
1982
Act
Information
Offical
the
under
Released


1982
Act
Information
Offical
the
under
Released


1982
Act
Information
Offical
the
under
Released


1982
Act
Information
Offical
the
under
Released

 Team:
Team:
1982
Name of primary contact for client:
Act
Primary contact designation:
Psychiatrist/SMO/RMO name:
Other team members, NGOs or community services involved
Formulation
Information
Provide a hypothesis of the cause and nature of presenting problems,
current clinical risks and prognosis. Construct a meaningful story, placing
the person’ s current presentation within the context of his or her life.
Have it aim to answer the fol owing questions:
Offical
•
Why this person?
•
Why this problem?
•
Why at this time?
the
Treatment goals
Goals for service intervention, of the person, whānau, and service which are
under
Specific, Measurable, Achievable, Realistic, Time-bound (SMART). “ What
matters to you?” across domains of wel being)
Clinical Team Actions
Clinical team actions for the person or whānau
Released
Client/whānau/family/others actions
MDT progress summary
Updated at each MDT review: what are we doing to contribute to a
person’ s wel being?
 Wellness Plan
Wellness Plan
Has an Advance Directive been lodged with MHAIDS?
What am I like when I’m wel ?
Things I do that keep me wel
Early warning signs
What can I do to help myself?
1982
What can others do to help me?
Act
Triggers
What can I do to help myself?
What can others do to help me?
When more is needed
Information
Things that don’t help
People I don’t want involved
Offical
People or groups that support me the
How my family, friends and I have been involved in putting this plan together
MHAIDS staff assisting preparation of plan
under
Date of Wel ness Plan:
Client given copies:
Released
Positive Behaviour Support Plan
for
XXXX YYYY
1982
Act
Information
Offical
[Place pho
the
to here]
under
Released
Layout of this Plan
Part A
Introduction
Page 3
Part B
A Bit About Me
Pages X – Y
• Who am I?
• My skills and talents
• My goals for the future
• Understanding me and my behaviour
• My wel being
1982
Part C
My Good Life
Pages X – Y
• My quality of life
Act
• My daily routine
• Proactive strategies for working with me
Part D
When the Going Gets Tough
Pages X – Y
• Non-restrictive de-escalation strategies
• Planned reactive strategies
Information
• Last resort restrictive reactive strategies and post-event
management
Offical
the
under
Released
Page
2 of
13
Part A - Introduction
Please note, this document is written in the first person
This plan provides you, the staff who work with me, guidance around how best to support
me through a shift. The approaches described in this document are informed by our service’s
Model of Care, in particular the principles of Positive Behaviour Support. Emphasis is placed
on promoting my quality of life, because that has been shown to be the most effective way
of improving my wellbeing and reducing the likelihood of me displaying behaviours of
concern. The use of proactive strategies are included, as well as ways to respond - in the
least restrictive manner - to any behaviours of concern that I may present with.
1982
This plan is based on following sources of information:
• What I have told health professionals directly involved in the creation of this plan
Act
• What the health professionals know of my personal preferences and goals
• Information the direct care staff I have worked alongside know about me
• My psychological formulation
This plan was created in partnership on [insert date] by my keyworker [insert name], clinical
psychologist [insert name], and care manager [insert name] with feedback from other
members of my multidisciplinary team. I met with [insert name] on [insert dates] to work on
Information
and review this plan.
This is a living plan, meaning it is added to and changed over time.
Offical
(include the fol owing information for subsequent plan reviews)
Last review date:
the
Key worker:
Clinical psychologist:
Care manager:
under
It is important that my plans are regularly reviewed. This plan should be formally reviewed
every six months, as part of the Good Lives Formulation process. My keyworker and clinical
psychologist are jointly responsible for this.
Released
Page
3 of
13
Part B - A Bit About Me
Who am I?
•
1982
Act
My skills and talents
•
Information
Offical
the
under
My goals - what my team and I are working on at the
moment and aiming for in the future
Released
•
Page
4 of
13

 Understanding my behaviour
Understanding my behaviour
• This table describes the common behaviours of concern I can resort to when I have been
unable to meet my needs in helpful ways.
• The behaviours of concern are listed in order of the frequency they occur (top of table =
most common; bottom of table = least common).
• Remember - I am less likely to engage in these behaviours if you work with me in
proactive ways to promote my quality of life.
My proactive strategies are outlined on
pages x – y.
The behaviour of What it looks Why it happens
Triggers
concern
like for me
1982
Act
Information
Offical
the
under
Released
Pages X – Y outline my early warning signs and ways to de-escalate me, as wel as how to
respond to the above behaviours so to maintain mine and others’ safety.
Page
5 of
13


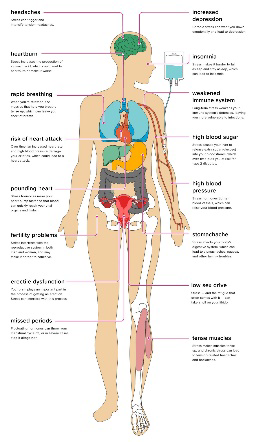
 My wellbeing
My wellbeing
What it looks like How it affects
includes
for me
me
Plan
Taha Tinana
(Physical Wellbeing)
My wellbeing
My wellbeing
What it looks like How it affects
includes
for me
me
Plan
Taha Tinana
(Physical Wellbeing)
1982
Act
Taha Hinengaro
(Mental and
Emotional Wel being)
Information
Offical
Taha Wairua
the
(Spiritual Wel being) under
Taha Whānau
Released
(Family Wellbeing)
Page
6 of
13
Part C - My Good Life
My quality of life
• My good life table is fil ed with activities and experiences that increase my quality of life
and the quality of life of those around me.
• If you are able to work with me
each day to promote the points in this table I wil feel
good, busy and satisfied. I will also be less likely to engage in any unhelpful behaviours of
concern (see page 4) to meet my needs.
1982
My quality of life will be best when… Act
•
Information
Offical
the
under
Released
Page
7 of
13

 My daily routine
My daily routine
• My day-to-day routine is important to me. There are aspects of my adaptive functioning
that I can do independently and others that I require support from you to complete.
• Active support is about you working with me at the right level of support for the given
task. It is important for my goal of moving into the community that I am able to continue
to practice the tasks and skills I can do independently, and learn to develop new skills.
• It is important that you know the tasks I require support to complete and how I need this
support to look.
Activities of daily living
What the support
Activities of daily
1982
that I require support
looks like
living that I can
to complete
complete m
Act
yself
Morning Routine
Information
Evening Routine
Offical
Budgeting and Personal Shopping
the
Use of Transport
under
Self-Occupation
Released
My Leave
Page
8 of
13
 Proactive strategies for working with me
Proactive strategies for working with me
• Proactive strategies are important to use consistently and in the first instance when
working with me to reduce the likelihood of harm to myself or other people.
• There are two types of proactive strategies: proactive
preventative and proactive
developmental.
Proactive preventative strategies
These strategies are focused on managing my environment, reducing my stress
and increasing my wellbeing.
The Strategy
What you need to do
1982
Act
Information
Offical
the
under
Released
Page
9 of
13
 Proactive developmental strategies
Proactive developmental strategies
These strategies are skil s, behaviours, and methods of coping that you can
reinforce when working with me. They are more helpful ways of meeting my needs
of safety, security, personal choice and positive emotion. It would be great if you
could also help me to practice these skills in different situations.
The Strategy
What you need to do
1982
Act
Information
Offical
the
under
Released
Page
10 of
13
Part D – When the Going Gets Tough
Reactive strategies are planned interventions you use with me when my early warning
signs are present or when I am engaging in a behaviour of concern. Early warning signs
are changes in my mood and behaviour to look out for.
My early warning signs
•
1982
Act
Information
Offical
Non-restrictive de-escalation strategies to use when I display my early
the
warning signs
•
under
Released
When the above de-escalation strategies have not worked, proceed as
outlined on page X
Page
11 of
13
When my de-escalation strategies have not worked,
proceed as outlined below
You should:
•
When I am being verbal y
aggressive
1982
Act
You should:
•
When I engage in acts of
property damage
Information
Offical
the
You should:
•
under
When I engage in acts of
physical aggression
Released
Page
12 of
13
As a last resort…
If the strategies specified in the blue boxes do not contain or reduce the behaviour I am
exhibiting
and you have safety concerns for myself or others you can consider the below
restrictive practices:
• Environmental restraint
• Personal restraint
• Prevent me (in the short term) from accessing planned activities or outings
If there is an imminent and/or lethal threat to my or someone else’s safety,
phone 111
1982
Act
Post-event management
• Complete an incident report with a full behavioural description of my behaviour, the
context and environment around me at the time. Please use A-B-C format.
Information
• Once safety is re-established, continue moving forward with my shift as planned. Re-
focus on my quality of life, as that is the most effective way of preventing another
incident.
Offical
• Offer me the chance to speak about my feelings or give me the time and space to
express any residual fears or worries I have.
the
• Offer me the opportunity to talk with members of my care team.
• Offer me the opportunity to com
under plete a chain analysis sheet with staff.
I was actively supported to read through this plan in its entirety by [insert staff name] on
[date].
Released
I signed this plan to acknowledge the above and to confirm I have received a hard copy of
my plan.
Signature ________________________
Thank you for reading and working with me in the way this
plan outlines.
Page
13 of
13
 HUIHUI
6 week initial assessment and 3-monthly multidisciplinary team review
HUIHUI
6 week initial assessment and 3-monthly multidisciplinary team review
Person’s name:
DOB:
NHI:
Date of admission:
Legal status (and court date if relevant):
Victim notification register:
Responsible Clinician:
Care Manager/Key Worker:
Date of last Huihui: Click or tap to enter a date.
1982
Date of this Huihui: Click or tap to enter a date.
Date of last SPR, (if relevant): Click or tap to enter a date.
Act
Date of this SPR, (if relevant): Click or tap to enter a date.
Record all attendees and their relationship to the person:
Did the person attend the Huihui? ☐ Yes / ☐ No
If not, state reason:
Current medication:
Diagnosis (
to be completed by Responsible Clinician)
Information
Psychiatric:
Medical:
Name:
Designation:
Offical
Date: Click or tap to enter a date.
the
Current pathway (
to be completed by Responsible Clinician with input from others)
Name:
Designation:
under
Date: Click or tap to enter a date.
Summary of key presenting issues (
to be completed by Responsible Clinician with input from others)
Summary of presentation:
Key issues to be discussed at Huihui:
Released
Name:
Designation:
Date: Click or tap to enter a date.
Page
1 of
12
 Issues for special patient review panel
Issues for special patient review panel (
must be completed if this report is to be used for the Special Patient
Reviews)
Any recommendations for change in leave status:
Any recommendations for change in legal status:
Last SPR recommendations and outcomes:
Other key issues for discussion:
Name:
Designation:
Date: Click or tap to enter a date.
Last SPR recommendations & outcomes:
1982
Risk summary, to be read with forensic history (
to be completed by Responsible Clinician, attach HCR-20/FAM as
an appendix for all people in the Forensic Service for 3 months or longer. Consider person-specific risks in
Act
formulation, including flight risk)
Risk summary and formulation:
Current level of risk to; Self: Choose an item. Others: Choose an item.
Current risk of absconding: Choose an item.
Flight risk assessment
Information
Dual citizenship: ☐ Yes / ☐ No
Relatives or connections overseas: ☐ Yes / ☐ No
Access to financial resources to fund travel: ☐ Yes / ☐ No
Expressed desire to travel: ☐ Yes / ☐ No Offical
Other incentives to travel: ☐ Yes / ☐ No
Possession of valid/current passport: ☐ Yes / ☐ No
the
Additional information:
For people in medium secure care only (
if not relevant, write N/A):
under
Is this person under night safety order: ☐ Yes / ☐ No
If so, does night safety order need to continue: ☐ Yes / ☐ No
If yes, record reasons:
Expiry date of night safety order, (if relevant): Click or tap to enter a date.
Name:
Designation: Released
Date: Click or tap to enter a date.
Leave (
to be completed by Care manager/Keyworker)
Current leave:
Ground access/community leave
Escorted/unescorted
Staff ratio
Name:
Designation:
Page
2 of
12
Date: Click or tap to enter a date.
Summary of Progress Since Last Review of Admission
Consent to treatment
Is the person still consenting to current medication: ☐ Yes / ☐ No
Date Signed: Click or tap to enter a date.
Persons own report (
to be facilitated by the keyworker. The person may, with you, write their own report, or
have the keyworker write it based on their input. Include comments on the person’s view of their own progress
and any key successes or challenges, their values, goals and long term aspirations and any requests for the
Huihui)
Date: Click or tap to enter a date.
Keyworker, Care manager and/or associates
Clinical report:
1982
Current mental state examination:
Summary of any incident reports since last Huihui:
Key nursing issues:
Act
Name:
Designation:
Date: Click or tap to enter a date.
Psychiatric (
to be completed by Responsible Clinician. Include progress, medication issues, physical issues, current
mental state, plan and recommendations and issues for the review)
Information
Name:
Designation:
Date: Click or tap to enter a date.
Psychology
Offical
Name:
Designation:
the
Date: Click or tap to enter a date.
Social Work
under
Name:
Designation:
Date: Click or tap to enter a date.
Occupational Therapist
Name:
Designation: Released
Date: Click or tap to enter a date.
Employment/education/training/activities update (
to be completed by Care Manager/Occupational Therapist)
Name:
Designation:
Date: Click or tap to enter a date.
Cultural and spiritual (
eg: cultural and spiritual workers such as chaplain)
Name:
Designation:
Page
3 of
12
Date: Click or tap to enter a date.
Other (
include any reports from key others involved in supporting the person. Eg: AOD clinician, mental health
support workers, family comments)
Name:
Designation:
Date: Click or tap to enter a date.
Person’s History
Summary of psychiatric history (
to be completed by Responsible Clinician)
Name:
Designation:
Date: Click or tap to enter a date.
Forensic history (
to be completed by Responsible Clinician. Describe index offence in detail) 1982
Name:
Designation:
Act
Date: Click or tap to enter a date.
Summary of alcohol and drug history (
to be completed by Responsible Clinician or designated other. Eg: AOD
clinician)
Name:
Designation:
Date: Click or tap to enter a date.
Information
Family history and personal history (
to be completed by Responsible Clinician/Social Worker. Include family
psychiatric history if applicable)
Name:
Offical
Designation:
Date: Click or tap to enter a date.
Medical History* See a
the
ppendix 3 for guide to completion
Relevant medical issues and update on management:
Diagnoses and past medical history:
Medical issues this admission: under
Side effect and physical health monitoring:
Date Completed: Click or tap to enter a date.
Designation:
Physical exam- CHAPS (
To be done
Weight, BMI, girth:
Smoker?
annually on all inpatients)
☐ Yes / ☐ No
Released
Smoking cessation (
include current
Date completed: Click or tap to
pattern of use):
Date completed: Click or tap to
enter a date.
enter a date.
Results:
Results:
Blood pressure, pulse:
HbA1c:
Lipids:
Date completed: Click or tap to
Date completed: Click or tap to
Date completed: Click or tap to
enter a date.
enter a date.
enter a date.
Results:
Results:
Results:
LFTs:
Electrolytes and Creatinine:
FBC:
Page
4 of
12
Date completed: Click or tap to
Date completed: Click or tap to
Date completed: Click or tap to
enter a date.
enter a date.
enter a date.
Results:
Results:
Results:
TFTs:
Prolactin:
Clozapine level:
Date completed: Click or tap to
Date completed: Click or tap to
Date completed: Click or tap to
enter a date.
enter a date.
enter a date.
Results:
Results:
Results:
Monitoring of cardiac enzymes, (
if
on Clozapine):
EPS or side effects:
Constipation:
Date completed: Click or tap to
Date completed: Click or tap to
Date completed: Click or tap to
enter a date.
enter a date.
enter a date.
Results:
Results:
Results:
Date of last ECG:
Dental check:
CT or MRI (
if relevant):
1982
Date completed: Click or tap to
Date completed: Click or tap to
Date completed: Click or tap to
Act
enter a date.
enter a date.
enter a date.
Results:
Results:
Results:
CVD risk:
Sexual health screening:
EEG (
if relevant):
Date completed: Click or tap to
Date completed: Click or tap to
Date completed: Click or tap to
enter a date.
enter a date.
enter a date.
Results:
Results:
Information
Results:
Next Due: Click or tap to enter a
Next due: Click or tap to enter a
date.
date.
Cervical smear:
Breast screening:
Immunisations:
Offical
Date completed: Click or tap to
Date completed: Click or tap to
Date completed: Click or tap to
enter a date.
enter a date.
enter a date.
Results:
Results:
the
Results:
Next due: Click or tap to enter a
Next due: Click or tap to enter a
Next due: Click or tap to enter a
date.
date.
date.
Diabetic patient HBa1C:
Retinal screen:
under
Serology status:
Date completed: Click or tap to
Date completed: Click or tap to
Date Completed: Click or tap to
enter a date.
enter a date.
enter a date.
Results:
Results:
Results:
Next due: Click or tap to enter a
Next due: Click or tap to enter a
date.
date.
Released Patient on Metformin – B12/Folate
Diabetic foot exam:
blood test:
Routine bloods due on:
Date completed: Click or tap to
Date completed: Click or tap to
Date completed: Click or tap to
enter a date.
enter a date.
enter a date.
Results:
Results:
Next due: Click or tap to enter a
Results:
date.
Past and Present Huihui Recommendations
Previous Huihui recommendations (
if previous Huihui has occurred)
Page
5 of
12
Recommendations:
1. Was this recommendation completed? ☐ Yes / ☐ No
2. Was this recommendation completed? ☐ Yes / ☐ No
3. Was this recommendation completed? ☐ Yes / ☐ No
4. Was this recommendation completed? ☐ Yes / ☐ No
5. Was this recommendation completed? ☐ Yes / ☐ No
Current Huihui recommendations and outcomes (
what is the planned pathway? What leaves are supported and
wil be requested? What do the team and the person need to do in order for progression to occur?)
1982
General recommendations:
1.
Act
Timeframe Click or tap to enter a date.
2. Timeframe Click or tap to enter a date.
3. Timeframe Click or tap to enter a date.
4. Timeframe Click or tap to enter a date.
5.
Information
Timeframe Click or tap to enter a date.
Any recommended changes in leave status or pathway progression: ☐ Yes / ☐ No
If yes, specify:
Offical
Person’s offered copy:
the
If yes: ☐ accepted / ☐ declined
If not, why?
Responsible Clinician’s Signature ____________________________ Date Click or tap to enter a date.
under
Released
Page
6 of
12
 Appendix 1: Dundrum
Dundrum 3 and 4
Appendix 1: Dundrum
Dundrum 3 and 4 (
complete by the MDT for all people in the Forensic Service for longer than three months. Refer
to Dundrum manual)
Programme
Dundrum 3: Programme Completion
0
1
2
3
4
Items
PC1
Physical health
☐
☐
☐
☐
☐
PC2
Mental health
☐
☐
☐
☐
☐
PC3
Drugs and alcohol
☐
☐
☐
☐
☐
PC4
Problem behaviours
☐
☐
☐
☐
☐
PC5
Self-care and activities of daily living
☐
☐
☐
☐
☐
PC6
Education, occupation and creativity
☐
☐
☐
☐
☐
PC7
Family and social networks
☐
☐
☐
☐
☐
Subtotal
1982
Recovery
Dundrum 4: Recovery Items
0
1
2
3
4
R1
Stability
☐
☐
☐
☐
☐
Act
R2
Insight
☐
☐
☐
☐
☐
R3
Rapport and working alliance
☐
☐
☐
☐
☐
R4
Leave
☐
☐
☐
☐
☐
R5
HCR-20 dynamic items
☐
☐
☐
☐
☐
R6
Victim sensitivities
☐
☐
☐
☐
☐
R7
Hope
☐
☐
☐
☐
☐
Subtotal
Information
Date completed: Click or tap to enter a date.
Offical
the
under
Released
Page
7 of
12
 Appendix 2: Structured professional judgement risk assessment tool: HCR 20/FAM* Coding
Appendix 2: Structured professional judgement risk assessment tool: HCR 20/FAM* Coding (
for all clients in
the Forensic Service for longer than three months. *FAM items to be fil ed in for females only)
Step 1: Gather relevant information
Sources of information:
Summary of psychosocial history
Family/childhood:
Education:
Employment:
Relationships:
Medical problems:
Mental/emotion problems:
Substance use:
Legal problems:
Other:
1982
History of violent behaviour; past and recent (
describe incidents and pattern; when, nature of harm, directed at
and relationship to person, why, where, personal reaction, chronicity, diversity, severity and escalation)
Act
History of violent ideation (
describe incidents and pattern; when, nature of harm, directed at and relationship to
person, why, where, personal reaction, chronicity, diversity, severity and escalation)
Step 2 and 3: Determine the presence and relevance of risk factors (
*fill in only if patient is female)
historical factors – history of problems with:
H1. Violence:
Presence:
Information Choose an item.
Relevance:
Choose an item.
H2. Other antisocial behaviour:
Presence:
Offical
Choose an item.
Relevance:
Choose an item.
the
H3. Relationship:
Presence:
Choose an item.
Relevance:
under
Choose an item.
H4. Employment:
Presence:
Choose an item.
Relevance:
Choose an item.
H5. Substance use:
Presence:
Choose an item.
Released
Relevance:
Choose an item.
H6. Major disorder definite/provisional extent, the most prominent and critical factor in
Presence:
index offense:
Choose an item.
Relevance:
Choose an item.
H7. Personality disorder definite/provisional:
Presence:
Choose an item.
Relevance:
Choose an item.
Page
8 of
12
H8. Traumatic experiences:
Presence:
victimisation/trauma:
Choose an item.
adverse childrearing experiences:
Relevance:
Choose an item.
H9. Violent attitudes:
Presence:
Choose an item.
Relevance:
Choose an item.
H10. Treatment or supervisor response:
Presence:
Choose an item.
Relevance:
Choose an item.
H11. Prostitution*:
Presence:
Choose an item.
Relevance:
1982
Choose an item.
H12. Parenting*:
Presence:
Act Choose an item.
Relevance:
Choose an item.
H13. Pregnancy at a young age*:
Presence:
Choose an item.
Relevance:
Choose an item.
Information
H14. Suicidality/self-harm*:
Presence:
Choose an item.
Relevance:
Choose an item.
Offical
H15. Other historical risk factors:
Presence:
Choose an item.
the
Relevance:
Choose an item.
Clinical factors – recent problems with:
C1. Insight:
Presence:
under
Choose an item.
Relevance:
Choose an item.
C2. Violent ideation or intent:
Presence:
Choose an item.
Relevance:
Released
Choose an item.
C3. Symptoms of major mental disorder definite/provisional:
Presence:
Choose an item.
Relevance:
Choose an item.
C4. Instability:
Presence:
Choose an item.
Relevance:
Choose an item.
C5. Treatment or supervision response:
Presence:
Choose an item.
Page
9 of
12
Relevance:
Choose an item.
C6. Covert, manipulative behaviour*:
Presence:
Choose an item.
Relevance:
Choose an item.
C7. Low self-esteem*:
Presence:
Choose an item.
Relevance:
Choose an item.
C8. Other clinical risk factors:
Presence:
Choose an item.
Relevance:
Choose an item.
1982
Risk Management Factors – Future Problems With (
specify context inpatient/community)
R1. Professional services:
Presence:
Choose an item.
Act Relevance:
Choose an item.
R2. Living situation:
Presence:
Choose an item.
Relevance:
Choose an item.
R3. Personal support:
Presence:
Information Choose an item.
Relevance:
Choose an item.
R4. Treatment or supervision response:
Presence:
Offical
Choose an item.
Relevance:
the
Choose an item.
R5. Stress or coping:
Presence:
Choose an item.
Relevance:
under
Choose an item.
R6. Problematic childcare*
Presence:
Choose an item.
Relevance:
Choose an item.
R7. Problematic intimate relationships*:
Presence:
Released
Choose an item.
Relevance:
Choose an item.
R8. Other risk management:
Presence:
Choose an item.
Relevance:
Choose an item.
Completed by:
Designation:
Date: Click or tap to enter a date.
Page
10 of
12
 Appendix 3: Previous Psychiatric Huihui Reports
Appendix 3: Previous Psychiatric Huihui Reports
Completed by:
Designation:
Date: Click or tap to enter a date.
1982
Act
Information
Offical
the
under
Released
Page
11 of
12
 Appendix 4: Guide for Medical History
Appendix 4: Guide for Medical History
• Physical Exam- CHAPS (To be done annually on all inpatients)
• Weight, BMI, girth (For mood stabiliser (carbamazepine, lithium, valproate, lamotrigine), baseline then at 3
and 6 months, more often if person gains weight rapidly. For antipsychotics, baseline then at least annually.
For clozapine and olanzapine, more often for the 1st year (1-3monthly) then at least annually.
• Blood pressure, pulse (For mood stabiliser, baseline then annually. For all antipsychotics, baseline, during
titration then annually)
• HbA1c (For antipsychotics, baseline, 3months then annual y if no changes noted and no other risk factor. If
person is high risk or on clozapine, olanzapine, monthly tests for first 3 months, then 3 monthly for the rest
of the year, then annually)
• Lipids (For antipsychotics, baseline, 3months then annual y. If person on clozapine, olanzapine,
phenothiazines, quetiapine, 3 monthly for the 1st year, then annually)
• LFTs. (Baseline then every 3-6mths for the 1st year then annually. More often if abnormal LFT’s, include
1982
prothrombin and albumin if abnormal.
• Electrolytes and creatinine (Baseline, then every 3-6 months for the 1st year then annually. More often if
Act
abnormal LFTs ,include prothrombin and albumin if abnormal)
• FBC (Baseline then every 6 months for antipsychotics. Annually for mood stabilisers. If on clozapine, follow
clozapine schedule)
• TFTs (
Baseline. Then every 6 months if on quetiapine, lithium or thyroid dysfunction)
• Prolactin (
Not required for mood stabilisers. For antipsychotics, baseline, then if symptoms occur. If on
amisulpiride, risperidone or typical antipsychotics, baseline, 6months then annually or symptoms occur)
Information
• Clozapine level (3 monthly for inpatients on clozapine. Monthly if suspected non-compliance)
• Monitoring of cardiac enzymes if on clozapine (For patient on clozapine, baseline CK, CRP, trop T and pro
BNP. Repeat CRP, trop T weekly for 1st 8 weeks. Be aware of myocarditis in 1st 1-2months of tx and for
cardiomyopathy any time)
Offical
• EPS or side effects (Baseline then 6 monthly)
• Constipation (On-going monitoring)
the
• Date of last ECG (
Baseline ECG in all patients. Annual ECG)
• Dental checking (Annual dental review for all long stay clients.)
• CT or MRI head (If relevant) under
• EEG (If relevant)
• When next blood tests are due
GP/ House Surgeon to complete:
• CVD risk
• Sexual health screening:
Released
• Cervical smear
• Breast screening
• Immunisations
• Serology status?
• Diabetic patient
• HBa1C
• Retinal screen
• Diabetic foot exam
• Patient on Metformin - B12/Folate blood test
Page
12 of
12
Document Outline