Position Description
Position Title
Position Description
Position Title
Occupational Therapist/Case Manager
Service Group
Adult Community Mental Health & Addictions Service
Team
Adult Community Mental Health Sector Team
Reports to
Clinical Co-ordinator (ACMH)
Direct Reports
Team Leader
Authority Level
N/A
Issue Date
September 2018
Approved By
The Bay of Plenty District Health Board
The District Health Board’s fundamental purpose is to work within the resources allocated to
it, to improve, promote and protect the health of the whole population within its district, and
to promote the independence of people with disabilities.
Vision:
Healthy, thriving communities.
Mission:
Enabling communities to achieve
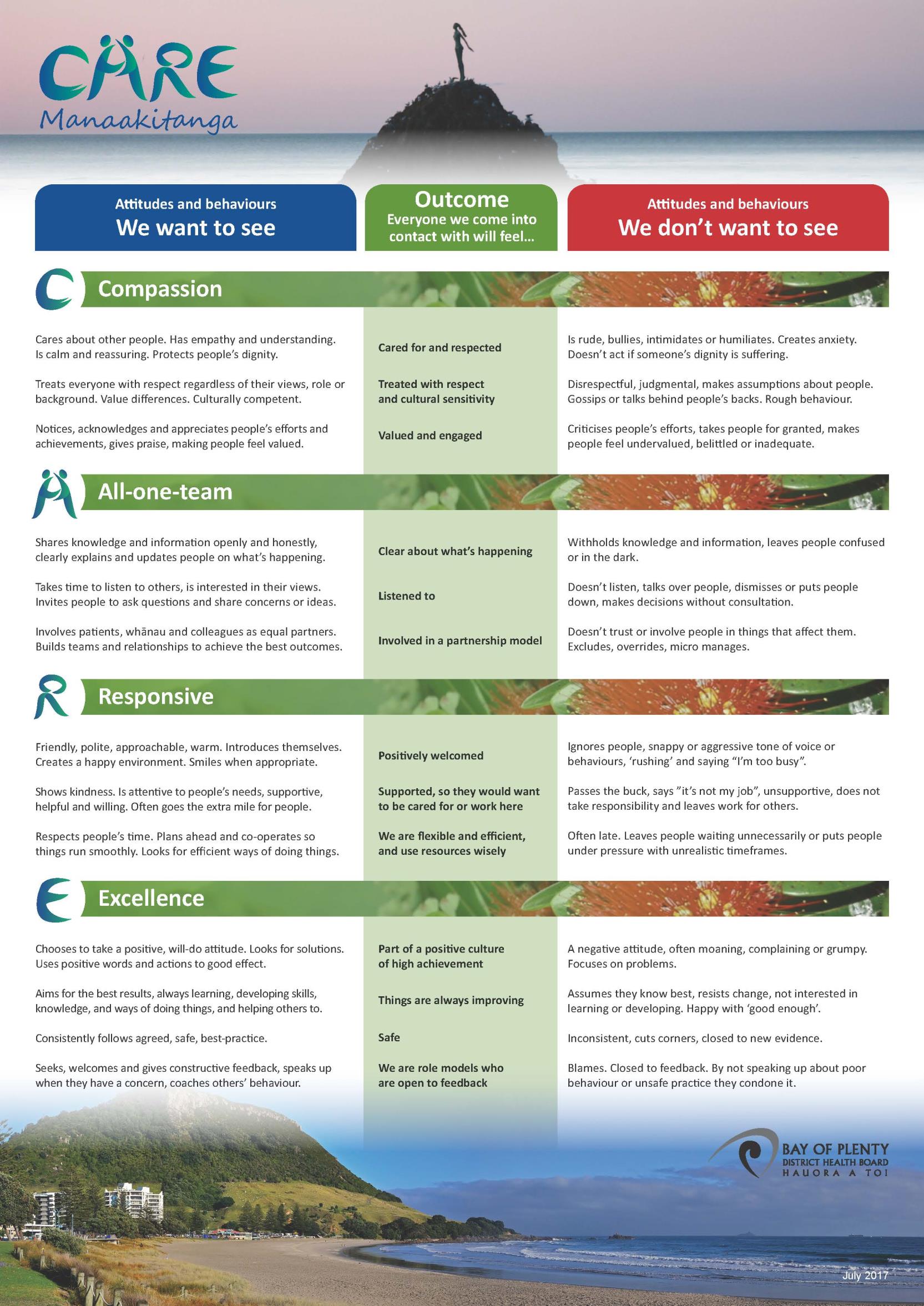
Our Values: Compassion,
All-one-team,
Responsive,
Excellence
under the Offical Information Act 1982
The Bay of Plenty District Health Board (BOPDHB) is committed to the Treaty of Waitangi
principles of Partnership, Participation and Protection, and to meaningful engagement in
decision-making with Tangata Whenua at strategic, operational and service levels.
Delivering this commitment is through: the implementation of our He Pou Oranga Tangata
Whenua Determinants of Health framework: respect for and promotion of our Kawa and
Released
Tikanga Māori; ensuring cultural safety; seeking to eliminate disparities in health between
Māori and Non Māori.
All staff have a part to play in this commitment.
Primary Purpose
The Occupational Therapist/Case Manager is employed to provide safe, effective client
centred intervention using professional knowledge and skills in accordance with the Bay of
Plenty District Health Board (BOPDHB) policies and protocols.

Occupational Therapy practice in adult community mental health will integrate timely
assessment and management of new referrals into the sector and new referrals and time
limited therapeutic interventions with a recovery focus. The case management role includes
but is not limited to:
Clinical responsibility for a designated caseload
Comprehensive assessment and risk assessment
Collaborative treatment planning and management of risk
Response to crisis
The provision of therapeutic interventions with a focus on recovery
Facilitation of transfer of care to the primary sector when treatment goals are met.
Case management of clients with a dual intellectual disability and mental health issue.
Key Responsibilities
Outcomes
1982
1. Cultural Safety
Care is individually focused and planned
in regard to ethnic, cultural, religious and
Act
other needs
Demonstrates a commitment to and
active understanding of the Treaty of
Waitangi and its application within Mental
Health to improve Maori health status
Demonstrates awareness of the impact
of own cultural background, attitudes and
values
Information
Demonstrates awareness of the impact
of own cultural background, attitudes and
values
Demonstrates the cultural and spiritual
Offical needs of service users are met with
sensitivity
including
those
of
family/whanau and significant others.
the Demonstrates that consultation occurs
with Maori Service providers in relation to
care for service users as appropriate
Attends
relevant
Treaty
of
under
Waitangi/Bicultural training as arranged
via BOPDHB
Released
 Key Responsibilities
Outcomes
2. Professional Responsibility
Key Responsibilities
Outcomes
2. Professional Responsibility
Adheres to professional standards of
practice
and
acknowledges
that
competent practice is influenced and
reinforced
through
membership
of
appropriate professional bodies
Is aware of legislation that impacts on
mental health care delivery and service
user rights and practices within legal
boundaries. This includes but is not
limited to the Mental Health (Compulsory
Assessment and Treatment) Act 1992;
the Privacy Act 1993 (Health Information
Privacy Code 1994); Protection of
1982
Personal and Property Rights Act 1988,
and the Health and Disability (Safety)
Act, 2001; Health and Safety at Work
Act
Act, 2015
Considers ethical issues in treatment
planning and contributes an ethical
perspective to decision-making
Demonstrates
knowledge
of,
and
accesses
policies
and
procedural
guidelines that have implications for
Information
clinical care
Has a clear understanding of the
principles
of
delegation
and
accountability and seeks advice and
support appropriately.
Offical
Demonstrates accountability for directing,
monitoring and evaluating service that is
the
provided
by
occupational
therapy
students and others
Actively engages in and effectively
utilises
clinical
supervision
and
under
offers/provides this to clinical staff within
the Mental Health Service as appropriate
and as per the Mental Health Service
Clinical Supervision Policy.
Maintains an up-to-date knowledge of
care/treatment/research in the area of
mental health and occupational therapy
Released
and ensures that practice is evidence-
based
Completes and maintains MH&AS Core
competencies
via
the
in-service
programme.
Maintains BOPDHB and Mental Health
Service mandatory certifications and
additional clinical skills relevant to area
 Key Responsibilities
Outcomes
3. Clinical Practice
Key Responsibilities
Outcomes
3. Clinical Practice
Utilises the clinical process to assess,
plan, implement and evaluate care and
maintains professional practice standards
in assessing, planning, implementing and
evaluating ongoing care for all service-
users,
actively
engaging
with
and
providing
support,
education
and
assistance to families/whanau and care-
givers.
Demonstrates the ability to manage the
environment by assessing risk factors,
identifying and implementing strategies to
maintain own safety and the safety of
1982
service-users and others
Demonstrates a flexible approach and
ability to cope with changing situations.
Act
Undertakes a timely comprehensive and
accurate
occupational
therapy
assessment using suitable assessment
tools to inform goals for intervention and
or provisional diagnostic formulation
Engages in robust ongoing assessment
and management of risk
Information
Develops individual treatment plans in
collaboration with service-users and their
families/whanau that reflects the issues
identified at assessment
Incorporates discharge planning as part
Offical of the overall care strategy, including
relapse
planning
and/or
advance
the
directives, and/or appropriate referrals to
internal/external agencies
Makes clinical judgements based on
current
evidence-based
knowledge,
under
research and reflective practice.
Demonstrates
competence
in
implementing therapeutic strategies eg.
Cognitive
Behavioural
Therapy
and
Occupational Therapy models of practice
Plans and prioritises workload.
Presents
health
information
and
Released
education
to
service-users
and
families/whanau in a sensitive manner
that is readily understood
 Key Responsibilities
Outcomes
4. Interpersonal Relationships
Key Responsibilities
Outcomes
4. Interpersonal Relationships
The principles and practice of partnership
are
incorporated
in
all
facets
of
assessment, intervention, treatment and
care.
Establishes,
maintains
and
concludes
therapeutic
interpersonal
relationships with service-users and their
families, and demonstrates effective
communication with colleagues.
Incorporates authentic therapeutic use of
self
and
interpersonal
and
micro-
counselling skills
Supports the personal autonomy and
resourcefulness of service-users and
1982
their families and encourages their
participation as partners in care
Works and communicates effectively as a
Act
member of the multi-disciplinary team,
demonstrating individual responsibility
and accountability.
Demonstrates an ability to manage
conflict constructively
5. Inter-professional Health Care and Collaborates with the multi-disciplinary
Information
Quality Improvement
team, and the wider community, to
facilitate care delivery and demonstrates
a commitment to the principle of
continuous improvement at a service and
personal level.
Offical
Demonstrates ability to present referrals
and crisis/acute cases for discussion at
the
the daily MDT meeting concisely, with
attention to all relevant information, and
participates in decision-making.
Establishes and maintains networking
under
relationships
with
GPs,
relevant
government and community agencies,
and provides consultation as necessary
Contributes to service development and
involves target group[s] in the planning,
provision and monitoring of services
Released
Demonstrates continuous commitment to
quality improvement initiatives
Provides guidance and support to
students, new graduates and Occupational
Therapists new to the clinical area
 Key Relationships
Internal
External
Key Relationships
Internal
External
Clinical Director/DAMHS
NGO’s and other agencies
Business Leader MH&AS
GP’s and Primary Health
Nurse Leader and Allied Health Leader,
Organisations
MH&AS
Service Users and their families/carers
Regional Maori Services
Consumer Advisor and Family/Whanau
Advisor
Mental Health & Addiction Services staff
Person Specification
1982
Essential
Desirable
Act
Qualifications Current Registration and Annual Postgraduate qualification with a
Practicing Certificate with OT
mental health focus
Board of NZ
Experience
Demonstrate sound knowledge
A minimum of 2 years clinical
and understanding of mental
experience in a mental health
illness and risk assessment in
inpatient or community setting
relation to community mental
Competence in comprehensive
health care
assessment, risk assessment
Information
Cultural awareness and safe
the use of the mental status
practice
examination and problem
Clinical skills in engagement,
formulation
de-escalation, conflict resolution Experience of working within
Offical
and problem solving
teams
A current clean motor vehicle
Experience of working with
driver’s licensethe
clients with dual intellectual
Knowledge of relevant
disability and mental health
legislation including Mental
issues.
Health (Compulsory
Assessment and Treatment) Act
under
1992, Privacy Act 1993, Health
& Disability Act, Health
Practitioners Competency
Assurance Act and the NZ
Health Strategy (Te Tahahu; Te
Kokiri).
Released
Attributes
Demonstrates a commitment to
Computer literate
quality
Demonstrates excellence in
Demonstrates flexibility and
micro-counselling skills
adaptability
Able to develop role in response
Ability to discuss and negotiate
to client needs
management plans with
Demonstrates a commitment to
clinicians
post-registration study and
Excellent communication skills
professional development
and interpersonal skills.
Able to prioritise work
requirements .

Values
Demonstrates behaviours
consistent with the BOPDHB
values
You agree
to demonstrate flexibility and a willingness to perform a variety of tasks to
promote and support BOPDHB initiatives.
You are required to meet the Health and Safety at Work Act 2015 requirements as set out in
the BOPDHB Health and Safety policies and protocols. This includes completing
successfully any health and safety training provided by the BOPDHB.
You are required to maintain a standard of health which will allow for the performance of all
duties and functions of the position. All BOPDHB sites are smokefree environments.
1982
Act
Philosophy and Strategic Guidance
The service embraces an eclectic approach which includes the Recovery, Strengths Based
and Crisis Resolution approaches as well as the Choice and Partnership Approach which is
service user and family/whanau centred
. It is expected that the incumbent will be guided by
the service philosophy, relevant legislation, national strategic service directives, policies,
protocols and annual business plans. This position description includes the seven Real Skills
as identified by the Let’s get Real framework.
Information
Health Practitioners Competence Assurance Act 2003
1.
You are required to maintain your current competency based practicing certificate.
2.
You must notify your Manager of any changes to scope or conditions on practice
(determined by Regulatory Authority).
3.
You must complete the requirements of any competency programme.
Offical
4.
You must notify your employer of concerns relating to the risk of harm to the public of
another health practitioner practicing below the required standard of competence.
the
5.
Know the provisions of the HPCAA as the governing legislation.
Vulnerable Children Act 2014
under
Due to this position having contact with children and the BOPDHB’s commitment to child
protection, you will be subject to ‘safety checks’ under the Vulnerable Children Act at the
time of hire and thereafter as per the relevant legislation.
Position Holders Declaration
I certify that I have read, understand, and agree to this position description.
Released
Name:
__________________________________________________
Signature:
__________________________________________________
Date:
__________________________________________________
1982
Act
Information
Offical
the
under
Released