APPENDIX 1
PATIENT ID LABEL
Date ............................ Time .........................
Contributors: to MDT – see over
OLDER ADULT MENTAL HEALTH/STAR 1
INITIAL MDT TREATMENT PLAN
Presenting complaint:
Assessments: Date:
CT Head
Cogs
Medical:
Functional
1982
Allied Health
Act
Primary focus of treatment:
Legal status:
WRITING
Information
FAMILY MEETING:
Offical
Referrals required/requested/completed:
the
BINDING MARGIN – NO
under
Issue:
Goal: Released
Actions:
Responsibility:
Issue:
Goal:
Actions:
Responsibility:
PATIENT ID LABEL
Issue:
Goal:
Actions:
Responsibility:
Issue:
Goal:
1982
Actions:
Act
Responsibility:
Contributors
Psychiatrist:
Medical Officer:
WRITING
Information
Associate Charge Nurse:
Charge Nurse Manager:
Clinical Nurse Specialist:
Offical
CPN:
CPN:
the
BINDING MARGIN – NO
CPN:
CPN:
CPN:
under
Occupational Therapist:
Social Worker:
Supportlinks:
Ward Nurse: Released
Student Nurse:
Other:
Proposed discharge destination:
Proposed date of discharge:
Follow up:
Signed on behalf of MDT:
MDHB-7164 Ver: 3 2021
This form relates to MDHB-6431
1141868 C: 2362


Name: ____________________________ NHI: ____________
Address: _____________________________________________
Date of Birth: ___________________ Gender:______________
GP or Consultant: - _________________ Area: _____________
WHAIORA ID LABEL HERE
INTERDISCIPLINARY PLANNING AND REVIEW MEETING
Mental Health and Addiction Service
Team:
Last review date:
Current review date:
E
Rationale for Review
□ Sudden major change in Mental State
□ Routine Case Review
□ Initial Case Review
□ Other (e.g. Incident – Please specify)
_______________________________
Interdisciplinary team and whānau wahiora present:
Name
Discipline/Link
Name
Discipline/Link
1982
□
□
□
□
Act
□
□
□
□
□
□
□
□
□
□
□
□
□
□
Information
□
□
□
□
□
□
□
□
□
Offical
□
□
□
□
□
the
□
□
Provisional/Principal formulation/diagnosis:
Other formulation/diagnosis:
_________________________________________
__________________________________
under
Legal status (example, MH Act, Informal, etc.) _________________________________________________
Leave conditions (inpatient): _______________________________________________________________
Cultural identity: _________________________________________________________________________
Released
Family whānau/significant other unable to participate (rationale):
______________________________________________________________________________________
______________________________________________________________________________________
Current wellbeing recovery plan
□ Yes
□ No
Current safety/risk assessment presented
□ Yes
□ No
HoNOS/HoNOSCA/HoNOS 65+/ADOM
□ Yes
□ No
Whānau whaiora strengths and identified needs:
MDHB-5451 Ver.8 2023
This form relates to MDHB-6431
Page 1 of 4
I:\Quality\Team\PHILIPPA\Ready to Import\2018\Specialist Community Consent and Confidentiality Form - Mental Health and Addiction Service.doc Printed 27/01/2024 4:24:00 pm


Name: ____________________________ NHI: ____________
Address: _____________________________________________
Date of Birth: ___________________ Gender:______________
GP or Consultant: - _________________ Area: _____________
WHAIORA ID LABEL HERE
Context and narrative discussion key points only:
Taha wairua:
E
Taha whānau:
1982
Taiao (environment, housing and income,etc.):
Act
Taha tinana:
Information
Offical
Taha hinengaro:
the
under
Wellness recovery action plan (WRAP):
Released
MDHB-5451 Ver.8 2023
This form relates to MDHB-6431
Page 2 of 4
I:\Quality\Team\PHILIPPA\Ready to Import\2018\Specialist Community Consent and Confidentiality Form - Mental Health and Addiction Service.doc Printed 27/01/2024 4:24:00 pm


Name: ____________________________ NHI: ____________
Address: _____________________________________________
Date of Birth: ___________________ Gender:______________
GP or Consultant: - _________________ Area: _____________
WHAIORA ID LABEL HERE
Please circle:
HoNOS/HoNOSCA/HoNOS 65+/ADOM
RATED 2 AND ABOVE:
Rating
Item Name
Rating
Item Name
Rating
Item Name
E
Identify and state the focus of intervention/therapy and actions required to enable wellbeing recovery and the
transfer or care or discharge from the service. Enter these directly into Wellbeing Recovery plan as headed
1982
up below.
Date
Identified
Interdisciplinary By whom
By when
Outcome/comments
Review
Act
Te Ra
wellness
plan, agreed
I a Wai
Te Rangi
Ngahuia/Ngakorero
Date
recovery
therapy
kia oti
Te Ra hei
goals
intervention
atu
Tirohanga
ano
Information
Offical
the
under
Released
MDHB-5451 Ver.8 2023
This form relates to MDHB-6431
Page 3 of 4
I:\Quality\Team\PHILIPPA\Ready to Import\2018\Specialist Community Consent and Confidentiality Form - Mental Health and Addiction Service.doc
Printed 27/01/2024 4:24:00 pm



Name: ____________________________ NHI: ____________
Address: _____________________________________________
Date of Birth: ___________________ Gender:______________
GP or Consultant: - _________________ Area: _____________
WHAIORA ID LABEL HERE
Transition/Discharge Goals
Actions
By Whom?
By When?
E
1982
Act
Planned Transition/Discharge Date: ____/____/____
Information
Next IDP Review Date: ____/____/____
Offical
the
Lead facilitator:______________________________
Care Coordinator:___________________________
under
Name: ____________________________________
Name:____________________________________
Discipline: _________________________________
Discipline:_________________________________
Released
MDHB-5451 Ver.8 2023
This form relates to MDHB-6431
Page 4 of 4
I:\Quality\Team\PHILIPPA\Ready to Import\2018\Specialist Community Consent and Confidentiality Form - Mental Health and Addiction Service.doc
Printed 27/01/2024 4:24:00 pm

Name:______________________________ NHI: ____________
Address: ______________________________________________
Date of Birth: _________________ Gender:_________________
GP or Consultant: _____________________________________
OR PATIENT ID LABEL HERE
MENTAL HEALTH AND ADDICTION SERVICE
DISCHARGE SUMMARY
Phone No:
Date first seen:
Date last seen:
Referral source:
E
Date of discharge:
GP/NP:
Name of Care Coordinator:
Psychiatrist name:
Presenting problems:
1982
Act
DSM IV Principal Diagnosis:
Treatment and Progress:
Smoker:
Yes
No
Smoking Cessation Programme offered:
Yes
No
Current Physical Medication (if known):
Current Mental Health Medication:
Relapse indicators:
Information
Whānau consulted in discharge plan (if appropriate):
Yes
No
Copy of discharge summary provided to:
GP:
Yes
No
Consumer:
Yes
No
Offical
Whānau: (if appropriate)
Yes
No
Other: Yes
No
the
Follow up recommendations:
under
Name of person completing discharge:
Designation:
Signature of person completing discharge:
Date:
Please tick appropriate service below:
Early Intervention Service
Child, Adolescent
Horowhenua Locality
Oranga
Oranga Hinengaro
Released
and Family Service
Hinengaro Kaupapa
Kaupapa Māori
Palmerston North
Māori Horowhenua
Manawatu
Phone: 0800 653 357
Palmerston North
Levin
Phone: 0800 653 357
Phone 0800 653 357
Levin
Palmerston North
Phone 0800 653 357 Phone 0800 653 357
Manawatu Locality
Tararua Locality
Specialist Primary
Ward 21- Acute
Crisis Resolution
Inpatient Unit
Palmerston North
Dannevirke
Palmerston North
Palmerston North
Phone 0800 653 357
Phone (0800 653 357
Phone 0800 653 357
Phone 0800 653
Phone 0800 653 357
357
MidCentral Mental Health and Addiction Service – Te Uru Rauhi
Ward 21 Interim Discharge Summary
Freephone 0800 653 357
Private Bag 11036,
PALMERSTON NORTH
MDHB-3798 ver.7 2023
This form relates to MDHB-6431
Page 1/1
I:\Quality\Team\DANIEL\IMPORTING\Referral and Triage Checklist - Alcohol and Other Drug Service -Form-.doc
Printed 27/01/2024 4:10 pm

Patient label here
CHILD AND ADOLESCENT MENTAL HEALTH SERVICE
My Just in Case Plan
Triggers that increase my distress (i.e., social media, school, home, environment, being bullied):
1.
1982
2.
Act
3.
4.
TING
TING
RI
RI
W
W
Information
5.
– NO
– NO
N
N
GI
GI
AR
AR
Offical
M
M
6.
G
G
IN
IN
the
D
D
BIN
BIN
Early warning signs or red flags to kno
under w that I may be getting worse (i.e., being more alone,
irritable, angry, upset, tearful, what I feel inside):
1.
Released
2.
3.
MDHB-8513 Ver.1 2023 This form relates to MDHB-2930, MDHB-3798 and MDHB-248
Page 1 of 3
C:\Users\Katherineel\Downloads\My Just In Case Plan INTERACTIVE -Form- (1).docx
Printed 1/28/2024 1:08:00 PM

Patient label here
Internal coping strategies which can take my mind off my thoughts and emotions (i.e., deep
breathing, grounding, mindfulness, positive thoughts):
1.
2.
3.
1982
External coping strategies to keep me safe (i.e., actions I can take):
Act
1.
2.
TING
TING
RI
RI
W
W
Information
3.
– NO
– NO
N
N
GI
GI
AR
AR
Offical
M
M
G
G
People and social settings which can support or distract me:
IN
IN
the
D
D
Name:
Phone:
BIN
BIN
Name:
Phone:
under
Name:
Phone:
Professionals/agencies I can ask for help – do they need a copy of the plan?
Name:
Phone:
Released
Name:
Phone
MDHB-8513 Ver.1 2023 This form relates to MDHB-2930, MDHB-3798 and MDHB-248
Page 2 of 3
C:\Users\Katherineel\Downloads\My Just In Case Plan INTERACTIVE -Form- (1).docx
Printed 1/28/2024 1:08:00 PM

Patient label here
Future Plans:
1.
2.
3.
1982
Act
Reasons for living (if no future plans):
1.
TING
TING
RI
RI
W
W
Information
2.
– NO
– NO
N
N
GI
GI
AR
AR
Offical
M
M
3.
G
G
IN
IN
the
D
D
BIN
BIN
Re-assess risk on:
under
Appointment scheduled with:
Young person’s name:
Caregiver’s name:
Clinician’s name:
Role:
Date completed:
Released
Acute Crisis Team: 0800 653 357
Youthline freephone 0800 376 633 / Lifeline 0800 543 354 /
Parentline freephone 0800 432 6459 / Need To Talk – free text/call 1737 anytime
CAMHS MidCentral (06) 350 8373
MDHB-8513 Ver.1 2023 This form relates to MDHB-2930, MDHB-3798 and MDHB-248
Page 3 of 3
C:\Users\Katherineel\Downloads\My Just In Case Plan INTERACTIVE -Form- (1).docx
Printed 1/28/2024 1:08:00 PM

Patient label here
CHILD AND ADOLESCENT MENTAL HEALTH SERVICE
My Transition Plan
Date:
Client Contact Number:
Keyworker:
Referral Source:
Date first seen:
Date last seen:
1982
Number of sessions:
Act
G
G
RITIN
RITIN
W
W
Reason for referral:
– NO
– NO
IN
IN
ARG
ARG
Information
M
G
M
G
IN
D
IN
D
BIN
BIN
Offical
the
under
The things that I have been working on:
Released
CHILD AND ADOLESCENT MENTAL HEALTH SERVICE
Konini House, Community Vil age, Te Whatu Ora – Health New Zealand | Te Pae Hauora o Ruahine o Tararua |
MidCentral, Private Bag 11036, Palmerston North Phone 06 3508373, Email:
[email address]
MDHB-8512 Version 2 2023
This form relates to MDHB-2930, MDHB-3798 , MDHB-248
Page 1 of 4
https://midcentraldhb-my.sharepoint.com/personal/nathans_mdhb_health_nz/Documents/Microsoft Teams Chat Files/My Transition Plan - INTERACTIVE -Form- 25 Sep 2023.docx
Printed 27/01/2024 4:09:00 pm

Patient label here
The things that I have achieved since I first came here:
1982
The things that have supported my wellbeing:
Act
G
G
RITIN
RITIN
W
W
– NO
– NO
IN
IN
ARG
ARG
Information
M
G
M
G
IN
D
IN
D
BIN
BIN
Things I can keep doing to support my wellbeing:
Offical
the
under
My plans for follow-up with other services after I finish here:
Released
Service name
What they do
Key contact person
Phone number
CHILD AND ADOLESCENT MENTAL HEALTH SERVICE
Konini House, Community Vil age, Te Whatu Ora – Health New Zealand | Te Pae Hauora o Ruahine o Tararua |
MidCentral, Private Bag 11036, Palmerston North Phone 06 3508373, Email:
[email address]
MDHB-8512 Version 2 2023
This form relates to MDHB-2930, MDHB-3798 , MDHB-248
Page 2 of 4
https://midcentraldhb-my.sharepoint.com/personal/nathans_mdhb_health_nz/Documents/Microsoft Teams Chat Files/My Transition Plan - INTERACTIVE -Form- 25 Sep 2023.docx
Printed 27/01/2024 4:09:00 pm

Patient label here
What I need from these other services:
My early warning signs:
1982
Act
G
G
RITIN
RITIN
W
W
– NO
– NO
IN
IN
ARG
My just-in-case plans:
ARG
Information
M
G
M
G
IN
D
IN
D
BIN
BIN
Offical
the
If I need support, I can contact:
under
Urgent:
Non-urgent:
Released
Diagnosis:
CHILD AND ADOLESCENT MENTAL HEALTH SERVICE
Konini House, Community Vil age, Te Whatu Ora – Health New Zealand | Te Pae Hauora o Ruahine o Tararua |
MidCentral, Private Bag 11036, Palmerston North Phone 06 3508373, Email:
[email address]
MDHB-8512 Version 2 2023
This form relates to MDHB-2930, MDHB-3798 , MDHB-248
Page 3 of 4
https://midcentraldhb-my.sharepoint.com/personal/nathans_mdhb_health_nz/Documents/Microsoft Teams Chat Files/My Transition Plan - INTERACTIVE -Form- 25 Sep 2023.docx
Printed 27/01/2024 4:09:00 pm

Patient label here
My medications:
Medication name
What it does
Dose
How to take it
When to take it
My appointments:
1982
Appointment with
Date
Phone number
Act
G
G
RITIN
RITIN
W
W
– NO
– NO
IN
IN
ARG
ARG
Information
M
Transition Planning Agreement
G
M
G
IN
D
IN
Client completing transition plan:
D
BIN
BIN
Name:
Signature:
Date:
Offical
the
Family completing transition plan:
Name:
Signature:
Date:
under
Clinician completing transition plan:
Name:
Signature:
Date:
Released
Copies of the Transition Plan sent to client/family/GP/ Others:
Please name:
CHILD AND ADOLESCENT MENTAL HEALTH SERVICE
Konini House, Community Vil age, Te Whatu Ora – Health New Zealand | Te Pae Hauora o Ruahine o Tararua |
MidCentral, Private Bag 11036, Palmerston North Phone 06 3508373, Email:
[email address]
MDHB-8512 Version 2 2023
This form relates to MDHB-2930, MDHB-3798 , MDHB-248
Page 4 of 4
https://midcentraldhb-my.sharepoint.com/personal/nathans_mdhb_health_nz/Documents/Microsoft Teams Chat Files/My Transition Plan - INTERACTIVE -Form- 25 Sep 2023.docx
Printed 27/01/2024 4:09:00 pm


Name:
Address:
PATIENT ID LABEL
NHI:
DOB:
Gender:
Consultant:
Ward:
SPECIALIST COMMUNITY CONSENT AND CONFIDENTIALITY FORM
FOR THE CHILD AND ADOLESCENT MENTAL HEALTH SERVICE (CAMHS)
By signing this agreement I consent to:
Receiving services as per the information and agreements outlined in this document.
• I understand that before any assessments or treatments are conducted, I have the right to be fully informed
about what they involve.
• I also understand that trained professionals will be the ones conducting the assessments and treatments,
and they will only do so with my consent, except when the law, such as the Mental Health (Compulsory
Assessment and Treatment) Amendment Act of 1999, requires otherwise.
•
1982
I also understand that with my consent only, my family, whānau, or significant others may be invited to
participate in my assessment and treatment.
Act
• If I am under 16 years old, my family, whānau, or legal guardian must give their consent for my assessment
and treatment.
• Furthermore, I understand that my treatment will involve a multi-disciplinary approach (MDT). This means
that the care I will receive may involve multiple professionals such as Social Workers, Occupational
Therapists, Mental Health Nurses, Doctors, Psychologists, a Dietician, Key Workers, and alcohol and drug
clinicians.
•
Information
I am aware that MidCentral Health protocol requires CAMHS staff to consider notifying the appropriate
authorities in situations where the safety of myself or others is at serious risk. These situations can include
cases of immediate risk of sexual or physical abuse.
• Additionally, I understand that when CAMHS staff work with my family where the parents involved in my
Offical
care are separated (and both are active in providing ongoing support), the staff may share information
relevant to my care with both caregivers/guardians.
the
• Lastly, I am aware that if I am unable to establish a working therapeutic relationship with my key worker or
responsible clinician (Dr) , I may request a change. Continuing with an unsatisfactory relationship could
impede my recovery.
under
Information collected about me will be used to provide health care and treatment and for the purposes of
administration. Non-identifying information will be used by MidCentral Health, and the Ministry of Health for
statistical purposes.
My health information about me will be accessible by my Primary Care Health Practitioner, (GP) and will be
shared with specialist healthcare providers involved in the delivery of my care unless I indicate otherwise.
Released
My health records (electronic and hardcopy) will be stored securely; these include all clinical information,
diagnostic results and treatment plans unique to me. Only staff involved in my care will have access to my
records.
NB: Full consent must be re-obtained and signed by the service user at each twelve-month anniversary of entry
to the MHAS outpatient service
MDHB-8462 ver.1 2023
This form relates to MDHB-1998
Page 1 of 2
I:\Quality\Team\PHILIPPA\Ready to Import\Specialist Community Consent and Confidentiality Form - Mental Health and Addiction Service -Form-.doc
Printed 27/01/2024
2:50:00 pm






Name:
Address:
PATIENT ID LABEL
NHI:
DOB:
Gender:
Consultant:
Ward:
I (name):_______________________ have been informed that:
(This is for either the parent/guardian, or young person age 16 or over to write their full name)
I/and/or my family/ whānau have the right to refuse any treatment or withdraw my/their consent to treatment at
any time unless specified by law e.g. Mental Health (Compulsory Assessment and Treatment) Amendment
Act, 1999).
I
have had this agreement fully explained to me, and I had the opportunity to ask questions and obtain any
clarification I might require.
I received information and was provided with the brochure: ‘
Your Rights and Responsibilities When Receiving
Health and Disability Services’ YES NO.
I have been informed how to access advocacy services YES NO
1982
I
do not consent to the following people being involved in my care:
Act
(This is to advise us of whom you do not want to be part of your care while you are with this service. You will
need to be specific)
_____________________________________________________________________
_____________________________________________________________________
I do
give consent for the following people/agencies (family/whānau/significant other/community support) to be
Information
involved in my care: name, contact and relationship to the person
(This is to advise us of whom we can contact for additional information/support as part of your care with this
service – we will check with you first if there is any need to link with other services to fnd out if this is okay first,
and we will ask you to update this information below as required).
Offical
_____________________________________________________________________
_____________________________________________________________________
the
Signature______________________________
Date______________________
This signature is to confirm that this part of the document has been discussed and completed with you.
under
(This section is providing your consent for treatment via the CAMHS team. For young people age 16 and over
you just need to sign and date at the bottom of this box. Parents that sign will need to complete this box in full.
I ____________________________(as the
Parent, Legal/Welfare guardian, EPOA) give
consent for treatment on behalf of ________________________________________
Released
Signed:_____________________________
Date:____________________
Name of Clinician: ___________________________ Signature: _____________________
Designation: ________________________________ Date: ________________________
If the Family/Client does not wish to sign the consent form, the clinician responsible for the care is to
document the discussion here:
MDHB-8462 ver.1 2023
This form relates to MDHB-1998
Page 2 of 2
I:\Quality\Team\PHILIPPA\Ready to Import\Specialist Community Consent and Confidentiality Form - Mental Health and Addiction Service -Form-.doc
Printed 27/01/2024 2:50:00 pm


 BINDING MARGIN – NO WRITING
Attach Patient ID label, or control F1 in box
BINDING MARGIN – NO WRITING
Attach Patient ID label, or control F1 in box
1982
TE OHU WHAKARAHI WHĀNAU Act
MENTAL HEALTH MDT CASE REVIEW MEETING
□ Risk assessment completed
□Honos / HonoSCA completed
□My Goals (ITP) completed
Client Name (NHI):
Age:
Family/Client Update:
Enter name of participants here:
Information
Date
Service
Service support plan / Goals
By whom
By when
Outcome / Comments
Review Date
Ministry of
Offical
Education support
the
Te Ohu Support
under
Oranga Tamariki
Support
Released
MDHB-8367 ver.1 2023 This form relates to MDHB-6431 and MDHB-672
BINDING MARGIN – NO WRITING
Page 1/2
C:\Users\PhilippaS\AppData\Local\Microsoft\Windows\INetCache\Content.Outlook\2CM0MP3Q\Nathans MDT Case Review Meeting Landscape (003).doc



 BINDING MARGIN – NO WRITING
Attach Patient ID label, or control F1 in box
BINDING MARGIN – NO WRITING
Attach Patient ID label, or control F1 in box
1982
Date:
Family/Whanau participation:
Act
Additional information:
Information
Offical
the
Agency sign off for the plan (at least two services):
Te Ohu:
Designation:__________________
Signature:________________
Date:___________________
under
Ministry of Education:
Designation:__________________
Signature:________________
Date:___________________
Oranga Tamariki:
Designation:__________________
Signature: _________________
Date:___________________
Released
MDHB-8367 ver.1 2023 This form relates to MDHB-6431 and MDHB-672
BINDING MARGIN – NO WRITING
Page 2 of 2
C:\Users\PhilippaS\AppData\Local\Microsoft\Windows\INetCache\Content.Outlook\2CM0MP3Q\Nathans MDT Case Review Meeting Landscape (003).doc
Printed 27/01/2024 4:12:00 pm
 BINDING MARGIN – NO WRITING
BINDING MARGIN – NO WRITING
Name: __________________________________________________
Address:_________________________________________________
NHI: _______________ DOB: ___________ Gender:__________
GP: ______________________ Area: ___
WHAIORA ID LABEL HERE
1982
MENTAL HEALTH AND ADDICTION SERVICE WELLBEING RECOVERY PLAN
Te Hotaka Whakapaipa
Act
MAHI AROHA
Date:
START assessment completed
Te Ra:
Te Aio Matawai Tupono
Honos/HonoSCA completed
Information
What is recovery for me? ( Whaiora Narrative)
Offical
the
Taiao
Environment:
under
Housing:
Community Connections:
Released
MDHB-2930 ver. 10 2023
This form relates to MDHB-248
Page 1/4
I:\Quality\Team\PHILIPPA\Ready to Import\2018\Mental Health and Addictions Service Integrated Treatment Plan (ITP) -Form-.doc
Printed 27/01/2024 4:26:00 pm
 BINDING MARGIN – NO WRITING
BINDING MARGIN – NO WRITING
Name: __________________________________________________
Address:_________________________________________________
NHI: ________________ DOB: ____________ Gender:__________
GP: ______________________Area: _________________________
WHAIORA ID LABEL HERE
1982
What I hope to achieve for my recovery and wellbeing
Act
Taha Wairua
Taha Whānau
Beliefs:
Connections:
Values:
Dynamics:
Tumanako,hopes:
Information
Taha Tinana
Taha Hinengaro:
Nurition:
Emotional regulation:
Offical
Exercise:
Processing my experience:
Sleep:
Insight:
the
under
Released
MDHB-2930 ver. 10 2023
This form relates to MDHB-248
Page 2/4
I:\Quality\Team\PHILIPPA\Ready to Import\2018\Mental Health and Addictions Service Integrated Treatment Plan (ITP) -Form-.doc
Printed 27/01/2024 4:26:00 pm
 BINDING MARGIN – NO WRITING
BINDING MARGIN – NO WRITING
N
a
m
e:
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
_
Address:_________________________________________________
NHI: _______________ DOB: ____________ Gender:__________
GP: ______________________ Area: _________________________
WHAIORA ID LABEL HERE
1982
Working to achieve my recovery
Act
Date
Recovery focused actions
Support intervention approaches
By whom
Review
Te Ra
The what
The how
Date
Information
Offical
the
under
Released
MDHB-2930 ver. 10 2023
This form relates to MDHB-248
Page 3/4
I:\Quality\Team\PHILIPPA\Ready to Import\2018\Mental Health and Addictions Service Integrated Treatment Plan (ITP) -Form-.doc
Printed 27/01/2024 4:26:00 pm
 BINDING MARGIN – NO WRITING
BINDING MARGIN – NO WRITING
Name: __________________________________________________
Address:_________________________________________________
NHI: ________________ DOB: ____________ Gender:__________
GP: ______________________Area: _________________________
WHAIORA ID LABEL HERE
1982
If I am starting to get unwell. WRAP
Act
What you may see:
Information
How you can help:
Offical
the
Our agreements: Whaiora, Whānau, IDP team, Others:
under
Signed:
Released
MDHB-2930 ver. 10 2023
This form relates to MDHB-248
Page 4/4
I:\Quality\Team\PHILIPPA\Ready to Import\2018\Mental Health and Addictions Service Integrated Treatment Plan (ITP) -Form-.doc
Printed 27/01/2024 4:26:00 pm
MidCentral Health Mental Health and Addictions Audit tool
Service Name: CAMHS
(Complete a minimum of 5 files)
Date: June 2023
EXECUTIVE SUMMARY – PART 1 PART 1.1 CONSUMER RIGHTS
Consumers receive safe services of an appropriate standard that comply with consumer rights legislation. Services are provided in a manner that is respectful of
consumer rights, facilitates informed choice, minimises harm, and acknowledges cultural and individual values and beliefs.
1982
Standard 1.1.1 Consumer Rights During Service Delivery: Consumers receive services in accordance with consumer rights legislation.
Evidence/EXAMPLE ANSWERS
Criteria 1.1.1.1 Providers demonstrate knowledge & understanding of consumer rights
File 1.
Evidence
Act
Y
and obligations, & incorporate in everyday practice.
File 2.
Y
File 3.
Y/N
File 4.
Y/N
File 5.
Y/N
Standard 1.1.2 Consumer Rights During Service Delivery: Consumers are informed of their rights.
Information
Evidence
Criteria 1.1.2.1 The Health and Disability Services Consumers’ Rights Code is clearly displayed and easily accessible to all consumers.
1.1.2.2 Information about the Code and other rights is provided at the earliest
File 1.
Evidence
Y/N
opportunity in languages and formats suited to consumers
File 2.
Y/N
Offical
(Is this documented in the service user’s file?)
File 3.
Y/N
the
File 4.
Y/N
File 5.
Y/N
under
1.1.2.3 Opportunities are provided for explanations, discussion, and clarification about
File 1.
Evidence
N
the Code with consumer, family/whanau / legal rep
File 2.
Y/N
You will need to Interview staff and consumers:
File 3.
Y/N
File 4.
Y/N
File 5.
Y/N
Released
1
1.1.2.4 Information about Nationwide H&D Advocacy Service is clearly displayed &
accessible & brought to the attention of consumers.
Standard 1.1.4 Recognition of Maori Values and Beliefs: Consumers who identify as Maori have their health and disability needs met in a manner that respects and
acknowledges their individual and cultural, values and beliefs.
Evidence
Criteria
1.1.4.1 Maori consumers receive services consistent with their cultural values and
1982
beliefs.
1.1.4.4 Maori consumers’ right to practise their cultural values and beliefs is
acknowledged and facilitated by service providers.
Act
1.1.4.5 The importance of whanau and their involvement with Maori consumers is
recognised and supported by service providers.
1.1.4.6 Tangata whenua are consulted when meeting the needs of Maori consumers.
M.H.A only: 1.1.4.7
The service provides education and support for tangata whaiora,
whanau, hapu and iwi, to promote Maori mental well-being.
Standard 1.1.10 Informed Consent: Consumers and where appropriate their family/whanau of choice, are provided with the information they need to make
Information
informed choices and give informed consent.
Evidence
1.1.10.1 Informed consent policies/procedures identify:
File 1.
Evidence
Y
(a)
Recording requirements;
Offical
File 2.
Y/N
(b)
Information (including documentation) provided to the consumer by the service.
File 3.
Y/N
the
File 4.
Y/N
File 5
Y/N
under
1.1.10.2 Service providers demonstrate their ability to provide the information that
consumers need to have, to be actively involved in their recovery, care, treatment, and
support as well as for decision-making.
1.1.10.3 Information is made available to consumers in an appropriate format and in a
timely manner.
Released
2
1.1.10.4 The service is able to demonstrate that written consent is obtained where
File 1. Consent form has not been completed
Evidence
N
required.
File 2.
Y/N
File 3.
Y/N
File 4.
Y/N
File 5.
Y/N
1.1.10.5 Service providers have a thorough knowledge and understanding of how to
meet their duties to consumers in relation to Rights 5, 6 and 7 of the Code.
1.1.10.6 Consumer choices and decisions are recorded and acted on.
File 1.
Evidence
1982
N
File 2.
Y/N
File 3.
Y/N
Act
File 4.
Y/N
File 5.
Y/N
1.1.10.7 Advance directives that are made available to service providers are acted on
where valid.
Standard 1.11.11 Advocacy and Support
Service providers recognise and facilitate the right of consumers to advocacy/support persons of their choice.
Information
Evidence
1.1.11.1 Consumers are informed of their rights to an independent advocate, how to
File 1.
Evidence
N
access them, and their right to have a support person(s) of their choice are to be
File 2.
Y/N
present.
Offical
File 3.
Y/N
File 4.
Y/N
File 5.
Y/N
the
1.1.11.2 The service has policies to facilitate the presence of advocates/support person.
1.1.11.3 Service providers are educated to recognise the right to have an
advocate/support person present and identify and appropriately address situations
where an advocate/support person is not possible or appropriate.
under
Released
3
EXECUTIVE SUMMARY – PART 3
PART 1.3 CONTINUUM OF SERVICE DELIVERY
Consumers participate in and receive timely assessment, followed by services that are planned, coordinated and delivered in a timely and appropriate manner,
consistent with current legislation.
1982
Standard 1.3.1 Entry to Services
Consumers’ entry into services is facilitated in a competent, equitable, timely and respectful manner, when their need for services has been identified.
Evidence
Act
1.3.1.1 Access processes and entry criteria are clearly documented, and are
File 1.
Evidence
Y
communicated to consumers, their family/whanau of choice where appropriate, local
communities and referral agencies.
File 2.
Y/N
File 3.
Y/N
File 4.
Y/N
File 5.
Y/N
1.3.1.3 Adequate and accurate information about the service is made available.
Information
1.3.1.4 Entry criteria, assessment and entry screening processes are documented and
clearly communicated to consumers, their family/whanau of choice where appropriate,
local communities, and referral agencies.
Offical
MHA only and Acute, secondary or tertiary services only
File 1.
Evidence
Y/N
1.3.1.5
To facilitate appropriate and timely entry to the service, a system is
File 2.
Y/N
the
implemented to prioritise referrals and identify potential risks for each consumer,
File 3.
Y/N
including considering previous risk management plans.
File 4.
Y/N
File 5.
Y/N
under
Released
4
Standard 1.3.3 Service Provision Requirements
Consumers receive timely, competent, and appropriate services in order to meet their assessed needs and desired outcomes/goals.
Evidence
1.3.3.2 Each stage of service provision (assessment, planning, provision, evaluation,
File 1.
Evidence
N
review, and exit) is developed with the consumer, and where appropriate their
family/whanau of choice or other representatives as appropriate.
File 2.
Y/N
File 3.
Y/N
1982
File 4.
Y/N
File 5.
Y/N
Act
1.3.3.3Each stage of service provision (assessment, planning, provision, evaluation,
File 1.
Evidence
N
review, and exit) is provided within time frames that safely meet the needs of the
consumer. Reference national KPIs – F/F assessment within 3 weeks of referral review
weekly
File 2.
Y/N
File 3.
Y/N
File 4.
Y/N
Information
File 5.
Y/N
1.3.3.4 The service is coordinated in a manner that promotes continuity in service
File 1.
Evidence
Y
delivery and promotes a team approach where appropriate.
Offical
File 2.
Y/N
the
File 3.
Y/N
File 4.
Y/N
under
File 5.
Y/N
Released
5
(as applicable)
Y/N
MHA only
1.
3.3.5 The service provides information about the consumer’s physical and mental
health and well-being to the consumer, their family/whanau of choice where appropriate
and other services it has links with.
1.
3.3.6 The service works to reduce as far as possible the impact and distress of ongoing
1982
mental illness, and provides or facilitates access to information, education, and
programmes for consumers and family/whanau, to reduce psychiatric disability, prevent
relapse, promote wellness and optimal quality of life for the consumer.
Act
This shall include, but is not limited to:
a) Consumer support group referrals;
b) Education programmes;
c) Consultation and liaison with community groups or relevant self-help groups.
Standard 1.3.4 Assessment
Consumers’ needs, support requirements and preferences are gathered and recorded in a timely manner.
Information
Evidence
1.3.4.2 The needs, outcomes and/or goals of consumers are identified via the
assessment process and are documented to serve as the basis for service delivery
planning.
Offical
Standard 1.3.5 Planning
Consumers’ service delivery plans are consumer focussed, integrated and promote continuity of service delivery.
the
Evidence
1.3.5.1 Service delivery plans are individualised, accurate and up to date.
File 1.
Evidence
N
File 2.
Y/N
under
File 3.
Y/N
File 4.
Y/N
File 5.
Y/N
Released
6
1.3.5.2 Service delivery plans describe the required support and/or intervention to
File 1.
Evidence
N
achieve the desired outcomes identified by the ongoing assessment process.
File 2.
Y/N
File 3.
Y/N
File 4.
Y/N
File 5.
Y/N
1982
1.3.5.3 Service delivery plans demonstrate service integration.
Act
MHA only
File 1.
Evidence
Y/N
1.3.5.4
The service delivery plan identifies early warning signs and relapse prevention.
The plan is developed in partnership with the consumer, the service provider, and
family/whanau if appropriate
File 2.
Y/N
File 3.
Y/N
Information
File 4.
Y/N
File 5.
Y/N
Offical
1.3.5.5 The service delivery plan is communicated in a manner that is understandable to
File 1.
Evidence
Y/N
the consumer and service provider responsible for its implementation and with the
the
consumer’s consent, their family/whanau of choice.
File 2.
Y/N
File 3.
Y/N
under
File 4.
Y/N
File 5.
Y/N
Released
7
Standard 1.3.6 Service Delivery/Interventions
Consumers receive adequate and appropriate services in order to meet their assessed needs and desired outcomes.
Evidence
1.3.6.1 The provision of services and/or interventions are consistent with, and
contribute to, meeting the consumers’ assessed needs, and desired outcomes.
MHA only
File 1.
Evidence
Y/N
1.3.6.3
The consumer receives the least restrictive and intrusive treatment and/or
support possible.
File 2.
Y/N
1982
File 3.
Y/N
Act
File 4.
Y/N
File 5.
Y/N
1.3.6.4 The consumer receives safe and respectful services in accordance with current
File 1.
Evidence
Y
accepted good practice, and which meets their assessed needs, and desired outcomes.
File 2.
Y/N
File 3.
Y/N
Information
File 4.
Y/N
File 5.
Y/N
MHA only
Y/N
Offical
1.3.6.5
The consumer receives services which:
(a) Promote mental health and well-being;
the
(b) Limit as far as possible the onset of mental illness or mental health issues;
(c) Provide information about mental illness and mental health issues, including
prevention of these;
(d) Promote acceptance and inclusion;
under
(e) Reduce stigma and discrimination
This shall be achieved by working collaboratively with consumers, family/whanau of
choice if appropriate, health, justice and social services, and other community groups.
Released
8
Standard 1.3.8 Evaluation
Consumers’ service delivery plans are evaluated in a comprehensive and timely manner.
Evidence
1.3.8.1 Evaluations are conducted at a frequency that enables the regular monitoring of
File 1.
Evidence
Y
progress towards achievement of desired outcomes.
File 2.
Y/N
File 3.
Y/N
1982
File 4.
Y/N
Act
File 5.
Y/N
1.3.8.2 Evaluations are documented, consumer-focussed, indicate the degree of
File 1.
Evidence
N
achievement or response to the support and/or intervention, and progress towards
meeting the desired outcome.
File 2.
Y/N
File 3.
Y/N
Information
File 4.
Y/N
File 5.
Y/N
Offical
1.3.8.3 Where progress is different from expected, the service responds by initiating
the
changes to the service delivery plan.
under
Released
9
Standard 1.3.9 Referral to Other Health and Disability Services (Internal and External)
Consumer support for access or referral to other health and/or disability service providers is appropriately facilitated, or provided to meet consumer choice/needs.
Evidence
1.3.9.1 Consumers are given the choice and advised of their options to access other
health and disability services where indicated or requested. A record of this process is
maintained.
1982
Standard 1.3.10 Transition, Exit, Discharge or Transfer
Consumers experience a planned and co-ordinated transition, exit, discharge or transfer from services.
Evidence
Act
1.3.10.1 Service providers facilitate a planned transition exit, discharge or transfer in
File 1.
Evidence
N
collaboration with the consumer whenever possible and this is documented,
communicated and effectively implemented.
File 2.
File 3.
File 4.
Information
File 5.
1.3.10.2 Service providers identify, document and minimise risks associated with each
File 1.
Evidence
Offical
N
consumer’s transition, exit, discharge or transfer, including expressed concerns of the
consumer and, if appropriate, family/whanau or choice or other representatives.
the
File 2.
File 3.
File 4.
under
File 5.
Released
10
Standard 1.3.12 Medicine Management
Consumers receive medicines in a safe and timely manner that complies with current legislative requirements and safe practice guidelines.
Evidence
1.3.12.1 A medicines management system is implemented to manage the safe and appropriate
prescribing, dispensing, administration, review, storage, disposal and medicine reconciliation in
order to comply with legislation, protocols and guidelines.
1.3.12.3 Service providers responsible for medicine management are competent to perform the
function for each stage they manage.
1982
1.3.12.4 A process is implemented to identify, record and communicate a consumer’s medicine-
related allergies or sensitivities and respond appropriately to adverse reactions or errors.
1.3.12.5 The facilitation of safe self-administration of medicines by consumers where
Act
appropriate.
1.3.12.6 Medicine management information is recorded to a level of detail, and communicated
to consumers at a frequency and detail to comply with legislation and guidelines.
MHA only 1.3.12.7 Continuity of treatment and support is promoted by ensuring the views of the
(As Applicable)
Evidence
consumer, their family / whanau of choice where appropriate, and other relevant service
Y/N
File 1.
providers, for example GPs, are considered and documented prior to administration of new
medicines and any other medical interventions.
Information
File 2.
Y/N
File 3.
Y/N
File 4.
Y/N
Offical
File 5.
Y/N
ALL Variances:
TOTAL
the
to be written as an Action plan ( see next page)
Y/N
Discussed at team quality meeting
Y/N
/5
Presented at MHOLG
Y/N
/100%
under
Released
11
MENTAL HEALTH & ADDICTION SERVICE AUDIT ACTION PLAN
ACTION PLAN
TEAM:
DATE: //
AUDIT IDENTIFIED:
Issue identified as
Steps Needed to rectify issue
By Whom
Reported to
Follow up audit to be
needing plan
done by
1982
EXAMPLE
- All staff to be aware of requirement to complete
Jo Bloggs
Monthly business
Jo Bloggs 21.5.17
Standard 1.3.7
Consumers are
family violence screening
meeting
kept safe and are not subjected
-
(C.M)
Act
to, or at risk, of, abuse and/or
Have all staff completed the revised Family -Violence
training?
neglect.
If no, complete a PDSA.
Evidence of this occurring is Discuss at team business meeting
staff completion of family
If yes Re Audit in 4 weeks
violence screening
3 out of 5 files evidenced
1.
Information
2.
3.
Offical
4.
the
5.
6.
under
7.
Released
12
APPENDIX 2
POLICY
TE MĀTĀPUNA O TE ORA, MENTAL HEALTH & ADDICTION
SERVICES (MHAS)
INTERDISCIPLINARY PLANNING AND REVIEW
Applicable to:
All registered clinical and
Issued by:
non-registered support staff working in
Mental Health & Addiction Services
Te Uru Rauhī Mental Health & Addiction
Services
Contact:
Operational Executive
STATEMENT OF COMMITMENT TO TE TIRITI O WAITANGI:
Te Uru Rauhi-Mental health and Addiction Services are committed to ensuring an authentic treaty
partnership is upheld.
Article I (Kawanatanga) as tangata tiriti we are kaitiaki (stewards) of the health and disability
1982
system.
Act
Article II (Tino Rangatiratanga) we are responsible partners who enable Māori to exercise
authority over their own health and well-being.
Article III (Oritetanga) to achieve equitable health outcomes for Māori.
The Ritenga declaration identifies the importance of enabling Māori to thrive live and flourish as
Māori by having access to rongoā, supporting access to culturally responsive mātauranga inclusive
services and through investing in kaupapa Māori service delivery.
Information
Te Uru Rauhi are committed to working in partnership with Pae Ora Paiaka Whaiora Hauora Māori
Directorate to improve health outcomes for Māori are a committed to reducing the significant
inequities that exist for Māori. Te Mātāpuna o te Ora is a connected care approach that proactively
supports whānau transition seamlessly across teams to best support whaiora recovery outcomes and
Offical
wellbeing
the
As part of our commitment Te Uru Rauhi will ensure culturally responsive practices are interwoven
across service and delivery design utilising whānau Māori, iwi and kaupapa Māori services are
engaged to ensure the voice of Māori is captured and responded to using a whānau centred approach.
whānau-centred refers to the idea that service design and delivery must meet the needs of whānau
under
first and foremost. Whānau-centred means delivering a service response that is informed and
accountable to whānau aspirations. Whānau-centred ways of working are strengths based, grounded
in aroha, and well resourced. Whānau-centred is a commitment to provide a multi-layered approach
to whānau requiring support.
All staff are to be always familiar with MDHB Te Tiriti O Waitangi policy MDHB 2031 and work in a
culturally aware manner. Improving health outcomes for Māori is a key obligation from an equity
Released
perspective. Locally Sir Mason Duries work is embraced to support wellbeing models of care. Te
Whare Tapa Wha as a common wellbeing practice model.
Document No: MDHB-6431
Page 1 of 11
Version: 5
Prepared by: Service Development Lead, Mental Health and Addiction Services
Issue Date: 07/Jun/2022
Authorised by: Nurse Director, Mental Health Services
https://thoughtnz-my.sharepoint.com/personal/rodger_thought_co_nz/Documents/MCHpolicy/MDHB 6431 - IDP Review -Policy-v5.doc
© MidCentral District Health Board 2022.
CONTROLLED DOCUMENT. The electronic version on the Control ed Documents site is the
most up-to-date version. MDHB wil not take any responsibility in case of any outdated paper or electronic copy being used and leading
to any undesirable consequence.
Printed 27/01/2024 4:24:00 pm
Policy for Interdisciplinary Planning and Review
1.
PURPOSE
To set Te Mātāpuna o te Ora, Specialist Mental Health and Addiction Service expectations for
Interdisciplinary Planning and review (IDP) processes. (Kaupapa services align to whānau Ora
and Hui for IDP.)
The central aim of the IDP is to improve health outcomes of whānau whaiora accessing Te
Mātāpuna o te Ora service and the wider Connected Care Network. The strength of the IDP
process is derived from the use of shared knowledge and perspective to best optimise progress
to Wellbeing Recovery for whanau whaiora.
IDP meetings are the forum for planning and reviewing interventions to support whānau
whaiora Wellbeing Recovery.
2.
SCOPE
1982
All registered clinical and unregulated staff working with whānau whaiora, Te Mātāpuna o te
Act
Ora, Mental Health and Addiction Services.
3.
ROLES & RESPONSIBILITIES
3.1 The Interdisciplinary process
The Connected Care Network is a whole of life/whole system. It provides a whānau whaiora
Information
centred approach that acknowledges Te Whare Tapa Wha as a holistic model of care to support
inclusive, adaptive, clinically, and culturally responsive service delivery. Whānau whaiora
access services within the network where engagement is a central aspect of the Wellbeing
Recovery partnership.
Offical
The most appropriate service to meet whānau whaiora needs is to be determined clinically and
culturally within the interdisciplinary planning and review process. The interdisciplinary
the
process is inclusive of different roles and professional disciplines contributing to connected care
in collaborative partnership with whānau whaiora.
The care team consists of the whānau whaiora, clinicians and unregulated support roles directly
involved in service provision to w
under hānau whaiora. They form the core interdisciplinary group
that supports development and review of the Wellbeing Recovery Plan (WRP) ensuring a
strengths-based Wellbeing Recovery focus and clearly identified whānau whaiora goals,
timelines and established progress to Wellbeing Recovery.
Recognition of the different professional bodies and the clinician’s professional scope and
responsibilities is considered during the Interdisciplinary process.
Released
The responsible/accountable/consulted/informed (RACI) matrix is a tool that identifies roles
and responsibilities within the Interdisciplinary team and helps formulate the varied level of
engagement different professionals have. A description of this model as it applies to Te
Mātāpuna o te Ora may be found in the Te Mātāpuna o te Ora Operational Manual.
3.2 Lead facilitator
Facilitates the Connected Care Network model and service response ensuring timely
assessment, evidence informed intervention and progress toward Wellbeing Recovery. Ongoing
clinical review is applied to understand whānau whaiora experience, engagement, and
Wellbeing Recovery. The Lead Facilitator oversees service audits and applies whānau whaiora
Document No: MDHB-6431
Page 2 of 11
Version: 5
https://thoughtnz-my.sharepoint.com/personal/rodger_thought_co_nz/Documents/MCHpolicy/MDHB 6431 - IDP Review -Policy-v5.doc
Printed 27/01/2024 4:24:00 pm
Policy for Interdisciplinary Planning and Review
feedback to support service quality and improvement. They ensure the IDP and quality process
guide service delivery and whānau whaiora goals toward wellbeing recovery.
The Interdisciplinary and review process will be facilitated by lead facilitators or delegates with
whanau whaiora playing a significant role.
3.3. The Care Co-ordinator
Care Co-ordination is a process within Te Mātāpuna o te Ora. Care Co-ordinator function may
be allocated to any role or discipline based within any team across the Connected Care Network
of Te Mātāpuna o te Ora. This may include Primary Care, iwi providers or NGO partners. The
Care Co-ordinator is responsible for:
•
Build trust and confidence as the main point of contact for whānau whaiora during their
Wellbeing recovery journey.
•
To ensure that whānau whaiora voice and participation is part of the Connected Care
Network on their Wellbeing Recovery journey.
1982
•
Ensures that documents and records pertaining to whānau whaiora are maintained and
reviewed within required timeframes.
Act
3.4 Medical Staff
Medical staff support the interdisciplinary process, taking responsibility for the care and
treatment of whānau whaiora who require specialist medical assessment, diagnosis, treatment
and the integration of biological and psycho-social factors relating to their distress. These
medically focused aspects of care, support and responsibility are in turn, supported by the
interdisciplinary process within the integrated connected continuum of care. In addition to
Information
providing medical services based in Locality Mental Health Centres, Doctors will provide
consult-liaison services within primary health clinics, NGOs and may undertake assessments in
the homes of whānau whaiora in collaboration with other team clinicians.
3.5 Psychologists
Offical
Psychologists contribute to the care coordination approach through application of their
the
specialist skills in assessment, case conceptualisation, formulation, as well as diagnosis of
mental health and / or addiction presentations. They are trained in using and interpreting
psychological tests and integrating that information into assessments to inform care. They can
provide a valuable perspective and guidance to the Interdisciplinary Team in treatment, risk
under
assessment and safety planning for complex cases.
Psychologists possess advanced knowledge and skills in delivering evidence based psychological
interventions and psychological therapies (eg CBT, DBT, MI, ACT, brief solution focused
therapy, family therapies, mindfulness based and metacognitive therapy) to people with a wide
range of clinical presentations. These interventions may be provided at the level of the whānau
whaiora, or group, across the continuum of severity. Psychologists may deliver psychotherapies
Released
directly to whānau whaiora or support other clinicians to deliver these interventions through the
provision of supervision, consultation, training, education, or programme design and delivery.
3.6 Nursing
Mental Health and Addiction Nurses are Registered Nurses who hold specialised post-graduate
qualifications and post-registration training in talking therapies in the field of Mental Health
and Addictions across primary, community and inpatient health services. The nurse provides
recovery orientated comprehensive care which includes health education, health promotion and
illness prevention, assessment, diagnosis, intervention, treatment and evaluation in a variety of
settings along the continuum of care and across the lifecycle. Within the context of Mental
Health and Addiction care, the nurse addresses whānau whaiora psycho-social and physical
Document No: MDHB-6431
Page 3 of 11
Version: 5
https://thoughtnz-my.sharepoint.com/personal/rodger_thought_co_nz/Documents/MCHpolicy/MDHB 6431 - IDP Review -Policy-v5.doc
Printed 27/01/2024 4:24:00 pm
Policy for Interdisciplinary Planning and Review
health care needs and ensures through direct care provision or referral, consultation and
co-ordination of care processes, that care is individualised and integrated in the context of
whānau whaiora social and cultural context.
Alongside care planned in partnership with whānau whaiora, nurses hold delegated
responsibility for enrolled nurses, community and peer support staff and supervision within the
credentialled process for Practice Nurses within primary care. Nurses undertake the role of a
Duly Authorised Officer and Registered Health Professional under Mental Health and Drug and
Alcohol legislation. Within the Interdisciplinary Planning Process, nurses are lead facilitators of
the Flexible Assertive Assessment Team (FACT) and unplanned care programmes. They also
lead nurse led services within primary and community care settings as well as acute care
responses across the continuum. Mental Health Nurses recognise the need for flexibility,
adaptability, responsiveness, and sensitivity as they shape their practice to the changing needs
of whānau whaiora and communities.
3.7 Social Work
1982
Social Workers mahi in partnership with whānau whaiora using strengths based and non-
judgemental interventions which are underpinned by research informed models of practice.
Act
They incorporate analyses of current and historical influences including ecological, social,
political, economic, spiritual, and psychological factors. They work to empower whānau whaiora
to achieve their goals and aspirations for well-being while building on their sense of belonging
and connectedness with their whanau, community and wider society. They help whānau
whaiora to access the resources they need to construct solutions in their lives. Social Workers
are committed to creating mana-enhancing relationships which are congruent with our
obligations under Te Tiriti o Waitangi. They strive to challenge injustice, oppression and
inequity in all daily relationships as well as in organisational, community and societal
Information
structures.
3.8 Occupational Therapy
Occupational therapists /nga kaiwhakaora ngangahau skills involve using occupation to
Offical
improve, maintain, and restore health and wellbeing by working in partnership with whānau
whaiora to connect or reconnect them with the everyday tasks they need and want to do. It is
the
about Whānau whaiora “doing what matters” and “purposeful doing”.
Occupation is defined as “…everything people do to occupy themselves, including looking after
themselves, enjoying life, and contributing to the social and economic fabric of their
communities”.
under
Occupational domains include self-care, productivity, leisure, and socialisation
Occupational therapy interventions in Mental Health and Addictions can be broadly grouped
into the
following themes:
1.
Interventions in employment or education: supported employment, supported education,
Released
other employment interventions.
2. Occupational therapy interventions involving psycho-education.
3.
Occupational therapy interventions using creative occupation or activity.
4. Occupational therapy interventions addressing time use or occupational balance.
5.
Occupational Therapy interventions in skills development (functional assessments),
lifestyle modification and occupational engagement.
6. Occupational therapy interventions using group or whānau whaiora approaches.
7.
Sensory interventions that support engagement in occupation.
8. Occupational therapy interventions using animals or animal assisted approaches.
Document No: MDHB-6431
Page 4 of 11
Version: 5
https://thoughtnz-my.sharepoint.com/personal/rodger_thought_co_nz/Documents/MCHpolicy/MDHB 6431 - IDP Review -Policy-v5.doc
Printed 27/01/2024 4:24:00 pm
Policy for Interdisciplinary Planning and Review
3.9 AOD Clinicians
A competent addiction practitioner works effectively within the scope of their practice to
support community wellbeing and reduce harm related to alcohol and other drugs. This is
demonstrated by working in collaboration with whānau whaiora using evidence informed theory
and knowledge of alcohol and other drug addiction and co-existing problems to assess, plan,
provide and evaluate intervention tailored to the strengths and needs of whānau whaiora. The
intervention may include working in collaboration with the withdrawal management team,
residential treatment facilities, and other specialist Mental Health and Addiction Services as
required.
A competent addiction practitioner understands the impact of stigma and discrimination and
role model strategies to both reduce and challenge stigma and promote social inclusion across
Mental Health Services and the wider community. An understanding of group process and
dynamics in addiction practice is essential together with the capacity to lead in the facilitation
1982
and development of groups to support clients and whānau in their recovery. Can demonstrate
an expert level of knowledge in a range of motivational strategies that support the client’s
treatment goal of either harm reduction or abstinence and is able to work collaboratively with
Act
whānau whaiora to achieve their goals.
3.10 Kairaranga
A Kairaranga (Primary whānau whaiora Care Co-ordinator) will follow the whānau whaiora
from community to acute and back out to community to ensure consistency and that whānau
whaiora will maintain a closer to home approach to their care. The whānau ora methodology
will be a key focus to the coordination and treatment pathway in the we
Information llbeing recovery plans
supported by the Kaiaraara link and Whanau ora Kaitautoko roles.
3.11 Whānau Ora Kaitautoko
Offical
The Whānau Ora Kaitautoko role is a key support for whānau ora centred approach, promoting
Māori responsive quality care with particular attention to supporting and facilitating seamless
pathways. This role is the link with othe
the r established Kaiaraara whānau link roles in the
community and DHB supporting senior clinicians and kaimahi with care planning and support
to services.
3.12 Responsible Clinician
under
The Responsible clinician has an enhanced role in IDP reviews for whānau whaiora supported
under a Compulsory Treatment Order of the Mental Health Act. For more information about
this, please refer below to the Guidelines to the Mental Health compulsory assessment and
treatment Act 1992 (2021 Ministry of Health).
https://www.tepou.co
Released
.nz/initiatives/guidelines-to-the-mental-health-compulsory-assessment-
and-treatment-act-1992
3.13 Interdisciplinary Planning IDP partners
•
Present to the IDP in the required timeframe as identified in this Policy.
•
Use the IDP review content guide within this Policy as a framework for thinking.
•
Follow the procedure and processes for IDP presentation.
•
The IDP process is inclusive of key partners to support wellbeing recovery planning.
•
IDP partners are responsible for delivery against agreed interventions and therapies as
shared responsibility is fundamental to an interdisciplinary model.
Document No: MDHB-6431
Page 5 of 11
Version: 5
https://thoughtnz-my.sharepoint.com/personal/rodger_thought_co_nz/Documents/MCHpolicy/MDHB 6431 - IDP Review -Policy-v5.doc
Printed 27/01/2024 4:24:00 pm
Policy for Interdisciplinary Planning and Review
•
Whānau whaiora presence or voice is an integral part of the IDP process, the Care Co-
ordinator function facilitates how this may best to occur, in person, representative,
advocate or other medium and document how this has occurred.
•
The central aim of the IDP is to bring together key people to ensure best therapeutic
interventions and treatments for progress to wellbeing recovery to be achieved in
partnership with whānau whaiora.
4.
PREREQUISITES
Each service team establishes a culture of regular IDP procedure and meeting schedule that is
inclusive of key interdisciplinary professionals, whānau whaiora. In the community localities the
Care Co-ordinator is responsible for overseeing and recording attendance at scheduled
meetings.
5.
POLICY
1982
Key registered and non-registered health professionals in collaborative partnership with
Act
whānau whaiora should be present at the scheduled IDP meetings (eg allied health, medical
staff, nursing, and whānau whaiora. Whānau whaiora presence or voice is an integral aspect of
collaborative planning).
Te Whare Tapa Wha as a wellbeing model will guide the IDP process.
Key health professional staff within Te Mātāpuna o te Ora, have a responsibility to attend
scheduled Interdisciplinary planning and review meetings (community and acute care) related
Information
to a whānau whaiora in their care unless an emergency/crisis occurs.
5.1 Community Localities, Mental Health and Addiction Services
All clinical staff to ensure they present whānau whaiora to IDP reviews within the following
Offical
timeframes:
the
•
Initial assessments are presented through the IDP process at the earliest opportunity but
not more than seven (7) working days by Care Co-ordinator outlining intervention plan
and outcome pathway to wellbeing recovery.
•
IDP reviews occur on average every three (3) months or earlier based on safety and need.
under
Outcomes and goal attainment drive interdisciplinary discussion and proposed adaptions
to intervention plans.
•
The IDP and review process is mindful that safety is a variable feature of mental distress.
•
IDP reviews document who is accountable for what action, intervention and therapy to
ensure recovery pathways are supported and evaluated against action goals and expected
progress toward Wellbeing Recovery.
•
Any variation to the three monthly review must be clearly documented with clinical
Released
rationale, whānau whaiora inclusion and will include a review date for the next IDP.
5.2 Acute Care Inpatient Setting
•
Care Co-ordinators should be involved as much as practical in all IDP even if whānau
whaiora are inpatient at the time.
•
IDP Reviews for inpatients/ whānau whaiora will occur weekly. Inpatient stays need to
plan treatment and interventions as promptly as possible to begin transfer of care back to
the community from the day of admission. IDP reviews must therefore be scheduled at
time of admission for as soon as practical within each week.
•
IDP Reviews are to be documented the same day the IDP occurs.
Document No: MDHB-6431
Page 6 of 11
Version: 5
https://thoughtnz-my.sharepoint.com/personal/rodger_thought_co_nz/Documents/MCHpolicy/MDHB 6431 - IDP Review -Policy-v5.doc
Printed 27/01/2024 4:24:00 pm
Policy for Interdisciplinary Planning and Review
•
Documented IDP reviews will be discussed with all whānau whaiora who have not
participated in IDP. They will be able to document any changes to the plan that they
require. Whānau whaiora voice must be present and documented in the IDP process to
ensure intervention and wellbeing recovery planning is in line with whānau whaiora goals.
•
IDP reviews will plan and document intervention, therapy, and transition plans to support
seamless service delivery. These will be communicated to the community team / care co-
ordinator if they have not been able to participate in the IDP.
•
IDP reviews will be communicated to the whānau whaiora and significant others.
Responsibility for this will be documented on the IDP form but would usually be the Care
Co-ordinator.
•
All community transitions from the Acute Care Centre must be able to evidence
involvement of whānau whaiora in the transition planning. Where a face-to-face meeting
about transition is impractical there should be all reasonable steps taken eg use of
technology mediums, and documented to ensure whānau whaiora inclusion.
6.
RECORDING IDP PROGRESS TO WELLBEING RECOVERY
1982
•
IDP reviews are to be documented on the day they occur.
Act
•
IDP reviews are recorded against the whānau whaiora NHI using IDP three monthly or
IDP six monthly.
•
The Care Co-ordinator presenting the whānau whaiora at IDP review records the ‘IDP’
against the whānau whaiora NHI and submits this data.
•
Individual outcome data as agreed in the outcomes framework must be entered to
evidence progress against outcomes.
•
Medical, Nursing and Allied health accountability is evaluated against recovery and action
goals of the Wellbeing Recovery Plan of care, intervention, treatm
Information ent and therapy
documented through the IDP process.
•
The clinical rationale for exceptions to three monthly reviews are recorded.
Offical
7.
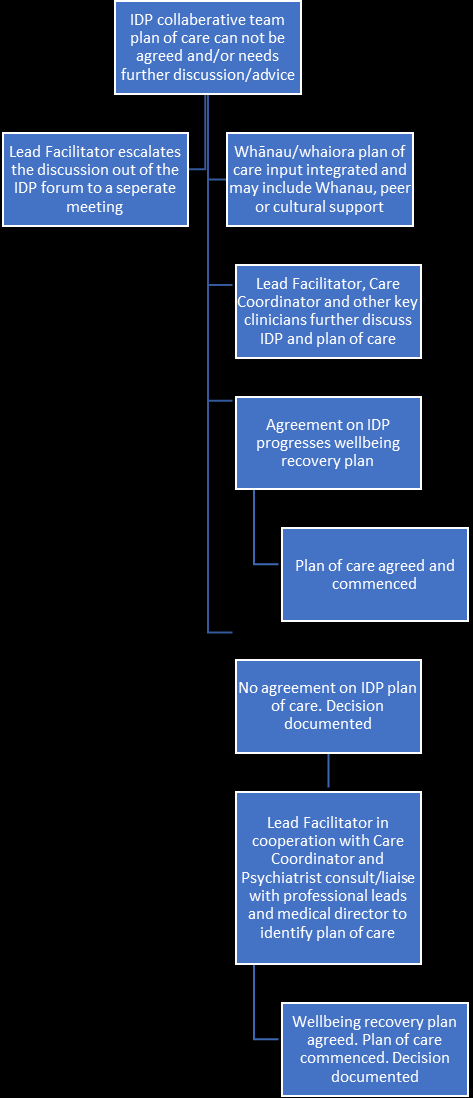
IDP WELLBEING RECOVERY PLANNING AND DISPUTE RESOLUTION
If within the IDP meeting timeframe a
the consensus could not be reached, further discussions are
to occur outside the IDP process. This follow up would be driven by the Care Co-ordinator
and/or Lead Facilitator. Flowchart, Appendix 1.
If whānau whaiora are not satisfied with the Interdisciplinary Planning decision process they
under
may be referred and supported to the MDHB complaints process.
Released
Document No: MDHB-6431
Page 7 of 11
Version: 5
https://thoughtnz-my.sharepoint.com/personal/rodger_thought_co_nz/Documents/MCHpolicy/MDHB 6431 - IDP Review -Policy-v5.doc
Printed 27/01/2024 4:24:00 pm
Policy for Interdisciplinary Planning and Review
8.
IDP REVIEW SHOULD INCLUDE THE FOLLOWING CONTENT:
Reason for review
Care Co-ordinator to outline what they are
seeking from the IDP review to support
whānau whaiora wellbeing recovery.
Who they are presenting
Whānau whaiora details, circumstances
relating to the referral, ie how, by who and
when, cultural considerations, iwi, hapu, social
situation, social support, agencies involved.
Brief background
Past mental health history and /or alcohol and
1982
other substance use and involvement with
services. Te Whare Tapa Wha model may be
Act
used identifying strengths and relationships.
Presenting issues
Presenting health issues – physical
health/metabolic screening/monitoring,
mental health and/or alcohol & other drug use
(duration, severity & impact) and any
significant life events that are impacting on the
Information
individual currently. Changes within the last
three (3) months. All inter-related aspects of
wellbeing must be considered for whānau
whaiora with multiple identified needs.
Offical
Legal Status
Confirm whānau whaiora current legal status
the
identifying which Act the whānau whaiora is
under eg Mental Health Act, SACAT, PPPR,
IDCCR.
under
The IDP and review process is
Specific actual or potential safety concerns to
mindful that safety and risk is
self or others, either intentional or otherwise
a variable feature of mental
and broad contributing factors, eg depression,
distress
age, sex, loss, alcohol, relationships.
Released
Clinical
Diagnostic or clinical impression or working
impression/formulation
diagnosis conceptualised as factors that are:
• Predisposing
• Precipitating
• Perpetuating
• Protective
Whānau whaiora input and cultural
considerations help inform this.
Document No: MDHB-6431
Page 8 of 11
Version: 5
https://thoughtnz-my.sharepoint.com/personal/rodger_thought_co_nz/Documents/MCHpolicy/MDHB 6431 - IDP Review -Policy-v5.doc
Printed 27/01/2024 4:24:00 pm
Policy for Interdisciplinary Planning and Review
Health Outcome Measure,
progress toward wellbeing
Wellbeing score, ADOM, HoNOS, HoNOSCA,
recovery
Hua Oranga or another outcome measure:
• If new to service – what is the score.
• If existing whānau whaiora – what
change has there been since the last
IDP?
Wellbeing Recovery Plan
If whānau whaiora is new to the service then
what are the proposed next steps (what does
the whānau whaiora want, and what does the
presenting clinician think needs to happen)
If current whānau whaiora with current
intervention, treatment plan (what is working
1982,
what isn’t, propose what needs to change, who
needs to be involved).
Act
Transition Plan – Relapse Plan Prior to transition whānau whaiora need a
wellness recovery plan (within WRP)
identifying early warning indicators, relapse
indicators and historical interventions that
have been helpful.
Information
Intensive/Complex
This occurs when a whānau whaiora has
Interdisciplinary Planning
multiple layers of need and is considered
complex in nature for intervention,
treatment/
Offical therapy. This may require extended
IDP support and timeframes for whānau
whaiora who require specific intervention and
the therapy. Some may not sit naturally within the
F.A.C.T model and delivery team. This
supports case by case continued support in
short to medium care team.
under
Record of Presence
To be maintained with key actions and
timeframes.
Use of agreed IDP template
Clearly documented.
Released
9.
PROGRESS TOWARD WELLBEING RECOVERY
Whānau whaiora progress toward wellbeing recovery is a primary focus of Te Mātāpuna o te
Ora. For the duration of engagement throughout the Connected Care Network multiple
assessment tools and measures will be used to understand the impact of interdisciplinary
planning and evidence informed therapy interventions. The monitoring and reporting
framework to support the understanding of progress toward wellbeing recovery is to be
developed and agreed. This may include existing and new measures.
Document No: MDHB-6431
Page 9 of 11
Version: 5
https://thoughtnz-my.sharepoint.com/personal/rodger_thought_co_nz/Documents/MCHpolicy/MDHB 6431 - IDP Review -Policy-v5.doc
Printed 27/01/2024 4:24:00 pm
Policy for Interdisciplinary Planning and Review
10. RELATED MDHB DOCUMENTS
MDHB-2031
Te Tiriti O Waitangi - policy
MDHB-5451 Mental Health IDP Review - Form Template
MDHB-7435 Te Mātāpuna o te Ora Mental Health and Addiction Connected Care Network
MDHB-255
Safety planning - Policy
MDHB-6853 Service User, Family Whānau Engagement - policy
MDHB-2767
Care Co-ordinator Roles and Responsibilities -Procedure-
MDHB-248 Te Mātāpuna o te Ora Wellbeing Recovery Planning -Policy-
Te Mātāpuna o te Ora Operational Manual
11. FURTHER INFORMATION / ASSISTANCE
Operational Leads
1982
Locality / Service Managers
Lead Facilitators
Act
Acute Care Charge Nurse
Medical Director
Associate Director of Nursing
Associate Director of Allied Health,
Clinical Governance Group
Information
Offical
the
under
Released
Document No: MDHB-6431
Page 10 of 11
Version: 5
https://thoughtnz-my.sharepoint.com/personal/rodger_thought_co_nz/Documents/MCHpolicy/MDHB 6431 - IDP Review -Policy-v5.doc
Printed 27/01/2024 4:24:00 pm
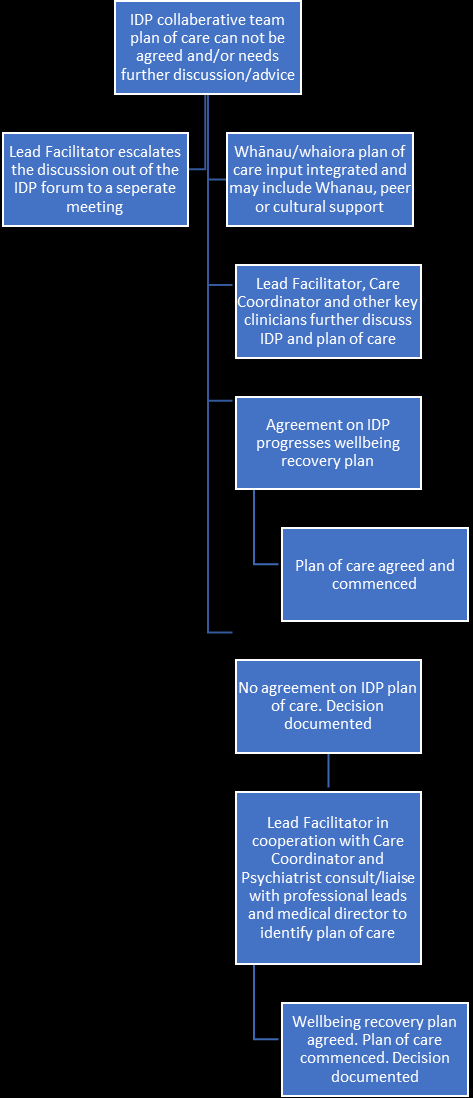
Policy for Interdisciplinary Planning and Review
APPENDIX 1
Resolution Flowchart
The flow chart is a quick reference guide to support a process of enhanced professional
discussion within the collaborative interdisciplinary team approach. Focusing on
shared decision making using a recovery strengths-based focus on solutions and
outcomes in partnership with whānau whaiora presentation and needs.
1982
Act
Information
Offical
the
under
Released
Document No: MDHB-6431
Page 11 of 11
Version: 5
https://thoughtnz-my.sharepoint.com/personal/rodger_thought_co_nz/Documents/MCHpolicy/MDHB 6431 - IDP Review -Policy-v5.doc
Printed 27/01/2024 4:24:00 pm
POLICY
TE MĀTĀPUNA O TE ORA
SPECIALIST MENTAL HEALTH AND ADDICTION SERVICES
WELLBEING RECOVERY PLANNING
Applicable to:
All Staff Te Mātāpuna o te
Issued by:
Mental Health and Addiction
Ora.
Services
Te Uru Rauhī Mental Health and
Contact:
Operations Executive
Addiction Services
STATEMENT OF COMMITMENT TO TE TIRITI O WAITANGI:
Te Uru Rauhī-Mental Health and Addiction Services are committed to ensuring an authentic treaty
1982
partnership is upheld.
Article I (Kawanatanga) as tangata tiriti we are kaitiaki (stewards) of the health and disability
Act
system.
Article II (Tino Rangatiratanga). We are responsible partners who enable Māori to exercise
authority over their own health and well-being.
Article III (Oritetanga) in order to achieve equitable health outcomes for Māori.
The Ritenga declaration identifies the importance of enabling Māori to thrive live and flourish as
Information
Māori by having access to rongoā, supporting access to culturally responsive mātauranga inclusive
services and through investing in kaupapa Māori service delivery.
Te Uru Rauhī are committed to working in partnership with Pae Ora Paiaka Whaiora Hauora Māori
Offical
Directorate to improve health outcomes for Māori and are committed to reducing the significant
inequities that exist for Māori. Te Mātāpuna o te Ora is a connected care approach that proactively
supports whānau transition seamlessly across teams to best support whaiora recovery outcomes and
the
wellbeing
As part of our commitment Te Uru Rauhī will ensure culturally responsive practices are interwoven
across service and delivery design utilising whānau Māori, iwi and kaupapa Māori services are
under
engaged to ensure the voice of Māori is captured and responded to using a whānau centred approach.
Whānau-centred refers to the idea that service design and delivery must meet the needs of whānau
first and foremost. Whānau-centred means delivering a service response that is informed and
accountable to whānau aspirations. Whānau-centred ways of working are strengths based, grounded
in aroha, and well resourced. Whānau-centred is a commitment to provide a multi-layered approach
to whānau requiring support.
Released
All staff are to always be familiar with MDHB Te Tiriti o Waitangi policy MDHB 2031 and work in a
culturally aware manner. Improving health outcomes for Māori is a key obligation from an equity
perspective. Locally Sir Mason Duries work is embraced to support wellbeing models of care. Te
Whare Tapa Wha as a common practice model.
Document No: MDHB-248
Page 1 of 4
Version: 9
Prepared by: Service Development Lead, Mental Health and Addiction Services
Issue Date: 03/Jun/2022
Authorised by: Operations Lead, Specialist Community and Primary Mental Health and Addiction Services
C:\Users\amandaro\Documents\Maternity Guideline & Outcomes Group\Postnatal Assessment and Readmission -Clinical Guideline-.doc
© MidCentral District Health Board 2022.
CONTROLLED DOCUMENT. The electronic version on the Control ed Documents site is the
most up-to-date version. MDHB wil not take any responsibility in case of any outdated paper or electronic copy being used and leading
to any undesirable consequence.
Printed 27/01/2024 4:25:00 pm
Policy for Transition wellbeing plan
Policy for Wellbeing and Recovery Planning
1.
PURPOSE
To outline the requirement of Wellbeing Recovery Planning for all whānau whaiora accessing Te
Mātāpuna o te Ora Mental Health and Addiction services.
The Wellbeing Recovery Plan (WRP) is the foundation of the interdisciplinary collaboration of
all people in the whānau whaiora wellbeing recovery journey and clearly identifies evidence
informed interventions, therapy, treatments, aspirations, and recovery goals.
2.
SCOPE
All staff in Te Mātāpuna o te Ora, Te Uru Rauhī Specialist Mental Health and Addiction
Services. Te Mātāpuna o te Ora is a philosophy and approach that facilitates a whole of
service/system integrated and Connected Care Network. This supports transition seamlessly
across teams to best support whānau whaiora wellbeing recovery goals and outcomes.
1982
3.
ROLES AND RESPONSIBILITIES
Act
3.1
The role of the Interdisciplinary Team in Wellness Recovery Planning
Whānau whaiora access services within the Connected Care Network based on age other factors
that identify the need for flexible, adaptive, and responsive service delivery.
The most appropriate service to meet whānau whaiora needs is to be determined clinically and
culturally within the interdisciplinary planning process. The interdisciplinary process is
inclusive of different professional disciplines contributing to the connected care in collaborative
Information
partnership with whānau whaiora.
The care team consists of the clinicians and support roles directly involved in service provision
to whānau whaiora. They form the core Interdisciplinary Group that supports the development
Offical
and review of the WRP to ensure strengths-based wellbeing recovery focus. Whānau whaiora
goals, timelines and progress toward wellbeing recovery are clearly identified.
the
Recognition of the different professional bodies and the clinician’s professional responsibilities
is considered within wellness recovery planning. The RACI matrix is a tool that identifies roles
and responsibilities within the Interdisciplinary team and helps formulate the varied level of
engagement different professiona
under ls have. A description of this model as it applies to Te
Mātāpuna o te Ora may be found in the Te Mātāpuna o te Ora Operational Manual.
3.2 The Care co-ordinator
Care Co-ordination is a process within Te Mātāpuna o te Ora. The Care co-ordinator function
may be allocated to any role or discipline based within any team across the connected care
Released
network of Te Mātāpuna o te Ora. This may include Primary Care, iwi providers or NGO
partners. The Care Co-ordinator is responsible for:
•
Build trust and confidence as the main point of contact for whānau whaiora during their
Wellbeing recovery journey.
•
To ensure that whānau whaiora voice and participation is part of the Connected Care
Network on their wellbeing recovery journey.
•
Ensures that documents and records pertaining to whānau whaiora are maintained and
reviewed within required timeframes.
Document No: MDHB-248
Page 2 of 4
Version: 9
\\pn-file1\I-Drive\HROD\SERVICEI\Doccont\EXCEL\Checking\IMPORTING\for importing\DMS PPG review\Procedure Template (revised).doc
Printed 27/01/2024 4:25:00 pm
Policy for Transition wellbeing plan
Policy for Wellbeing and Recovery Planning
Kairaranga:
A Kairaranga (primary whānau whaiora care co-ordinator) will follow whānau whaiora from the
community to specialist services and back out to the community. Kairaranga aim to ensure
consistency and that whānau whaiora will maintain a closer to home approach to their care. The
whānau ora methodology will be a key focus to the coordination and treatment pathway in the
wellbeing recovery plans supported by the Kaiaraara link and whānau ora Kaitautoko roles.
3.3
The Lead facilitator
Facilitates the connected care network model and service response ensuring timely assessment,
evidence informed intervention and progress toward wellbeing recovery. Ongoing clinical
review is applied to understand whānau whaiora experience, engagement and wellbeing
recovery. The Lead Facilitator overseas service audits and applies whānau whaiora feedback to
support service quality and improvement. They ensure the IDP and quality process guide service
delivery and whānau whaiora goals toward wellbeing recovery.
1982
The Interdisciplinary and review process will be facilitated by lead facilitators or delegates.
Act
3.4 The Responsible clinician
The Responsible Clinician has an enhanced role in IDP reviews for whānau whaiora supported
under a Compulsory Treatment Order of the Mental Health Act. For more information about
this, please refer below to the Guidelines to the Mental Health Compulsory Assessment and
Treatment Act 1992 (2021 Ministry of Health).
Information
https://www.tepou.co.nz/initiatives/guidelines-to-the-mental-health-compulsory-assessment-
and-treatment-act-1992
3.5
Other roles
Offical
Key responsibilities and accountabilities for each role in relation to wellbeing recovery planning
the
can be found in the relevant job description and in the Te Mātāpuna o te Ora Operational
manual.
under
4.
POLICY
Wellbeing recovery plans must be used across the Connected Care Network and are inclusive of:
•
strengths based approach that support autonomy and self determination
•
Whānau whaiora as a central part of the collaborative partnership
•
developed in partnership with Interdisciplinary Planning (IDP) and whānau whaiora
Released
•
developed with clinical and cultural safety and advocacy support as appropriate for the
whānau whaiora
•
consideration of Kaupapa Māori pathways to support wellbeing recovery planning
•
clinically and culturally safe evidence informed practice delivery of planned interventions
and therapies inclusive of safety planning
•
Documented on the day developed and shared with agreed partners (connected care record)
Where wellbeing recovery plans can not be agreed as part of the Interdisciplinary process refer
to the IDP resolution flowchart (MDHB 6431-Interdiciplinary Planning and Review -policy) to
support decision making and agreement on WRP.
If whānau whaiora are not satisfied with the wellbeing recovery planning they may be referred
and supported to the MDHB complaints process.
Document No: MDHB-248
Page 3 of 4
Version: 9
\\pn-file1\I-Drive\HROD\SERVICEI\Doccont\EXCEL\Checking\IMPORTING\for importing\DMS PPG review\Procedure Template (revised).doc
Printed 27/01/2024 4:25:00 pm
Policy for Transition wellbeing plan
Policy for Wellbeing and Recovery Planning
Please refer to the Te Mātāpuna o te Ora Operational manual for a detailed description of the
WRP process.
5.
DEFINITIONS
Refer to Glossary in the Te Mātāpuna o te Ora Operational manual.
6.
REFERENCES
Transition Planning:
http://www.health.govt.nz/publication/transition-planning-guidelines-infant-child-and-
adolescent-mental-health-alcohol-and-other-drugs
Guidelines to the Mental Health Act:
1982
https://www.tepou.co.nz/initiatives/guidelines-to-the-mental-health-compulsory-assessment-
and-treatment-act-1992
Act
7.
RELATED MDHB DOCUMENTS
Mental Health and Addiction Services
MDHB-2031
Te Tiriti o Waitangi policy
MDHB-7435 Te Mātāpuna o te Ora Mental Health and Addiction Connected Care
Network policy
Information
MDHB-255
Safety planning and risk Policy
MDHB-7173
Risk Assessment Review - Mental Health and Addiction Service -Form-
MDHB-6853 Service User, Family Whānau Engagement Policy
MDHB-2767
Care Coordinator Roles & Responsibilities Procedure
Offical
MDHB-6431 Interdisciplinary Team Planning and Review
Te Mātāpuna o te Ora Operational Manual
the
MidCentral District Health Board
MDHB-2031
Treaty of Waitangi
under
8.
KEYWORDS
Assessment, Wellbeing Recovery Plan, Lead Facilitator, Care co-ordinator, Te Mātāpuna o te
Ora, Mental Health Service, Safety planning and Risk.
Released
Document No: MDHB-248
Page 4 of 4
Version: 9
\\pn-file1\I-Drive\HROD\SERVICEI\Doccont\EXCEL\Checking\IMPORTING\for importing\DMS PPG review\Procedure Template (revised).doc
Printed 27/01/2024 4:25:00 pm
Document Outline