 Early Pregnancy Disorders Referral Pathway
Type:
Early Pregnancy Disorders Referral Pathway
Type: Clinical Guideline
HDSS Certification Standard:
Issued by: Maternity Audit Group
Version: 1.0
Applicable to: Gynaecology, Primary Care, Acute Services,
Document Owner: Alex Williamson –
Outpatients, Maternity
Maternity Clinical Quality Facilitator
Purpose
To provide a Wairarapa DHB-specific pathway for General Practitioners, Lead Maternity Carer
(LMC) Midwives, Acute Services staff and other providers to triage patients with miscarriage and
associated disorders.
To ensure timely, standardised, evidence-based management with efficient use of resources
while recognising and providing women’s choice.
Scope
Applies to all LMC midwives, medical, midwifery and nursing staff that provide care to women
requiring referral for cases of miscarriage or ectopic pregnancy.
Roles and Responsibilities
The
Primary Care Provider will:
1. Use the 3D Health Pathways
(3d.healthpathways.org.nz) for initial assessment and management.
2. Contact the Triage Midwife on 0275720283, Monday-Friday 0900-1600.
3. At other times institute initial management and contact the Triage Midwife when available.
4. Provide relevant documentation/investigations (email [email address] or
fax to: 069469848)
4.1 Referral letter
4.2 Ultrasound scans
4.3 Blood tests.
5. If there is high suspicion of ectopic pregnancy, uncontrollable vaginal bleeding or serious clinical
concern transfer directly to the Emergency Department (ED). On admission to ED manage as
appropriate and complete Early Pregnancy Follow up Form (Appendix 2).
The
Triage Midwife will:
1. Provide advice for further primary care management referring to Appendix 1 and the guideline
content.
2. Request and process relevant documentation/investigations.
3. Arrange elective secondary care management
3.1. Process relevant documentation/investigations
3.2. Arrange urgent clinic appointment via the booking clerk (on 069469833).
4. Discuss semi-urgent cases with the on-call Gynaecologist.
5. If there is high suspicion of ectopic pregnancy, uncontrollable vaginal bleeding or serious clinical
concern recommend transfer directly to ED.
Document author: David Cook, Gynaecologist Authorised by Maternity: Audit Group
Issue date: 08/05/19
Review date: 08/05/22
Date first issued: 08/05/19
Document ID: Allocated by WrDHB SharePoint
Page 1
CONTROLLED DOCUMENT – The electronic version is the most up to date version. The DHB accepts no responsibility for the consequences
that may arise from using out of date printed copies of this document.
Summary of findings and triage recommendation
Fetal pole
Adnexal
Free
Serial
Bleeding
IU Sac
POC
FHR
Triage
(CRL)
mass
fluid
BhCG
Threatened
Any
Present
-
Present
Present
¶
Absent
Rising
Primary
Uncertain
Any
<25mm
-
<7mm
Absent
¶
Absent
Any
Primary
Complete
Heavy
Absent
Absent
Absent
-
¶
Absent
Falling
Primary
Incomplete
Heavy
Any
Present
Any
Absent
¶
Absent
Falling
Primary/S
Anembryonic
Nil
>25mm
-
Absent
-
¶
Absent
Static
Primary/S
Missed
Nil
Any
-
Present
Absent
¶
Absent
Static
Primary/S
PUL
Minor
Absent*
-
Absent
Absent
¶
Absent
Any
Primary/S
Ectopic
Minor
Absent*
-
Absent
Any**
Present
Present
Any
S/ED
Mole
Any
Absent
Plentiful
Absent
Absent
¶
Maybe
High
S/ED
* Small, irregular pseudo sac might be seen
** FHR sometimes seen outside the uterine cavity
¶Corpus luteal cyst possible with any pregnancy
Most cases can be referred electively via the Triage Midwife.
Guideline
Women should be offered evidence based information and support to enable them to make
informed decisions about the management of their pregnancy. Women’s views and concerns are an
integral component of the decision making process. Women may choose expectant, medical or
surgical management this choice may be influenced by the clinical presentation and accessibility to
services.
Initial Assessment
Clinical assessment should be undertaken including medical history and baseline
investigations.
Check Rhesus status and anti-D requirement in all women.
Exclude significant anaemia.
Share information regarding choice of management options, women should be involved in
choosing their preferred option.
Consider
Non-obstetric causes of vaginal bleeding and pain.
Pregnancy supplements: Iron, folate and iodine.
Emotional and social support, share information regarding Crisis Pregnancy Support
Wairarapa.
Discuss future pregnancy plans, if desires another pregnancy can attempt to conceive when
she feels ready.
If not planning another pregnancy, discuss contraception and prescribe as necessary.
Early Pregnancy Disorders Referral Pathway Guideline
Page
2 of
7
Threatened miscarriage
Bleeding can be heavy but compatible with a viable pregnancy. Cramping and an open cervix
suggest inevitable miscarriage.
Slowly rising or falling hCG predicts non-viable pregnancy.
Institute expectant management.
Counsel regarding blood loss assessment.
Reduce daily activities (mainly of psychological value).
Repeat TV-USS for viability (7-10 days if persistent bleeding, selectively if asymptomatic).
Uncertain
Early viable pregnancy, early failed pregnancy or ectopic.
Slowly rising or falling hCG predicts non-viable pregnancy.
Repeat TV-USS when sac should be >25mm (grows 1mm per day).
Counsel regarding symptoms/signs of ectopic.
Complete miscarriage Expect vaginal bleeding to steadily decline over 10-14 days.
Repeat TV-USS if bleeding increases or is prolonged.
Incomplete miscarriage
Anembryonic pregnancy (‘Blighted ovum’)
Missed miscarriage
Discuss and determine management plan.
Ensure formal review if expectant management and repeat TV-USS if prolonged.
Counsel regarding symptoms/signs of infection.
Refer to secondary care for medical or surgical treatment.
Pregnancy of Unknown Location (PUL)
Expectant management with planned review,
Counsel regarding symptoms/signs of ectopic.
Measure serial hCG levels.
If hCG level increasing repeat TV-USS.
Ectopic pregnancy
Trophoblastic disease (e.g. Hydatidiform mole)
Refer directly to secondary care for expectant, medical or surgical treatment.
Early Pregnancy Disorders Referral Pathway Guideline
Page
3 of
7
Implementation and monitoring compliance with/effectiveness of document
Data captured for acute presentation in the Emergency Department will continue to measure the
effect of the introduction of internal referral systems on a quarterly basis.
Monitoring of complaints regarding miscarriage management within the DHB will continue with a
vision that these will significantly reduce.
Workload for the Antenatal Clinic midwife will be monitored as the triage component is an
introduction to this role.
Definitions
Early Pregnancy: gestation up to 12 weeks and 6 days. (For pregnancy loss at ≥12+6/40 gestation see
mifepristone protocol).
Miscarriage: The recommended medical term for pregnancy loss under 20 weeks is ‘miscarriage’ in
both professional and woman contexts. The term ‘abortion’ should not be used.
Threatened miscarriage: a viable pregnancy is confirmed by ultrasound, but there has been an
episode of PV bleeding.
Missed miscarriage: a non-viable intrauterine pregnancy. No fetal heart activity is seen, the
gestational sac is intact, the cervix is closed and no POC have been passed.
Incomplete miscarriage: some pregnancy tissue has been passed but there is a clinical or ultrasound
evidence of retained tissue.
Complete miscarriage: all the pregnancy tissue has been passed and the uterus is empty.
Anembryonic pregnancy (blighted ovum): the gestational sac has developed but the embryo hasn’t.
References
Horne. A.W and Alexander. C. Recurrent miscarriage,
BMJ Sexual & Reproductive Health.
2005, 31 (2), pp 103-107.
https://www.midwife.org.nz/women/for-women/pregnant/miscarriage/
Prager. S, Mase. M, Dalton. V.K and Schreiber, C. A. Pregnancy Loss (miscarriage): Risk
factors, etiology, clinical manifestations and diagnostic evaluation. Up-to-date.com,
https://www.uptodate.com/contents/pregnancy-loss-miscarriage-risk-factors-etiology-
clinical-manifestations-and-diagnostic-evaluation
Regan, L. Epidemiology and the medical causes of miscarriage,
Best Practice & Research
Clinical Obstetrics & Gynaecology. 2000, 14 (5), pp 839-854.
Related Documents
WrDHB Early Pregnancy Follow up Form (available as standalone document on SharePoint Forms
and Templates)
Early Pregnancy Disorders Referral Pathway Guideline
Page
4 of
7
 Keywords for searching
Keywords for searching
Miscarriage
Early pregnancy
Ectopic pregnancy
Appendices
1. hCG and Ultrasound Parameters
2. Early Pregnancy Bleeding Follow Up
Disclaimer: This document has been developed by Wairarapa District Health Board (WrDHB) specifically for its own use. Use
of this document and any reliance on the information contained therein by any third part is at their own risk and WrDHB
assumes no responsibility whatsoever for such use.
Approval Authority Signature
Name:
Michelle Thomas …………………………………………………..
Role:
MQSP Coordinator…………………………………………………
Signature:
Date:
08/05/19 …………………………………………………………………
Early Pregnancy Disorders Referral Pathway Guideline
Page
5 of
7
Appendix 1 - hCG and Ultrasound Parameters
From LMP Normal hCG levels
hCG doubling
IU Sac
CRL
Yolk sac
FHR
(weeks)
(mIU/ml)
time
Non-pregnant
<5.0
3
5 - 50
4
5 - 426
N/A
31-72 hours
5
18 - 7,340
(longer with
10 mm
2-3 mm
advancing
6
1,080 - 56,500
gestation)
14-16 mm
2-4 mm
3.5 mm
7-8 7, 650 - 229,000
20-28 mm
8-15 mm
3.8-4.3
Visible
mm
9-12 25,700 - 288,000
38+ mm
26+ mm
4.8-5.1
hCG levels off
mm
13-16 13,300 - 254,000
17-24
4,060 - 165,400
N/A
hCG levels fall
25 - 40
3,640 - 117,000
Postmenopausal
<9.5
Early Pregnancy Disorders Referral Pathway Guideline
Page
6 of
7
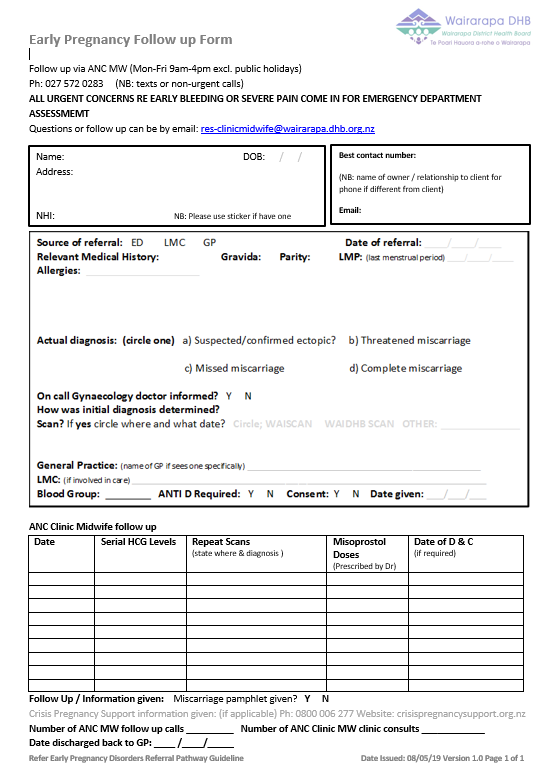
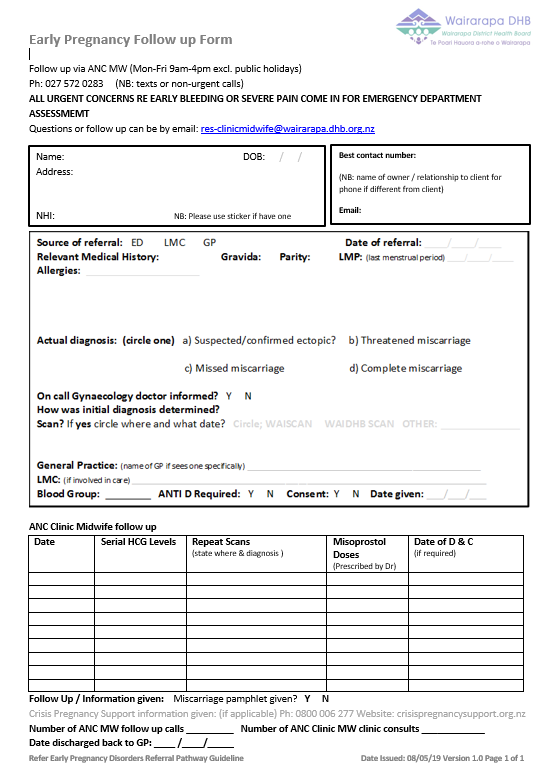 Appendix 2 – Early Pregnancy Follow up Form
Appendix 2 – Early Pregnancy Follow up Form
Early Pregnancy Disorders Referral Pathway Guideline
Page
7 of
7