POLICY
Elective Patient Journey – Planned Care and Process Management
Policy Responsibilities and Authorisation
Department Responsible for Policy
POLICY
Elective Patient Journey – Planned Care and Process Management
Policy Responsibilities and Authorisation
Department Responsible for Policy
Operational Performance and Support
Document Facilitator Name
Leigh Singers
Sana Maqsood
Document Facilitator Title
Manager – Elective Services
Data Quality Analyst / NPF Project Manager
Document Owner Name
Christine Lowry
Document Owner Title
Executive Director - Hospital and Community Services
Target Audience
Clinical and Non-Clinical Staff
Authorised By
Executive Leadership Team
Date Authorised
Disclaimer: This document has been developed by Waikato District Health Board specifically for its
own use. Use of this document and any reliance on the information contained therein by any third party
is at their own risk and Waikato District Health Board assumes no responsibility whatsoever.
Policy Review History
Version
Updated by
Role
Summary of Changes
01
Sana Maqsood
Data Quality Analyst / NPF Project Manager
Policy rewritten as part of
developing new policy and
guideline system (on intranet) and
under Official Information Act 1982
processes
Released
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DAY OF PRINTING
Page 1 of 38
link to page 5 link to page 5 link to page 5 link to page 6 link to page 6 link to page 7 link to page 8 link to page 8 link to page 8 link to page 8 link to page 8 link to page 9 link to page 9 link to page 10 link to page 10 link to page 10 link to page 10 link to page 11 link to page 11 link to page 11 link to page 12 link to page 13 link to page 13 link to page 13 link to page 14 link to page 15 link to page 18 link to page 18 link to page 18 link to page 18 link to page 19 link to page 19 link to page 19 link to page 19
 POLICY
Elective Patient Journey – Planned Care and Process Management
Contents
1
Introduction ................................................................................................................................................ 5
1.1
Purpose............................................................................................................................................ 5
1.2
Scope ............................................................................................................................................... 5
1.3
Exclusions ........................................................................................................................................ 6
2
Definitions .................................................................................................................................................. 6
3
Policy Statements ...................................................................................................................................... 7
4
Roles and Responsibilities ......................................................................................................................... 8
1982
4.1
Chief Executive Officer / Executive Director - Hospital & Community Services .............................. 8
4.2
Directors, Clinical Directors, and Head of Department .................................................................... 8
Act
4.3
Clinicians ......................................................................................................................................... 8
4.4
Managers ......................................................................................................................................... 8
4.5
Referral Coordination Centre (RCC) ............................................................................................... 9
4.6
Clinical Nurse Specialist (CNS) ....................................................................................................... 9
4.7
Pre-Hospital Preparedness (PHP Team) ...................................................................................... 10
4.8
Clinical Records ............................................................................................................................. 10
Information
4.9
Administration Team Leaders ........................................................................................................ 10
5
Ministry of Health Planned Care Measures ............................................................................................. 10
5.1
Elective Services Patient Flow Indicators (ESPIs) ........................................................................ 11
5.2
Faster Cancer Treatment (FCT) Indicators ................................................................................... 11
Official
5.3
Diagnostics Indicators .................................................................................................................... 11
6
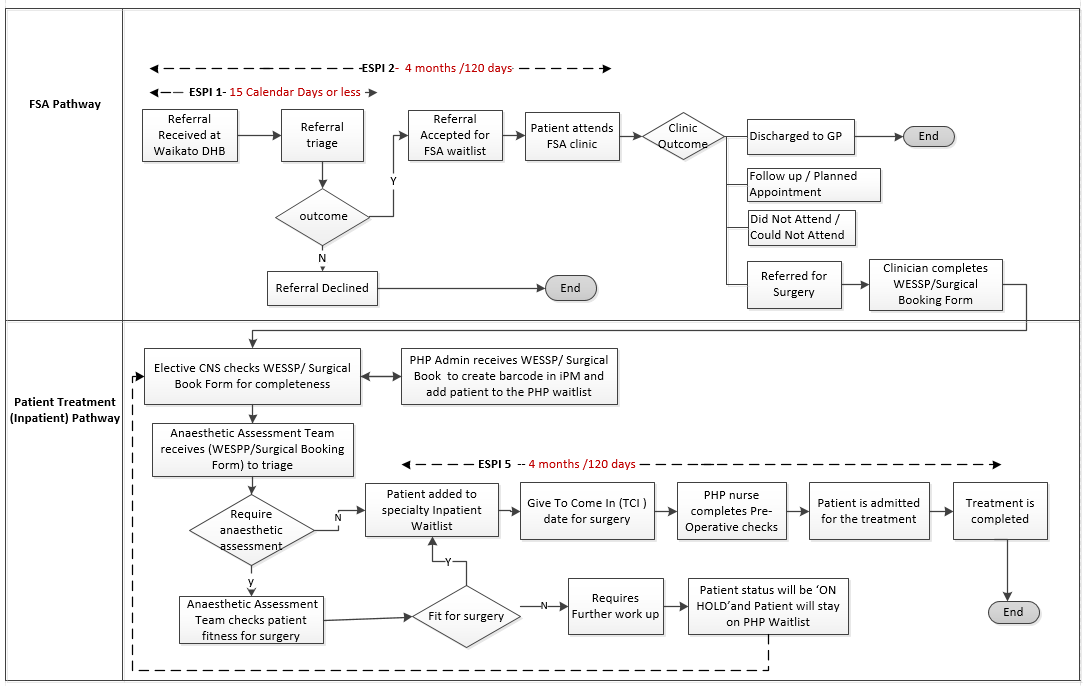
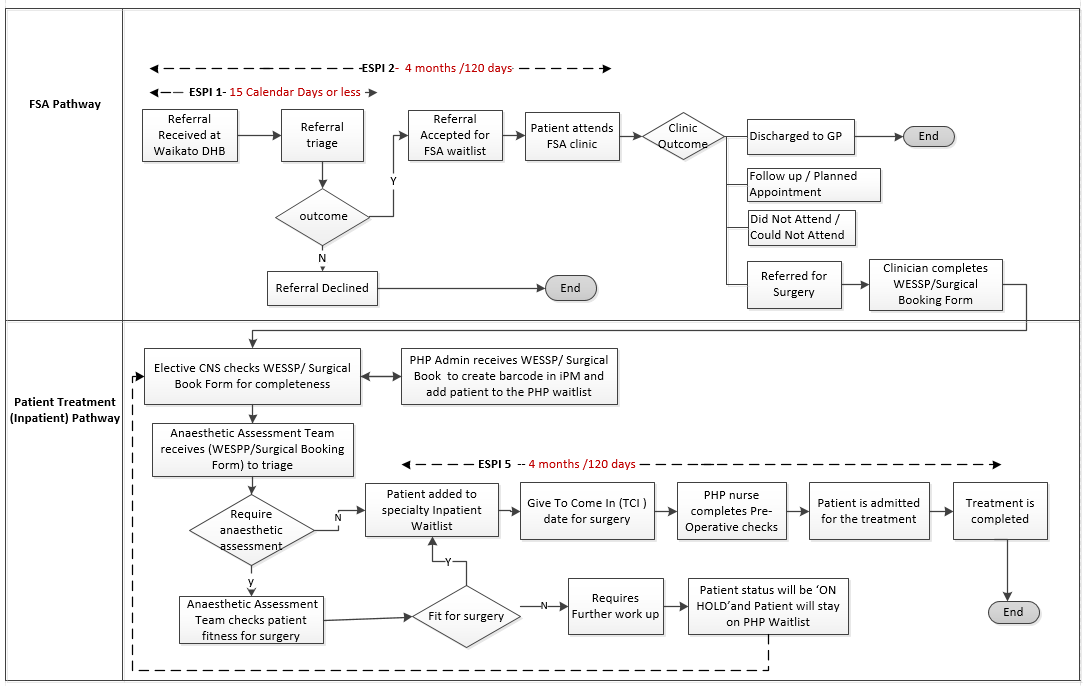
Elective Patient Journey (FSA to the Surgery Completion) - Process Flow Diagram (Non- Cancer) ..... 12
7
Policy Processes ..................................................................................................................................... 13
under
7.1
Referrals Minimum Criteria for GP/Referrers ................................................................................ 13
7.2
Referrals processed by Referral Coordination Centre (RCC) ....................................................... 13
7.3
Referrals processed by the Service ............................................................................................... 14
7.4
Principles for creating iPM Referrals ............................................................................................. 15
7.5
Clinician to Clinician (C2C) Referrals / Internal Referrals ............................................................. 18
Released
7.6
Referrals from One Facility to Another within Waikato DHB ......................................................... 18
7.7
Referrals from other DHB’s / Private Providers ............................................................................. 18
7.8
Patient Opting to go to the private provider ................................................................................... 18
7.9
Direct Access Referrals ................................................................................................................. 19
7.10 ACC injury related Referrals .......................................................................................................... 19
7.11 Non – Eligibility Patient Referrals .................................................................................................. 19
7.12 Management of Open Referrals .................................................................................................... 19
POLICY
Elective Patient Journey – Planned Care and Process Management
Contents
1
Introduction ................................................................................................................................................ 5
1.1
Purpose............................................................................................................................................ 5
1.2
Scope ............................................................................................................................................... 5
1.3
Exclusions ........................................................................................................................................ 6
2
Definitions .................................................................................................................................................. 6
3
Policy Statements ...................................................................................................................................... 7
4
Roles and Responsibilities ......................................................................................................................... 8
1982
4.1
Chief Executive Officer / Executive Director - Hospital & Community Services .............................. 8
4.2
Directors, Clinical Directors, and Head of Department .................................................................... 8
Act
4.3
Clinicians ......................................................................................................................................... 8
4.4
Managers ......................................................................................................................................... 8
4.5
Referral Coordination Centre (RCC) ............................................................................................... 9
4.6
Clinical Nurse Specialist (CNS) ....................................................................................................... 9
4.7
Pre-Hospital Preparedness (PHP Team) ...................................................................................... 10
4.8
Clinical Records ............................................................................................................................. 10
Information
4.9
Administration Team Leaders ........................................................................................................ 10
5
Ministry of Health Planned Care Measures ............................................................................................. 10
5.1
Elective Services Patient Flow Indicators (ESPIs) ........................................................................ 11
5.2
Faster Cancer Treatment (FCT) Indicators ................................................................................... 11
Official
5.3
Diagnostics Indicators .................................................................................................................... 11
6
Elective Patient Journey (FSA to the Surgery Completion) - Process Flow Diagram (Non- Cancer) ..... 12
7
Policy Processes ..................................................................................................................................... 13
under
7.1
Referrals Minimum Criteria for GP/Referrers ................................................................................ 13
7.2
Referrals processed by Referral Coordination Centre (RCC) ....................................................... 13
7.3
Referrals processed by the Service ............................................................................................... 14
7.4
Principles for creating iPM Referrals ............................................................................................. 15
7.5
Clinician to Clinician (C2C) Referrals / Internal Referrals ............................................................. 18
Released
7.6
Referrals from One Facility to Another within Waikato DHB ......................................................... 18
7.7
Referrals from other DHB’s / Private Providers ............................................................................. 18
7.8
Patient Opting to go to the private provider ................................................................................... 18
7.9
Direct Access Referrals ................................................................................................................. 19
7.10 ACC injury related Referrals .......................................................................................................... 19
7.11 Non – Eligibility Patient Referrals .................................................................................................. 19
7.12 Management of Open Referrals .................................................................................................... 19
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 2 of 38
link to page 19 link to page 19 link to page 20 link to page 20 link to page 20 link to page 20 link to page 21 link to page 22 link to page 23 link to page 23 link to page 24 link to page 24 link to page 25 link to page 25 link to page 25 link to page 26 link to page 26 link to page 26 link to page 27 link to page 27 link to page 28 link to page 28 link to page 28 link to page 28 link to page 28 link to page 29 link to page 29 link to page 29 link to page 30 link to page 30 link to page 31 link to page 31 link to page 32 link to page 32 link to page 32
 POLICY
Elective Patient Journey – Planned Care and Process Management
7.13 Management of Duplicate Referrals .............................................................................................. 19
7.14 Management of Non-Contact FSA Referrals ................................................................................. 19
8
Clinical Review and Referral Triage / Prioritisation ................................................................................. 20
9
Referral Notification to GP/ Referrer and Patient .................................................................................... 20
10 Outpatient Waitlist Management ............................................................................................................. 20
10.1 Principles ....................................................................................................................................... 20
10.2 First Specialist Assessment (FSA) Booking – ESPI 2 Start Date.................................................. 21
10.3 Management of Outpatient Clinic – Session Templates ............................................................... 22
1982
10.4 Selection of Patients for Clinic Appointment ................................................................................. 23
11 Clinic Outcome for Outpatient Appointment ............................................................................................ 23
Act
12 Management of Patients not attending the Outpatient Appointment or Surgery ..................................... 24
12.1 Outpatient Appointment - Did Not Attend (DNA) ........................................................................... 24
12.2 Outpatient Appointment - Could Not Attend (CNA) ....................................................................... 25
12.3 Rescheduling Outpatient Appointment- Patient Request (PR) ...................................................... 25
12.4 Rescheduling Outpatient Appointment - Hospital Request (HR)................................................... 25
12.5 Planned Surgery / Procedure - Patient Did Not Attend (DNA) (Adult) .......................................... 26
Information
12.6 Planned Surgery / Procedure Patient Did Not Attend (DNA) (Paediatric) ..................................... 26
12.7 Vulnerable Patients ........................................................................................................................ 26
12.8 Hard to Contact Patient ................................................................................................................. 27
12.9 Change of Patient Address ............................................................................................................ 27
Official
12.10 Transfer between Providers for Elective Surgery .......................................................................... 28
12.11 Transfer of SMO / Clinician for Elective Surgery ........................................................................... 28
13 Management of Hospital Driven Cancellation ......................................................................................... 28
under
13.1 Clinic Cancellation ......................................................................................................................... 28
13.2 Theatre / Procedure Cancellation .................................................................................................. 28
14 Elective Admission including Day Cases ................................................................................................. 29
14.1 Elective Surgical & Procedural Pathway - Key Principles ............................................................. 29
14.2 Patient Assessment to add into Inpatient Waitlist ......................................................................... 29
Released
14.3 Anaesthetic Assessment Process ................................................................................................. 30
14.4 Anaesthetic Assessment Clinic (AAC) ........................................................................................... 30
14.5 Clearance for Surgery .................................................................................................................... 31
14.6 Addition to the Inpatient Waitlist / Waitlist start date (ESPI 5) ....................................................... 31
15 Booking Patient for Surgery or Procedure ............................................................................................... 32
15.1 Surgical Patient’s Booking Order ................................................................................................... 32
15.2 Pre - Operative Nurse Assessment by PHP Team ....................................................................... 32
POLICY
Elective Patient Journey – Planned Care and Process Management
7.13 Management of Duplicate Referrals .............................................................................................. 19
7.14 Management of Non-Contact FSA Referrals ................................................................................. 19
8
Clinical Review and Referral Triage / Prioritisation ................................................................................. 20
9
Referral Notification to GP/ Referrer and Patient .................................................................................... 20
10 Outpatient Waitlist Management ............................................................................................................. 20
10.1 Principles ....................................................................................................................................... 20
10.2 First Specialist Assessment (FSA) Booking – ESPI 2 Start Date.................................................. 21
10.3 Management of Outpatient Clinic – Session Templates ............................................................... 22
1982
10.4 Selection of Patients for Clinic Appointment ................................................................................. 23
11 Clinic Outcome for Outpatient Appointment ............................................................................................ 23
Act
12 Management of Patients not attending the Outpatient Appointment or Surgery ..................................... 24
12.1 Outpatient Appointment - Did Not Attend (DNA) ........................................................................... 24
12.2 Outpatient Appointment - Could Not Attend (CNA) ....................................................................... 25
12.3 Rescheduling Outpatient Appointment- Patient Request (PR) ...................................................... 25
12.4 Rescheduling Outpatient Appointment - Hospital Request (HR)................................................... 25
12.5 Planned Surgery / Procedure - Patient Did Not Attend (DNA) (Adult) .......................................... 26
Information
12.6 Planned Surgery / Procedure Patient Did Not Attend (DNA) (Paediatric) ..................................... 26
12.7 Vulnerable Patients ........................................................................................................................ 26
12.8 Hard to Contact Patient ................................................................................................................. 27
12.9 Change of Patient Address ............................................................................................................ 27
Official
12.10 Transfer between Providers for Elective Surgery .......................................................................... 28
12.11 Transfer of SMO / Clinician for Elective Surgery ........................................................................... 28
13 Management of Hospital Driven Cancellation ......................................................................................... 28
under
13.1 Clinic Cancellation ......................................................................................................................... 28
13.2 Theatre / Procedure Cancellation .................................................................................................. 28
14 Elective Admission including Day Cases ................................................................................................. 29
14.1 Elective Surgical & Procedural Pathway - Key Principles ............................................................. 29
14.2 Patient Assessment to add into Inpatient Waitlist ......................................................................... 29
Released
14.3 Anaesthetic Assessment Process ................................................................................................. 30
14.4 Anaesthetic Assessment Clinic (AAC) ........................................................................................... 30
14.5 Clearance for Surgery .................................................................................................................... 31
14.6 Addition to the Inpatient Waitlist / Waitlist start date (ESPI 5) ....................................................... 31
15 Booking Patient for Surgery or Procedure ............................................................................................... 32
15.1 Surgical Patient’s Booking Order ................................................................................................... 32
15.2 Pre - Operative Nurse Assessment by PHP Team ....................................................................... 32
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 3 of 38
link to page 33 link to page 33 link to page 34 link to page 34 link to page 34 link to page 35
 POLICY
Elective Patient Journey – Planned Care and Process Management
15.3 Removal from the Inpatient Waitlist List ........................................................................................ 33
16 Validation and Active Management of Waitlist ........................................................................................ 33
17 Management Information and Reporting ................................................................................................. 34
18 Monitoring and Audit ................................................................................................................................ 34
19 Associated Documents ............................................................................................................................ 34
Appendix A - Glossary ..................................................................................................................................... 35
POLICY
Elective Patient Journey – Planned Care and Process Management
15.3 Removal from the Inpatient Waitlist List ........................................................................................ 33
16 Validation and Active Management of Waitlist ........................................................................................ 33
17 Management Information and Reporting ................................................................................................. 34
18 Monitoring and Audit ................................................................................................................................ 34
19 Associated Documents ............................................................................................................................ 34
Appendix A - Glossary ..................................................................................................................................... 35
1982
Act
Information
Official
under
Released
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 4 of 38
 POLICY
Elective Patient Journey – Planned Care and Process Management
1
Introduction
1.1 Purpose
POLICY
Elective Patient Journey – Planned Care and Process Management
1
Introduction
1.1 Purpose
This document outlines the Waikato DHB policy, process management and best
practices to be followed by staff to manage the patient’s elective pathway processes
effectively.
This policy is aligned with the Ministry of Health ‘Planned Care’ principles which will
enable Waikato DHB to provide more timely care in the most appropriate settings with
the right workforce, including services that can be delivered in primary care and
community settings.
1982
This policy document will also help to achieve:
A consistent standard for the administrative management of the elective patient
Act
journey.
Auditable data quality that contributes to patient safety.
Timely patient assessment and access to the best treatment options.
Monitoring of referral wait times to ensure equitable access to care for all New
Zealanders.
Transparency and usability of referral wait times to plan services effectively.
Compliance to internal and external performance indicators.
Information
Proactive, concise and timely communication with patient and GP to deliver the best
care.
Compliance with the MOH data collections and KPIs (National Patient flow (NPF),
National Booking Reporting System (NBRS), National Minimum Data Set(NMDS) and
National Non- Admitted Patient Collection(NNPAC)).
Official
Transparency of the service delivery process, equity of health outcomes and
elimination of health disparities.
This policy sets a minimum standard for the Waikato DHB. Services may opt to have
service-specific guidelines that extend the minimum standard outlined in the policy.
under
Where issues arise with the staff not complying with the policy, the issue will be resolved
between the relevant manager and the individual concerned. Failure to reach an
agreement will be referred to the appropriate Director.
1.2 Scope
This policy applies to the elective patient journey that includes elective referrals,
outpatient waitlist, diagnostics/Investigation/Tests, clinic scheduling, and appointment
Released
booking subsequently followed by elective admissions including inpatient waitlist, Day
case Admissions.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 5 of 38
 POLICY
Elective Patient Journey – Planned Care and Process Management
1.3 Exclusions
POLICY
Elective Patient Journey – Planned Care and Process Management
1.3 Exclusions
Management of acute patients except where the event impacts elective services
Management of Henry Rongomau Bennett Centre - Mental Health referrals
Management of community referrals
Management of Te Puna Oranga (TPO) acute referrals
Patient Flow Manager (PFM) referrals
2
Definitions
Abbreviation
Description
1982
ACC
Accident Compensation Corporation
Act
AAC
Anaesthetic Assessment Clinic
BPAC
Best Practices (Electronic Referral System)
CD
Clinical Director
can
Could Not Attend
CNS
Clinical Nurse Specialist Information
CPAC
Clinical Prioritisation Assessment Criteria
C2C
Clinician to Clinician
CRC
Community Referral Centre
Official
CWS
Clinical Workstation System
DHB
District Health Board
DNA
Did Not Attend
under
DTT
Decision To Treat
ES
Elective Surgery
ESPI(s)
Elective Services Patient Flow Indicators
FCT
Faster Cancer Treatment
Released
FSA
First Specialist Assessment
FU
Follow Up
GP
General Practitioner
HSCAN
High Suspicion of Cancer
HO
House Officer
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 6 of 38
 POLICY
Elective Patient Journey – Planned Care and Process Management
IDF
POLICY
Elective Patient Journey – Planned Care and Process Management
IDF
Inter-District Flow
IP–WL
Inpatient Waitlist
iPM
Patient Management System
KPI
Key Performance Indicator
MoH
Ministry of Health
MCC
Meade Clinical Centre
NBRS
National Booking Reporting System
1982
NHI
National Health Index
Act
ncFSA
Non-Contact FSA
NPF
National Patient Flow
OP, IP
Outpatient, Inpatient
PFB
Patient Focused Booking
PHQ
Patient Health Questionnaire
Information
PHP
Pre-hospital Preparedness
PVS
Price Volume Schedule
RCC
Referral Coordination Centre
Official
RMO
Registered Medical Officer
SLA
Service Level Agreement
SBF
Surgical Booking Form
under
SMO
Senior Medical Officer
TCI
To Come In
WL
Waitlist
WESSP
Waikato Elective Surgical & Procedural Pathway
Released
3
Policy Statements
The application and implementation of this policy is the responsibility of all staff that manage
the elective patient pathway and undertake patient administration and clinical activities.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 7 of 38
 POLICY
Elective Patient Journey – Planned Care and Process Management
4
Roles and Responsibilities
4.1 Chief Executive Officer / Executive Director - Hospital & Community Services
POLICY
Elective Patient Journey – Planned Care and Process Management
4
Roles and Responsibilities
4.1 Chief Executive Officer / Executive Director - Hospital & Community Services
This policy will be endorsed by the Chief Executive Officer (CEO) and Executive Director
- Hospital and Community Services.
4.2 Directors, Clinical Directors, and Head of Department
Directors, Clinical Directors, and Division Heads are responsible for ensuring
adherence to this policy, and ensure there are adequate resources for its
implementation.
Work in clinical partnership with the relevant managers to ensure services are
1982
delivered effectively through the promotion of evidence-based practice and
responsive patient-focused care in collaboration with other clinical and non-clinical
Act
services across the DHB.
Each service has a process in place to identify urgent patients waiting on all elective
waitlists. The criteria for booking order could be the highest scoring - longest waiting
or from analysis of their demand to understand what the booking order needs to be.
If a service is consistently receiving clinically inappropriate referrals, it is the
responsibility of the Clinical Director - Strategy Funding and Primary Care to liaise
with external referrers to discuss this matter.
Information
4.3 Clinicians
The elective referrals received at Waikato DHB is required to be triaged within six
working days and within the Ministry of Health guidelines, using National Clinical
Prioritisation Tools / agreed triaging criteria.
Patients attending clinic appointment will be informed about the clinic outcome.
Official
When patient meets the criteria for a surgical procedure, WESPP/Surgical Booking
form will be completed with the required information.
Work collaboratively and in partnership with clinical and non-clinical staff to comply
with policy requirements to manage the elective patient pathway.
under
4.4 Managers
Oversee and co-ordinate adherence to agreed patient administration standards and
processes for the designated Specialty / Service.
Monitor, guide, audit and validate that key standards and processes required for the
safe administrative management of the patient pathway are adhered to and ensure
Ministry of Health compliance timeframes and targets are met.
Released
Monitor and audit internal processes to promote equity of access for Maori and other
vulnerable patient groups.
Monitor the Specialty / Service compliance with the Planned Care Indicators and
other quality and performance standards.
Notify the Operations Director and Clinical Director of any potential risks and issues.
Monitor and manage the designated specialty Inpatient and Outpatient wait list,
suspended list and planned appointments.
Support Ministry of Health initiated projects/data collections.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 8 of 38
 POLICY
Elective Patient Journey – Planned Care and Process Management
POLICY
Elective Patient Journey – Planned Care and Process Management
It is the responsibility of the Manager of each elective service to ensure that
procedures are being booked in the correct order based on wait time and urgency
score.
Provide exception reporting and analysis to the Director (when required) if there are
potential capacity/demand issues.
Conduct the following activities in partnership with the Director, Manager, Clinical
Director, and designated specialty leads:
Manage the service delivery for designated specialty
Quantify the service capacity and forecast the demand
Ensure iPM data compliance to meet the MoH data collection requirement
1982
Alignment between production and funding contracts
4.5 Referral Coordination Centre (RCC)
Act
Ensure referrals received at RCC are processed and notified within timeframes as
outlined in section 7.2 (Referrals processed by Referral Coordination Centre (RCC).
Ensure patient details, address, eligibility status, and GP details are updated. If
patient is not eligible for publically funded health services then send an email to
[email address]
Monitor and communicate ESPI 1 performance with Managers and Clinical Directors.
Communicate RCC performance issues and implication to the relevant service
Information
manager and clinical director.
Perform an audit to verify the referral details recorded in iPM with the information
received in BPAC referral.
If ACC details are provided, enter this information on the referral. If the referral is
likely to be an ACC related or specifies key injury/accident related terminology but it
Official
not flagged as ACC, send an email t
o [email address] to check for
claim information.
Work closely with the Data Quality team to monitor the accuracy and completeness of
the data recorded in iPM.
under
4.6 Clinical Nurse Specialist (CNS)
Monitor and manage the patient journey from the date of referral receipt until the date
treatment is completed.
Triage patients for urgency and is responsible for reviewing the outcome of the
assessment and developing a plan.
Contact ACC team to get the funding approval prior to the patient surgery when ACC
Released
details are not completed by the clinician on the WESPP/Surgical Booking Form.
Provide clinical oversight and advice to the booking team on priority and urgency.
Coordinate the plans and care of the complex patient – this will include vulnerable
patients, patients with special or complex needs, and patients travelling distances.
Proactively manage patients who did not attend (DNA) or could not attend (CNA), or
are identified as high risk of not attending their scheduled appointments.
Weekly/Fortnightly meetings with the anaesthetists to develop management plans for
‘On Hold’ patients.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 9 of 38
 POLICY
Elective Patient Journey – Planned Care and Process Management
POLICY
Elective Patient Journey – Planned Care and Process Management
Monitor and manage the waitlists to ensure there is sufficient capacity to treat patients
within the compliance timeframe. Where constraints are identified this should be
escalated to the appropriate Manager and Clinical Director.
Facilitate and communicate with key clinicians and clinical areas.
4.7 Pre-Hospital Preparedness (PHP Team)
Pre Hospital Preparedness (PHP) admin creates barcode in iPM for WESSP/ Surgical
Booking Form and add patients onto PHP Register (waitlist).
PHP Nurse makes contact with the patient to complete final pre & post-operative
checks for the surgery.
Issues that may impact surgery are to be escalated to the surgical team, anaesthetist
1982
and CNS immediately.
Act
4.8 Clinical Records
Ensure appropriate documentation is prepared and available for the clinic prior to the
patient appointment.
Ensure patient’s medical files and their versions/ volumes are traceable in iPM e.g.
document dispatched date, location and transfers.
4.9 Administration Team Leaders
Support administration staff to adhere to this policy.
Information
Ensure referrals, appointment and clinical priority requirements are met, and are
processed within the agreed timeframes of Planned Care indicators.
Audit and monitor the waitlist to ensure information is correct and accurate, and policy
is followed to comply with the Ministry of Health Planned Care Indicators.
Perform a random audit on iPM referrals to ensure the patient journey is linked with
Official
the correct specialty referral and take corrective actions where necessary.
Guide the administration staff on the process of recording the clinic outcome when
this is not indicated on the clinic outcome form.
Ensure administration staff is aware of the process when a patient is unable to attend
under
the outpatient appointment /surgery. For further guidance, refer to the section
12:Management of Patients not attending for Outpatient Appointment or Surgery)
Monitor waitlist to ensure DNA/CNA and vulnerable patients have appointments
negotiated in a timely manner.
Work closely with the Data Quality team to monitor the accuracy and completeness of
the data recorded in iPM.
Released
Liaise with the Computer Application Training Team to ensure staff is well trained and
are aware of this policy.
5
Ministry of Health Planned Care Measures
Planned Care Initiative previously known as ‘The Elective or Ambulatory Initiative’ services
encompasses medical and surgical activity that is delivered by hospitals. The intention of the
Planned Care Initiative is to take more deliberate steps toward considering these concepts
collectively and in the context of quality of services, service user’s experience and equitable
health outcomes.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 10 of 38
 POLICY
Elective Patient Journey – Planned Care and Process Management
POLICY
Elective Patient Journey – Planned Care and Process Management
As a patient moves through the pathway there are a number of key decisions/indicators
from when the person is referred to the specialist through to when decisions are made
about whether or not assessment, diagnostic and treatment will be given, to the point
when the patient returns to the care of their GP (or primary care provider). These
indicators are measured and reported through the Planned Care Performance
Indicators.
5.1 Elective Services Patient Flow Indicators (ESPIs)
The following key indicators are being used to measure the DHB’s performance of
elective services:
1982
ESPI 1: DHB services appropriately acknowledge and process more than 90% of all
patient referrals in 15 calendar days or less.
Act
ESPI 2: All patients accepted for an FSA should be seen within 4 months of the date of
referral. The goal is no patients wait for more than 4 months for an FSA.
ESPI 5: All patients given a commitment to treatment should receive it within 120 days /
4 months. The goal is to ensure no patients given certainty status remain untreated after
4 months.
The following indicators (ESPI 3, ESPI 6 and ESPI 8) are compiled by the Ministry from
these National Collections: NBRS, NNPAC, NMDS and NPF.
Information
5.2 Faster Cancer Treatment (FCT) Indicators
Definition of first/definitive cancer treatment: First cancer treatment is the first
treatment a person receives for their cancer and includes surgery, radiation treatment,
chemotherapy, targeted therapy, non-intervention management such as active
Official
surveillance, and palliative care. FCT is divided into 62 day indicator and 31 day
indicator for reporting purpose.
The
62 day indicator is 90% of patients are to receive their first cancer treatment (or
other management) within 62 days of being referred with a high suspicion of cancer.
under
(The initial referral needs to be triaged as HSCAN and the patients need to be seen
within two weeks).
The
31 day indicator is 85% and is the maximum length of time a patient should wait
from the date of the decision to treat to receive their first treatment (or other
management) for cancer.
5.3 Diagnostics Indicators
Released
Some indicators are linked with the patients who are receiving the below diagnostics
within required timeframes. For Example, Coronary Angiography, CT scan, MRI scan,
Urgent Colonoscopy, Non- urgent Colonoscopy, Surveillance Colonoscopy.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 11 of 38

 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
6
Elective Patient Journey (FSA to the Surgery Completion) - Process Flow Diagram (Non- Cancer)
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
6
Elective Patient Journey (FSA to the Surgery Completion) - Process Flow Diagram (Non- Cancer)
1982
Act
Information
Official
under
Released
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 12 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
7
Policy Processes
7.1 Referrals Minimum Criteria for GP/Referrers
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
7
Policy Processes
7.1 Referrals Minimum Criteria for GP/Referrers
All elective referrals sent to the Waikato DHB must contain the following minimum
requirements:
o Patient name – Surname, First name
o Patient NHI
o Date of Birth
o Referrer name
o Referrer organisation
o Referrer contact details
1982
o The name of the service to which the patient is being referred
o The name of the facility to which the patient is being referred
o
Act
Suitable clinical information on why the patient is being referred(referral reason)
All referrals will be reviewed by the SMO/ triage clinicians and if referral does not
contain this minimum information, this will be returned to the GP/Referrer as per the
clinician advice.
The referrer should specify any special needs of patients that may include disabilities
or any other requirements including Interpreter, vulnerable patients, hearing
impairment, and any religious or spiritual support.
Waikato DHB expects that when a patient is referred for a procedures/ treatment, the
Information
GP/Referrer deems that the patient is clinically fit, available and eligible for treatment
within 4 months of referral to the DHB.
7.2 Referrals processed by Referral Coordination Centre (RCC)
90% of elective/non-acute referrals are processed by the RCC. RCC staff receives
Official
referrals from internal/external sources through the web based tool known ‘Best
Practice (BPAC)’.
Some referrals are received via paper, email, or letter/fax and are entered into BPAC
to provide a centralised view of the referrals. All BPAC referrals are triaged
under
electronically by the triaging clinician and referral outcome is notified to the GP
electronically.
If a service is not using BPAC system, the RC staff will send the paper referral with a
triage sheet to the service.
RCC staff records all BPAC referrals information into iPM along with the referral triage
and waitlist details as advised by the clinician.
The following medical and surgical services referrals are processed by the RCC staff:
Released
Medical Services
Surgical Services
o Cardiology
o Maxillofacial
o Dermatology-General, Acute, and
o General Surgery - General,
Suspected Skin Cancer
Colonoscopy direct access
o Gastroenterology – General,
o Colonoscopy
Hepatitis C, Colonoscopy direct
o Breast Care
access
o Plastic Surgery – includes Burns
o General Medicine
o Orthopaedics
o Haematology
o Gynaecology
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 13 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
o Respiratory Medicine – General,
o Ear Nose and Throat
Suspected Lung Cancer, Sleep study o Vascular Surgery
o Rheumatology
o Paediatrics Surgery
o Infectious Diseases
o Dental
o Immunology
o Neurosurgery
o Endocrinology
o Ophthalmology
o Paediatric Medicine
o Vascular Surgery
o Pain Management
o Women’s Assessment Unit (Antenatal,
o Renal
Obstetrics)
o Audiology
o Cardiac Procedures - Interventional,
o Physiotherapy
Electro - Physiology and Structural
o Occupational Therapy
Heart Disease
1982
o Hand Therapy
o Child Development Centre
o Oncology
Act
o Older Persons and Rehabilitation
o Mother craft
o Neurology
o Strength and Balance
o Echocardiography
o CRIU(Cardiac and Respiratory Tests)
o Some Nurse Led Services i.e. Leg
Ulcers
Information
RCC staff will action the referrals in an agreed timeframe as given below:
Urgent referrals will be processed within
24 hours of receiving the referral
Non – urgent referrals will be processed within
2 working days of receiving the
referral
The date when a referral is received at the Waikato DHB is the date the clock starts
Official
for ESPI1. Once the referral is triaged and the decision is made to transfer to another
specialty, the clock does not restart; the original date of the receipt of the referral
remains the same.
The RCC staff can amend errors in any referral in iPM. (This excludes referrals
under
created by services, who will have to authorise the RCC separately for any change to
the referral.)
7.3 Referrals processed by the Service
Services may receive patient referrals through the BPAC, paper, email or fax. The
service admin will create an iPM referral to book the patient for the clinic appointment.
Paper referrals will be date stamped on the day of receipt by the organisation. This is
Released
then the official ‘date of referral’ as defined by the Ministry.
The following services are required to comply with these guidelines as their referrals
are not processed by the Referral Coordination Centre(RCC):
Urology
Mental Health
Community Referral Centre (CRC)
Diabetes
Palliative Care
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 14 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
Sexual Health
Radiology
Cardiothoracic
Gynaecology (Only “Termination of Pregnancy (TOPs)”, all other types of
Gynaecology referrals are created by RCC staff).
Some Nurse Led Services
This policy will also be followed to manage the external provider referrals including
Private Practices, Other DHBs.
When a new patient is referred to a specialty and is identified as more suitable to be
managed by another specialty, the patient can be transferred to the care of the
appropriate Specialty. The date of the referral will remain unchanged (i.e. the date of
1982
receipt of referral at the Waikato DHB).
Act
7.4 Principles for creating iPM Referrals
i.
Patient details including address, contact number, residency status and ACC details
(if applicable) must be checked before creating iPM referral. When a patient residency
status is non-resident, the staff will send an email t
o [email address]. When a referral is related to any injury with no ACC details, a query will be sent to
[email address]. This information assists in early identification of
patient eligibility for publically funded health services.
ii.
Referrals are compulsory for all type of patient events/activities created in iPM.
Information
iii. A referral is required to attach with patient journey in the following scenarios:
o When a request of service is made to the hospital by external
providers/GPs/Referrers.
o All inpatient ward and theatre admissions.
o Patient care is transferred from one service to another within the facility.
Official
o Patient care is transferred from one facility to another within the Waikato DHB.
o For all clinic presentations, appointments and contacts .e.g. Direct Attend, Walk-in
Patient, Follow-up, annually follow-ups, post-discharge follow-up, telehealth,
phone consultations.
under
iv. Emergency Department staff will be creating referrals in the following conditions:
o All acute admissions including acute theatre bookings which must have an
associated inpatient admission.
o All non-resident patients presenting in ED.
o ED attendance where the ED discharge is Admit or transfer to the ward.
o Patients are seen in ED and routinely discharged through the transit lounge.
o All ACC patients including failed to wait in ED or referred to the outpatient clinic. ED
Released
staff will not be creating referrals for the non ACC patients referred to the outpatient
clinics.
o ED staff do not create a referral to admit patients in Women’s Health and Mental
Health and Addiction Services.
v. When creating a referral in iPM, the referral is required to contain the following minimum
data requirements:
o Referral received date
o Date on letter
o Referral source
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 15 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
o Referral Reason
o Priority
o Comments – problem/ issue as described in the referral letter
o Referred By
o Referred To – Clinician, specialty and Health Org
o Referral status
o ACC details - if the details are present in the referral
o Outcome tab – GP referred HSCAN, GP referred confirmed status
o Triage Outcome
vi. Record the patient’s ethnicity in iPM if it is provided on referral by the GP/Referrer.
vii. Record the patients’ residency status and country of birth if it is provided by the
1982
GP/Referrer.
viii. Referrals will be created in iPM with one of the following referral reasons:
Act
Referral Reason
When to Use
Assessment
Use when the referrer is requesting for a non-FSA appointment for an
assessment. Maybe a new referral for a patient already receiving treatment,
or a patient recently discharged, but re-referred with the same condition.
May include non-specialist assessments such as nurse assessment,
anaesthetic pre-admission assessment, or allied health.
Information
Emergency
Use for ED referrals by the Emergency Department for acute and elective
Department
patients.
Follow-up
Use when a new Referral is received for a patient currently or recently under
care. Follow up is an assessment type of Referral.
Official
A follow up is a subsequent patient consultation with a registered medical
practitioner of registrar level or above, or a registered nurse practitioner, for
the same condition in the same specialty.
For Advice
Use for situations where the Referrer is not requesting a transfer of care but
under
would like some advice. Most frequently this is the clinician to clinician/GP
and does not include a written plan of care sent to the patient.
FSA
Use when the referral is for patient’s first assessment by a registered
medical practitioner of registrar level or above, or a registered nurse
practitioner for a particular referral (or with a self-referral, for a discrete
episode). The patient receives treatment, therapy, advice, diagnostic or
Released
investigatory procedures within three hours of the start of the consultation.
This could be used when the referrer is requesting the specialist
assessment but the specialist believes that the patient can be managed at
the primary care and intends to manage this referral via non-contact FSA.
Investigation /
The referrer requests a test for the patient. Tests may be community
Test
referred (i.e. referred by a GP or private specialist) or include
investigation/tests for patients who are under treatment by a DHB, either as
an inpatient or outpatient. Investigation/Test is primarily a non-interventional
investigation.e.g. Echo, ETT, Spirometry.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 16 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
An investigation test is performed to investigate the patient's
problem/disease and monitor the severity of the disease to determine a
course of treatment.
Procedure /
A procedure is a discrete therapeutic or diagnostic intervention. Includes all
Treatment
intended elective admissions for a procedure or treatment.i.e.Endoscopy.
Some procedures include diagnostic components, such as a biopsy or
angiography.
ix. A referral will contain one of the following statuses in iPM:
o Awaiting Grading
o Accepted
1982
o Declined
o Diagnostic Required - when clinician advises tests
Act
x. When a clinician advises a necessary diagnostic/ tests (For example, MRI to decide
the referral outcome of either ‘accepted or declined’, the staff wil be following the below
process:
o Select the referral status ‘Diagnostic Required’
o Place the referral onto the diagnostic waitlist and send a notification letter to
GP/Referrer and Patient.
o The clinician reviews the diagnostics/tests results and decides to see the patient in
clinic, the diagnostic waitlist will be removed, referral status will be updated from
Information
‘Diagnostic Required’ to ‘Accepted’, and the same referral wil be used for FSA
waitlist. The process of FSA booking will be followed (refer to section10.2 FSA
Booking – ESPI 2 Start Date).
o When a clinician decides to decline the referral, the referral status will be updated
from ‘Diagnostic Required’ to ‘Declined’ and the referral will be completed with the
Official
completed reason. The clinician will be following the non-contact FSA (ncFSA)
process to notify the referral outcome to GP/Referrer and Patient.
xi. All declined referrals will be marked as completed in iPM with the decline reason and
completed reason.
under
xii. Referral outcome must be notified to the GP /Referrer within 15 calendar days of the
receipt of the referral at the Waikato DHB.
xiii. Services are required to formally document the process of triaging referrals including
triaging clinicians and the criteria to be adhered to. A current copy of this document
will be lodged with the Manager or delegate. Each clinician responsible for triaging
referrals must have dedicated time for this activity scheduled into their timetable.
Released
xiv. Use the correct referral to link the patient elective journey. It is not acceptable to use
referrals from different specialties or hospitals other than the one the patient is being
admitted to.
xv. Once a referral is created for a specialty, this referral should not be overridden/
changed/copied with another specialty referral.
xvi. When a patient is transferred from one ward to another ward within the same facility for
the same problem then the admitting referral will be used to link with the patient journey.
xvii. When a patient is discharged from the ward and requires post-discharge follow-
up in the same specialty clinic, the ward referral will be used to link with the outpatient
appointment.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 17 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
7.5 Clinician to Clinician (C2C) Referrals / Internal Referrals
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
7.5 Clinician to Clinician (C2C) Referrals / Internal Referrals
Clinicians may refer patients to other clinicians /colleagues in different service for
advice/consultation. If a patient is referred and the other clinician identifies a new
condition i.e. a condition not related to the original referral, it may be appropriate to
discharge the patient back to their GP advising of this. (GP can then make the
appropriate referral as required or seek advice from the appropriate specialty) or, in
some circumstances, a specialty to specialty referral may be appropriate within the
Waikato DHB.
For internal referrals, a referral form approved by the relevant service directors (or
delegate) will be completed by the Clinicians. While all efforts will be made to
1982
accommodate individual service needs, services do not have the authority to
generate and use their own referral form.
Act
7.6 Referrals from One Facility to Another within Waikato DHB
When a patient is transferred between facilities for the same problem, the same
referral will be used to link the patient journey.
When a patient is transferred between facilities for a new problem, the admitting
facility will be creating a new referral in iPM.
7.7 Referrals from other DHB’s / Private Providers
There are few cases when a referral is directly sent to the service:
Information
When a patient has been assessed by Waikato DHB specialist at another
DHB/Private Facility and referred to the Waikato DHB for treatment, a new referral
‘Procedure/treatment’ will be created by the Inpatient staff to link with the Inpatient
waitlist.
Official
When a patient has been assessed by a specialist and referred to the Waikato DHB,
this will be processed as a new referral. Fol owing Clinician triage the patient’s referral
may be processed as either requiring an Inter-District Flow (IDF) process (New
Referral - change of Domicile) or Follow Up - this must be discussed with the related
under
specialty Manager for guidance on the appropriate process and action required.
All referrals from other DHB’s wil be processed if the referral is on the correct DHB
Letterhead as per the Inter-District Flow process otherwise the referral will be
declined. An exception exists where the services may have an agreement with the
other DHBs to treat the patient .e.g. oncology, haematology.
Patients can be referred to the Waikato DHB from a private provider at any point
during their treatment pathway. The referral must be processed as a new referral.
Released
When the referral is accepted by the clinician then this will be added to the outpatient
waitlist with the clinical priority and timeframe.
7.8 Patient Opting to go to the private provider
The referral and waiting list for patients who notify Waikato DHB of their decision to seek
private care will be closed from the date of this being advised by the patient, and the GP
notified.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 18 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
7.9 Direct Access Referrals
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
7.9 Direct Access Referrals
Direct Access referrals are managed by RCC and services where primary care clinicians
request for the diagnostic services without an FSA being undertaken .e.g. Colonoscopy.
These referrals will be created in iPM with the referral reason ‘Procedure/Treatment’.
7.10 ACC injury related Referrals
All ACC injury related referral queries will be sent t
o [email address].
When a patient is accepted for the surgery, the request to generate ‘Assessment Report
and Treatment Plan (ARTP)’ will be sent to
[email address] by the
SMO/Clinician.
1982
7.11 Non – Eligibility Patient Referrals
When a patient referral is received and the patient residency status is non-resident, the
Act
staff should send a Non-Residency query at
[email address]. Non-
eligible patients will be suspended on the waitlist until the eligibility criteria is confirmed
by the Eligibility team.
7.12 Management of Open Referrals
When the referral is older than a year from the date of last activity and there is no
current activity or planned appointment attached to it, the referral will be completed in
iPM. This is required to comply with the Ministry of Health directive as described in
Information
the ‘National Patient Flow’ data collection.
A referral will be completed with a reason and will not be re-opened to attach new
activities when the clinical outcome is discharged from the service or treatment is
completed.
Official
7.13 Management of Duplicate Referrals
A referral is a duplicate when both (new & existing) referrals have exactly the same
patient NHI; problem/diagnosis; referral received date and the referrer. Do not load
this referral in iPM.
under
A referral is not a duplicate when both (new & existing) referrals have exactly the
same patient NHI; problem/diagnosis; referral received date but the referrer is
different. Check the existing referral status in iPM and also create new referral with
status ‘2nd Referral for review’ and completed reason ‘Patient current to service’.
7.14 Management of Non-Contact FSA Referrals
The below process will be followed for the ncFSA referrals:
Released
Clinician triages the referral and accepts for ncFSA.
RCC staff record this referral in iPM and place onto ncFSA waitlist.
Clinician dictates a care plan letter or completes the care plan template in BPAC for
the patient and GP (In both cases, the referral needs to be placed onto ncFSA
waitlist).
When clinician completes the care plan in BPAC, RCC staff will create this referral in
iPM and place onto ncFSA waitlist and will remove subsequently with the waitlist
removal reason ‘Treatment completed as ncFSA’.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 19 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
When clinician dictates a care plan for the patient, the booking clerk will be notified
through the email /phone. The booking clerk will remove the patient from ncFSA
waitlist with the removal reason ‘Treated as ncFSA’ and complete the referral. The
booking clerk will be regularly monitoring ncFSA waitlist to ensure patients are being
removed from the waitlist when their care plan has been dictated.
8
Clinical Review and Referral Triage / Prioritisation
When elective referrals are sent to the services for triage, the triage Clinicians/SMO/Nurse will
be completing the triaging process within 6 calendars days of the receipt of the referral in the
service.
Referrals indicated by the GP / Referrer as
Urgent priority, High Suspicion of Cancer,
1982
Confirmed Cancer – must be triaged within one working day of receipt in the DHB.
The triaging Clinician/Nurse is responsible for ensuring that:
Act
The referral is triaged within the Ministry of Health guidelines.
The referral is triaged according to the agreed assessment criteria for triaging.
The triaging of referral is delegated by the triage clinician/nurse to a colleague when leave
is taken and this should be documented on the leave request form or discussed with the
Manager to determine the delegated triage clinician/nurse.
Patients that do not require specialist care or meet clinician threshold for acceptance are
returned to their GP/referrer for on-going monitoring and care.
Information
Referrals outcome will be clearly indicated by the triage clinician/nurse.
When a referral is triaged and accepted then the clinical priority will need to be mentioned
in the referral form.
9
Referral Notification to GP/ Referrer and Patient
Official
Waikato DHB services that are receiving FSA referrals should acknowledge and process
more than 90% of referrals in 15 calendar days or less to meet ESPI 1 compliance.
A referral outcome will be notified to the Patient and GP/Referrer to about the clinical
decision.e.g. Referral is accepted/declined, diagnostics/test required, or will be managed
under
through the ncFSA.
The referral monitoring report ‘NPF_ESPI1 Monitoring Tool 15Day’
should be used by each
service to track the ESPI-1 compliance and to take appropriate actions if required. If you
cannot access the report, send an email to
[email address].
10 Outpatient Waitlist Management
Released
10.1 Principles
All patients who have their FSA referral accepted by the Waikato DHB are entitled to
receive their first specialist assessment (FSA) within four months of the date of the
receipt of the referral in the DHB to comply with ESPI 2.
All services will ensure that session templates for outpatient clinics reflect the correct
balance of FSA/Follow-up slots to meet demand.
Outpatient sessions are required to be booked in accordance with the clinic template.
Any variations to the approved session template will be approved by the Manager.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 20 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
FSA patients will be booked from FSA waitlist using the highest clinical
priority/longest waiting.
Waitlist must be created using the correct referral where there is not an appropriate
referral, create a new referral.
Use the ‘Date Referral Received’ for the ‘Date on List’ when creating an outpatient
waitlist from FSA referral.
FSA, diagnostics, and non-contact FSA must be managed on a separate unique
waitlist.
Where there is an authorised acuity tool, SLA must be in place. The patient should be
booked under the guidance of the clinical team using acuity rating to establish clinical
priority.
1982
Patient flow processes will be managed effectively, in line with the principles of clarity,
timeliness, equity, and fairness.
Act
10.2 First Specialist Assessment (FSA) Booking – ESPI 2 Start Date
Urgent, Priority 1, High Suspicion of Cancer or Confirmed Cancer referrals must
be booked within required clinical priority timeframe under the guidance of the clinical
team.
Non- Urgent patient referrals must be booked in chronological order - from date of
referral i.e. longest wait first). The below table refers to the priority order to waitlist
the patient for FSA.
Information
Priority
Rules
HSCAN
A patient will be offered an appointment within 14 days of
referral receipt date
Cat1
A patient will be offered an appointment within 30 days of
referral receipt date
Official
Cat 2
A patient will be offered an appointment within eight weeks of
referral receipt date
Cat 3-4
A patient will be offered an appointment within four months of
referral receipt date
under
If service is using an acuity tool, patient prioritisation criteria should be documented.
Patients that are older, have young families, or live rurally must have their
appointment discussed by phone.
The booking clerk wil confirm and update the Patient’s demographic details when
contacting the patient. The details include ‘Country of Birth’, Place of Birth’, ‘Ethnicity’,
‘Address’, for patients born in New Zealand, ‘Next of Kin’ (minimum two if possible)
and ‘GP details’ including checking ‘GP address’
Released
The booking clerk must check that the dependent resources entered on the OP
Waitlist or diagnostic waitlist have been completed. If not contact the relevant service
to ensure diagnostic referral has been received and when these will be
completed. Appointments should be coordinated with other tests/diagnostics and or
treatments.
Where staff is unable to book the patient appointment within the required timeframes
they must advise the Manager of the capacity shortfall and be guided as to when to
book the affected patients.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 21 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
Where cancellations of the appointment are initiated by Waikato DHB, patients should
be contacted and offered an alternative appointment at their convenience
acknowledging the clinical priority, compliance and/or target timeframes. This will be
done with advice and agreement of the responsible SMO.
Approved elective services letters and communications must provide appointment
details and associated information. Alternative methods of communication should be
considered for patients who require a different method of communication such as
email, texts.
Re-scheduled and cancelled appointment must be recorded in iPM indicating either
patient or DHB initiated reason.
1982
10.3 Management of Outpatient Clinic – Session Templates
Clinics will be booked in accordance with the session template. The Administration
Act
Team Leader (booking clerks or delegate) is responsible to ensure clinics are
appropriately booked to meet the planned target.
Services are responsible for the accuracy and management of their iPM clinic session
templates.
Services will review their outpatient clinic session templates annually to align with the
agreed contract volumes and workforce availability.
The master schedule describes the plan for the year ahead in a repeating pattern with
the exception of planned interruptions (public holidays etc.).
Information
Changes to the clinic master schedule structure will be agreed and administered by
the relevant service Manager. Once the master schedule is agreed, variations and
cancellations will be managed as follows:
The schedule will be reviewed by the Manager and the relevant service six weeks in
advance and any potential risks or interruptions to the schedule identified and
Official
mitigated.
It will be assumed that all lists or sessions planned to meet the service demands will
be staffed and delivered according to the schedule.
No clinic will be cancelled within two weeks of the date scheduled without the
under
permission of the Director of the Service.
No planned clinic will be cancelled within 72 hours of that clinic date without
permission of the Operations Director at the time a decision is being sought.
Variance to the master clinic schedule (requests outside of agreed plan i.e. additional
clinics) must be negotiated six weeks prior to the change required. Variance to MCC
requests should go to
[email address]
Released
Each service is required to plan for sufficient capacity (FSA clinic slots available in
i.PM) to book all the patients on the FSA waiting list
within the timeframes indicated
when the referral is waitlisted.
Each service is required to ensure that there are enough free (un-booked) follow-up
clinic appointments available in iPM to meet their requirements. This should align
with the service annual Price Volume Schedule (PVS) and/or delivery plan.
If it is not possible to increase capacity for a defined period, this should be escalated
through to the agreed escalation level in each service.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 22 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
Where capacity shortfalls can be predicted (For example, around public holidays) the
service should control annual leave and other arrangements to ensure the continued
delivery of the above timeframes.
10.4 Selection of Patients for Clinic Appointment
Patients who require outpatient appointments will be booked on the following criteria
to ensure equity and to minimise the social disruption in their normal routine:
Older patients (particularly those in rest home care), paediatric patients and patients
travelling (For example, to Hamilton from the Thames, Tokoroa, Taumaranui and
regional) are to be scheduled in the mid to late morning slots in the ‘am’ clinics and
in the first appointment slots for ‘pm’ clinics.
1982
It is expected appointments for the above-mentioned patient groups are discussed
with the patient/parent/caregiver by phone before the appointment is made and
notes made in the comments field.
Act
For the patient from outside of Hamilton, the booking clerk should attempt to
coordinate the appointments of patient waitlisted for more than one appointment
(FSA or follow-up).
FSA that cannot be booked within the required timeframes must be discussed with
the Manager for guidance on actions required.
11 Clinic Outcome for Outpatient Appointment
Information
When a patient attends the clinic, the clinician must record the clinic outcome on the
‘Outcome Form’. This information is mandatory to comply with the Ministry of Health
reporting requirements.
All patients will be informed about the outcome of their clinic attendance before they leave
the clinic.
Official
All clinic outcome forms must be checked on the day of the clinic to ensure urgent actions
are completed on that day. When a clinic outcome is left blank or not completed then the
clinic admin staff will contact the Clinic Nurse/Clinician to know the patient
attendance/appointment outcome. In case of any issues, relevant speciality CNS can be
under
contacted to follow-up on the patient clinic outcome.
Appointment Outcome: Waitlist
When a patient attendance outcome is ‘Waitlist’ which means patient requires
surgery/procedure.
When a clinician advises surgery as a treatment option after an FSA appointment, iPM
outcome should be recorded as ‘Waitlist’.
When a clinician and patient agree surgery is the preferred option of treatment and the
Released
surgery is related to ACC injury, the SMO/Clinician must contact the DHB ACC Team at
[email address] to notify the surgery decision and request an
‘Assessment Report and Treatment Plan (ARTP)’ to be completed for funding prior
approval.
Appointment Outcome: Follow up appointments < 6 weeks:
o Follow up appointments due in less than 6 weeks and not subject to test results will have
the date and time discussed with the patient before they leave the clinic. If this is not
possible then the patient should be contacted as soon as possible to ensure the new
appointment date/time meets their needs.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 23 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
Follow up appointments subject to test results and/or Planned Follow-ups > 6 weeks:
o Patients seen in the clinic and require a follow-up appointment will either be:
Booked for a follow-up appointment with the patient directly on the day of the
outpatient appointment (designated specialities with specific follow up timeframes) by
the outpatient reception staff. All follow up appointments are to be managed by the
relevant specialty team under the guidance and direction of the Manager /
Administration Team Leader.
Booked for an urgent follow-up appointment by phone (where possible) under the
guidance of the clinical team.
Added to a ‘Planned follow-up appointment’ list according to the follow-up
appointment timeframe under the guidance and direction of the CNS and
1982
Administration Team Leader to ensure bookings are made within the required
timeframe, with appropriate dependent resources available.
Act
Follow up appointments will be booked under the guidance of the clinical team, using
the
‘Follow-up appointment report’ to ensure follow-up appointments are booked or
planned within the required timeframe requested by the discharging clinician.
Appointment Outcome: Discharged/Treatment Completed
o When a clinician decides to discharge the patient from the service with no follow-up. The
appointment outcome will be marked as ‘Treatment Complete’ and the relevant referral
will be completed in iPM with an appropriate completion reason.
12 Management of Patients not attending the Outpatient Appointment or Surgery
Information
Patients identified as high risk of non-attendance should be proactively supported to attend
their appointments. Where appropriate referrals should be made to Waikato DHB Kaitiaki,
Public Health Nurse, K’aute Pasifika or Whānau Ora providers either prior to scheduled
appointment or following a missed appointment, or for difficult to contact patients.
Official
Every free text entry in iPM must start with a date, comment and user name. E.g. 10/05/15
called the patient to offer surgery date of 10/06/15 but the patient declined – maqsoosa.
12.1 Outpatient Appointment - Did Not Attend (DNA)
under
A patient is classified as DNA if they did not attend the outpatient clinic appointment and
there was no communication before the appointment.
HSCAN and confirmed cancer DNA must be rebooked as per Clinician / CNS
guidance.
The appointment maker must contact the patient by phone to negotiate a new
appointment day/time.
Released
FSA DNA status must be entered in the
waitlist comment and DNA reason must be
recorded in iPM under appointment outcome.
When a patient is DNA on follow-up appointment, the DNA reason will be recorded in
iPM under appointment ‘Comments’.
The patient’s GP/Referrer should be notified each time a patient fails to attend the
appointment.
If a patient DNA’s an appointment for a second time, the clinician will review the
referral and clinical notes prior to the end of the clinic and indicate the required action
on the clinic outcome form.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 24 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
The patient can be discharged back to the care of their GP/Referrer having first
ensured that:
the appointment was clearly communicated to the patient
discharging the patient is not contrary to their best clinical interest
the clinical interests of vulnerable patients are protected
the responsible Clinician has been consulted
12.2 Outpatient Appointment - Could Not Attend (CNA)
A patient is classified as CNA if they did not attend the outpatient clinic appointment
and there was a communication before the appointment. This is considered as
Cancellation in iPM.
1982
HSCAN, Priority 1 and Confirmed Cancer patients to be discussed with the relevant
clinical team and Administration Team Leader / Manager.
Act
The outpatient admin staff will negotiate the reschedule appointment with the
patient/caregiver within priority and compliance timeframe.
When the FSA reschedule date is negotiated outside of the compliance timeframes,
the waitlist comment should be updated to indicate appointment date was due to
patient advising the clinic they could not attend (CNA). The Administration Team
Leader / Manager must be informed when the compliance time frame will not be met.
12.3 Rescheduling Outpatient Appointment- Patient Request (PR)
Information
When a patient requests to reschedule the planned appointment, a new appointment
date should be discussed with the relevant clinical team, Administration Team Leader
/ Manager.
Schedule the reschedule appointment within the clinically indicated priority and
compliance timeframe. Official
If the FSA reschedule is negotiated outside of the compliance timeframes the waitlist
comment must be updated to indicate appointment date was at Patient Request (PR).
12.4 Rescheduling Outpatient Appointment - Hospital Request (HR)
under
HSCAN, Priority 1 and Confirmed Cancer to be discussed with the authorised service
requesting the hospital reschedule.
Consideration should be given to travel, urgency and patients identified as high risk or
vulnerable when rescheduling the appointment.
The Outpatient Booking Clerk will contact the patient/caregiver to advise the
cancellation of the appointment and reason via the patients chosen method of
contact.
Released
The Outpatient Booking Clerk will at the time of advisement of cancellation to
patient/caregiver negotiate new FSA appointment within clinically indicated priority
and compliance timeframe.
If the FSA reschedule is negotiated outside of the compliance timeframes the waitlist
comment must be updated to indicate appointment date was due to Hospital
Reschedule (HR). The Administration Team Leader / Manager must be informed
when the compliance time frame will not be met.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 25 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
12.5 Planned Surgery / Procedure - Patient Did Not Attend (DNA) (Adult)
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
12.5 Planned Surgery / Procedure - Patient Did Not Attend (DNA) (Adult)
If a patient fails to attend their planned elective procedure /surgery admission an
attempt should be made (by the area they were expected to present too) to contact
them immediately to find the reason. The outcome tab on the ‘Admission Offer (TCI)’
must be completed with the outcome date, outcome reason, and any relevant notes.
The waitlist start date must remain the same.
Urgent, Priority 1 and High Suspicion of Cancer, Confirmed Cancer patient DNA’s
must be immediately discussed with the CNS for guidance with the rebooking
process. Consideration should be given to the barriers to attending and what support
can be provided to resolve this. The patient GP and relevant service CNS should be
contacted to assist with coordination.
1982
Paperwork (For example, WESPP/Surgical Booking Form) is returned to the CNS or
nurse coordinating the care. They should contact the patient to negotiate a new date.
Act
If a patient fails to attend their planned elective procedure /surgery admission a
second time the CNS / coordinating health care professional will discuss with the
responsible SMO / clinician. The clinician will review the referral and clinical notes.
Where the patient is discharged back to the GP/Referrer, both the GP/Referrer and
patient (and referring clinician, if different), must be informed by the responsible
SMO/clinician by letter.
12.6 Planned Surgery / Procedure Patient Did Not Attend (DNA) (Paediatric)
Information
Where a paediatric patient fails to attend their planned elective procedure /surgery
admission an attempt should be made (by the area they were expected to present
too) to contact them immediately to find out the reason. The outcome tab on the
‘Admission Offer (TCI)’ must be completed with the outcome date, outcome reason,
and any relevant notes. The waitlist start date must remain the same.
Official
Paperwork (For example, WESPP/Surgical Booking Form) is returned to the CNS /
nurse coordinating the care. They should contact the child parents/carer to negotiate
a new date.
If a paediatric patient fails to attend their planned elective procedure /surgery
under
admission a second time the CNS / Coordinating Health Care Professional will
discuss with the responsible SMO / Clinician.
The paediatric patient’s GP/Referrer or health provider and/or public health nurse
should be contacted when a paediatric patient fails to attend a planned
surgery/procedure event, in addition to direct contact with the patient’s parent or legal
guardian prior to rescheduling. Consideration needs to be given to barriers to
Released
attending and support required in resolving these.
12.7 Vulnerable Patients
It is essential that patients who are vulnerable for whatever reason identified at the point
of referral and their journey actively supported by a coordinating health care professional
and other support. This group of patients includes:
Patients with intellectual disabilities
Patients with physical disabilities or mobility problems or who require special support
or assistance during attendance
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 26 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
Children – known support attendance needed, clinical acuity or complexity or unable
to contact and Māori, Pacific of other ethnicities living in New Zealand deprivation
index 9 or 10(quintile 5).
A patient who requires an interpreter
People with dementia living alone
Patients with cognitive problems.
Patients reliant on others to attend hospital (For example, patients in residential care
or reliant on carers to transport them).
All relevant information must be recorded in iPM to ensure that when selecting a
patient for admission, their needs are identified and appropriate arrangements are
made.
1982
Any additional needs should be considered when negotiating appointments for
patients under these criteria.
Act
To avoid social disruption and ensure equity of access and attendance to these
patient groups specific focus should be given to
negotiation of appointments to suit the patients’ needs
contacts made based on the patient preferred method
coordination of (multiple) appointments where possible or procedures/surgeries
where the patient requires more than one surgery
Contact Enduring Power of Attorney (EPOA) as appropriate.
Information
12.8 Hard to Contact Patient
A patient who is unable to be contacted by phone on the information provided in iPM
will have the following attempts made to contact them
failure by phone or text message after three attempts (message left as able)
Official
contact the person named as next of kin
contact GP/Referrer and/or other health providers to check current contact detail or
establish the best method of contact
refer to Waikato DHB Kaitiaki, appropriate CNS, Public Health Nurse or K’aute
under
Pasifika, Whānau Ora providers.
send a 10-day letter requesting the patient make contact.
When a patient cannot be contacted, then the patient’s information will be provided by
the booking clerk/CNS to the responsible SMO/Clinician for decision to discharge the
patient and return the patient to the care of their GP is removed from waitlist and a
letter will be sent to both the patient and their GP/Referrer by the responsible
SMO/Clinician.
Released
Urgent, Priority 1 and High Suspicion of Cancer, Confirmed Cancer patient - a referral
should be made to the appropriate CNS to provide support.
Paediatrics - a referral should be made to public health nurse to provide support.
12.9 Change of Patient Address
A patient’s address and other contact details should be checked and updated as
required on every contact with Waikato DHB to ensure that their details are up-to-date
Patients who change their address to the outside of Waikato DHB domicile whilst
waiting for Elective admission should not be disadvantaged by the change in
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 27 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
circumstances. Their waiting time may need to be adjusted if they have not advised
the DHB and do not respond to a TCI or validation letter/ contact. Otherwise, the
patient will be referred to the domiciled DHB.
If the patient cannot be contacted, then the patient’s information wil be provided to
the responsible SMO/clinician for the decision to discharge the patient and return the
patient to the care of their GP.
12.10 Transfer between Providers for Elective Surgery
Transfers to and from other providers must be managed with the consent of the patient
and responsible SMO /clinician.
1982
12.11 Transfer of SMO / Clinician for Elective Surgery
On occasion, patients may be offered to have their surgery /procedure performed by
another SMO/clinician within the same specialty.
Act
Where a patient declines the offer, it would be acceptable to select waitlist booking
status ‘Planned’ in iPM until the date that the patient’s requested surgeon is available. It
should be fully explained to the patient so that they will wait longer.
13 Management of Hospital Driven Cancellation
A hospital initiated cancellation is when a patient is given an appointment date/time to
attend the hospital and then the hospital chooses to change this time. Under this
Information
definition, a ‘move’ or ‘rebooking’ is a cancellation.
13.1 Clinic Cancellation
If Waikato DHB cancels a clinic or pre-anaesthetic assessment appointment the patient
must be re-appointed in the next available appointment slot and in accordance with
Official
clinically indicated priority and compliance timeframes. Urgent, Priority 1 patients are to
be scheduled immediately and under the guidance of the clinical team.
13.2 Theatre / Procedure Cancellation
under
Once a TCI (to come in) date has been agreed with the patient, the date must not be
cancelled within one week without approval by the Manager or delegated authority.
All patients who have their surgery cancelled for non-clinical reasons within 72 hours
require the approval of the Operations Director.
All patients who have their surgery cancelled for non-clinical reasons on the day of
admission will be offered a binding date within 28 days, and/or within clinical priority
and/or compliance timeframe. A date should be agreed with the patient on the day of
Released
cancellation, where possible.
All theatre session cancellations (less than 6 weeks) must be authorised by the
Manager and Clinical Director in discussion with the Operations Director.
Urgent, Priority 1 and High Suspicion of Cancer, Confirmed Cancer patient
cancellations by the hospital must be discussed with the Manager and approved by
the Operations Director.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 28 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
14 Elective Admission including Day Cases
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
14 Elective Admission including Day Cases
This policy applies to all patients who are waiting for and will be admitted for a surgical
procedure, as an inpatient or day case on an elective or planned basis. The policy outlines
how the Waikato DHB will communicate with patients and plan their admission within clinical
priority and maximum compliance timeframe (ESPI 5).
Some health specialities are being reported in ESPI 5 as per the Ministry’s requirement.
However, this policy applies to all health specialities to ensure that patients are seen within the
compliance timeframes.
14.1 Elective Surgical & Procedural Pathway - Key Principles
1982
Coordination of the patient journey is the responsibility of the Clinical Nurse Specialist
(CNS). They are the primary point of contact for the patient. When the service does
not have a CNS, the responsibility remains with the referring SMO/Clinician.
Act
When a patient and clinician agree surgery is the preferred treatment option, the
decision will be noted on the Clinic Outcome Form.
The WESSP/ Surgical Booking Form will be completed with the CPAC score.
When a patient does not meet the clinical threshold, they must be informed of the
outcome.
When a patient meets the clinical threshold, they need to complete the ‘Patient Health
Questionnaire’.
Information
The required documentation i.e. WESPP /Surgical Booking Form (inclusive CPAC
score and Procedure code) and Patient Health Questionnaire must be completed
prior to a patient being added to the inpatient waitlist. Procedure information should
match the CPAC score assigned for the specialty.
The clinician will complete the patient ACC details including ACC claim number on
Official
the WESPP /Surgical Booking Form if patient injury/surgery is related to ACC.
Pre-admission assessment and anaesthetic review are considered to be an integral
part of the patient’s admission. The policy is to ensure that assessment starts at the
point the decision to treat is taken i.e. at the start of the waiting time. However, some
under
patients may also require assessment within a month prior to admission.
14.2 Patient Assessment to add into Inpatient Waitlist
The required documentation i.e. WESPP /Surgical Booking Form (inclusive CPAC
score and Procedure code) and Patient Health Questionnaire will be sent to the
Elective CNS to check for completion.
The completed documentation (WESSP/ Surgical Booking Form and Patient
Released
Questionnaire) is forwarded to the Pre Hospital Preparedness (PHP) admin.
Urgent (Priority 1) patients will be barcoded in iPM and added to the PHP waitlist
within 48 hours.
Non-urgent patients will be barcoded in iPM and added to the PHP waitlist within 72
hours.
When patient’s ACC details are not completed on WESPP/Surgical Booking Form by
the Clinician/SMO, the Elective CNS/relevant SMO team will contact ACC team to get
the funding approval prior to the patient surgery.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 29 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
The patient WESPP /Surgical Booking Form will be triaged by the Anaesthetic
Assessment team. The triage outcome will result in;
The patient being cleared as fit to proceed for surgery and do not need to be seen by
the Anaesthetic Assessment team. These patients will be placed onto specialty IP
waitlist.
The patient requiring further assessment to establish fitness for surgery. These
patients will be added to the Anaesthetic Assessment outpatient waitlist.
Patient referred for ‘Local Anaesthetic (LA)’ surgery do not require Anaesthetic
Assessment (AA) by Anaesthetist. These patients will be placed onto specialty IP
waitlist.
Patients identified on the WESPP/Surgical Booking Form as suitable for outsourcing
1982
and triaged by the appropriate Elective CNS can be sent to an external provider after
anaesthetic assessment.
Act
14.3 Anaesthetic Assessment Process
A patient requires ‘General Anaesthesia’ for the surgery needs to be assessed by the
Anaesthetic Assessment (AA) team as fit for surgery before being added to the
inpatient waitlist.
The pre-anaesthetic assessment process should be completed within 4 weeks for a
routine patient without complications.
Urgent, Priority 1 patients are to be scheduled immediately and under the guidance of
Information
the CNS and clinical team.
If following an anaesthetic assessment, a patient is deemed unsuitable to proceed to
surgery, this must be clearly communicated to the responsible CNS and
SMO/Clinician by Anaesthetist team.
The Anaesthetic Assessment team assesses the patient’s fitness for surgery and
Official
assessment can be conducted via phone call, clinical notes review or clinic
appointment.
14.4 Anaesthetic Assessment Clinic (AAC)
under
Patients with significant co-morbidities/suspicious symptoms and/or undergoing more
complex surgery will need further assessment and are required to attend a pre-
anaesthetic assessment clinic appointment with a nurse and/or an anaesthetist, this
should take place within 4 weeks of addition to the Anaesthetic Assessment waitlist.
Urgent, Priority 1 patients are to be scheduled within one week and under the
guidance of the clinical team and elective CNS.
Released
If a patient attending a speciality clinic for an FSA need surgery within 2 weeks and
meets the criteria set by AAC , the CNS can arrange a ‘walk-in’ appointment’ in AAC
on the same day, this is accommodated where resources allows.
If a patient requires onward referral to another service, or is pending the outcome of
investigation/assessment to determine if the patient will proceed to surgery (i.e. a
decision point) the patient is listed as ‘On Hold’ on the AAC waitlist returned to the
care of CNS to coordinate the patients journey.
The CNS meets weekly/fortnightly with the anaesthetists to discuss management of
for ‘On Hold’ patients.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 30 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
All patient interactions will be lodged in iPM comment field starting with a date,
comment and user name e.g. 10/05/15 called patient to offer surgery date of 10/06/15
but the patient declined - maqsoosa
14.5 Clearance for Surgery
Once the patient is signed off as fit for surgery by the Anaesthetic team, the
WESPP/Surgical Booking Form is returned to the CNS within 24 hours.
The CNS will move patient from the PHP register/waitlist.
The Inpatient Booking Clerk will add the patient to the appropriate speciality waitlist.
On the date it is confirmed that a patient is to be added to the inpatient waitlist, the
patient must be fit for admission, available and willing to proceed within the next 120
1982
days/4 month (ESPI 5 -clock starts).
14.6 Addition to the Inpatient Waitlist / Waitlist start date (ESPI 5) Act
Services where the patient requires Anaesthetic Assessment prior to surgery, the
Inpatient waitlist start date will commence from the date the patient has received
anaesthetic clearance as being fit for surgery.
Services who are not using Anaesthetic Assessment, the waitlist start date is
‘decision to treat’ or when a patient is cleared as fit for surgery.
Urgent, Priority 1 patients must be placed onto the Inpatient waitlist on the same day
as receipt of waitlist documentation (WESPP/Surgical Booking Form).
Information
Non- urgent patients will be added to the Inpatient waiting list within two working days
of receipt of the waitlist documentation forms (WESPP/Surgical Booking Form).
All patient details recorded on the WESPP/Surgical Booking Form must be checked
against information recorded in iPM and updated, where applicable.
Patients who are available and fit for elective procedures or treatment within four
Official
month timeframe will be assigned Procedure type ‘Normal’ on the inpatient waitlist.
Procedure types - Staged, Planned and Surveillance flags are used to identify
patients who are to receive an elective procedure outside the required six month
timeframe
(For definitions, please refer to Appendix).
under
Active Review status will be selected for those patients whom elective surgery is
considered to be the best option for their care, but where the service is not available
within the current capacity; and there is a realistic probability that the patient will be
able to be offered treatment in the near future (e.g. within 10-12 month). Patients in
Active Review are the patients who would next receive treatment if provider capacity
increases.
Released
Note: Priority scores are an indicator of clinical acuity and are not to be altered unless
authorised and documented by an appropriate clinical person and the hard copy of
the referral grading sheet or waitlist booking to surgery form amended and signed (or
documented by a clinician through the e-triage/e-referral process). Procedure code
should be relevant for the CPAC score for the specialty.
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 31 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
15 Booking Patient for Surgery or Procedure
15.1 Surgical Patient’s Booking Order
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
15 Booking Patient for Surgery or Procedure
15.1 Surgical Patient’s Booking Order
The waiting list or ‘Assured and Unbooked ESPI 5’ Report will be used to select
patients from the report for surgery, based on clinical priority and time waiting.
Confirmation should be provided in writing of the TCI date and appointment details.
Patients are treated in accordance with their clinical priority; clinically non-urgent
patients are managed on a “next in turn” (chronological) basis and within the ESPI 5
compliance time 120 days / 4 month.
Urgent, Priority 1 patients must be scheduled under the guidance of the CNS in
conjunction with the clinical team. If required documentation/information has not been
1982
completed for an Urgent Priority 1 patient this must be immediately discussed with the
Manager of elective services or relevant service Manager.
Act
Patients should be given at least two weeks’ notice of their TCI (to come in) date and
offered at least two dates. Where available, patients can be offered earlier dates e.g.
when there are available theatre dates within three weeks, however, patients will
have the right to decline without any impact on their waiting times.
If a Clinician leaves Waikato DHB, any patient waitlisted under their name must be
transferred to the lead consultant or another clinician as advised by the Manager.
If at the time of being offered a surgical treatment or procedure and the patient wishes
time to consider, this will be discussed by the listing SMO/clinician to call the relevant
Information
CNS within one month to check if they wish to proceed. The patient will have a
procedure type ‘Planned’ on the waitlist until the date they wish to proceed with the
surgery, this should be within the one month timeframe.
15.2 Pre - Operative Nurse Assessment by PHP Team
Official
The completed theatre list should be provided to the PHP team at least seven days
prior to the date of surgery for routine non-urgent patients.
Additions to a list (For example, as result of a sick patient being replaced) are to be
provided to the PHP nurse immediately following confirmation of the TCI.
under
Issues identified by the PHP nurse that may impact surgery are to be escalated to the
surgical team, case anaesthetist and CNS immediately and documented in WESPP
and Clinical Workstation System (CWS).This should include an inability to make
direct contact with the patient.
Consideration should be given to the barriers to attending and what support can be
provided to resolve these. The patient’s GP /Referrer and Community services may
Released
be contacted to assist with coordination of their hospital stay.
The PHP nurse completes the final check prior to surgery, ensuring patient
readiness. The patient is contacted to ensure they are fit and well for surgery,
instructions regarding arrival time, NBM (Nil by Mouth) time and medication
amendments are given to the patient.
Pre-op preparation is explained and sent out to the patient. For example, bowel prep,
chlorhexidine wash.
Checks are made that pre- operative blood tests and x-rays are complete if not these
are arranged. This is an opportunity for patients to ask questions about their hospital
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 32 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
stay and ensure they have transport and, plans in place to minimise delays at
discharge. Pre and Post-operative information is given to the patient regarding their
stay in hospital.
15.3 Removal from the Inpatient Waitlist List
The patient and their GP/Referrer must be informed in writing (iPM letter or dictated) by
the responsible SMO/clinician (or delegate) of all decisions that result in the removal of
the patient from the inpatient waitlist and/or discharge back to the care of the
GP/Referrer.
Patients may be removed from the waiting list without treatment for several reasons:
Intended treatment is no longer required (patient or clinician advised). 1982
The patient has moved out of the area and opted to transfer to their domiciled DHB.
The patient has personal circumstances that prevent acceptance of offer date for the
Act
foreseeable future.
The patient has not attended an agreed TCI date and efforts to contact the patient
have failed.
The patient has cancelled a TCI date more than twice (providing it is not contrary to
their best clinical interest and patient circumstances have been acknowledged)
Clinician review completed and the patient must be discussed with the Managers.
The patient is not fit for admission, not available or unwilling to proceed or unable to
contact the patient.
Information
If following pre-anaesthetic assessment clearance and waitlist, there is a change in a
patient’s condition that may result in them becoming unfit for surgery, the CNS wil
liaise with the surgeon and
Anaesthetist to establish the priority of treatment.
When a patient requires onward referral to another service, requires more than four
Official
weeks to be optimal for surgery, or
When the outcome of investigation/assessment is pending to determine the patient’s
fitness to proceed with the surgery (i.e. a decision point). In both cases, the patient
should be removed from the inpatient waitlist and returned to ‘on hold’ under the case
under
management of the CNS, or discharged back to the GP depending on the level of
intervention required.
The reason for removal must be recorded on the system and in the medical/clinical
notes.
Patients who advise the CNS that they do not wish to proceed with surgical treatment
will be referred back to their responsible SMO/clinician with a view that the patient
should be discharged to the care of their GP/Referrer. The patient will be removed
Released
from the waitlist.
16 Validation and Active Management of Waitlist
It is the responsibility of the Manager to ensure ongoing weekly review, administrative
validation and clinical validation of all waiting lists and suspend lists.
Suspend lists must be reviewed weekly by the appropriate specialty nurse co-ordinator
and/or Manager to ensure validation of the list. All actions taken must be recorded in the
Suspend List Comments in iPM. (All clinical decisions/actions must be recorded in Waikato
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 33 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
DHB system by the clinical team (e.g. Peri-operative Nurse
Co-ordinator).
A clinical validation process must be undertaken on a weekly basis of all patients who are
deferred/suspended for medical reasons by the clinical team (e.g. Peri-operative nurse
coordinator).
The Administration Team Leaders are responsible for ensuring appropriate and accurate
data entry and update of patient details on the ‘Current Waiting List Report’ under the
guidance of the Manager.
If a clinician leaves Waikato DHB, any patients under their care will be transferred to the
lead consultant or another clinician as advised by the Manager.
1982
17 Management Information and Reporting
The Business Analysts will make available a wide range of detailed and summary
Act
information/reports to the management and Managers in the DHB to help manage and monitor
performance against internal and external KPIs, using relevant Waikato DHB systems.
18 Monitoring and Audit
Managers and the Data Quality team will monitor and audit patient management processes in
iPM and will work closely with stakeholders where any issues/ opportunities for improvement
are identified.
19 Associated Documents
Information
Referral Coordination Centre (RCC) Manual
Waikato DHB Outpatient Clinic Manual
iPM Referral Process & Business Rules
Ministry of Health - Planned Care Strategic Approach (ESPIs)
Official
Waikato DHB
Electronic Result Acknowledgement: The Responsibilities of Senior Medical
Officers and the Delegation of Authority to Resident Medical Officers policy (Ref. 1452)
Operational Policy Framework 2018/2019
Ministry of Health - Bowel Screening pilot monitoring indicators
under
Ministry of Health- Faster Cancer Treatment indicators
Ministry of Health NZ; NBRS for Elective Treatment Guide (January 2015), Guide to NBRS
Procedure flags (June 2016), Guide to Active review (June 2016)
Ministry of Health ‘Common counting standards 2013-14final_Jan2017’
Equity of Health Care for Māori: Framework
https://www.health.govt.nz/system/files/documents/publications/equity-of-health-care-for-
Released
maori-a-framework-jun14.pdf
National Collections Glossary
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 34 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
Appendix A - Glossary
Acute Admission (AC)
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
Appendix A - Glossary
Acute Admission (AC)
Acute Admission - An unplanned admission on the day of presentation at the admitting healthcare facility.
Admission may have been from the emergency or outpatient departments of the healthcare facility or a
transfer from another facility.
Referenc
e: https://nsfl.health.govt.nz/purchase-units/common-counting-standards-2013%E2%80%9314
Admission Offer (TCI- To Come in) Date
This is the date the patient is told to arrive at the hospital for elective inpatient admission. This may be the
same as the date of the procedure but may also be prior to the date of the procedure.
Arranged Admission (AA)
1982
A planned admission where the admission date is less than seven days after the date the decision was made
by the specialist that this admission was necessary; or the admission relates to normal maternity cases of 37
to 42 weeks gestation delivered during the event. These maternity patients will have been booked into the
Act
admitting facility (national collections).
Referenc
e: https://nsfl.health.govt.nz/purchase-units/common-counting-standards-2013%E2%80%9314
Booking date
The date on which a patient is offered a (future) date of attendance at the hospital. This can be for an
outpatient appointment or inpatient episode. It is mandatory that a letter must have been posted to the
patient within 24 hours of the booking date informing the patient of their attendance date.
BPAC (Best Practice) System / Electronic Referral System
Information
Best practice Decision Support is a web-based system that is designed specifically to support general
practice in the management of a patient’s health through screening, risk assessment, management and
referral.
Cancellation (Patient initiated)
To be used where the DHB is made aware that the patient has chosen to receive the service in a non-
publicly funded environment (i.e. Insurance or self-funded). This reason should only be used after
Official
Prioritisation. Reference
: https://www.health.govt.nz/publication/national-patient-flow-file-specification
Clinician to Clinician (C2C) referrals
This is a type of elective referral where a hospital clinician requests a transfer of care to, or consultation with,
another hospital clinician. These are classified as new referrals. Note, C2C stands for Clinician to Clinician.
under
Day Case Patient
A patient admitted for healthcare with a length of stay three hours or more but less than one day, regardless
of intent. Day case events will have the same event start and end date. This term is synonymous with ‘same
day patient’ and ‘short stay event’.
Reference: National Collections Glossary
Did Not Attend (DNA)
A patient is classified as DNA if they did not attend the outpatient clinic appointment and there was no
Released
communication before the appointment. If there was communication, this is a cancellation.
Referenc
e: https://nsfl.health.govt.nz/purchase-units/common-counting-standards-2013%E2%80%9314
Direct attend
A direct attend outpatient is one where the patient comes directly to an outpatient clinic without a prior written
referral being received in the hospital and there is not an available clinic session.
Elective Admission (WN)
Elective admission is a planned admission where the admission date is seven or more days after the date
the decision was made by the specialist that this admission was necessary.
Referenc
e: https://nsfl.health.govt.nz/purchase-units/common-counting-standards-2013%E2%80%9314
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 35 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
First Specialist Assessment (FSA)
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
First Specialist Assessment (FSA)
An FSA is a patient’s first assessment by a registered medical practitioner of registrar level or above, or a
registered nurse practitioner for a particular referral (or with a self-referral, for a discrete episode). The
healthcare user receives treatment, therapy, advice, diagnostic or investigatory procedures within three
hours of the start of the consultation. Service is provided in ward and/or designated outpatient clinic or by
telehealth. Excludes ED and outpatient attendances for pre-admission assessment/screening (National
Collections).
Referenc
e: https://nsfl.health.govt.nz/purchase-units/common-counting-standards-2013%E2%80%9314
Inpatient (IP)
A patient admitted for healthcare. Includes day case (same day) events. Includes patients who are
transferred from another healthcare facility, and or inter-departmental transfers (statistical discharge between
specific health specialities) within the same facility. For events reported with an event end date before 1 July,
1982
2013 the definition of ‘inpatient’ included ‘where the intention at admission was that it would not be a day
case event’. Reference: National Collections Glossary
Inpatient Length of Stay
Act
The time in days between admission to hospital ‘X’ and discharge, death or transfer from hospital ‘X’, minus
leave days from hospital ‘X’.
Reference: National Collections Glossary
Multi-disciplinary Clinics
A multidisciplinary clinic constitutes of a mix of clinicians meeting with a patient together to provide an
assessment, for example where an oncologist, surgeon and allied health specialist are present at the same
appointment for the treatment of a cancer patient.
Referenc
e: https://nsfl.health.govt.nz/purchase-units/common-counting-standards-2013%E2%80%9314
Information
National Booking Reporting System (NBRS)
The National Booking Reporting System (NBRS) is a national collection that contains information by health
specialty and booking status on how many patients are waiting for treatment (elective surgery), and how long
they have had to wait for before receiving treatment.
Reference:
https://www.health.govt.nz/search/results/National%20Booking%20Reporting%20System
Official
National Collections Annual Maintenance Programme (NCAMP)
The National Collections Annual Maintenance Programme (NCAMP) is an annual project in order for the
Ministry of Health to meet its statutory obligation of delivering information from the Ministry’s national
collections. NCAMP requires DHBs to initiate changes to their PMS. This covers NMDS data.
Reference
:https://www.health.govt.nz/search/results/NCAMP%202020%20changes%20to%20the%20Nation
under
al%20Collections
National Minimum Dataset (NMDS)
The NMDS is used for policy formation, performance monitoring, research and review. It provides statistical
information, reports, and analyses about the trends in the delivery of hospital inpatient and day-patient health
services both nationally and on a provider basis. It is also used for funding purposes.
Referenc
e:https://www.health.govt.nz/search/results/National%20Minimum%20Dataset%20%28hospital%20events%29
National Non-Admitted Patient Collection (NNPAC)
Released
The National Non-Admitted Patient Collection is a national collection of non-admitted (outpatient and
emergency department) activity, which was introduced 1 July 2006.
Referenc
e: https://www.health.govt.nz/publication/national-non-admitted-patient-collection-file-specification
National Patient Flow (NPF)
The NPF collection will provide information on the patients referred for specialist services, the outcome of
referrals and the time it takes to patients to access care. This collection will contribute to the better-integrated
care so that patients can receive the most appropriate services, in the right setting and in a timely way to
improve overall health outcomes. It will capture the outcome of the referral decision so that the demand for
services and whether it is being appropriately met can be better understood. It will connect related patient
referrals and activities to provide a complete view of the patients' secondary care.
Referenc
e: https://www.health.govt.nz/publication/national-patient-flow-file-specification
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 36 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
Non-Contact FSA (NC FSA)
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
Non-Contact FSA (NC FSA)
A review is undertaken of patient records and any diagnostic test results by a registered medical practitioner
of registrar level or above, or a registered nurse practitioner. The original referral should only be generated
after a face-to-face contact by the referrer. A written plan of care is developed for the patient and provision of
that plan and other necessary advice is sent to the referring clinician and the patient. The non-contact FSA
does not include the triaging of referral letters. The patient should not be present during the assessment.
Referenc
e: https://nsfl.health.govt.nz/purchase-units/common-counting-standards-2013%E2%80%9314
Nurse Led Outpatient Clinic Definition
Assessment, treatment, education and/or management clinics led by a nurse specialist for specialist groups
of clients.
Referenc
e:https://nsfl.health.govt.nz/purchase-units/common-counting-standards-2013%E2%80%9314
1982
Outpatient (OP)
An outpatient is a patient who receives a preadmission assessment, or a diagnostic procedure or treatment
at a healthcare facility, and who is not admitted, and the specialist’s intent is that they wil leave that facility
Act
within three hours from the start of the consultation. When patients receive a general anaesthetic they are
deemed not to be outpatients. All outpatients are elective.
Reference: National Collections Glossary
Procedure Types
o
Normal
This is the default for all procedures that are not assigned Planned, Staged or Surveillance.
o
Planned
A planned procedure is a procedure that is intentionally delayed, where the delay in treatment is for medical
Information
reasons and lasts for more than six months from the decision to treat.
o
Staged
A staged procedure is the second (and any subsequent) in a series of procedures that must be performed in
a sequenced order.
o
Surveillance
Official
A surveillance procedure type is used when the patient requires an ongoing series of routine surveillance
procedures. The surveillance procedures are provided at regular (i.e. annual or longer) intervals to assess
health status.
Reference:
https://www.health.govt.nz/system/files/documents/publications/nbrs-file-specification-v4.4.pdf
under
Referral
A referral is a request to shift patient care from primary care to secondary/tertiary care. The actual transfer of
responsibility is recorded by (usually) a change from one status to another or a change of responsible
clinician. The request may precede the assumption of responsibility by some time, the difference being the
waiting time.
A written document, from a medical professional, requesting a patient be assessed for, or receive hospital
services. All elective referrals must be entered into iPM so an electronic record exists of the paper
equivalent.
Released
Note: elective referrals are divided between GP referrals and Internal or C2C referrals.
Responsible Clinician
For the purposes of this policy the responsible clinician is the person who has overall clinical responsibility for
the healthcare provided to the patient/client. This may be the Senior Medical Officer, midwife, nurse, Mental
Health and Addictions Service key worker, psychologist, physiotherapist, occupational therapist, dietician,
social worker, speech language therapist, other Allied Health workers.
For patients/clients admitted under the Mental Health (Compulsory Assessment and Treatment) Act 1992, the
term responsible clinician is legal y defined by this Act, as ‘the clinician in charge of the treatment of that
patient.’
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 37 of 38
 POLICY
Elective Patient Journey – Planned Care Policy & Process Management
Walk-in Patients
POLICY
Elective Patient Journey – Planned Care Policy & Process Management
Walk-in Patients
When a clinician has agreed to see the patients in the clinic. All walk-in services are acute and a session is
currently available.
1982
Act
Information
Official
under
Released
Doc ID:
6270
Version:
01
Issue Date:
1 OCT 2021
Review Date:
1 OCT 2024
Facilitator Title:
Data Quality Analyst / NPF Project Manager
Department
Op. Perf. And Support
IF THIS DOCUMENT IS PRINTED, IT IS VALID ONLY FOR THE
:
DA
Y OF PRINTING
Page 38 of 38