 MINISTRY OF
MINISTRY OF
HEALTH
MANAT\J IIAUORA
Document 1
Briefing
Internal Review of the June Sydney to Wellington Traveller Case 2021
Date due to MO: 24 September 2021
Action required by:
N/A
Security level:
IN CONFIDENCE
Health Report number: 20211771
To:
Hon Chris Hipkins, Minister for COVID 19 Response
Copy:
Hon Dr Ayesha Verra II, Associate Minister of Health
1982
Act
Contact for telephone discussion
Name
Position
Telephone
Information
Bridget White
Deputy Chief Executive, COVID 19 Health s 9(2)(a)
I
System Response
Official
Minister's office to complete:
the
D Approved
D Decline
D Noted
D Needs change
D Seen
D Overtaken by
events
under
D See Minister's Notes
D Withdrawn
Comment:
Released
 Internal Review of the June Sydney
Internal Review of the June Sydney
Document 1
to
Wellington Traveller Case 2021
Security level:
IN CONFIDENCE
Date:
24 September 2021
To:
Hon Chris Hipkins, Minister for COVID-19 Response
Copy:
Hon Dr Ayesha Verrall, Associate Minister of Health
Purpose of report
1982
1.
The purpose of this briefing is to provide you with an overview of the internal review of
the health system response to the June Sydney to Wellington Traveller Case.
Act
Summary
2.
As part of the Ministry of Health's (the Ministry) commitment to continuous
improvement, an interval review was undertaken into the response of the June Sydney to
Wellington Traveller Case that resulted in Wellington moving into Alert Level Two on 23
June 2021.
Information
3.
The review highlights that the overall response was rapid and effective which led to no
community outbreaks occurring.
4.
There have been lessons identified and this review makes six recommendations with
Official
specific actions to strengthen these areas. The relevant teams within the Ministry have
been made aware of the actions necessary to support these findings and the report
the
outlines progress made against these. Consistent with our approach for continuous
improvement, we have already enhanced and adjusted some crucial processes and
systems derived from these learnings. These have been outlined in the review.
under
5.
Please note, that the
Interval Review of June Sydney to Wellington Traveller Case 202 7
was completed prior to the current Auckland outbreak. A review which captures lessons
identified throughout the current outbreak will be explored at the conclusion of the
response.
Released
Briefing: HR202!1771
1982
Act
Information
Official
the
under
Released
 Internal Review of June Sydney
Internal Review of June Sydney
Document 1
to
Wellington Traveller Case 2021
Context
1.
The June Sydney to Wellington Traveller Case 2021 begun on 23 June when it was
identified that an individual who travelled from Sydney to Wellington on 18 June and
returned on the 21 June returned a positive test result for COVID-19.
2.
The Case resulted in zero community cases, two close-plus contacts, 981 close contacts
and 1743 casual plus contacts. The Case was confirmed by New South Wales health
authorities as an epidemiological link to the Bondi/Westfield Cluster in Sydney, Australia.
3.
On July 6 2021, the formal process to review the outbreak began through a series of
1982
debriefs and reports. In addition, a questionnaire self-assessment tool was developed to
inform the process and gain further insight into key learnings identified.
Act
4.
On 23 July 2021, an eight-week quarantine-free travel suspension from all Australian
states and territories to New Zealand came into effect due to the deteriorating COVID-
19 situation in Australia.
Review Overview
5.
The COVID-19 Advisory Group within the COVID-19 Health System
Information Response Directorate
led the review into the Case. The organisations, groups and agencies involved in the
response included:
a.
Department of the Prime Minister and Cabinet
Official
b. Capital and Coast District Health Board
c.
Ministry of Business, Innovation
the and Employment
d. Ministry of Foreign Affairs and Trade
e.
Ministry of Health
under
f.
Ministry for Primary Industries
g.
National Emergency Management Agency
h.
New Zealand Police
i.
Regional Public Health
Released
j.
Wairarapa District Health Board
Recommendations
6.
The recommendations that the review make are outlined below. The review provides
further details and current progress.
a. Further mitigate risk of staff fatigue and workforce pressures across the health
system through providing resource support and assistance.
Briefing: HR20211771
b. Re evaluate the available surge capacity health workforce so that the Ministry is well
Document 1
prepared to deliver increased operational resources in response to future incidents
and/or outbreaks
c. Examine communication channels with Australian counterparts to clarify delays and
ensure efficient information flow.
d. Review operational procedures and protocols to adjust to the developing COVID-19
situation, including the presence of the Delta variant and how this may affect our
response processes and practice.
e. Explore self-isolation procedures for individuals who are unable to self-isolate safely
f. Improve communication, collaboration and engagement across government
agencies so that decision-makers are well supported and are provided with the best
possible advice.
7.
Many any of these recommendations were already underway or already have existing
1982
processes.
Act
Communications Approach
8.
The release of the report may generate moderate public and media interest.
9.
If you choose to publicly release the report, we will provide you with a communications
pack to support your decision.
Next steps
Information
10.
We will provide you with an update in the coming months regarding the progress of the
review recommendations.
11.
We will provide you with a communications pack if you wish to proactively release the
Official
report and work with your office on necessary steps for release.
the
ENDS.
under
Released
Briefing: HR20211771
 Appendix 1: June Sydney to Wellington Traveller Case 2021
Appendix 1: June Sydney to Wellington Traveller Case 2021 Document 1
1982
Act
Information
Official
the
under
Released
Briefing: HR20211771
1982
Act
Information
Official
the
under
Released
Document 1
TABLE OF CONTENTS
INTRODUCTION
3
Case Summary and Timeline ............................................................................................................... 3
Incident Management Team Structure ............................................................................................... 3
Review Methodology Process ............................................................................................................. 4
SUMMARY KEY FINDINGS
4
The Incident Management Team Response Process .......................................................................... 5
Communications ................................................................................................................................. 5
1982
Capacity and Capability ....................................................................................................................... 6
Contact Tracing and Testing ................................................................................................................ 6
Act
RECOMMENDATIONS
7
NEXT STEPS 8
Information
APPENDIX 1: RECOMMENDATIONS 9
Official
the
under
Released
2
IN CONFIDENCE
Document 1
INTRODUCTION
A key strength of New Zealand’s response to COVID-19 is the commitment to continually review,
adjust and apply learnings to future activities.
The purpose of this internal review of the Ministry of Health’s (the Ministry) public health response
to the ‘June Sydney to Wellington Traveller Case,’ is to uncover the challenges experienced and
lessons identified, to inform our process of, and commitment to, continuous improvement. The
review outlines specific actions and work streams addressing issues identified.
CASE SUMMARY AND TIMELINE
On 23 June 2021, the Ministry was notified through the Australian National Focal Point that a
confirmed COVID-19 case travelled to Wellington from Sydney on 18 June 2021; returning to Sydney
on 21 June 2021. While the incident reported zero community cases, there were two close-plus
contacts, 981 close contacts and 1743 casual plus contacts identified. The case returned a positive
test result in Sydney from a test taken on 21 June 2021. s 9(2)(a)
and received their first vaccination dose for
COVID-19. New South Wales health authorities confirmed an epidemiological link to the
Bondi/Westfield Cluster.
In response to the incident, the Greater Wellington region moved to Alert Level 2 at 6:00pm on 23
June 2021, with the remainder of New Zealand staying at Alert Level 1. Further to the Alert Level
change, a public health risk assessment was undertaken regarding the Quarantine Free Travel (QFT)
status with New South Wales, Australia. As a result, at 11:59pm on 22 June 2021 a pause on QFT was
put in place for a period of 72 hours. At 11:59pm on 29 June 2021, the Greater Wellington region
moved back to Alert Level 1 alongside the remainder of New Zealand.
The COVID-19 situation has since deteriorated in New South Wales and expanded to the Queensland
and South Australian States. Subsequently, on 23 July 2021, the Australian QFT status was demoted
and an eight-week QFT suspension from all Australian States and territories to New Zealand came
under the Official Information Act 1982 into
effect.
INCIDENT MANAGEMENT TEAM STRUCTURE
The Ministry’s COVID-19 Incident Management Team (IMT) manages and coordinates the national
Released
health response to COVID-19 incidents and outbreaks and is the point of contact for public health
units (PHUs), district health boards (DHBs), Ministers, the Ministry’s Executive Leadership Team, and
other stakeholders. IMT is activated upon identification of a community case of COVID-19 and
includes a range of expertise from across the Ministry.
External organisations involved in the response include:
• Department of the Prime Minister and Cabinet
3
IN CONFIDENCE
Document 1
• Capital and Coast DHB
• Ministry of Business, Innovation and Employment
• Ministry of Foreign Affairs and Trade
• Ministry for Primary Industries
• National Emergency Management Agency
• New Zealand Police
• Regional Public Health
• Wairarapa DHB
REVIEW METHODOLOGY PROCESS
This internal review of the June Sydney to Wellington Traveller Case encompasses findings from the
1982
following:
1. A memo to Dr Ashley Bloomfield, Director-General of Health on 5 July 2021 titled
Situation
Act
Summary Report: Sydney to Wellington Acute Case.
2. A joint Ministry and DPMC briefing titled
Quarantine-Free Travel with Australia: Key
Learnings and Process Improvements. This briefing outlined key learnings from QFT
incidents, including how these learnings have informed actions to strengthen the QFT
system and better inform decision making.
3. A debrief with key stakeholders on 6 July 2021, chaired by the Group Manager, IMT.
Information
4. A self-assessment questionnaire of the incident was developed by the Ministry’s COVID-19
Advisory Group for this review and distributed on 21 July 2021 to key stakeholders listed
above who were involved in the response. Findings were collected, analysed and
summarised to inform this review. Official
5. A review and debrief analysis of the May-June 2021 Incidents titled
May-June 2021 Incidents
Analysis Reviews & Debriefs. This focused on key learnings and process improvements in
the
relation to the QFT incidents. These incidents include the Victoria QFT pause, June Sydney to
Wellington Traveller Case, New South Wales QFT pause and the Australia-wide QFT pause.
under
SUMMARY KEY FINDINGS
The review found that the Ministry response has continued to operate under a process of ongoing
improvement and agility throughout the maritime responses, which has proved effective in
responding to the incident.
Released
The key findings identified in this review are:
•
IMT: Robust structure and processes, as well as timely updates to key stakeholders which
provided assurance that the response was ‘fit for purpose’.
•
Cross government agency and stakeholder: Positive relationships and clear communication
channels ensured an efficient and aligned incident response.
4
IN CONFIDENCE
Document 1
•
Sector communications: Proactive communications ensured smooth information flow to the
wider health and government sectors.
While findings were largely positive, some areas are in need of strengthening:
•
External communications: Clarity of messaging and information provided to the public is
required, such as the communication of places of interest and the definition of close
contacts.
•
Workforce capacity and capability: Improved surge workforce capacity could alleviate staff
pressure and fatigue across the health system.
•
Isolation facilities: Ensuring there is facility capacity and contingency planning for contacts
required to self-isolate but do not have an appropriate place to do so.
•
Contact tracing and testing: Improved QR code placement advice, plans to mitigate the
1982
challenges of congestion at testing sites and availability of a surge contact tracing workforce.
Act
THE INCIDENT MANAGEMENT TEAM RESPONSE
The Ministry IMT processes for managing incidents were clear and efficient which allowed for quick
activation and notification of the incident which enabled a proactive response. Regular training
ensured that staff were familiar with response standard operating procedures (SOPs) resulting in a
rapid response while providing flexibility to adjust as the situation evolved.
Information
Regular IMT updates to response stakeholders ensured roles and responsibilities were clearly
defined. This included systematic IMT meetings with internal and external stakeholders, held daily,
which allowed for good information sharing and helped frame issue management during the
Official
response.
The review has also shown that some SOPs should be reviewed and adjusted as COVID-19 variants
the
emerge and the global situation develops.
COMMUNICATIONS
under
There have been noticeable improvements in incident response communication, in terms of pace,
external communication and cross-agency collaboration in comparison to previous events. The
established communication channels and flow of information through the system allowed for any
issues raised to be immediately addressed and effectively managed. However, there is an identified
Released
need to reduce confusion around information sources and the movement of unconfirmed
information. It is necessary for IMT to be the single source of truth, to avoid any misinformation or
duplication of effort.
Critical information and messaging to the public must be quick and accurate, especially regarding
information for contacts of a case and providing places of interest. Due to unclear messaging
following the June Sydney to Wellington Traveller Case, testing stations were crowded by people
that did not need to be tested.
5
IN CONFIDENCE
Document 1
There were initial challenges due to the delay of the provision of information regarding the traveller
case from Australian colleagues. In the future, the Ministry will set clearer expectations for incident
responses where international time zones and different processes between jurisdictions may cause a
delay in information gathering and sharing.
CAPACITY AND CAPABILITY
It is clear from the findings that health system capacity and capability continue to be a concern
across the sector.
Firstly, there is a need for the system to continue to work proactively to develop the existing
1982
capability and recruit or employ additional work force. Enabling swift response action and ensuring
flex in the system will support the fatigue of our key health workers externally, and Ministry staff
Act
internally in the event of an incident or outbreak.
Secondly, there is a system wide issue concerning the placement of those identified as being a close
contact not having a suitable facility to self-isolate safely. There are various reasons individuals are
unable to safely self-isolate e.g. living with family members or travellers. In this instance, 29 contacts
were placed in managed isolation facilities (MIF) to self-isolate. A risk was identified in this area as
there are no clear procedures in place for contacts or community cases in the event that they do not
Information
have anywhere to safely self-isolate. MBIE is responsible for the network of managed isolation and
quarantine facilities, with the Ministry holding relevant health components. As multiple agencies
contributed to this work, this will need to be escalated through the DPMC.
Official
Other key pressures noted included: the
• The impact of rapidly commissioned policy changes for programmes such as QFT and Alert
Levels, on Ministry teams who were already fatigued from expanded business as usual
deliverables.
•
under
The limited capacity to redeploy workforce to operational areas in order to provide
adequate surge. It was indicated that surge capacity could not sustain long periods of
operation due to limited resourcing, e.g. testing can scale up to 40,000 swabs a day but can
only be sustained at this level for a three-week period.
CONTACT TRACING AND TESTING
Released
There were numerous lessons identified in the contact tracing and testing components of the
response.
In this incident, over 2500 contacts were identified for a single traveller. Although the current
contact tracing capability was able to cope in this event, it was recognised that a larger scale
operation would put the National Investigation and Tracing Centre (NITC) under immense strain to
6
IN CONFIDENCE
Document 1
support the response to an incident or outbreak. In addition, there was QR code confusion, for
example, one location may have one QR code for upstairs and downstairs areas. There is a need to
ensure consistency of QR codes across locations so that they are easy to find and use, resulting in
more people scanning and accurate location information.
There were capacity issues with testing stations in terms of availability, waiting times, appointments,
drop ins, and priority groups for people who were identified as close contacts and at locations of
interest. As a result, some people did not receive their test result within the 48-hour period. It was
observed that PHUs need to update contingency plans to stand up sufficient testing sites to meet
increased demand in response to an incident, especially with the emergence of more infectious
variants of COVID-19 that could put immense strain on resources. In addition, people seeking
information or guidance from Healthline often faced long wait times (in some instances, waiting
times reached up to two hours) due to capacity challenges and the increase of callers. This resulted
1982
in many people giving up; increasing the risk of the public not getting the information they require.
Act
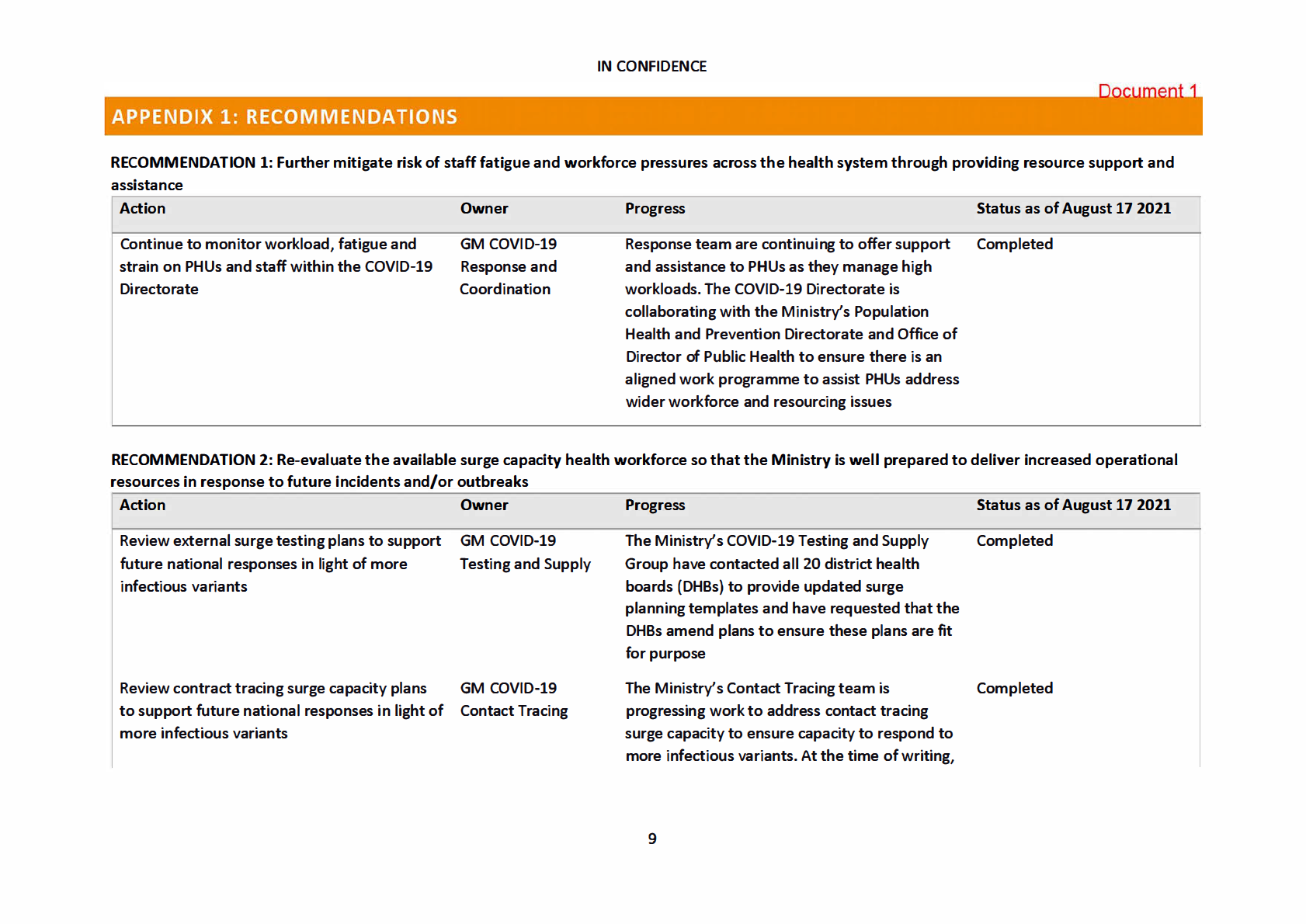
RECOMMENDATIONS
As a result of the above findings, outlined below are recommendations to streamline and enhance
the response to future incidents. These will be as part of SOP and process, amendments, to improve
the Ministry’s response to community outbreaks and incidents. The key themes identified to
strengthen planning for, and execution of, future responses are:
Information
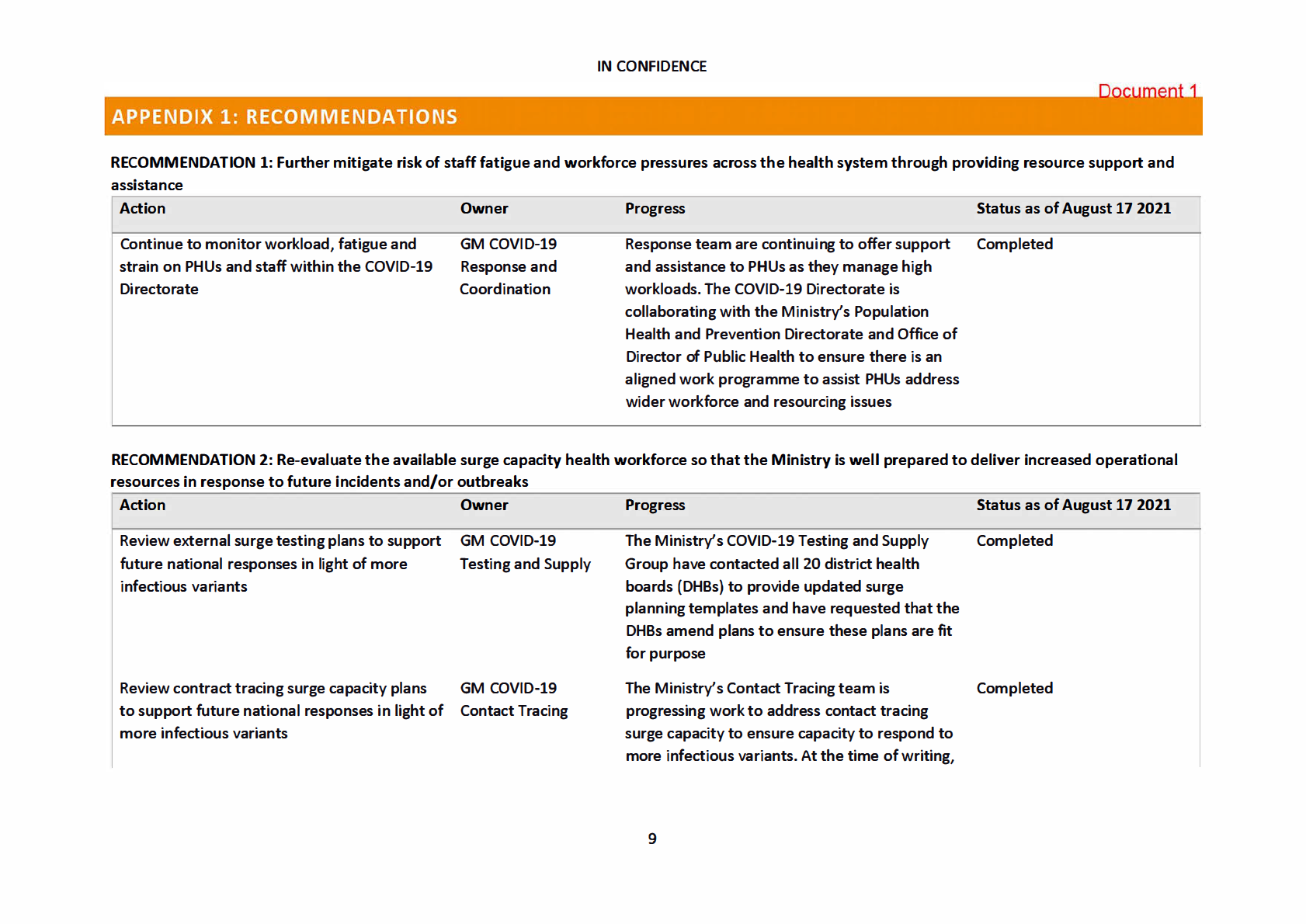
1.
Further mitigate the risk of staff fatigue and workforce pressures across the health system
through providing resource support and assistance
2.
Re-evaluate the available surge capacity health workforce so that the Ministry is well
Official
prepared to deliver increased operational resources in response to future incidents and/or
outbreaks
the
3.
Examine communication channels with Australian counterparts to reduce delays and
ensure efficient information flow
4.
Review operational procedures and protocols to adjust to developing COVID-19 situation,
under
including the presence of the Delta variant and how this may affect our response processes
and practice
5.
Explore self-isolation procedures for individuals who are unable to self-isolate safely
6.
Improve communication, collaboration and engagement across Government agencies so
that decision makers are well supported and are provided with the best possible advice.
Released
Many of these recommendations were already underway or already have existing processes in place
during or shortly after this response was concluded. However, by undertaking this review and
identifying recommendations, this provides the Ministry an opportunity to further strengthen its
response processes and procedures.
7
IN CONFIDENCE
Document 1
NEXT STEPS
Identified actions to be implemented as a result of the key recommendations discussed can be
found in Appendix 1.
In addition, the Ministry’s practice to review and reflect on each incident has developed a culture of
continuous improvement. As a result, actions will continue to be tracked and updated as part of our
business-as-usual processes which includes sharing this review and the identified recommendations
with the COVID-19 Independent Continuous Review, Improvement and Advice Group and Minister
for COVID-19 Response.
1982
Act
Information
Official
the
under
Released
8
1982
Act
Information
Official
the
under
Released
 IN CONFIDENCE
IN CONFIDENCE
Document 1
a report is currently with Hon Chris Hipkins,
Minister for COVID-19 Response, for his
consideration. The Ministry will continue to
update Ministers as this work progresses.
Develop self-isolation options and alternatives DPMC COVID-19
The Ministry has identified this issue with DPMC Underway - to be competed
1982
for individuals who are unable to safely self
Response Group
and they are working to identify suitable
by November 2021
isolate
(Health input/DPMC
alternatives to address this issue. Act
led)
Re-evaluate DHBs and PHUs contingency
GM Response and
The Ministry IMT are undertaking regional visits
Completed
planning to stand up COVID-19 testing centres Coordination
with all DHBs and PH Us to ensure readiness
testing and provide assurance on contingency
planning. This includes pre-identified pop up
COVID-19 testing centres that have the ability
Information
to rapidly surge in response to a Delta variant
outbreak or incident.
RECOMMENDATION 3: Examine communication channels with Australian counterparts to reduce delays and ensure efficient information flow
Official
Action
Owner
Progress
Status as of August 17 2021
the
Continue to review the process of gathering
GM COVID-19
There are monthly meetings with Australian
Completed
information through Australian National Focal
Intelligence and
counterparts that the Ministry attends to
Point portal
Surveillance
discuss a range of matters including information
sharing and any issues that may arise with the
under
current process. These have been very
productive to date and the Ministry is
continuing to build relationships with our
Australian counterparts.
Released
10
 IN CONFIDENCE
IN CONFIDENCE
Document 1
RECOMMENDATION 4: Review operational procedures and protocols to adjust to developing COVID-19 situation, including the presence of Delta
Action
Owner
Progress
Status as of August 17 2021
Review of COVID-19 response process in light
GM COVID-19
The Ministry has established an internal
Underway - to be completed
of emerging Delta variant to ensure these
Advisory
working group to drive a programme that will
by November 2021
methods are fit for purpose
review each of the response areas and update
1982
them if necessary, to ensure they are fit for
purpose to respond to the increased threat
Act
posed by the Delta variant.
Review of Alert Level frameworks in light of
GM System, Strategy As part of the working group above, the Alert
Underway - to be completed
emerging Delta variant
and Policy
Level guidance will be reviewed to ensure that
by November 2021
the framework is fit for purpose to respond to
the increased threat posed by the Delta variant.
Review Public Health Risk Assessment criteria
Office of the Director As part of the workstream above, the Public
Underway to be completed
Information
of Public Health
Health Risk Assessment criteria will be reviewed by November 2021
to ensure that the framework is fit for purpose
to respond to the increased threat posed by the
Delta variant.
Official
RECOMMENDATION 5: Explore self-isolation procedures for individuals
the
who are unable to isolate safely
Action
Owner
Progress
Status as of August 17 2021
Support the develop of self-isolation options
DPMC COVID-19
The Ministry has identified this issue with DPMC Underway - to be completed
under
and alternatives for individuals who have
Response Group
and they are working to identify suitable
by October 2021
unsuitable facilities to safely self-isolate
(Health input/DPMC
alternatives to address this issue.
led)
Released
11
IN CONFIDENCE
Document 1
RECOMMENDATION 6: Improve communication, collaboration and engagement across Government agencies so that decision makers are well supported
and are provided with the best possible advice.
Action
Owner
Progress
Status as of August 17 2021
Providing SOPs/diagram outlining sources of
Manager, Office of
The Ministry is reviewing and standardising our
Underway - to be completed
contact and how and when to engage with the the Deputy Chief
current approaches and finalising a flowchart
October 2021
1982
Ministry of Health during a response to an
Executive
for circulation to the relevant agencies in due
outbreak and/or incident.
course.
Act
Continue to clarify the key health messages
GM Communications The Ministry has further clarified our key
Completed
and guidance provided to the public, so that
and Engagement
messages about who needs to be tested,
there is greater public understanding of
particularly with regards to secondary contacts
actions needed and decisions made. This will
(ie about them not needing to isolate or be
ease the current pressure felt by COVID-19
tested, unless their contact develops
Information
operations.
symptoms); and communicate this to key
stakeholders such as Ministers, DPMC, DHBs
etc.
Official
The Ministry are also updating our 'easy read'
Underway - to be completed
materials on the website to ensure the most up- September 2021
the to-date public health advice is disseminated.
The Ministry continues to work with the DPMC
Communications team who are developing a
fact sheet on staying at home/self-isolating for
under
people with English as a second language or
who have a disability.
Released
12

Document 2
Briefing
Changes to implement shorter stay MIQ and self-isolation
Date due to MO: 4 November 2021
Action required by:
N/A
Security level:
IN CONFIDENCE
Health Report:
20212389
1982
To:
Hon Chris Hipkins, Minister for the COVID-19 Response Act
Contact for telephone discussion
Name
Position
Telephone
Information
Maree Roberts
Deputy-Director General, System Strategy s 9(2)(a)
& Policy
Bridget White
Deputy Chief Executive, COVID-19 Health
s 9(2)(a)
Official
System Response
the
Minister’s office to complete:
under
☐ Approved
☐ Decline
☐ Noted
☐ Needs change
☐ Seen
☐ Overtaken by events
☐ See M nister’s Notes
☐ Withdrawn
Released
Comment:

Document 2
Changes to implement shorter stay MIQ
and self-isolation
Security level:
IN CONFIDENCE
Date:
04 November 2021
To:
Hon Chris Hipkins, Minister for COVID-19 Response
1982
Purpose of report
Act
1.
This paper updates you and seeks your agreement to changes for the implementation
of shorter stay MIQ and self-isolation for people crossing the border into New Zealand.
Summary
2.
This paper provides information on how the 7 days managed isolation followed by 3
Information
days in self isolation will be implemented ahead of November 14.
3.
We are proposing a high-trust model for the self-isolation component that requires
people to stay at home, and will provide guidance to support self-management.
Official
4.
To manage the public health risk, we are enhancing the testing regime to allow for a
day 0/1 test, day 3 test, day 5/6 test, a rapid antigen test on departure from Managed
the
Isolation when required, and a compulsory day 9 test once in self-isolation.
5.
We will be amending the COVID-19 Public Health Response (Isolation and Quarantine)
Order 2020 to enact this new regime, and will be making subsequent amendments to
the Air Border Order and Mari
under time Border Order to enact these changes.
6.
There are processes underway to identify solutions to manage unique situations where
people may not be able to enter self-isolation, or may require assistance to identify an
appropriate setting for self-isolation.
Released
Recommendations
We recommend you:
a)
Note that the changes we are proposing are necessarily light touch and high
Noted
trust due to the low public health risk and competing pressures on the health
and managed isolation system
b)
Note that people who are self-isolating will be expected to travel to their
Noted
home or accommodation and be self-sufficient for 3 days, only leaving to
undertake a day 9 test


Document 2
c)
Agree that the COVID-19 Public Health Response (Isolation and Quarantine)
Yes/ No
Order 2020 be amended to reflect the 7 day managed isolation and 3 day
self-isolation requirements
d)
Note that we are developing guidance to support people during self-
Noted
isolation, including access to health services
e)
Note that an email-based compliance check will occur on day 10 for those
Noted
who have not yet accessed their day 9 test at a community testing centre, and
then on days 11, 12, 13 and 14 if needed
f)
Note we are enacting changes to the Isolation and Quarantine Order and an
Noted
associated direction under clause 9 of the Order to make tests on day 9
compulsory while people are self-isolating
1982
g)
Agree to move from a day 6/7 PCR test to a day 5/6 PCR test to increase the
Yes/No
likelihood that people will receive a test result prior to leaving managed
Act
isolation and to help manage workforce pressures
h)
Agree that rapid antigen tests are only used prior to departure when a day
Yes/No
5/6 PCR test result has not been received and the person is travelling outside
of the Auckland region
i)
Agree that the Maritime Border Order is amended to align maritime arrivals
Yes/No
to a 10 day isolation period
Information
j)
Note that we are working through potential situations where the Maritime
Noted
Border Order may need to retain a 14 day isolation period, including where
people are not vaccinated or due to undertake onwards travel
Official
k)
Note we are actively developing processes to enable day 9 testing including
Noted
regulatory changes to make this compulsory
the
l)
Note we are not going to proceed with the saliva based PCR testing trial in
Noted
MIQ facilities at this time due to resource pressures
under
m)
Note we are working to enact changes to relevant legislation to enable these
Noted
changes to occur and you will receive further advice to enact these changes
Released
Dr Ashley Bloomfield
Hon Chris Hipkins
Director-General of Health
Minister for COVID-19 Response
Te Tumu Whakarae mō te Hauora
Date:
Date: 4/11/2021
Briefing: <HR20212389>

Document 2
Changes to implement shorter stay MIQ
and self-isolation
Context
1.
On 28 October 2021 Ministers agreed to shorter stays in MIQ and self-isolation until
receipt of a negative day 9 test result from 14 November 2021 for those arriving by ai
1982 r
[HR20212360 refers].
Act
2.
The length of stay in managed isolation will reduce from 14 days (336 hours) to 7 days
(168 hours) followed by self-isolation until individuals return a negative day 9 test
before they are able to exit self-isolation. Note that this may mean a slightly longer
period of self-isolation than 3 days, depending on lab turnaround times from the day 9
test.
3.
This paper provides information on how we will mplement these changes.
Information
4.
These changes are taking place at a time when the MIQ and health system are both
under considerable pressure. Given the limited public health risk from reducing MIQ
stays, we have prioritised light touch and high trust interventions where possible.
5.
The changes also provide an opportunity to trial self-isolation at scale and learn for
Official
future changes to support a greater role for large scale self-isolation.
the
Changes to implementation shorter stay MIQ and self-isolation
Testing regime
under
6.
There are several changes to the testing regime that are recommended in order to
better align with shorter stays in MIQ and the self-isolation component.
Shifting to a day 5/6 test from a day 6/7 test
7.
To support more people receiving the result of their last PCR test before they leave
Released
MIQ, we recommend changing to a day 5/6 test from the current day 6/7 test.
8.
This change has a range of benefits. It spreads out the testing workload for the MIQF
health workforce, managing surges in demand for testing that could exceed workforce
capability in MIQ facilities. There is a real risk that if we remain with day 6/7 testing as
well as additional rapid antigen tests on departure, some testing could not occur due to
workforce limitations.
9.
Changing the day of testing would also reduce the likelihood that a rapid antigen test
would need to be used, as the confirmatory PCR test would have already been received.
This helps to manage the risks of false positive test results delaying travel.
10.
From a public health perspective there is a low risk of missing cases by testing a day or
two earlier, especially given the low numbers of cases in MIQ and the earlier

Document 2
identification of positive cases through testing of the Delta variant. The addition of day
9 tests also helps to promptly identify cases that may emerge later.
Implementing day 9 testing
11.
The day 9 test will need to be provided through a community testing centre or by GPs.
Access to the day 9 test may be limited in some cases, especially remote areas of New
Zealand with no weekend testing providers and where people need to travel many
hours to their closest community testing centre or GP.
12.
Testing on day 9 will be compulsory, as required by the testing requirement in the
Isolation and Quarantine Order. Compliance will be tracked through an automated
system that will send emails to people who have not undertaken a test on day 9, on
days 10 through 14 as needed.
1982
13.
The Ministry for Business Innovation and Employment (MBIE) is prepa ing changes to
the Isolation and Quarantine Order to enact the changes to Managed Isolation and the
Act
3 day self-isolation requirement, as well as acting on advice from the Ministry of Health
to make a day 9 test compulsory.
Rapid antigen testing on departure from Managed Isolation
14.
We recommend the use of rapid antigen tests only when the result of the day 5/6 test
has not been received prior to an individual’s scheduled release on day 7.
Information
15.
The use of rapid antigen testing will be a new process in MIQ facilities. We recommend
that rapid antigen tests are only required of those who have not yet received their
result from a day 5/6 test and those who are travelling outside the Auckland region.
16.
We propose the testing will be conducted by a MI
Official Q health worker and provide a level
of assurance pending the result of the PCR test result. It will also help to streamline and
not hold up the departure process.
the
17.
The change in approach from elimination to managed protection in Auckland means
that the use of rapid antigen tests to promptly identify cases is of less value. Other
regions in Alert Level 3 will sti
under ll require testing before travel particularly to provide an
added layer of assurance for those without day 5/6 test results if they are using public
transport (e.g. domestic flights) to travel to their place of self-isolation.
18.
When a rapid antigen test provides a positive result, the person will need to remain
iso ated until the result of the PCR test is received. If both the rapid antigen test and
PCR test are positive, they will be required to enter quarantine or self-isolation
Released
depending on the assessment of the Medical Officer of Health
Saliva testing
19.
With the shortening of MIQ stays, Ministers agreed to pause the pilot to introduce
saliva testing at MIQFs. DHBs will continue to use PCR nasopharyngeal tests in the new
shorter duration model MIQF system as these are considered the best test for the
purpose of diagnosing COVID-19 in facilities before returnees are released into self-
isolation, and because the operational processes for administering nasopharyngeal
swabbing are well established.
Briefing: <HR20212389>

Document 2
20.
We will re-visit whether and how saliva testing could be incorporated into the returnee
testing regime in the first quarter of 2022, once these changes to the MIQF system are
bedded in.
Review of testing regime for managed isolation and self-isolation
21.
As part of implementing these new changes, we will be conducting a review of the new
testing regime and assessing implementation. The review process will inform future
changes to the testing process, particularly for those in self-isolation.
Self-isolation component
Self-isolation will be similar in practice to self-isolation for low-risk contacts
1982
22.
The self-isolation approach for those arriving by air will be light touch and high trust.
There is a relatively low risk to public health by those arriving by air self-isolating
Act
compared to the public health risks posed by community cases or close contacts,
particularly in the Auckland region.
23.
Individuals will be strongly encouraged to self-isolate in a dwelling that does not
accommodate anyone except themselves and their travel bubble members. However, if
this is not available, self-isolating in a household with whānau or friends that are
already in Aotearoa New Zealand will be permitted. In this instance, self-isolation
involves isolating away from other members in the household (for ex
Information ample, have no
physical contact, minimise time in shared spaces like kitchens and bathrooms, and do
not share items such as cutlery and linen), while in their home or accommodation.
24.
No visitors to the household will be permitted during the period of self-isolation,
Official
however, household members who are not part of the travel bubble will not be
required to self-isolate i.e. they will be permitted to go to work and school while the
returnee(s) are self-isolating. the
25.
Unlike in the self-isolation pilot, no restrictions will be placed on the nature or
requirements of the self-isolation dwelling (e.g. specific ventilation requirements),
except that:
under
a. It cannot be in a shared accommodation venue that requires use of facilities (e.g.
bathrooms and/or kitchens) that are shared with someone that the returnee does
not know (e.g. hostels, boarding houses), and
b
It must be somewhere with cell-phone coverage, so that returnees can be called
Released
and/or texted by public health officials if needed, and
c. It must be somewhere from which the returnee(s) can access a COVID-19 testing
centre, so that they can meet the requirement to be tested on day 9.
26.
There will be no individual assessment of people’s self-isolation plans before they leave.
People will be provided communication to ensure they understand expectations of
them and how to raise questions or concerns.
27.
People will travel to their home or accommodation and be expected to stay there until
they receive a negative day 9 test result. Private transportation (i.e. self-driving) will be
strongly recommended. However, if this is not available, they will be permitted to use
public transportation (e.g. taxis or domestic flights) to travel to their place of self-
Briefing: <HR20212389>

Document 2
isolation. It is not operationally feasible to require or provide private transportation
services for all those entering self-isolation.
28.
Returnees will be advised to adhere to typical public health measures during travel,
including mask use, maintaining physical distancing from those not in their bubble
where possible, and performing regular hand hygiene. Returnees will be advised to take
the fastest and most direct route to their place of self-isolation, and will not be
permitted to stop at public venues (e.g. supermarkets) or visit people along the way.
29.
Returnees will be responsible for their own basic supplies during their period of self-
isolation. People will be encouraged to have supplies delivered wherever possible,
however we acknowledge that will not always be possible.
30.
We are developing guidance for self-isolation that will cover where people can access
support and health care, wellbeing advice, information on testing, as well as self-
1982
isolation requirements. This guidance will be shared with returnees at multiple points
prior to their travel (e.g. on public websites and in MIAS), as well as during their stay in
Act
a MIQF.
This will operate as a high trust model
31.
Given the lower public health risk of people in self-isolation in this model, the need for
intensive compliance monitoring is lower. Given resource restraints, we will not be able
to review self-isolation arrangements.
Information
32.
A final health check will be completed on leaving the MIQ facility and no further health
checks will be completed during the final three days of self-isolation. People will be
given clear guidance on what to do if they develop symptoms during that period which
will require them to contact Healthline or their GP.
Official
33.
People who do not attend testing on day 9 will be in breach of the Isolation and
Quarantine order. People are released from self-isolation once they receive the result of
the
their day 9 test.
People who self-isolate will have access to health support
under
34.
People will have access to Healthline, or their GP, as a first point of contact for health
issues. As part of guidance provided to people in self-isolation, we will provide advice
on how they can contact Healthline (or their GP), and wording to declare that they are
currently in self-isolation. Healthline will be able to triage people and provide advice on
access to further health services.
Released
35.
We will not be conducting daily health or symptom checks during the self-isolation
period. The email on days 10 to 14 will be to check for compliance when a test has not
been completed. If a person becomes unwell, they will call their GP or Healthline
advising that they are a recent returnee, or go to a community testing centre to be
tested.
Isolation requirements for specific groups
36.
We expect that nearly all people will be able to go into self-isolation after 7 days,
however we are working with MBIE on the implications of the change for specific
groups, including people travelling to Antarctica, sports teams and Russian mariners.
Briefing: <HR20212389>

Document 2
Maintaining a fixed 7 day time period assists planning, and prevents potential
inequities where blanket rules could lead to inequities between groups.
37.
We are working through what will happen in particular cases where people will be
unlikely to have access to accommodation or be subject to particular requirements
during the transitional period, including refugees, ‘501’ deportees or people travelling
to Antarctica.
Management of positive cases
38.
If cases are identified in Managed Isolation, they will continue to be treated in the same
way as current cases, i.e. they will be transferred to quarantine. If people have
symptoms, but no positive test result, these cases will be screened through the low-risk
indicators process and released following clearance from a health professional
1982
following existing processes and protocols.
39.
For cases identified when people are self-isolating, their management will depend on
Act
their accommodation and any other needs that they may have. We are proposing that
as with other community cases, they will be assessed by a Medical Officer of Health and
an appropriate plan put in place.
Regulatory changes to enable these changes
Changes to the IQO will be enacted
Information
40.
Changes to the COVID-19 Public Health Response (Isolation and Quarantine) Order
2020 will be made to reflect the change to a 7 day managed isolation stay followed by
3 day self-isolation. We will also be developing changes to enact the compulsory day 9
Official
test for people in self-isolation. We will also be drafting subsequent changes to the Air
Border Order and Maritime Border Order to reflect the shorter MIQ stay.
the
Changing the Maritime Border Order to align to the IQO
41.
We seek your approval to amend the Maritime Border Order to reduce the length of
under
isolation from 14 days to 10 days to align with the changes for those arriving by air
42.
Consistency across the air and maritime border in terms of isolation period is
important. A difference in isolation period for those coming across the maritime border
could result in an inequitable outcome for both the commercial and recreational
maritime sector.
Released
43.
The risk associated with reducing the isolation requirements at the maritime border is
considered to be manageable. This reflects that the incubation period of the Delta
variant is less than 10 days and that there are a range of stringent public health
controls in place for seafarers disembarking their vessel. If crew are seeking shore leave,
they must satisfy the low-risk indicators of a negative PCR test and be permitted to
disembark by the Medical Officer of Health situated at the port.
44.
For the majority of recreational maritime vessels, the transit time to New Zealand is
usually longer than 14 days and they tend to have smaller crew sizes that are arriving
from lower-risk countries (i.e. Pacific Countries).
Briefing: <HR20212389>

Document 2
45.
We are working through potential circumstances where a longer stay in MIQ may be
required.
Equity
46.
Those returning to New Zealand should not have to stay in MIQF any longer than is
necessary to protect the public health of New Zealanders.
47.
Recent evidence indicates that the increased risk of transmission of COVID-19 from
reducing a returnee’s isolation period to 10 days is low, with the series of tests and
other appropriate mitigations now in place. This is consistent with our proposed
approach to the management of community close contacts.
48.
Reducing the length of stay in MIQF will half the cost for returnees making the system
more affordable and equitable to a wider range of people.
1982
Next steps
Act
49.
We are continuing work on detailed implementation planning We will be working
closely with MBIE and other agencies to develop appropriate support for people who
will not be able to self-isolate. The expectation is that people leave Managed Isolation
on day 7, unless there is an exceptional reason.
50.
Health and MBIE will continue to work through the legislative options. We will provide
advice on enacting changes to the COVID-19 Public Health Response (Isolation and
Information
Quarantine) Order 2020, and subsequent regulatory changes outlined in this briefing
before 14 November.
51.
We have recently met with the Office of the Ombudsman who are keen to proactively
engage to support the development of processe
Official s that are consistent with relevant
human rights frameworks. We will work with them as we fine tune proposals.
the
ENDS.
under
Released
Briefing: <HR20212389>
MINISTRY OF
HEALTH
MANAlU IIAUORA
Document 3
Briefing
Public health settings for medium-risk pathway
Date due to MO: 18 November 2021
Action required by:
19 November 2021
Security level:
IN CONFIDENCE
Health Report number: 20212528
To:
Hon Chris Hipkins, Minister for COVID-19 Response
1982
Act
Contact for telephone discussion
Name
Position
Telephone
Maree Roberts
Deputy Director-General, System Strategy <Mobile>
and Policy
Information
Stephen Harris
COVID-19 Policy, System Strategy and
<Mobile>
Policy
Official
Minister's office to complete:
the
□ Approved
□ Decline
□ Noted
□ Needs change
□ Seen
under
□ Overtaken by events
□ See Minister's Notes
□ Withdrawn
Comment:
Released
 Public health settings for medium-risk
Public health settings for medium-risk
Document 3
pathway
Security level:
IN CONFIDENCE
Date:
18 November 2021
To:
Hon Chris Hipkins, Minister for COVID-19 Response
Purpose of report
1.
This briefing seeks your approval on public health settings for the medium-risk pathway
as part of the plan for Reconnecting New Zealanders with the world.
1982
Summary
Act
2.
New Zealand is now entering the next phase as we near a 90 percent vaccination rate
across the country and we shift our Elimination Strategy to a minimisation and
protection approach and adopt the new COVID-19 Protection Framework [CAB-21-MIN-
0421].
3.
Under the new approach - and with increasing vaccination rates - many systems and
processes designed with the goal of stamping out COVID-19 must now
Information be adjusted to
reflect the new goals of minimising the spread of COVID-19 in the community and
protecting those most vulnerable to the disease and ensuring the health system is not
overwhelmed.
Official
4.
This shift in our overall context is also shaping the way we reconnect with the world;
settings for arrivals is adapting to reflect the changing risk. Critically, as part of the
the
Reconnecting New Zealanders strategy, international travellers self-isolating is intended
to become one of the primary ways that people enter New Zealand from early 2022.
5.
This approach for medium-risk travellers will complement low- and high-risk pathways
as part of the risk-based approach
under to international arrivals Cabinet has agreed to adopt.
6.
Even with high vaccination rates domestically and internationally, and a general
reduction in risk of international arrivals transmitting COVID-19, residual risks are likely
to remain for categories of international travel.
7.
For this reason, we will need to implement public health settings and entry requirements
Released
for incoming travellers under medium risk-pathway to reflect and manage the evolving
level of COVID-19 risk posed.
8.
This paper seeks your decision on the public health requirements under the medium-risk
pathway including vaccination, testing and isolation settings.
Briefing: HR 20212528
 Recommendations
Recommendations
Document 3
We recommend you:
a)
Note that opening the border under steps 1 and 2 of the medium-risk
Yes/No
pathway for Reconnecting New Zealanders require consideration of public
health settings to reflect and manage the evolving level of COVID-19 risk
posed
b)
Note that as part of the Reconnecting New Zealanders strategy, international
Noted
travellers self-isolating is intended to become one of the primary ways that
people enter New Zealand from early 2022
c)
Note that recent Hight Court ruling has thrown into question the NZ BORA
Noted
public health justification of the MIQ requirements for New Zealand arrivals
d)
Note that this ruling and expected further legal challenges mean we must
Noted
1982
consider self-isolation for both vaccinated and unvaccinated New Zealand
arrivals
Act
e)
Agree to one of the following options for vaccination requirements for
arrivals under the medium-risk pathway:
i. Allow all returnees regardless of the vaccination status, to go into self-
Yes/No
isolation with 7 days for vaccinated and 10 days for unvaccinated; or
11. Allow all returnees regardless of the vaccination status, to go into self-
Yes/No
Information
isolation except for unvaccinated individuals arriving from higher risk
countries, who will need to go into MIQ
f)
Agree that the current standards for pre-departure testing are continued
Yes/No
under the medium-risk pathway
Official
g)
Note that public health advises that mixed flights do not pose a risk as long
Noted
the
as other checks are in place including vaccination, isolation, and testing
requirements.
h)
Note that to manage risk on arrival, the most effective option would involve
Noted
under
an initial test, either by RAT or PCR
i)
Agree we recommend that a RAT is the most effective test to conduct at the
Yes/No
airport but could pose significant operational challenges
j)
Agree to require self-declaration of previous 14 days travel history for arrivals
Yes/No
under the medium-risk
Released pathway
k)
Agree that self-isolation and quarantine of returnees under the medium risk
pathway will be under the same conditions as for cases and contacts in the
community, and will include:
1. No limitations or requirements on how people travel from their arrival
Yes/No
airport to their location of isolation/quarantine
ii. No limitations on where people undertake self-isolation or who may
Yes/No
be present in the home in the home while a person is undertaking
Briefing: HR 20212528
2

1982
Act
Information
Official
the
under
Released
 Health settings for medium-risk pathway
Health settings for medium-risk pathway
Document 3
Context
9.
New Zealand is now entering the next phase as we near a 90 percent vaccination rate
across the country and we shift our Elimination Strategy to a minimisation and protection
approach and adopt the new COVID-19 Protection Framework [CAB-21-MIN-0421].
10. Under the new approach - and with increasing vaccination rates - many systems and
processes designed with the goal of stamping out COVID-19 must now be adjusted to
reflect the new goals of minimising the spread of COVID-19 in the community and
protecting those most vulnerable to the disease and ensuring the health system is not
overwhelmed.
11. The ongoing Delta outbreak is also part of our changing context in terms of our domestic
1982
risk profile and providing us with community models of care and support.
12. This shift in our overall context is also shaping the way we reconnect with the world;
Act
settings for arrivals is adapting to reflect the changing risk. Critically, as part of the
Reconnecting New Zealanders strategy, international travellers self-isolating is intended to
become one of the primary ways that people enter New Zealand from early 2022.
13. This approach for medium-risk travellers will complement low- and high-risk pathways as
part of the risk-based approach to international arrivals Cabinet has agreed to adopt.
14. Even with high vaccination rates domestically and internationally, and a
Information general reduction
in risk of international arrivals transmitting COVID-19, residual risks are likely to remain for
categories of international travel.
15. For this reason, we will need to implement public health settings and entry requirements
Official
for incoming travellers under medium risk-pathway to reflect and manage the evolving
level of COVID-19 risk posed.
the
16. This paper seeks your decision on the public health requirements under the medium-risk
pathway including vaccination, testing and isolation settings. These settings aim to provide
the base on which specific measures can be built, maintained, and adjusted in response to
developments. It does not address
under operational consideration, which will be subject to
separate advice, including from other agencies.
17. The advice set out in this briefing for the medium-risk pathway ties in with the recent
advice to you on the updated public health risk assessment of current border settings. That
assessment concludes that the risk presented by cases arriving at the border has changed,
and self-isolation is now considered a more proportionate management measure for most
Released
arrivals. This advice on also notes that any transition will need to be carefully managed to
reduce potential impacts on communities and the health system resulting from the risks of
changing from one system to another too quickly.
Expected stages of the medium-risk pathway
18. On Monday 15 November 2021, Cabinet endorsed the approach to Reconnecting New
Zealanders with the World, by opening up the medium-risk pathway in the following steps:
Briefing: HR 20212528
4

a. Step 1 - opening the medium-risk pathway to fully vaccinated New Zealand citizens,
Document 3
residence-class visa holders, and other travellers eligible under our current
restrictive border settings from Australia from 11.59 pm on 16 January 2022
(provided they have been in Australia or New Zealand for the past 14 days);
b. Step 2 - expanding the medium-risk pathway to fully vaccinated New Zealand
citizens, residence-class visa holders, and other travellers eligible under our current
restrictive border settings, from all but higher-risk countries, by 14 February 2022,
with staging if required;
c.
Step 3 - expanding the medium-risk pathway to fully vaccinated foreign nationals
(possibly staged by visa category) by 31 May 2022.
19.
Under step 1, we expect approximately 9,000 arrivals a week. While in step 2, we would
open up to significant extra volumes and a wider lane of risk. However, we envisage that
1982
the same public health settings would manage the risk proportionately.
Timing of reopening will align with domestic settings
Act
20.
To achieve our goals of protecting people and minimising health impacts by containing
outbreaks, we will need to be confident in the effectiveness of the COVID-19 Protection
Framework to manage COVID-19 and protect the vulnerable alongside changes to our
border settings.
21. This includes ensuring that changes to domestic settings, such as the increased movement
Information
across the Auckland boundary, are bedded in before significant changes are made to
border settings.
22.
Health system preparedness must also be taken into consideration as measures to allow
greater freedom of movement, both domestically and across our borders, must not create
Official
undue impacts on the health system s ability to cope. There will be increased pressures in
the next few weeks to manage COVID-19 domestically, including supporting cases to
the
isolate safely at home.
23.
We will learn more about how to support returnees to self-isolate and quarantine more
successfully during an initial period at step 1 that will inform a more sustainable model of
under
self-isolation and quarantine at step 2 and beyond.
Public health requirements for medium-risk pathway
24.
The medium-risk pathway aims to ensure that there are suitable risk mitigations in place for
travellers in line with our
Released minimisation and protection strategy, while also enabling a larger
number of travellers to enter New Zealand. In essence this means detecting as much as
possible infection prior to departure using PDT and using vaccination status as a measure
of protection to guide management of individuals after arrival.
25.
The following section lays out the proposed settings to inform Cabinet advice. We note that
any final settings will be subject to a public health assessment at the time of reopening to
ensure they are proportionate to the level of risk posed.
Briefing: HR 20212528
5
 Holding risk off-shore - pre-departure settings
Holding risk off-shore - pre-departure settings
Document 3
Pre-departure testing will remain a measure to hold risk offshore
26. A negative pre-departure test prior to boarding provides a key layer of protection by
detecting and holding risk offshore.
27. It is recommended that the current standards are continued as we move forward with the
medium-risk pathway. Currently, to enter New Zealand, most travellers are required to have
a negative COVID-19 test within 72 hours of their first international departure. This can be a
PCR, LAMP, or antigen test.
Rapid-antigen test at point of departure has been explored
28. Current options for testing at the point of departure include rapid antigen testing (RAT) and
PCR testing. Rapid antigen testing is a potential tool to enable quicker COVID-19 testing, as
1982
some tests are capable of point of care and community-based application.
29. RATs which usually test anterior nasal swab samples (that can be self-collected,
Act or collected
by a healthcare worker), are able to provide a much quicker turnaround time for individual
tests than most polymerase chain reaction (PCR) tests and have the potential to be
deployed as point of care or self-tests without the need for a laboratory. While these are
highly desirable characteristics, the main disadvantage of RATs is reduced sensitivity when
compared with PCR testing.
30. Rapid antigen test at departure has been explored as a possible option to provide
Information
assurance that a person is not acutely infectious during travel and therefore reduces the
chance of in-flight transmission. Current options require significant oversight, space to
conduct at any volume, and time before results are known. One option, yet to be explored,
might be to conduct any RAT grg-departure, eg in a departure area, while passengers are
Official
held in a confined area for a sufficient period before boarding.
31. However, given the expected volumes,
the there are constraints around feasibility of this
measures, particularly in countries/airports that are not as well-resourced.
Establishing vaccination status
32. If we are to differentiate between
under vaccinated and unvaccinated, it is also critical to define
what we mean by 'fully vaccinated'. The efficacy of different COVID-19 vaccines currently in
use internationally varies. While most vaccines offer protection against severe disease and
illness, some do not appear to offer the same level of protection against infection and
transmission.
33. On 11 November, you
Released agreed that the recognised vaccines for New Zealand's definition of
"fully vaccinated" are any of the Medsafe or World Health Organization Emergency Use
Listing approved vaccines.
34. It is expected that where unvaccinated children under 17 are travelling with adults who are
eligible for the medium-risk pathway, they will enter on the same entry pathway as their
adult guardians.
Vaccination credentials are also a critical consideration
35. Since 1 November, for all non-New Zealand citizen arriving by air must provide proof of
vaccination, in order to enter MIQ. Under this policy a broad approach has been taken for
Briefing: HR 20212528
6

defining what will constitute proof of vaccination, given that additional risk mitigation
Document 3
measures are in place (including testing, isolation and quarantine). This decision reflects a
number of pragmatic and equity-related factors.
36. For the medium risk pathway, we may wish to apply a more rigorous approach, in order to
have greater confidence in the authenticity, integrity and validity of the documentation.
However, if we were only to accept digital certificates in the medium-risk pathway, there
may be unacceptable trade-offs such as NZ BORA and equity impacts for those who were
vaccinated in countries that do not issue digital certificates.
37. Under Reconnecting New Zealanders step 1, we can assume that most returning New
Zea lander citizens and residents entering via Australia will hold a digital vaccination
certificate issued in either New Zealand, Australia, the United Kingdom or one of the other
49 countries who are members of the EU Digital COVID-19 Certificate framework. However,
not all will hold such certification.
1982
38. As the Travel Health Declaration System will not be operational until later in Q1 2022,
assessing vaccination status will need be done in person, by presenting a document to a
border official for checking. This will require manually checking both the pre-departure
Act
test
document and the vaccination document and will have impacts on managing passenger
flow through airports.
39. While needing to have reasonable confidence in the authenticity of vaccination
documentation, it is recognised this is another layer in the COVID-19 protection, and
therefore understanding some level of risk may be acceptable.
Information
Vaccination status of returnees may need to be considered as part of entry requirements
40. In all our previous advice on risk-based pathways under the Reconnecting New Zealanders
framework, the Ministry of Health has recommended that any returnees coming through
the medium-risk pathway should be fully vaccinated with appropriate credentials.
Official
41. However, the public health advice on this issue has shifted: to recommending entry of both
vaccinated and unvaccinated returnees
the through the medium-risk pathway. This is due to
the high vaccination rates domestically, which shifts the risk calculus and puts in question
the public health justification under the New Zealand Bill of Rights Act 1990 (NZ BORA) to
require vaccination as entry requirements.
under
En-route
settings
42. Under the risk-based approach, it is assumed that the risk-profile of travellers on some
flights will be mixed, which may include some vaccinated and non-vaccinated travellers on
the same flight. Additionally, many airlines will not allow non-vaccinated passengers to
board.
Released
43. Based on public health advice, we do not consider that mixed flights pose a risk as long as
other checks are in place including vaccination, isolation, and testing requirements.
Post-arrival settings
44. Public health advice has maintained the value of MIQ for unvaccinated arrivals. The recent
High Court ruling in the Bolton case has not changed this public health rationale, but it is
expected to continue to be tested in the courts. The public health view is that we can
manage the possible risk presented by unvaccinated returnees not just through short-stay
MIQ, but also through other measures, including self-isolation and testing. COVID-19
Vaccination Certificate (CVC) requirements will allow us to buffer the risks presented by
Briefing: HR 20212528
7

unvaccinated returnees, who would be limited in their access to many domestic locations
Document 3
without a eve.
45. We have considered the option of allowing only fully vaccinated returnees to enter through
the medium-risk pathway. This would reduce any infection risk presented by unvaccinated
returnees - which current evidence shows is around three times higher than from a
vaccinated individual. The likelihood of legal challenges referred to above makes this option
less tenable.
46. Therefore, there are two options regarding for vaccination requirements for the medium-
risk pathway:
Option 1 - Allow all returnees, regardless of the vaccination status, to go into self
isolation with 7 days for vaccinated and 10 days for unvaccinated; or
Option 2 - Allow all returnees, regardless of the vaccination status, to go into self
isolation except for unvaccinated individuals arriving from higher risk countries, who
1982
will need to go into MIQ. This is because the residual risk presented by these
individuals is greater than posed by unvaccinated individuals from lower risk places (eg
Act
low-risk Australian states).
47. Should unvaccinated arrivals bypass MIQ we recommend they be required to self-isolate
for 10 days, as opposed to seven days for vaccinated New Zealand arrivals under steps 1
and 2 of the medium-risk pathway.
Arrival settings
Initial testing
Information
48. Point of arrival testing has been considered as an option for an added layer of protection. It
has shown to detect a significant number of cases - previously 60% of cases were detected
through this test but this percentage has dropped more recently. There are a few options
Official
for conducting the initial test:
RAT for point of arrival testing at the airport
the
49. The advantages of RAT are that the test itself is straightforward to perform on an individual.
From the point the swab is collected, it is only 15 minutes before a result can be read. The
Auckland Airport trial has shown that the use of the RAT test is currently not significantly
under
affecting processing rates due to low demand.
50. However, with expected volumes, this will likely change, and it may not be feasible to
conduct this test on every returnee. The delays in conducting the tests and awaiting the
results, plus operational logistics including having sufficient workforce and infrastructure
remains a key concern.
Released
51. Further, the public health perspective is that RAT on arrival is most effective for people that
are highly infectious, so there is some merit in having capability present at the airport to
conduct RAT on arrival for some categories of arrivals, eg those who are unvaccinated or
coming from higher risk places, or who are symptomatic.
52. RAT can be through nasal or mouth swab, or through a saliva sample.
53. Operational agencies support the option of having some RAT capability at the airport that
would allow us to test some categories of passengers when and if needed. It is expected
that all airports have existing provisions to facilitate the option of some RAT testing.
Briefing: HR 20212528
8
 PCR as option for point of arrival testing at the airport
PCR as option for point of arrival testing at the airport
Document 3
54. Alternatively, PCR testing has been considered as an option. However, there are several
constraints, particularly laboratory capacity. Another significant issue is that we lose the
benefit of seeing the results immediately (as we would with RAT) and there is a risk of PCR
picking up historical cases.
PCR as option for testing at Day 0/7
55. Day 0/1 PCR testing is currently being used and remains a reliable option. This could be an
alternative to a test at the airport as the test at the start of the home isolation/quarantine
period.
Verification on arrival at the airport
56. Self-declaration of previous 14 days travel history is recommended.
57. This requirement should remain as we still have the 'very high risk' (VHR) countries
1982
category. Additionally, knowledge of travellers' routes to New Zealand is needed to enable
ongoing monitoring of any potential traveller origin specific risks including the emergence
Act
of new variants.
Self-isolation settings
58. Any domestic settings imposed on returnees will need to align with the shift in our
management of cases and contacts in the community, with self-isolation and self-isolation
now being the default position. As we are no longer generally managing close contacts of
cases in a managed isolation facility, there is a case for treating New Zealand international
Information
arrivals in the same way, because we now consider the risks posed by both groups of
people to be broadly equivalent.
Duration and location for self-isolation and quarantine of returnees
59. In order to facilitate a large and increasing number
Official of travellers is recommended entering
through the medium-risk pathway, a high-trust approach will need to be taken to self
isolation requirements, supported by appropriate
the
, targeted testing. A high-trust approach is
also consistent with the level of public health risk posed by travellers entering through the
medium-risk pathway not being significantly greater than the infection risk from cases in
the community.
under
60. Broadly, and as agreed in the recent joint briefing between the Ministry of Health and the
Ministry of Business, Innovation and Employment [HR 20212434 refers], we recommend
that this includes:
a no limitations or requirements on how people travel from their arrival airport to
their location of isolation; and
Released
b. no limitations or requirements on where people may undertake their self-isolation
or who else may be present in the home while a person is undertaking self-isolation.
However, if a returnee were to test positive, their household contacts would be
required to self-isolate for 7 days (vaccinated) or 10 days (unvaccinated).
61. In line with the management of close contacts of community cases, we also recommend the
duration of self-isolation for returnees coming under the medium-risk pathway to be 7 days
for those who are vaccinated, and 10 days for those who unvaccinated (if they are allowed
to bypass MIQ).
Briefing: HR 20212528
9

62. We recommend that support is traveller-initiated and in-home welfare support for people
Document 3
undertaking their self-isolation is focused on highlighting existing community services to
travellers, with the expectation that they would be 'self-sufficient'.
63. Further consideration will be given to directing travellers towards resources that they can
access through existing community services that can be accessed remotely (eg Healthline).
This mirrors the approach recommended for travellers self-isolating under the current
short-stay MIQ model1•
Testing requirements for self-isolation and quarantine of returnees
64. This period of self-isolation will be supported through appropriate, targeted testing that
will allow us to find cases among the returnees.
65. It is likely that there is a greater risk of transmission for close contacts of community cases,
as compared to returnees. This has implications as to where we target the resources of
discretionary testing.
1982
66. Our recommended testing requirements for returnees who are self-isolat ng would be the
same as we do for close contacts of community cases - day 0/1 test and day 5/6 test. This
Act
will ensure consistency but may mean that resources are diverted from community where
they are needed more.
67. Within these the initial settings, the default for the test would be a PCR. As we move
forward, we may start seeing a transition to more usage of RAT. However, there are
concerns about how effective a RAT may be when self-administered.
Escalation pathway for returnees who test positive
Information
68. We recommend that if returnee tests positive while in isolation, they are expected to
contact Health line and follow the instructions.
Compliance and monitoring requirements will be a high-trust, low touch model
Official
69. Issues of compliance are still being worked through with the relevant agencies.
the
Equity
70.
Those returning to New Zealand should not have to stay in MIQF any longer than is
necessary, if at all, to protect
under the public health of New Zealanders.
71.
However, we need to still take some risk mitigation measures. If a large number of
additional COVID-19 cases are seeded at the border, there is a risk that there may be
some additional health and non-health effects of COVID-19 in the community. We know
that COVID-19 has had a disproportionate health impact on Maori and Pacific
communities as Maori, and younger age groups of Pacific peoples currently have low
Released
rates of vaccination compared with the wider population and could be
disproportionately impacted.
72.
The settings outlined in this briefing will help to ensure that the impacts of COVID-19 in
the community are minimised, and that vulnerable population groups are protected.
1 This approach is for travellers who are self�isolating, and is distinct from health and welfare support that is provided to individuals who test positive for
COVID�19 and are medically assessed as being able to safely and appropriately isolate at home, Such individuals will continue to receive appropriate
support under the care in the community model.
Briefing: HR 20212528
10
 Next steps
Next steps
Document 3
73. This advice will feed into Reconnecting New Zealanders paper going to the Cabinet on 22nd
November 2021 and will subsequently feed into the expected government announcements
relating to the Reconnecting New Zealanders' plan.
ENDS.
1982
Act
Information
Official
the
under
Released
Briefing: HR 20212528
11