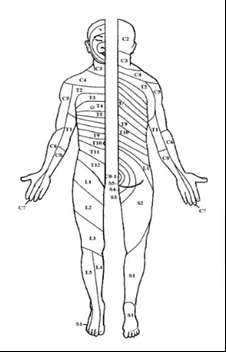
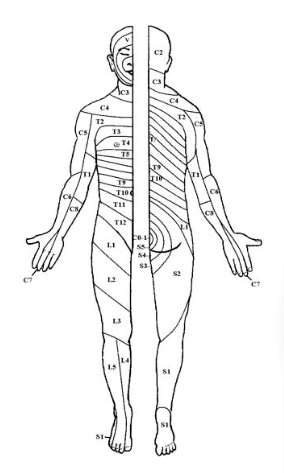
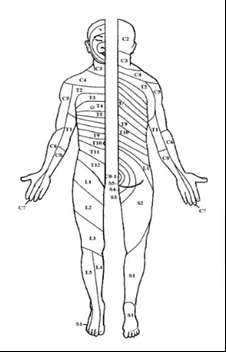
Dermatome Level:
Bromage Scale: 0 □ 1 □ 2 □ 3 □
Sedation Score:
OFFICE ONLY Date Received:
First Seen:
CNS
ACUTE PAIN SERVICE REFERRAL PATHWAY
Bromage Score
AUTHOR:
CNS Acute Pain Nurse
FILE NUMBER:
APR1
AUTHORISED:
June 2021
REVIEW DUE:
June 2023
This is a controlled document. The electronic version is the most up-to-date. Printed versions are valid on the day of printing only.
Page
1 of
2


 UNCONTROLLED PAIN
Contact
UNCONTROLLED PAIN
Contact Acute Pain CNS by
mobile phone
(See Anaesthetist roster)
Clinical hours
Morning hours: 830-1130
Afternoon hours: 1300-1530
After hours: House Officer to contact Duty Anaesthetist
Complete referral and email to [email address]
POSTOPERATIVE - DAY ONE
TRAUMA
Dermatome Map
YES
NO
COMPLETE REFERRAL FORM
COMPLETE REFERRAL FORM
PATIENT WILL BE REVIEWED
PATIENT WILL BE REVIEWED
AM WARD ROUND
PM WARD ROUND
IMPORTANT POINTS TO CONSIDER
Has the patient had regular analgesia?
Has the patient had PRN analgesia?
Is bowel function documented?
Have laxatives been charted?
Function Activity Score
PALLIATIVE RESOURCES
A = no limitation of activity due to pain
IHUB
Knowledge Base
Palliative Care
Please refer to Palliative Care Team
B = mild limitation of acticity due to pain
03 6872421 or after hours Palliative SMO
C = unable to compelte activity due to pain
AUTHOR:
CNS Acute Pain Nurse
FILE NUMBER:
APR1
AUTHORISED:
June 2021
REVIEW DUE:
June 2023
This is a controlled document. The electronic version is the most up-to-date. Printed versions are valid on the day of printing only.
Page
2 of
2
 Appendix C:
CLINICAL SERVICE PRACTICE MANUAL
GUIDELINES
Minimum Observations Guide- Acute Pain Patients
Post-Operative Observations- if stable
Pulse, BP, Resp rate, SPO2 &
Pain Score, Nausea, and Sedation
Temperature
score
First 4 hours once returned to the ward
Appendix C:
CLINICAL SERVICE PRACTICE MANUAL
GUIDELINES
Minimum Observations Guide- Acute Pain Patients
Post-Operative Observations- if stable
Pulse, BP, Resp rate, SPO2 &
Pain Score, Nausea, and Sedation
Temperature
score
First 4 hours once returned to the ward
On arrival, then 30min for 2hrs,
On arrival, then 30min for 2hrs,
from PACU
hourly for 2hrs
hourly for 2 hrs if stable
If stable after first 4 hours
2 Hourly
2 Hourly
If stable after first 8 hours
4 Hourly
4 Hourly
Patient Controlled Analgesia (PCA)-if stable
Pulse, BP, Resp. rate, Pain Score, Nausea,
Insert Site & Infusion pump check
SPO2, Temperature and Sedation score
First 12 hours since
Commencement of
Commencement of
Insertion site 4 hourly
commencement
infusion,
infusion,
of infusion
Then 1 hourly
Then1 hourly
Programme check every shift change
If Stable after first 12 hours 4 Hourly
4 Hourly
Insertion site checked minimum
since commencement of
4 hourly
infusion
Programme check every shift change
After Clinician Bolus
Every 5 minutes
Every 5 minutes for 15 Insertion site and Programme check
injection
for 15 minutes
minutes
after bolus
Epidural Analgesia- If Analgesia is inadequate, motor block is excessive or patient is hypotensive then
identify sensory block and degree of motor block.
Pulse, BP, Resp. Pain Score, Nausea, Level of
Degree of
Insert Site & Infusion pump
rate, SPO2,
and Sedation score Sensory
motor block check
Temperature
block
Inpatient first Every 15 mins for Every 15 mins for 2
4 hourly
4 hourly
Insertion site checked minimum
6 hours
2 Hours
Hours
4 hourly
Every 30 mins
Every 30 mins
for 4 hours
for 4 hours
Programme check every shift
change
If stable after Hourly for
Hourly for 4 hours
4 hourly
4 hourly
Programme check every shift
6 hours
4 hours
change
(if remains stable)
(if remains stable)
4 hourly
4 hourly
Starting
Every 5 minutes Every 5 minutes for
Before bolus Before bolus Programme check
infusion or
for 20 minutes
20 minutes
30 minutes
30 minutes
after bolus
After Bolus
and 1 hour
and 1 hour
injection
after
after
AUTHOR:
CNS Acute Pain
FILE NUMBER:
CSPM A12
AUTHORISED:
Nov 2020
REVIEW DUE:
Nov 2024
This is a controlled document. The electronic version is the most up-to-date. Printed versions are valid on the day of printing only.
Page
1 of
2

 CLINICAL SERVICE PRACTICE MANUAL
GUIDELINES
Intrathecal/Epidural Morphine for Acute Pain Management
Temperature
Pulse, BP, Resp. rate, Pain Score, Nausea, and
Height of
SPO2
Sedation score
Sensory block
Inpatient first
CLINICAL SERVICE PRACTICE MANUAL
GUIDELINES
Intrathecal/Epidural Morphine for Acute Pain Management
Temperature
Pulse, BP, Resp. rate, Pain Score, Nausea, and
Height of
SPO2
Sedation score
Sensory block
Inpatient first
2 Hourly
2 Hourly
2 Hourly
2 Hourly
24 Hours
Bromage Score (motor test)
Dermatome Map (sensory test)
Sedation Score
0
No sedation/ alert
1
Mild, occasionally drowsy, eay to rouse
2
Moderate, frequently drowsy, easy to rouse
3
Severe, somnolent, difficult to rouse
S
Asleep but easily roused
AUTHOR:
CNS Acute Pain
FILE NUMBER:
CSPM A12
AUTHORISED:
Nov 2020
REVIEW DUE:
Nov 2024
This is a controlled document. The electronic version is the most up-to-date. Printed versions are valid on the day of printing only.
Page
2 of
2
 Appendix D:
MENTAL HEALTH SERVICE
PROCEDURE
Management of Suicidal People
Objective:
Appendix D:
MENTAL HEALTH SERVICE
PROCEDURE
Management of Suicidal People
Objective: To provide a guide to staff in the appropriate assessment and management of people who are at risk
of suicide.
Responsibility: All staff working with people who are at risk of suicide must follow the guidelines set out within this
policy and refer to other relevant Procedures/Protocols.
Client Group:
All people entering the South Canterbury District Health Board (SCDHB) Mental Health & Addictions
Service.
Associated Documents:
Memorandum of Understanding with NZ Police
Involving Families Procedure
Clinical Documentation Guidelines - Mental Health Service
Important Information
Staff will actively seek assistance from and give information to family/whānau/caregivers
throughout the assessment, crisis management and subsequent recovery process of their
family member.
A staff member may override a suicidal client’s refusal to involve family/whanau/caregivers
following consultation with the on call psychiatrist or the Multi-Disciplinary Team (MDT).
Clients who are not presenting with risk to self or others have the right to refuse to have
family/whanau/caregivers involved and the right to refuse treatment.
Clients who are under the Mental Health Act do not have the right to refuse to have
family/whanau/caregivers involved and do not have the right to refuse treatment.
Risk should be reviewed at every contact and documented in the progress notes.
Clients at risk of suicide should be discussed frequently in the MDT.
Referrals
All calls regarding threats of suicide, suicide attempts or deliberate self harm must be regarded
as a psychiatric emergency.
The person receiving the call is responsible for ensuring the caller is linked to the appropriate
staff member. That is, within working hours to their case manager or after hours to the TACT
team.
All calls regarding suicide risk or intent or deliberate self harm must, as well as action(s) taken,
must be recorded on a Triage Form or in the Progress Notes (if already known to MHAS).
Assessment of New Clients
A full risk assessment, which involves a comprehensive psychiatric assessment and collateral
information from family/whanau/friends will be carried out by the case manager or TACT team and
documented on the respective forms as per Service Framework Process.
Information is to be obtained from the National Health Index (NHI), HCS and Ajexus regarding any
previous admissions to psychiatric services. If there is a file locally this must be retrieved and reviewed
in terms of past diagnosis and previous risk patterns.
AUTHOR:
Clinical Director, Suicide Prevention Co-ordinator
FILE NUMBER: MHSM1
AUTHORISED: May 2020
REVIEW DUE: May 2022
This is a controlled document. The electronic version is the most up-to-date. Printed versions are valid on the day of printing only.
Page 1 of 4
 MENTAL HEALTH SERVICE
PROCEDURE
MENTAL HEALTH SERVICE
PROCEDURE
If suicide risk is identified, the assessment must be presented to the MDT or on-call psychiatrist for
the formulation of a safety plan. One of the options available to manage the risk is to admit to the
inpatient unit and if required, use of the Mental Health Act.
The Safety Plan (Crisis Plan) must be written up and discussed with the client. It will also be discussed
with family/whānau/caregivers wherever possible. If not available for discussion this must be
documented and future attempts made to discuss the Safety Plan with them.
If the client is to remain an outpatient, the case manager or TACT must discuss a comprehensive
Safety Plan with the family/whānau/caregivers and provide them with appropriate written information
about managing suicide risk e.g. being aware of treatment details of the underlying mental illness,
details of early warning symptoms, relevant contact details for health personnel if the risk increases.
This must include a conversation about when to use the Police and the reasons for approaching the
Police intervention e.g. in the event of any immanency to safety, if there are any physical harm
concerns etc.
The client’s assessment and management plan must be presented at the next MDT. If this occurs
over a weekend or public holiday the plan must be discussed with the on call psychiatrist then to the
MDT.
Counselling regarding restricting access to means:
Counselling about access to lethal means is a standard part of patient Safety Plans. However, staff
often advocate for removal of means without warning families of the risk of substitution of other
methods. We recommend that staff should be reminded that if they advocate restriction of access to
a preferred method of suicide, families and friends of the at-risk patient should routinely be warned
that removal of access to the preferred method may mean that some patients may substitute other,
more lethal methods, and that access to these methods should also be monitored.
Consider the client’s occupation and place of residence which may indicate obvious access to lethal
means.
Document what you have advised the client and/or family/whānau/caregivers to do to promote safety
and to restrict access to lethal means.
During subsequent phone calls/visits to the client continue to check access to means and that specific
items of concern have been removed.
Firearms
Ask all clients and their family/whanau/caregivers about access to firearms.
Advise families/whanau/caregivers to remove potential weapons, in particular, firearms. The safest
option is for the family to contact the police and request that firearms are removed. If an emergency
Tact should contact the police directly.
Medications and poisons and other means of suicide.
Advise the family/whanau/caregivers of the following:
1.
Ensure medications are accounted for and that medications (including paracetamol) are
locked away after they have been used.
Any prescription medications should be of a minimum amount. Check on HCS the current medications
being prescribed by the GP and request that they are close controlled.
AUTHOR:
Clinical Director, Suicide Prevention Co-ordinator
FILE NUMBER: MHSM1
AUTHORISED: May 2020
REVIEW DUE: May 2022
This is a controlled document. The electronic version is the most up-to-date. Printed versions are valid on the day of printing only.
Page 2 of 4
 MENTAL HEALTH SERVICE
PROCEDURE
MENTAL HEALTH SERVICE
PROCEDURE
Remove all medications that are lethal.
Clean out the medicine cabinet and dispose of all unused, out-of-date-medications.
2.
Ensure poisons, pesticides and, if applicable, agricultural chemicals are locked away. Dispose
of all unwanted poisons, pesticides and agricultural chemicals.
3.
Remove dangerous knives like machetes, and crossbows. If the person has fashioned a hose
for carbon monoxide poisoning or has fashioned a noose, remove these too.
Please note: staff are not expected to remove anything from a person’s property. They are to
advise family and/or the police.
Follow up
The suicidal client must be reviewed face-to-face and via telephone as often as directed by the MDT
and / or on-call psychiatrist until the period of risk has passed.
The client can remain under the care of the TACT in the acute phase then referred for case
management to the CMHT. Care is formally handed over at the time of the Partnership Appointment.
If the client does not attend for a scheduled appointment the TACT/case manager must make
telephone contact as soon as possible and if no answer, should phone family/whānau/caregivers
detailed on the Consent Form.
If no contact is made within 2 hours and there is serious concern about risk to self or others the Police
will be contacted and a Welfare Check requested.
Child and Adolescents
If a child or adolescent presents after hours and there is concern about serious suicide risk, they will
be assessed by the TACT with discussion with the on-call Adult Psychiatrist. The assessment and
management plan will then be discussed with the most appropriate iCAMHS staff the following day
and arrangements made for the client to be reviewed by the Child and Adolescent Psychiatrist as soon
as possible.
In the event an adolescent is unwilling to engage, the case manager or Tact Team will meet or make
phone contact with the family/whanau/caregivers to develop a clear Safety Plan (Crisis Plan
If the risk is at a lower level it may be prudent to discuss the situation with the child’s
family/whānau/caregivers by phone (including the child if of appropriate age) and to formulate a Safety
Plan for overnight. The duty ICAMHS worker or case manager will then see them the following day.
Assessment of Intoxicated People
People who present expressing suicidal ideation or following a suicide attempt whilst grossly
intoxicated are likely to be detained in the police cel s or in a ‘health facility’ (ED or the Kensington
Centre) for the prevention of suicide. The decision as to where the person should be seen will be
made by the police and Tact Team. They can only be held at the cells for a maximum of 6 hours.
Following this they will be assessed by the TACT Team and a Safety Plan developed as for any other
client. This includes family/whānau/caregivers involvement. Assessment should focus on their
immediate risk and a management plan formulated to address this
Those presenting with suicidal ideation whilst intoxicated, but not requiring police detention, will have
a Safety Plan developed jointly with the family, Tact Team and police if they are involved (ie: called to
the home due to a dispute) with arrangements made for the person to be contacted by Tact the
following day.
AUTHOR:
Clinical Director, Suicide Prevention Co-ordinator
FILE NUMBER: MHSM1
AUTHORISED: May 2020
REVIEW DUE: May 2022
This is a controlled document. The electronic version is the most up-to-date. Printed versions are valid on the day of printing only.
Page 3 of 4
 MENTAL HEALTH SERVICE
PROCEDURE
Safety Plan (Crisis Plan)
MENTAL HEALTH SERVICE
PROCEDURE
Safety Plan (Crisis Plan)
All clients must have a Safety Plan which is reviewed and updated at each appointment.
The purpose of the Safety Plan:
To minimise the risk and maximise the safety of the client.
To establish an effective therapeutic partnership with the client and
family/whānau/caregivers.
To institute an effective management plan in keeping with the principles of recovery and good
clinical practice.
As part of the Safety Plan the client and family/whanau/caregivers must be given contact phone
numbers to call for advice in a mental health emergency or suicide crisis.
At a minimum, the following numbers should be provided:
Need to Talk? - 1737 (phone call or text)
SCDHB Mental Health Tact Team number 0800277997
In an emergency, Police contact 111.
Emergency Department
A copy of the Safety Plan is to be sent to the Emergency Department (ED) for those people who have
a history of suicidal ideation, suicide attempts and/or self-harm. This is to be kept up to date and is
the responsibility of the case manager.
When clients present to the ED, staff are to check on Ajexus to see if the client is or has been involved
with the SCDHB MHAS and contact their case manager.
These clients are discussed at the quarterly ED/Mental Health Interface Meeting to ensure that the
Safety Plan is current and that the client still needs to be on this list.
Cultural Issues
Cultural contacts and beliefs must be considered in the assessment of clients.
This includes issues of identity, protocol within their culture, beliefs about suicide, culturally determined
preferences for methods of suicide, use of interpreters and the involvement of family and specialist
cultural workers.
AUTHOR:
Clinical Director, Suicide Prevention Co-ordinator
FILE NUMBER: MHSM1
AUTHORISED: May 2020
REVIEW DUE: May 2022
This is a controlled document. The electronic version is the most up-to-date. Printed versions are valid on the day of printing only.
Page 4 of 4
Document Outline