Document 1
Disability Support Services
Operational Policy
DSS Eligibility
Doug Funnell, Contract Relationship Manager,
Author:
Service Access Team, Disability Support Services
Policy Sponsor:
Phil Wysocki, Manager Service Access Team
Date effective:
20 March 2017
Date of expiry:
19 March 2020
Version:
2
Toni Atkinson, Group Manager Disability
Authorised by:
Support Services
Authorisation:
………………………………………..
Date:
………………………
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
1 of 13
link to page 2 link to page 12 link to page 2 link to page 2
Document 1
Purpose
The purpose of this Operational Policy is to define the eligibility for the Ministry of Health’s
(the Ministry) funded disability support services. This policy is intended to support Ministry-
contracted Needs Assessment and Service Coordination organisations (NASCs) to apply a
nationally consistent approach to implementing eligibility criteria.
This Operational Policy explains the process for eligibility determination, presents the
definitions of intellectual, physical and sensory disability and clarifies cross funder
relationships.
The Policy also includes information about the NASC process, high level guidance for
NASCs on funding relationships with DHBs and description of the disability support
services that can be accessed without a NASC assessment.
This Operational Policy is for the use of Ministry staff and NASCs.
Scope
This is a national Operational Policy.
Background
In 1992, under the “New Dea
l1” the Government realigned responsibilities and funding for
people with disabilities. Between 1993 and 1995 most Department of Social Welfare
disability-related programmes and services progressively transferred and were
consolidated with existing Ministry of Health services under the regional health authorities
(RHAs) and Vote: Health. The basis of access to services was shifted from nationally
specified 'entitlements' to individually assessed needs, within available or capped funding.
In 1994, The New Zealand Framework for Service Delivery (the DSS Framework) was put
in place by the RHAs under the direction of the Ministry. Under the DSS Framework, in
order to access a range of Ministry funded support services, an individual had to first meet
the Ministry’s definition of disability, and then have their needs assessed and undergo
service coordination or planned allocation of services, within available resources.
Assessment and allocation of services had to have an auditable separation from the
provision of services, which in most instances was by contracted providers.
The definition of an eligible person was outlined in the Government’s definition of a ‘person
with a disability’ for the purpose of accessing disability support services [CAB (94) M 3/5
(1a)]
(see
Appendix one). People identified as having a physical, psychiatric, intellectual, sensory or age-related
disability (or a combination of these) fell under the 1994 definition.
Since the 1994 definition the responsibility and funding for psychiatri
c2 and age relate
d3
disability has devolved to the DHBs. There has been further clarification of responsibility
1
The New Deal: Support for Independence for People with Disabilities, Ministers of Social Welfare and Health, 1992.
2 Devolved 2001
3 Devolved 2003
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
2 of 13
link to page 3 link to page 3 link to page 3 link to page 3 link to page 3 link to page 3 link to page 12 link to page 3
Document 1
and funding for people with Long Term Support needs resulting from Chronic Health
Condition
s4 (LTS-CHC) and people diagnosed with Autism Spectrum Disorde
r5. Responsibility and funding for people with physical, intellectual and sensory disability
remained with the Ministry.
Service eligibility
Eligibility means the right to be considered for publicly funded health and disability
services. It is not an entitlement to receive any particular service. If a person wishes to
access disability support services they are required to meet access criteria. If a person is
not eligible for publicly funded service
s6, they are liable for the full cost of the services they
receive and will access these independently.
Service Access
Most disability support services are accessed through Needs Assessment and Service
Coordination (NASC) organisations. A list of these can be found at:
http://www.health.govt.nz/your-health/services-and-support/disability-services/getting-
support-disability/needs-assessment-and-service-coordination-services
1.
Process for determining eligibility
To be considered for most Ministry funded disability support service
s7, a person may
self-refer or is referred to a Ministry-contracted NASC.
a. The NASC screens the refe
rral8 to confirm that the person referred:
• can be considered for the full range of publicly funded health and disability
services under the current Eligibility Directio
n9, and
• is likely to meet the Government’s definition of a ‘person with a disability’ for
the purposes of accessing DSS (CAB (94) M 3/5 (1a) (see
Appendix one), and
• is likely to have a physical, sensory or intellectual disability, or a combination
of these after provision of equipment, treatment and rehabilitation, and
• does not have an injury that is likely to meet ACC’s cover and entitlement
criteria under the Accident Compensation Act 200
110.
b. The NASC may request a specialist assessment or clinical reports to help
confirm eligibility for Ministry DSS.
c. If a person meets the above criteria, this triggers a needs assessment to confirm
that they meet the criteria to receive Ministry funded DSS.
4 Devolved to DHBs in July 2011
5 Clarification that disability related support needs resulting from ASD may be supported through DSS from 2014.
6 Refer http://www.health.govt.nz/new-zealand-health-system/eligibility-publicly-funded-health-services/eligibility-
direction
7 Refer section Other Information - DSS that do not require a NASC assessment.
8 This is the general practice however some NASCs move directly to determining eligibility at the time of the needs
assessment.
9 Refer http://www.health.govt.nz/new-zealand-health-system/eligibility-publicly-funded-health-services.
10 Some people are eligible for supports from both Ministry DSS and ACC, such as those with pre-existing disabilities
who have an accident that results in additional support needs. The Ministry funds supports received for any pre-existing
disability. Where it is too difficult to determine which support needs are due to a pre-existing disability and which to an
accident, a pragmatic joint funding/shared services arrangement will be negotiated.
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
3 of 13
link to page 8 link to page 4 link to page 12 link to page 4
Document 1
2.
Ministry DSS client group inclusions
The Ministry’s DSS client group consists of people who:
a. are eligible for publicly funded health and disability services, and
b. present for assessment for DSS before the age of 65, and
c. have a physical, intellectual, or sensory disability or a combination of these,
which is likely to:
• remain even after provision of equipment, treatment and rehabilitation
• continue for at least six months, and
• result in a need for ongoing support
d. do not meet the exclusion criteria (refer section
Ministry DSS funding exclusions).
In addition, the Ministry funds Environmental Support Services for a broader group of
people. This includes those outlined above, people with disabilities associated with
ageing, people first referred over the age of 65 and people aged under 65 with
disabling chronic health conditions.
A person’s diagnosis is a factor in determining eligibility for Ministry funded DSS but
is not the main determinant. It provides a guide as to whether a person is:
a. likely to have, or likely to develop (in the case of young children), a physical,
intellectual and/or sensory disability and also whether the person is likely to have
ongoing support needs mainly due to this disability
b. likely to have primarily personal health needs that could be significantly
ameliorated by treatment and/or that are likely to require ongoing clinical
intervention.
3.
Applying the definitions of physical, sensory and intellectual disability
The Ministry’s definition of its client group is informed by the disability type definitions
in “Support for Independence for People with Disabilities: A New Deal
” 11 (refer
Appendix one for a list of these definitions).
The sub-groups within the broader Ministry DSS client group accessing individualised
services are listed below. Impairments under each sub-group are accompanied by
examples of conditions that may result in these types of impairments but this is not
intended to be a diagnostic ‘in’ and ‘out’ list.
a. Physical disability
The Ministry’s DSS client group with physical disabilities accessing support
services includes people with impaired limb function affecting independence in
activities of daily living and/or mobilit
y12.
11 Minister of Social Welfare and Minister of Health.
Support for Independence for People with Disabilities: A New
Deal. 1992. Wellington: Parliament Buildings.
12 This group includes people with chronic medical conditions who, following active treatment and rehabilitation, are
assessed as having a long-term physical disability and an ongoing support need where physical disability (as opposed to
physical incapacity) is the primary reason for support.
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
4 of 13
link to page 5 link to page 5 link to page 5
Document 1
Physical disability may be due to (but is not limited to):
• partial/total absence or loss of limbs (e.g. at birth or following amputation as a
result of diabetes)
• structural impairments of limbs (e.g. achondroplasia)
• paralysis (e.g. hemiplegia following a stroke or brain tumour; paraplegia due to
spina bifida; tetraplegia due to debulking of a spinal tumour)
• reduced muscle strength (e.g. following guillain-barré)
• ataxi
a13 (e.g. with cerebral palsy or multiple sclerosis)
• muscle wasting (e.g. with muscular dystrophy or motor neurone disease)
• muscle tone abnormalities (e.g. due to acquired brain injury not covered by
ACC)
• limited range of movement (e.g. juvenile rheumatoid arthritis, osteoarthritis).
Some impairments arising from significant skeletal malformations (e.g. severe
scoliosis) may also meet the physical disability eligibility criteria, depending on the
nature of the resulting impairment.
b. Sensory disability
The Ministry’s DSS client group with sensory disabilities accessing support
services includes people with the following types of long-term sensory
impairments that are generally not responsive to treatment and affect
independence in activities of daily living and/or mobilit
y14: • blind
• deaf
• deaf-blind
• significant visual impairment
• significant hearing impairment
• significant other sensory loss (e.g. no taste or touch – rare
)15.
c. Intellectual disability
The Ministry’s DSS client group with intel ectual disabilities accessing support
services includes people with intellectual disability present at birth or generally
acquired in the development years (before age 18) (e.g. due to Angelman’s
syndrome, microcephaly or meningitis).
A NASC may request a specialist assessment to confirm a person has an
intellectual disability. This may include a cognitive assessment (generally, an IQ
test score of up to 70 indicates a limitation in intellectual functioning) and
standardised assessment of adaptive functioning in the areas of conceptual
skills, social skills and practical skills.
13 Ataxia is a lack of muscle coordination during voluntary movement, such as walking or picking up objects, generally
due to disorders in the brain or spinal cord.
14 This group includes people with chronic medical conditions who, following active treatment are assessed as having a
long-term sensory disability and an ongoing support need where sensory disability is the primary reason for support
(e.g. blind due to diabetes).
15 Note, sensory impairment does not include hypersensitivity or perceptual impairments such as auditory processing
disorder.
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
5 of 13
link to page 12 link to page 12 link to page 6
Document 1
Eligibility for Ministry funded Intellectual Disability Compulsory Care and
Rehabilitation services is legislatively mandated (Section 7 of the Intellectual
Disability (Compulsory Care & Rehabilitation) Act refers).
Eligibility for Ministry funded DSS contracted for people with intellectual disability
is outlined in the
‘Operational Guideline for the Assessment of Intellectual
Disability to Access Disability Support Services Contracted for People with
Intellectual Disability in New Zealand 2012’.
Where a person has been assessed as eligible for DSS on the basis of a
physical or sensory disability and the person has a co-existing significant
intellectual impairment that was acquired at age 18 or older and is not covered by
another funder (e.g. ACC), the Ministry may fund the full package of support.
4.
Other eligible groups
There are certain other groups that the Ministry funds support services for whose
impairments do not strictly meet the DSS definition of physical, sensory or intellectual
disability. Their inclusion generally reflects long-standing practice.
a. Disability in young children where presence of a physical, sensory and/or
intellectual disability is not yet confirmed
The Ministry funds disability support services for children who are medically
stable and have significantly delayed physical, intellectual and/or sensory
development (often global developmental delay) for whom there are indicators of
likely long-term physical, intellectual and/or sensory disabilities and where
clinical/rehabilitative intervention is not expected to significantly reduce the need
for long-term support. Eligibility is on an interim basis until a long-term disability
(usually an intellectual disability) with associated ongoing support needs is
confirmed (generally by age seven).
If the presence of a long-term disability and ongoing support need is not
confirmed, the NASC Service Coordinator facilitates the gradual withdrawal of
Ministry funded supports. DHB specialist clinical and allied health services may
continue to be available to these children.
b. Disability associated with acquired brain injury and certain neurological
conditions
The Ministry has funded disability support services for some people who have
acquired brain injuries and certain neurological conditions that do not result in a
physical or sensory disability or an intellectual disability that meets the intellectual
disability criteria in the “Operational Guideline for the Assessment of Intellectual
Disability to Access Disability Support Services Contracted for People with
Intellectual Disability in New Zealand 2009
”16.
This included some people who, after treatment and rehabilitation, have long-
term significant cognitive impairment (e.g. due to multiple sclerosis, a stroke, or a
benign brain tumour). Clinical reports were generally required to support the
16 When LTS-CHC devolved to DHBs in 2011 clarification was made that people with cognitive impairment without a
physical, sensory or intellectual disability would remain part of LTS-CHC client group. Funding was devolved
accordingly.
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
6 of 13
link to page 7 link to page 12 link to page 7 link to page 7 link to page 8 link to page 12
Document 1
referral to NASC. Eligibility decisions took into consideration the age of the
person, whether the person has any significant co-existing medical conditions
and the nature of the person’s support need.
The Ministry does not fund DSS for people who require support:
• due to cognitive impairment arising from a mental illness or addiction or due to
the consequences of treatment for these conditions (e.g. people with
Korsakoff’s psychosis or other substance induced brain damage)
• solely due to behavioural problems.
c. Autism Spectrum Disorder
Effective April 2014 DSS and Mental Health jointly agreed a national position with
respect to people diagnosed with ASD. This enabled people with ASD to be
considered for disability support services regardless of whether they also have a
co-existing physical, intellectual or sensory disability.
The clarification was made to: address inconsistent access and practice across
the country, recognise there are still service gaps requiring service development,
and commit to a joined up solution where organisations and funders work
together in finding pragmatic and sustainable solutions for this group of people.
5.
Needs assessment and service coordination process
Any person assessed by a NASC as likely to meet the Ministry DSS eligibility criteria
is entitled to have a needs assessment to identify disability support needs and
assessed goals. This does not confer an automatic entitlement to services as the
provision of services is prioritised on the basis of the person’s level of assessed need
related to their disability. Some people with lower level needs may not receive DSS.
The needs assessment includes assessing, wherever possible, what is primarily
driving the person’s support need. Support needs that are not primarily attributable
to an ongoing physical, intellectual and/or sensory disability or an impairment
included in 1.4 (denotes DSS eligibility) are not DSS’ funding responsibilit
y17. Where
a DSS eligible disability is contributing to broader support needs, DSS will negotiate
joint funding or joint service package arrangements with the relevant other funder.
When a person presents for assessment for DSS between the age of 50 and 65, the
Ministry NASC also screens the referral to determine whether the person is likely to
meet the
‘close in interest’ criteri
a18. If screening indicates that the person is likely to
meet these criteria, the NASC forwards the referral on to a DHB needs assessment
service.
If the needs assessment confirms that the person has disability support needs, a
service coordination process follows to determine:
• what natural supports the person has to meet these need
s19
• which needs can be fulfilled within the range of services the Ministry funds within
its capped budge
t20, and/or
17 In practice, some funding for supports needed due to co-existing conditions does occur.
18 Refe
r Close in Interest Operational Policy
19 In the case of young children, this includes taking account of the level of support a parent would normally be
expected to provide for a child of that age.
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
7 of 13
link to page 8 link to page 8 link to page 8 link to page 8
Document 1
• where other avenues of support are indicated (with a view to referral on to
appropriate services).
For people assessed as eligible for Ministry DSS, the services available to meet their
support needs are services that already exist within DSS’ service framewo
rk21.
6.
Ministry DSS Funding Exclusions
The Ministry’s DSS does not fund support services for people with conditions or
situations covered by other funders including:
• support to address short-term needs i.e. less than six months duration e.g.
following surgery or medical event
s22 (DHBs’ Personal Health)
• support for people who first present for assessment for long-term supports at age
65 or over (DHBs’ Health of Older People - CAB Min (03) 5/5 refers)
• support for people who first present for assessment for long term supports
between ages 50 and 65 who are clinically assessed by a DHB clinician or needs
assessor as being ‘close in interest’ to older peopl
e23 (DHBs’ Health of Older
People - CAB Min (03) 5/5 refers). Refer to the DSS Close in Interest Operational
Policy.
• aged residential care for Ministry DSS clients who have been reassessed by a
DHB needs assessor as requiring this service (DHBs’ Health of Older People -
CAB Min (03) 5/5 refers)
• support for people who first present for assessment for long-term supports before
the age of 65 whose support need is due to impairments that do not meet DSS’
operational definition of physical, sensory or intellectual disability. This includes
people who will be referred to DHBs’ Long Term Supports – Chronic Health
Conditions services.
• support for ‘medically fragile children’ - children with high health needs and/or
multiple impairments whose health status has not yet stabilised and for whom a
physical, sensory and/or intellectual disability with associated ongoing support
needs has not been identified (DHBs’ Personal Health / Long-term Supports –
Chronic Health Conditions [LTS-CHC], Primary Care)
• support for needs arising primarily from physical incapacity (e.g. shortness of
breath, fatigue or pain) due to a chronic health condition (DHBs’ LTS-CHC /
Personal Health, Primary Care)
• support for additional care needs arising from a condition in the palliative stag
e24
(DHBs’ Palliative Care)
20 Some eligible people will have a low level of support need and access services such as information and advice or
fieldworker services from a non-government organisation rather than individualised services.
21 This is the current arrangement however the Demonstration Projects to implement the New Model for Disability
Support and Enabling Good Lives includes expanding the range of services that people under Individualised type
funding arrangements can purchase with their allocated support funding, through contracted and non-contracted
providers.
22 This includes ‘topping up’ existing Ministry DSS support packages for Ministry DSS clients in these situations.
23 People with long-term conditions more commonly experienced by older people and requiring integrated health and
disability support services.
24 This includes specialist palliative care services for people receiving Ministry DSS.
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
8 of 13
link to page 9 link to page 9 link to page 9 link to page 9 link to page 9
Document 1
• support for needs arising from a mental illness and/or addictio
n25 including
physical, sensory and cognitive impairments attributable to this underlying
condition e.g. tardive dyskinesia due to long-term use of psychotropic medication,
cognitive impairment due to alcohol or other substance abuse, impaired mobility
due to alcohol related peripheral neuropathy or functional difficulties due to
conversion disorder (DHBs’ Mental Health and Addiction / LTS-CHC, Primary
Care
)26
• support services needed primarily as a result of dementia or substance abuse
(DHBs’ Health of Older People / Mental Health of Older People / LTS-CHC,
Primary Care)
• support services needed primarily as a result of behavioural problems (e.g.
associated with Foetal Alcohol Syndrome or substance abuse) except where the
person has a co-existing disability that meets DSS eligibility criteri
a27 (some
services are funded by other government agencies, in other situations this is a
funding gap)
• support due to an injury that meets ACC’s cover and entitlement criteria under the
Accident Compensation Act 200
128
• support for situations covered by other central government agencies such as the
Ministry of Education and the Ministry of Social Development (including the Child,
Youth and Family Service
)29
• support needs solely due to social/environmental factors (e.g. housing or where
parents need support for their own health needs). [Some services are funded by
other government agencies, in other situations this is a funding gap].
Cross Funder Relationships
1.
Shared arrangements for people with DSS eligible disabilities and other
conditions
Joint funding or shared service arrangements may apply where a person assessed
as needing formal support:
a. meets Ministry DSS eligibility and access criteria, and
b. has a personal health condition, chronic health condition, condition in the
palliative stage, mental illness and/or addiction, and/or injury.
Where a person has support needs arising from both a DSS eligible disability
type and a co-existing condition or situation for which another funder (e.g. DHB,
ACC or Ministry of Education) has support funding responsibility, the Ministry will
negotiate joint funding or shared service arrangements with the relevant other
25 Responsibility for planning and funding disability support services for people with psychiatric disabilities was
devolved to DHBs in 2001 (CAB Min (01) 12/12 refers). All residual contracts and funding were devolved in 2003
(CAB Min (03) 23/8 refers).
26 People who have a mental illness and/or addiction and a co-existing physical, sensory or intellectual disability that
meets Ministry DSS eligibility criteria may receive both DHB and Ministry DSS funded supports.
27 Where a person has behavioural issues due to an acquired brain injury or certain degenerative neurological conditions
(e.g., Huntington’s disease) secondary to a co-existing physical, sensory or intellectual disability, Ministry DSS may
fund the full support package.
28 Refer footnote 9.
29 Some people will receive supports from both Ministry DSS and another agency(ies).
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
9 of 13
link to page 10 link to page 10
Document 1
funder. The Ministry contributes to the person’s support package by funding the
DSS required as a result of the DSS eligible disability.
In complex situations where the cause of impairment is unclear (e.g. injury vs
acquired) or a person has multiple impairments/causes of impairments, the
Ministry works with other funders to determine a pragmatic joint funding / shared
services arrangement to support prompt access to essential supports (e.g. 50/50
split or inter-funder transfer via the Crown Funding Agreement). Further work is
needed across funders to agree consistent and efficient pathways for resolving
funding responsibility in these situations.
2.
Resolving funding responsibility between the Ministry and DHBs
Where there is disagreement between funders over whether a person’s support
needs are the funding responsibility of the Ministry or a DHB, it is important that the
interests of the person needing support are protected in the first instance.
The following resolution procedures apply:
• any disagreement about access to Ministry or DHB funded services will be
resolved in the first instance by discussion between the relevant needs
assessment services, this may include the support of the NASC National Reviewer
if required.
• where resolution cannot be achieved through discussion between Ministry and
DHB needs assessment services, the first level of escalation will be to the
operational management within the Ministry’s Disability Support Services Group
and to the DHB Portfolio Manager
• where resolution cannot be achieved through the involvement of the DHB and
Disability Support Services Group, the dispute resolution processes in the
Operational Policy Framework will appl
y30.
3.
Transferring funding responsibility for existing clients
In respect of moving disability clients between Ministry DSS and DHB Health of Older
People funding (CAB (03) M 23/8 refers), Ministry clients can move to become DHB
clients, but DHB clients cannot move to become Ministry client
s31. A Ministry client
will become a DHB client only if they are reassessed as requiring aged residential
care.
4.
Transfers between Ministry DSS and DHB Long-term Support Chronic Health
Conditions funding
DHB Long-term Support Chronic Health Conditions (LTS-CHC) clients can move to
become Ministry DSS clients (or to shared funding arrangements) if they acquire a
disability that meets the Ministry’s DSS eligibility and access criteria and this disability
is now the main reason why the person needs ongoing support.
30 Refer section 8, Operational Policy Framework 2011/12 - http://www.nsfl.health.govt.nz/apps/nsfl.nsf/pagesmh/387
31 Note that even if the client had previously been a Ministry client, having moved to become a DHB client they cannot
return to the Ministry for funding. All movements are one way - from the Ministry to a DHB - unless both funders
agree that the funding associated with that person has been incorrectly devolved or incorrectly assessed. In cases of
disagreement between funders, the dispute resolution processes in the CFA will apply.
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
10 of 13
Document 1
Further information
1.
Disability Support Services that do not require a NASC assessment
While most disability support services are accessed through a NASC process, some
services can be accessed on self-referral, GP referral or referral by a qualified
person.
Services that can be accessed on self and/or GP referral include: Disability
Information and Advisory Services; and some services supporting people with
hearing or visual impairments. Services generally accessed through referral by a
qualified person (often a health professional) include Child Development Services,
Assessment Treatment and Rehabilitation (AT&R) Services and most Environmental
Support Services.
2.
Disability Information and Advisory Services (DIAS)
DIAS provide information for people with disabilities and other members of the
community on how to find support and advocacy groups, NASC services or
community support organisations, specific information related to particular disabilities
and other topics related to disability.
3.
Child development services
Child Development Services are multidisciplinary community-based services that
provide specialist assessment, intervention and management services for young
children (mostly pre-schoolers) who have disabilities or who are not achieving
developmental milestones. The Ministry funds the allied health component of these
services. Child development Services work with other agencies providing services to
children to support children to achieve their potential.
4.
Assessment, Treatment and Rehabilitation Services (AT&R)
Ministry-funded AT&R services are DHB provided multidisciplinary services delivered
in a range of settings for people with disabilities under the age of 65. They include
specialised and clinical assessment, treatment and rehabilitation to enable people to
participate in daily activities and fulfil valued roles in their home and community.
5.
Environmental Support Services (ESS)
Environmental Support Services are a range of services and supports funded by the
Ministry that are available to a broader group than DSS accessed via NASC. They
include:
• Equipment and Modifications Services (EMS) - such as equipment, housing
modifications and vehicle purchase and modifications)
• Supports and services for people with hearing loss (such as hearing aids,
hearing aid subsidies, cochlear implants and services; interpreter services and
hearing therapy)
• Supports for people with vision loss (such as spectacle and contact lens
subsidies, and services for blind and deafblind people)
• Other subsidies and benefits (including wigs and breast prostheses)
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
11 of 13
link to page 12
Document 1
• Some specialised assessment services (such as wheelchairs, seating and
postural management and communication assistive technology) and assessor
training.
ESS are funded through DSS for: people with physical, sensory and intellectual
disabilities; people with disabilities associated with aging; and people aged under 65
with disabling chronic health conditions.
People access EMS and hearing aid and spectacle subsidies via a specialised
assessment with a DHB assessor or a private assessor (the person may pay for
services such as audiology) who is a suitably skilled or qualified person (e.g. an allied
health professional or an audiologist who is an approved or credentialed EMS
Assessor as described in the DSS Accreditation Framework).
Access to services is prioritised so that people with the most urgent needs receive
services first. A new prioritisation tool for EMS has been developed which prioritises
access to resources on the basis of a person’s ability to benefit from the service and
other relevant factors.
6.
Health and disability services funded in New Zealand
The
Health and Disability Services Eligibility Direction 2011 (the direction) sets out
the groups of people eligible for publicly funded health and disability services in New
Zealand. This direction was made by the Minister of Health under section 32 of the
New Zealand Public Health and Disability Services Act 2000. The direction became
effective on 16 April 2011, and applies from that date forward. Part B1 states that a
person is eligible under the Act if the person is in New Zealand when the services are
received.
A person must meet one of the criteria in the Eligibility Direction to be considered for
these publicly funded services. If the person is not eligible, they are liable to be
charged for the full costs of any medical treatment or disability support service
received.
LINKS TO IMPORTANT DOCUMENTS
➢ Guide to Eligibility for Publicly Funded Services
➢ Health and Disability Services Eligibility Direction 2011
➢ Close in Interest
➢ NASC Operational Policy
➢ Operational Guideline for the Assessment of Intellectual Disability
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
12 of 13
link to page 13
Document 1
Appendix 1: Definitions
1. Government’s definition of ‘person with a disability’ for the purpose of
accessing disability support services [CAB (94) M 3/5 (1a)]
“A person with a disability is a person who has been identified as having a physical,
psychiatric, intellectual, sensory or age-related disability (or a combination of these),
which is likely to continue for a minimum of six months and result in the reduction of
independent function to the extent that ongoing support is required.
Where a person has a disability which is the result of a personal injury by accident
which occurred on or after 1 April 1974, it should be determined whether they are
eligible for cover under the Accident Rehabilitation and Compensation Act.
Where a person’s level of independent function is reduced by a condition which
requires ongoing supervision from a health professional (e.g. in the case of renal
dialysis), that person is considered to have a personal health need rather than a
disability. Where a person has both a disability and a personal health need, the
services provided to address those needs are disability support services and
personal health services respectively”.
Subsequent to this definition being agreed by Cabinet, Cabinet decided to transfer
responsibility for some disability groups to DHBs. Funding responsibility for DSS for
people with psychiatric disability transferred to DHBs in 2001 and for people with
age-related disability in 200
332. The latter group included:
• people who first present for assessment for DSS at age 65 and over, and
• people aged between 50 and 65 who are clinically assessed as ‘close in
interest’ to older people (having poorer health and disability status than the
general population and conditions/disabilities normally acquired at age 65 or
over).
2. Definitions in “Support for Independence for People with Disabilities: A New
Deal”
[Minister of Social Welfare and Minister of Health. 1992.
Support for Independence
for People with Disabilities: A New Deal. Wellington: Parliament Buildings]
• “Physical disability - reduced physical capacity (for example, through loss or
impaired use of limbs)
• Sensory disability - impairment of the senses (mostly sight and hearing)
• Intellectual disability - permanently impaired learning ability (usually from birth)
which prevents or inhibits people from developing the range of physical and
social skills usually found in a person of that age
• Psychiatric disability - Disability arising from continuous or intermittent disorders
related to thinking, feeling, volition, or behaviour (for example, schizophrenia,
severe chronic depression, or long-term addiction to alcohol and drugs
• Age-related disability - Physical, intellectual or psychiatric conditions related to
the onset of old age. This includes conditions that can affect younger people,
such as Alzheimer’s disease or stroke, but which are more often found amongst
older people”.
32 Note, this devolution also included residual Ministry funded long-term support services for people with personal
health conditions, mental illnesses and palliative care needs.
Title: DSS Eligibility
Version: 2
Authorised By: Toni Atkinson, DSS Group Manager
Effective date:
Expiry date:
Filepath:
Page
20/3/17
19/3/20
DSS Admin\Policy\Operational Policies
13 of 13

Document 4
Briefing
Date:
20 December 2023
For:
Hon Penny Simmonds, Minister for Disability Issues
File reference:
REP/WHK/23/12/015
Security level:
In confidence
Background on the approach to scoping
the Review of Eligibility for Disability
Support Services
Purpose
This briefing responds to your request for further information on our work to review
eligibility for Disability Support Services (DSS) funded by Whaikaha, including
information about the engagement we are undertaking and next steps.
Recommendations
It is recommended that you:
a)
Note the contents of this briefing.
Noted
Hon Penny Simmonds
Minister for Disability Issues
Date:
Helen Walter
Group Manager Policy,
Policy, Strategy and Partnerships
20/12/23
Actions for private secretaries: N/A
IN-CONFIDENCE
Document 4
Background on the Review of Eligibility for
Disability Support Services
Context
1. In February 2023, the previous Minister for Disability Issues agreed to Whaikaha
scoping a medium-term policy work programme to review eligibility to access
DSS (REP/22/9/848 refers). You have asked for more information about this
work.
2. We are considering a range of issues, including the constraints in the current
fiscal environment, to inform the scope.
3. Eligibility for DSS is an issue that many disabled people, tāngata whaikaha Māori
(disabled Māori), family and whānau are interested in.
4. Whaikaha-funded (previously Ministry of Health-funded) DSS eligibility is not
defined in legislation but was mandated by Cabinet in 1994. A person must have
Autism or an intellectual, sensory, or physical disability which is expected to
continue for at least six months, where their impairments limit their ability to
function independently - requiring ongoing support.
5. Further detail on the status quo is provided at Appendix 1, including the verbatim
1994 Cabinet minute [CAB (94) M 3/5(1a)].
Whaikaha is developing advice on the scope of the review
6. This review presents an opportunity to examine gaps in support and services
available to disabled people, their families and whānau - including the systemic
cost of unmet disability needs, and how government can respond to this.
Why we are reviewing eligibility now
7. The October 2021 Cabinet paper that established Whaikaha noted that ‘the
disability community has called for eligibility to be based on the functional impact
of disability rather than on impairment. Once structures are in place, the Ministry
will be well placed to consider these eligibility issues, including for example
support needs for those with fetal alcohol spectrum disorder (FASD), whose
support and service requirements fall across multiple agencies’ (CAB-21-MIN-
0395 refers).
8. In 2022, New Zealand was examined by the United Nations Committee on the
Rights of Persons with Disabilities (the UN Committee). The Committee’s
Concluding Observations - Observation 54 (c) - included to “Ensure people with
fetal alcohol syndrome disorder, chronic fatigue syndrome and other chronic and
rare conditions have access to the disability support system and are included in
disability policies and programmes.”
REP/WHK/23/12/015 Background on the approach to scoping the Review of Eligibility
2
IN-CONFIDENCE
Document 4
9. The previous Government accepted this observation with modification, meaning
that work will be done to consider the observation, while noting that Cabinet or
Budget decisions would be required to fully implement it (SWC-23-MIN 0083
refers).
10. Whaikaha and previous Ministers have received correspondence from individuals
and groups who have conditions which meet the UN’s definition of disability and
have unmet needs yet are ineligible to access DSS funded by Whaikaha.
11. In August 2023, the Health Committee released its report on the petition of the
Associated New Zealand ME Society (ANZMES) seeking reclassification of ME/CFS
as a disability and for people living with ME/CFS to be eligible to access DSS
funded by Whaikaha. In its report, the Committee encouraged Whaikaha to
consider amending its eligibility criteria to enable people with ME/CFS to access
Whaikaha-funded DSS.
Approach to the review
12. We are considering a broad range of issues before advising you on scope for the
review. Whaikaha is currently analysing options for scope and objectives for the
review, and engaging with disability community groups, tāngata whaikaha Māori,
and family/whānau representatives on the relative merits and costs of these
options.
13. s9(2)(g)(i), s9(2)(ba)(i)
14.
REP/WHK/23/12/015 Background on the approach to scoping the Review of Eligibility
3
IN-CONFIDENCE
Document 4
s9(2)(g)(i), s9(2)(ba)(i)
REP/WHK/23/12/015 Background on the approach to scoping the Review of Eligibility
4
IN-CONFIDENCE
Document 4
s9(2)(g)(i), s9(2)(ba)(i)
Ends
Author: Mary Fisher, Policy Analyst, Policy, Strategy and Partnerships
Responsible manager: Amber Coyle, Manager, Policy, Strategy and Partnerships
REP/WHK/23/12/015 Background on the approach to scoping the Review of Eligibility
5
IN-CONFIDENCE
Document 4
Appendix 1: Whaikaha-funded Disability Support Services
eligibility criteria
Whaikaha-funded (previously Ministry of Health-funded) Disability Support Services
(DSS) eligibility is not defined in legislation but was mandated by Cabinet in 1994
[CAB (94) M 3/5(1a) refers]. The mandated definition of ‘a person with disability for
the purpose of accessing disability support services’ is as follows:
“A person with a disability is a person who has been identified as having a
physical, psychiatric, intellectual, sensory or age-related disability (or a
combination of these), which is likely to continue for a minimum of six
months and result in the reduction of independent function to the extent
that ongoing support is required.
Where a person has a disability, which is the result of a personal injury by
accident which occurred on or after 1 April 1974, it should be determined
whether they are eligible for cover under the Accident Rehabilitation and
Compensation Act.
Where a person’s level of independent function is reduced by a condition
which requires ongoing supervision from a health professional (eg in the
case of renal dialysis), that person is considered to have a personal health
need rather than a disability. Where a person has both a disability and a
personal health need, the services provided to address those needs are
disability support services and personal health services respectively."
Decisions were subsequently made to transfer responsibility for some disability
groups to district health boards (now Te Whatu Ora – Health New Zealand), with
people with psychiatric disability transferring in 2001, people with age-related
disability in 2003, and people with long-term support needs resulting from chronic
health conditions in 2011.
Eligibility for DSS for people with autism spectrum disorder (Autism) was clarified in
2014 through a Ministerial by the Minister of Health rather than Cabinet decision
(prior to 2014, there had been inconsistent practice regarding eligibility for people
with autism).
The process and criteria for service access to DSS is further defined through the
Ministry of Health’s (now Whaikaha – Ministry of Disabled People’s) DSS Operational
Policy: DSS Eligibility 2017-2020, which includes:
• the role of NASCs in determining eligibility and needs assessments
• access generally applies to people who present before the age of 65
• descriptions and examples of eligible intellectual, sensory, and physical
disabilities
• exclusion criteria including where support is funded by other agencies (e.g.
people with FASD).
REP/WHK/23/12/015 Background on the approach to scoping the Review of Eligibility
6
IN-CONFIDENCE
Document 4
Appendix 2: List of organisations currently represented on
the Advisory Group for the review
• Fetal Anti-convulsant Syndrome NZ,
• Attention Deficit Hyperactive Disorder New Zealand,
• Associated New Zealand ME society (Myalgic Encephalomyelitis/Chronic Fatigue
Syndrome),
• Complex Chronic Illness Support,
• Fetal Alcohol Spectrum Disorder Care Action Network
• Rare disorders New Zealand,
• Ehlers Danlos Syndromes New Zealand,
• Tourette's Association of New Zealand,
• Autism NZ,
• NZ Carer's Alliance,
• Stroke Foundation of New Zealand,
• Epilepsy New Zealand,
• Youth representative.
REP/WHK/23/12/015 Background on the approach to scoping the Review of Eligibility
7

Document 5
Brian Co ey, Director of the O ce for Disability Issues
o [email address]
28th August 2023
Dear Brian
We write to you to commend the O ce for Disability Issues for supporting the
implementation of the United Nations Convention on the Rights of Persons with
Disabilities (UNCRPD) and the New Zealand Disability Strategy.
We would like to take this opportunity to highlight a situation that requires your attention
to ensure that the UNCRPD recommendations are adhered to.
In September 2022, the UNCRPD released a report, in which they stipulated that people
with ME/CFS should have access to the disability support system and be included in
disability policies and programmes (53c).1 Our government has not implemented these
actions to date.
those who have long-term physical, mental, intellectual, or sensory impairments which in
interaction with various barriers may hinder their full and e ective participation in
society on an equal basis with others.2
The New Zealand Disability Strategy also uses the UNCRPD definition of disability.3
1 Convention on the Rights
of Persons with Disabilities, CRPD/C/NZL/CO/2-3 (9 September 2022). Advanced Unedited Version. Committee on the
Rights of Persons with Disabilities
2 Office of Disability Issues (no date). Things you should know: Definitions, concepts and approaches
https://www.odi.govt.nz/disability-toolkit/things-you-should-know-definitions-concepts-and-approaches/
3 As above.
1
Document 5
Other disability definitions are as follows:
A disability is an impairment — physical, intellectual or sensory — that lasts for more than
6 months and limits your ability to carry out day-to-day activities. This can include
psychiatric illness.4
Any self-perceived limitation in activity resulting from a long-term condition or health
problem; lasting longer or expected to last longer than six months or more and not
completely eliminated by an assistive device.5
Physical disability or impairment: physical illness: psychiatric illness: intellectual or
psychological disability or impairment: any other loss or abnormality of psychological,
physiological: or anatomical structure or function: reliance on a guide dog, wheelchair, or
other remedial means: the presence in the body of organisms capable of causing illness.6
Disability refers to the interaction between individuals with a health condition (e.g.,
cerebral palsy, Down syndrome and depression) and personal and environmental factors
(e.g., negative attitudes, inaccessible transportation and public buildings, and limited
social supports).7
Any restriction or lack (resulting from an impairment) of ability to perform an activity in the
manner of or within the range considered normal for a human being.
Persons with disabilities include those who have long-term physical, mental, intellectual
or sensory impairments which in interaction with various barriers may hinder their full
and e ective participation in society on an equal basis with others.8
4 Ministry of Health NZ. Disability. (2021).
https://www.health.govt.nz/our-work/populations/maori-health/tatau-kahukura-maori-health-statistics/nga-mana-hauora-tuto
hu-health-status-indicators/disability.
5 Statistics New Zealand. Disability Survey: 2013. (2013).
https://www.stats.govt.nz/information-releases/disability-survey-2013
6 Human Rights Act 1993 No 82 (as at 10 May 2022), Public Act 21 Prohibited grounds of discrimination – New Zealand
Legislation. https://legislation.govt.nz/act/public/1993/0082/latest/DLM304475.html.
7 World Health Organisation. (2021). Disability and health.
https://www.who.int/news-room/fact-sheets/detail/disability-and-health
8 United Nations. UN Enable : First 50 Years : Chapter II - What is a disability?. (2003-04).
https://www.un.org/esa/socdev/enable/dis50y10.htm.
2
Document 5
On the
, it states:
“Ministry funded disability support services are available to people who have a physical,
intellectual or sensory disability (or a combination of these) which: is likely to continue for
at least six months, needs ongoing support to live independently, to the extent that
ongoing support is required. These services are mainly for people under the age of 65
years. The Ministry will also fund disability support services for people with: some
neurological conditions that result in permanent disabilities, some developmental
disabilities in children and young people, such as Autism, physical, intellectual or
sensory disability that co-exists with a health condition and/or injury.”9
Despite the symptoms of ME/CFS meeting many of these definitions, the illness is not
categorised as a disability in New Zealand for the purpose of health-related funding and
support. On the Whaikaha website, it mentions that the first step is a Need Assessment.
The Needs Assessment Coordination Service have confirmed that people with ME/CFS
are not eligible for assessment unless over 65 years of age, have a mental health
condition, or are of very high needs - requiring 24/7 care.
The
diagnostic criteria for ME/CFS classified that the
state of impairment, in the ability to engage in pre-illness levels of occupational,
educational, social, and personal activity, must have lasted at least 6 months and is not
alleviated by rest. This means to be diagnosed with ME/CFS the individual must have
been in this state of impairment for at least 6 months (other criteria also apply). This
long-term health condition is accompanied by symptoms including non-restorative sleep,
post-exertional malaise, cognitive impairment, immune dysfunction, pain, autonomic
dysfunction, and/or orthostatic intolerance. Other case definitions used are the
Canadian Criteria (CC) based on the International Consensus Criteria (ICC).
Since 1969, ME has been classified by the
as a neurological
disease (ICD-10/323). In 2019, it was also classified as a post viral fatigue syndrome
under diseases of the nervous system (ICD-10/G93.3).
People with these debilitating conditions face a barrier to support under the current
classification of “chronic illness” and as a result experience poor quality of life and health
inequity. With increasing numbers of people with long COVID (lC) being diagnosed with
ME/CFS the existing support through nonprofit organisations is set to become
unmanageable, with case numbers still rising. This means that the government needs to
work in collaboration and contract with the National Advisory on ME (who can coordinate
9 Whaikaha Ministry of Disabled People. How to access support (no date).
https://www.whaikaha.govt.nz/assessments-and-funding/how-to-access-support/
3
Document 5
with the regional nonprofit organisations) to successfully support the needs of all people
living with these disabling conditions.
In
- a Report for Manatū
Hauora Ministry of Health (January 2023) it states “Long COVID has resulted in a newly
disabled population of people who need ongoing support and the development of new,
and improved access to existing, multi-disciplinary, integrated and consumer led
services. Paula Tesoriero, Disability Rights Commissioner and new CEO of Whaikaha -
Ministry of Disabled People, has identified that for many people, long COVID meets
accepted criteria of disability, and thus should open doors for additional support
(Tesoriero, 2022). The lack of support for those with long COVID highlighted in this report
emphasises this need.” (p. 11).
We would like to point out that not only do many with long COVID meet the diagnostic
criteria for ME/CFS, but people with long COVID have a higher chance of recovering (20%
likely to recover, 10% like to remain chronically unwell). Therefore if people with long
COVID are considered to be living with a disability, those with ME/CFS (only 5% recover,
95% chronic or lifelong) must be considered as living with a disability too.
In 2012, following a petition submitted by our executive committee member Wendy
Matthews, the Health Select Committee recommended to the government that ME/CFS
should be reclassified as a disability. This was not implemented by the government. As
such, people living with ME/CFS have continued to be excluded from vital support
services and funding opportunities, despite a very real need.
On September 20, 2022 ANZMES presented a petition to parliament calling for the
reclassification of ME/CFS from a chronic illness to a disability, with 6,444 signatures.
On May 3 2023 we provided an oral submission to the Health Select Committee (which
followed our written submission presented in October 2022). You can watch the oral
submission here.
ANZMES created this petition to draw attention to the fact that the system is not working
for people with ME/CFS. Despite meeting the definition for disability, ME/CFS does not fit
the criteria to access disability support services.
People with ME/CFS are theoretically entitled to support under the chronic illness
classification, however they are not receiving it in practice. The body that approves
applications - The Needs Assessment and Service Coordination (NASC) organisation -
4
Document 5
confirms that ME/CFS patients are not considered for assessment. Currently eligibility
criteria for NASC is for over 65 years of age, those with mental health conditions, or those
requiring seven days per week care - meaning that those with disabling disease
requiring 3-4 days care are not eligible or considered for assessment. The majority of the
NASC providing services for under 65’s, for example Auckland Regions Taikura Trust, do
not provide services for people with health conditions or long term chronic illnesses and
refer this to the DHB. This means that access to services is subject to a postcode lottery,
as there are di ering processes, eligibility, and levels of support across the regions,
resulting in inconsistent services across Aotearoa. This creates healthcare access
inequity.
On August 17, 2023, the Health Select Committee presented their report to parliament, in
response to our petition. You can view the full report here. In their report the HSC
recommended that eligibility criteria for disability services be amended. The 10 page
report recommends that the Government take note stating “we understand that ME/CFS
meets the Government’s definition of a disability. We therefore, encourage Whaikaha to
consider amending its eligibility criteria to enable people with ME/CFS to access
Whaikaha-funded disability support services.” (pg. 9).10
The report also acknowledged concerns raised by ANZMES that the current classification
and system is flawed with complicated assessment processes and policies and disparity
between regions causing access inequality. The committee report acknowledged that the
eligibility criteria di er between Whaikaha and Te Whatu Ora-funded services, resulting
in inequitable access.
The HSC report ME/CFS is recognised as a disability under the UNCRPD. Whaikaha also
stated this in the oral and written submission.
We have released a press release in response to the HSC report, which you can read
here.
Although the HSC report states that a person does not require a classified disability to
access health services (based on the written submission by Martin Chadwick, Chief
Allied Health Professionals O cer), in practice we have found that many with ME/CFS are
denied help despite the obvious need. We understand that support needs to be
prioritised but at present, due to a misconception around the severity of the illness and
the lack of functionality that results, many are seen as low on the priority scale.
10 Report of the Health Committee Petition of Associated Myalgic Encephalomyelitis Society Incorporated: Reclassification
of ME/CFS to disability August 2023 https://selectcommittees.parliament.nz/v/6/ae4007f6-f35f-4590-7a2a-08db9ea64502
5
Document 5
Along with the petition ANZMES also provided a comprehensive written report with a
series of solutions, beginning with reclassification and includes dedicated funding, a
contract for wraparound services and the creation of a tailored support structure with a
tiered system that recognises the varying degrees of disability experienced by people
with ME/CFS. We also recommend that we align our health care approach with the latest
research and recommendations by implementing a multi-disciplinary pilot.
People with ME/CFS want to see the actual implementation of these recommendations.
Practical help is urgently needed for this growing under-supported, disabled community
that could lead to a better prognosis and better quality of life.
We urge you to implement the HSC Report recommendations, and we welcome a meeting
with you via zoom to discuss how we can work together to ensure that people living with
both ME and lC can gain access to vital disability support services, be recognised as
living with disability, and be included in policies and programmes. We o er you our
expertise to help make this a lived reality for all those a ected, and their family/whānau.
Ngā Mihi
Yours sincerely
Fiona Charlton
President
6

Document 5
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is often triggered by a
viral illness and involves overwhelming fatigue and other symptoms that range in severity
as it a ects many body systems, such as the immune, neuroendocrine and autonomic
nervous system.
The key characteristic of ME/CFS is post exertional malaise (PEM) which presents 12-48
hours after exertion, and can result in days to weeks of exacerbated symptoms. For the
very severe, this exertion can be simply trying to speak, or eat.
We are the National Advisory on ME in Aotearoa/New Zealand. With four decades of
knowledge and experience, we are the trusted leaders in ME education, representation,
and research. Our expertise comes from a reputable medical team of advisors, including
a world renowned expert and MNZM recipient, a fellow of the Royal NZ College of General
Practitioners (RNZCGP) and a network of academic researchers, clinicians, and
representatives from the ME community. The executive committee comprises experts in
their respective fields for governance, policy, leadership, representation, and education.
Always a trail-blazer, it was the first ME charity of its kind in the world, established in
1980, as ANZMES, to provide support, information dissemination, and representation,
achieving past outcomes through dedication, passion, time, and knowledge of lived
experience. Today, the organisation leads as a Royal New Zealand College of General
Practitioners (RNZCGP) Continuing Medical Education (CME) Registered Provider, proud
funder of vital research, and steward of the community voice.
We continue to disseminate evidence-based information nationally, and represent the
ME voice globally as a founding member of the World ME Alliance through advocacy and
leadership. ANZMES latest education programme - Know M.E. - is a video podcast and
news series featuring up-to-date, evidence based research and information on ME and
Post COVID Conditions.
7

IN-CONFIDENCE
Document 6
Level 4, 56 The Terrace
Wellington 6011
New Zealand
9 October 2023
Fiona Charlton
Associated New Zealand Myalgic Encephalomyelitis Society Inc.
Community House
301 Moray Place
Dunedin 9016
Tēnā koe Fiona
Thank you for your letter to Brian Coffey on behalf of Whaikaha – Ministry of Disabled
People (Whaikaha) in August this year. I acknowledge the advocacy you do on behalf
of those living with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS).
I am responding on behalf of Whaikaha.
Your letter draws attention to the many different ways that disability is described in
Aotearoa New Zealand and internationally, and the gaps in support for people with
ME/CFS linked to these different and sometimes conflicting definitions.
I acknowledge the challenges for people with ME/CFS that arise from government
supports being difficult to navigate, with multiple eligibility criteria for different
services making it difficult for people to know what support they are entitled to.
Government supports have criteria and descriptions that may be narrower than the
United Nations Convention on the Rights of Persons with Disabilities (UNCRPD) and
the New Zealand Disability Strategy. On this point, you referred to the 2022 review of
New Zealand’s compliance with our UNCRPD obligations by the United Nations
Committee on the Rights of Persons with Disabilities, and the Committee’s concluding
observation to
Ensure people with foetal alcohol syndrome disorder, chronic fatigue
syndrome and other chronic and rare conditions have access to the disability support
system and are included in disability policies and programmes (Observation 54 (c))
.
The Government confirmed its response to the Committee’s concluding observations
in August this year. The Government accepted observation 54 (c) with modification,
which means that there will be practical work to consider the intent of the change,
while noting that Cabinet or Budget decisions will be required to fully implement it.

IN-CONFIDENCE
Document 6
More information about the Government’s response to the Committee’s concluding
observations can be found here: Cabinet agrees on a response to recommendations
from UNCRPD examination - Office for Disability Issues (odi.govt.nz).
In accordance with this response, Whaikaha has begun scoping a medium-term work
programme on eligibility to access government funded disability support services
(DSS). As part of this work, we will be seeking to build a picture of how current DSS
structures function alongside support funded by other agencies, including what gaps
there are.
We would like to take up your offer to meet over Zoom and discuss how ANZMES
might be able to inform this work. If you would like to, please contact my colleague
Helen Walter, Group Manager, Policy to have this kōrero. Her email address is
9(2)(a)
@whaikaha.govt.nz and she looks forward to meeting with you.
Thank you again for your mahi and for contacting Whaikaha.
Ngā mihi nui
Ben O’Meara
Deputy Chief Executive, Policy, Strategy and Partnerships

Document 7
Hon. Priyanca Radhakrishnan
Minister for Disability Issues
[email address]
31st July 2023
Dear Hon. Radhakrishnan,
We would like to properly introduce ourselves and initiate a dialogue about ME/CFS and
disability support access, as we hope to have the opportunity to work together in the future.
We are the
/CFS (
/Chronic Fatigue Syndrome).
Founded in 1980, Associated New Zealand Myalgic Encephalomyelitis Society (ANZMES) was the
first of its kind in the world and we have been pioneering change for 43 years through our world
renowned medical advisors, network of researchers, community expertise, and lived experience.
Our
is a world where ME/CFS is recognised and supported. This vision focuses our
to improve outcomes for people with ME/CFS by informing best practice in healthcare,
legislation, and service provision, as the trusted leader in education, representation, and
research. This vision and mission drives our
as the leading national advisory that
produces quality, reputable, authoritative, evidence-based information to ensure that health
professionals are completely informed of best practice for the appropriate, patient-centred care
of people with ME/CFS; and that accessible service, funding, and legislation is in place to support
the needs of those with ME/CFS and their carers.
- Helping people with ME/CFS, their carers, and whānau.
- Educating through evidence-based information about ME/CFS.
- Giving people with ME/CFS a voice and taking action for them.
- Encouraging new research to help understand and treat ME/CFS.
Long COVID support
ANZMES also includes long COVID in our services due to the overlap in diagnosis, symptoms, and
management (as similar if not the same post viral condition) and the need for support.
Document 7
Fibromyalgia and dysautonomia are common comorbid conditions and/or symptom clusters that
we provide information and education about too.
ANZMES is a
and currently o ers the Know M.E. Series for health
professionals, which you are welcome to subscribe to, here:
https://anzmes.org.nz/new-cme-accredited-series-for-health-professionals/
In this Series, delivered to health professionals monthly, we explain the physiological, biomedical
evidence for ME/CFS, appropriate diagnostic criteria and tools, evidence-based, best practice for
symptom management and much more. We cover long COVID and comorbidities. We also
produce a podcast and vodcast published on public platforms featuring interviews with experts
in their respective fields about these conditions.
We have also recently produced two Resources: ME/CFS in Primary Care and long COVID in
Primary Care which provide vital information for GPs, Nurse Practitioners, Health Improvement
Practitioners, and Allied Health Professionals to use as their go-to guide for responsive patient
care. You can access these resources here:
https://anzmes.org.nz/anzmes-release-resources-for-primary-care/.
All education and resources produced by ANZMES are approved by our team of medical advisors.
On September 13 2022 ANZMES petition was presented to parliament calling for the
reclassification of ME/CFS from a chronic illness to a disability. The petition is currently with the
Health Select Committee, who are due to provide their recommendations to parliament in the
coming months. This follows an oral submission (you can watch it here
https://anzmes.org.nz/anzmes-speaks-to-parliament/) by ANZMES on May 3rd 2023, a written
submission presented in October 2022, and the petition with 6,444 signatures, submitted to
parliament in September 2022.
ANZMES created this petition to draw attention to the fact that the system is not working for
people with ME/CFS. ME/CFS fits the definition for disability, however does not fit the criteria to
access disability support services.
The government and its ministers have a legal obligation to adhere to the United Nations
(UNCRPD) Report (September 2022), which recommends that people with ME/CFS should have
access to the disability support system and be included in disability policies and programs.
People with ME/CFS are theoretically entitled to support under the chronic illness classification,
however they are not receiving it in practice.
The Needs Assessment and Service Coordination (NASC) organisation who assess home help
eligibility confirm that ME/CFS patients are not considered for assessment. Currently eligibility
criteria for NASC is for over 65 years of age, those with mental health conditions, or those

Document 7
requiring seven days per week care - meaning that those with disabling disease requiring 3-4
days care are not eligible or considered for assessment. The majority of the NASC providing
services for under 65’s, for example Auckland Regions Taikura Trust, do not provide services for
people with health conditions or long term chronic illnesses and refer this to the DHB, which then
provides inconsistent services across the regions with di ering processes and eligibility and
levels of support. This creates health care access inequity.
Along with the petition ANZMES also provided a comprehensive written report with a series of
solutions, beginning with reclassification and includes dedicated funding, a contract for
wraparound services and the creation of a tailored support structure with a tiered system that
recognises the varying degrees of disability experienced by people with ME/CFS. We also
recommend that we align our health care approach with the latest research and
recommendations by implementing a multi-disciplinary pilot.
We would like to work with you to achieve standardised nationwide criteria, policies, and services
that recognise the severely debilitating nature of this condition.
We welcome and invite you to meet with us to discuss how we can collaborate to develop quality,
accessible, disability services for people with ME/CFS and long COVID in New Zealand.
Yours sincerely
Fiona Charlton
President


Document 8
Reclassification of ME/CFS to “disability”
Addressing the needs of people with ME/CFS
Compiled for: Ministry for Disabled People, Health & Disabilities
Commissioner, Disability Rights Commissioner, Health Select
Committee, Health Ministers, COVID-19 Response Minister
Compiled by: Associated Myalgic Encephalomyelitis Society
Incorporated (ANZMES)
© 2022

Document 8
Report
Reclassification of ME/CFS to “disability”
Addressing the needs of people with
ME/CFS
Contents
Summary
3
ME/CFS
3
Diagnostic Criteria
3
Burden of ME/CFS
4
ME/CFS Status in New Zealand
4
Long COVID and ME/CFS
6
Support required
7
Home Help Services
7
Housing / Accommodations to housing
8
Financial Support
8
Social Support
9
Healthcare Equity
9
Education of Ministry and Medical Staff/Students
9
Enabling Good Lives Initiative
9
Conclusions
10
References
11
2022
2
Document 8
Summary
The Associated New Zealand Myalgic Encephalomyelitis Society (ANZMES) is calling for
reclassification of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) to disability to
allow access to support for those who suffer.
Currently ME/CFS is classified as a chronic illness, which significantly impacts the funding that people
living with ME/CFS are able to access. Currently, support is mainly provided by nonprofit
organisations.
For those people who do not recover from Long COVID (LC) after six months, they move into the
ME/CFS category, and are potentially looking at life-long or at least years of illness with significant
disability. The ME/CFS nonprofit organisations have taken on LC clients to provide requested support.
Given the estimates of prevalence due to Omicron, the burden to these organisations, and to the
healthcare system will rise significantly and require government investment.
ME/CFS patients require home help, housing support, financial support, and counselling access.
This report highlights the primary issues with delivery and support for people living with ME/CFS and
LC; and outlines potential practical solutions.
Who are ANZMES?
The Associated New Zealand Society for ME/CFS (ANZMES) has been providing information, building
awareness, funding research, and advocating for people with ME/CFS for the past 42 years (since
1980). As the national advisory body for ME/CFS in New Zealand, ANZMES disseminates
evidence-based information nationally, and represents the ME/CFS voice, globally as a founding
member of the World ME Alliance. ANZMES acts as the voice of all people living with this disabling
disease through advocacy and leadership.
ME/CFS
ME/CFS is a debilitating chronic condition, which can cause significant illness burden. Although the
precise disease burden in New Zealand is unknown, it is estimated there could be between
20,000-44,000 individuals suffering from ME/CFS in New Zealand, based on illness prevalence.1,2 The
disease affects all ages, ethnicities, and socio-economic groups.
Diagnostic Criteria
ME/CFS lacks a universally accepted case definition, and symptoms vary, but the condition can be
characterised by chronic fatigue that is not alleviated by rest. Symptom clusters for this condition
include dysfunction and dysregulation of multiple body systems, in particular the immune,
neuroendocrine and autonomic nervous systems.3,4
The 2015 Institute of Medicine (IoM) diagnostic criteria for ME/CFS classified that the state of
impairment, in the ability to engage in pre-illness levels of occupational, educational, social, and
personal activity, must have lasted at least 6 months and is not alleviated by rest.5 This long-term
health condition is accompanied by symptoms including non-restorative sleep, post-exertional
2022
3
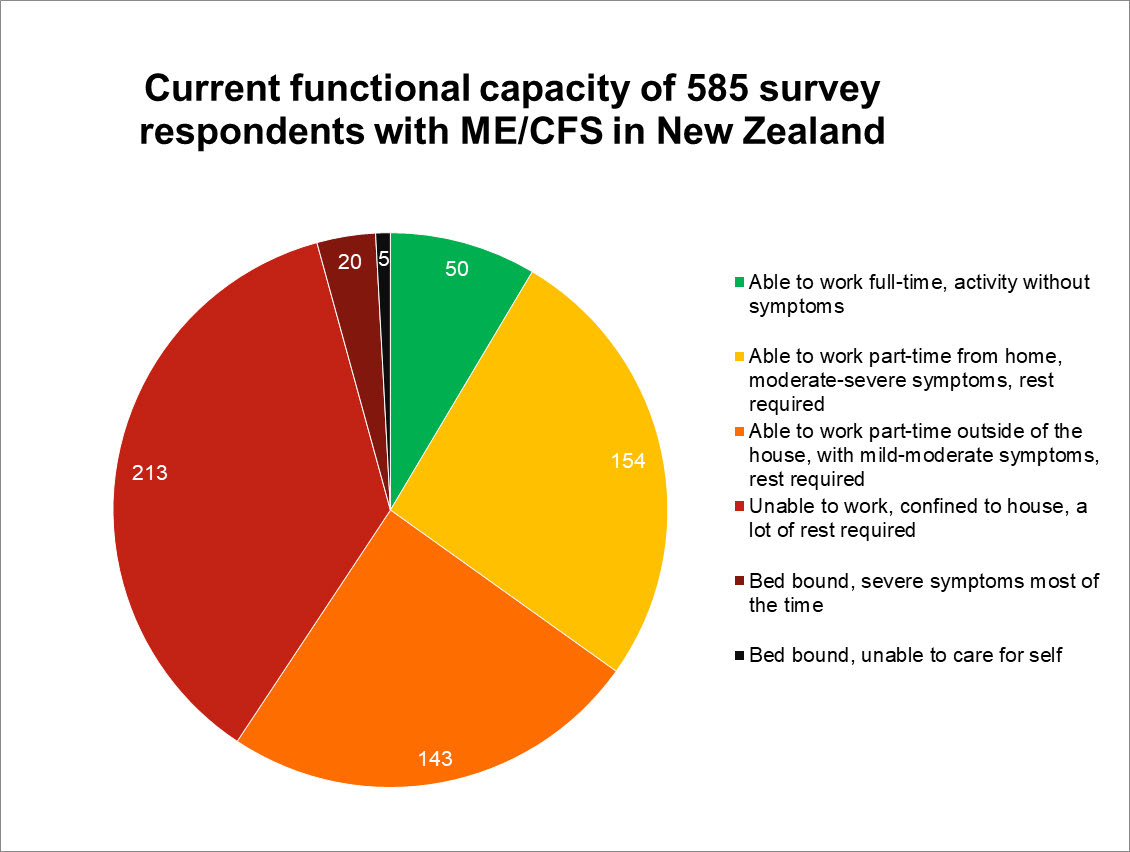
Document 8
malaise, cognitive impairment, immune dysfunction, pain, autonomic dysfunction, and/or orthostatic
intolerance.6,7 Other case definitions used are the Canadian Criteria (CC) and the International
Consensus Criteria (ICC).8
Burden of ME/CFS
Although ME/CFS experiences vary, in order to meet threshold for diagnosis, symptom severity must
cause substantial reduction in activity levels by at least 50%.9 ‘Severe’ disease is classified as house or
bed-bound, which is approximately 25-29% of CFS/ME patients.10 In a survey conducted by ANZMES
of 585 respondents with diagnosed ME/CFS, 40% reported being extremely functionally limited,
defined as unable to work, house-bound or bed-bound (
Figure 1). This limitation in functional
capacity affects ability to attend work or school and often results in severe social isolation.11 It’s
estimated that the economic cost to each individual living with ME/CFS is approximately
NZD$35-45,000 annually (based on 2017 data).12,13
Figure 1. Current functional capacity of 585 survey respondents with ME/CFS in New Zealand
ME/CFS Status in New Zealand
ME/CFS is currently classified as a “chronic illness” rather than a disability in New Zealand, a
fundamental problem, which causes difficulties with access to funding for essential support.
2022
4
Document 8
Disability is an umbrella term, with several definitions available:
New Zealand Government:
A disability is an impairment — physical, intellectual or sensory — that lasts for more than 6
months and limits your ability to carry out day-to-day activities. This can include psychiatric
illness.14
Statistics NZ:
Any self-perceived limitation in activity resulting from a long-term condition or health
problem; lasting longer or expected to last longer than six months or more and not
completely eliminated by an assistive device.15
The Human Rights Act 1993:
Physical disability or impairment: physical illness: psychiatric illness: intellectual or
psychological disability or impairment: any other loss or abnormality of psychological,
physiological: or anatomical structure or function: reliance on a guide dog, wheelchair, or
other remedial means: the presence in the body of organisms capable of causing illness.16
The World Health Organisation:
Disability refers to the interaction between individuals with a health condition (e.g., cerebral
palsy, Down syndrome and depression) and personal and environmental factors (e.g.,
negative attitudes, inaccessible transportation and public buildings, and limited social
supports).17
The United Nations:
Any restriction or lack (resulting from an impairment) of ability to perform an activity in the
manner of or within the range considered normal for a human being.
Persons with disabilities include those who have long-term physical, mental, intellectual or
sensory impairments which in interaction with various barriers may hinder their full and
effective participation in society on an equal basis with others.18
Despite the symptoms of ME/CFS meeting many of these definitions, the illness is not categorised
as a disability in New Zealand for the purpose of health-related funding and support.
Both the New Zealand Disability Support Network (NZDSN) and Access Alliance recognise ME/CFS as
a disability, allowing ANZMES to be voting members of their organisations. People with ME/CFS are
entitled to use the Hāpai Access Card to alert retailers of the barriers they face when accessing
amenities.
ME/CFS leads to significant financial disadvantages for those affected, and there is currently little or
no access to supported living services. Many of those who need it do not have access to Home and
Community Support, Respite Services, Carer Support Subsidies, and Individualised Funding. The
criteria for Home Help currently excludes ME/CFS patients as sufficiently disabled, despite significant
disease burden and limited functionality.19 The Needs Assessment and Service Coordination (NASC)
organisation confirms that ME patients are not considered for assessment. The closest equivalent
2022
5
Document 8
disease, Multiple Sclerosis (MS), is accepted for assessment, despite robust evidence that MS has
lower prevalence and less associated functional disability.25,29,36
Reclassification will lead to real improvements in quality of life for those in need. Some people with
ME/CFS become ill and never return to their pre-illness capabilities - this makes the condition
life-long.3
The Health Select Committee report 2012 supported the notion of ME/CFS as a disability. Members
of the Ministry of Health have recently advised that it would make more sense for ME/CFS to be
classed as a disability in order for a more robust level of care through ministry services.
Reclassification of ME/CFS to disability would result in:
● legitimisation and validation of a person living with ME/CFS as a disabled person, and a
protection of their rights as a disabled person,
● easier access to governmental financial support and ministry services,
● increased access to social services,
● access to need assessments as a recognised disabled person,
● access to home-help support and services, including mobility aids, and grants for home
modifications for wheelchair use,
● access to free immunisations on a voluntary basis,
● increased level of care and support through social services and educational institutions.
Long COVID and ME/CFS
It is recognised LC will likely have a substantial public health impact. Complications of COVID-19 can
sometimes linger long after initial infection, referred to as Long COVID (LC)
.20,21 A 2021 systematic
review of 57 studies, including over 250,000 people with COVID-19, showed >50% of people infected
with COVID-19 suffer at least one post-acute symptom of COVID-19, six months after infection.20
Some of those with LC have found the disease has had a debilitating impact on daily life, with brain
fog and fatigue impacting the ability to carry out usual activities, work or care for their children.3 The
current estimates suggest between 10-30% of all infections will result in LC.21 An estimated 20% of
these
may recover within 3-6 months; the rest may remain unable to return to pre-illness levels of
activity for several years, or for decades, or life – and receive an ME/CFS diagnosis.22 It is apparent
the ramifications of this wave of chronic illness will be significant.
LC and ME/CFS have been shown to have undeniable clinical similarities when using the International
Consensus Criteria for the diagnosis of ME/CFS. People living with ME/CFS understand the impact of
a prolonged and disabling illness, and insight can be gained from their experiences. ANZMES
advocated for ME/CFS experts to be included in the LC expert advisory group because of this
extensive knowledge, and insight. However these representatives were not selected to be a part of
the group, which demonstrates the governments’ unwillingness to take ME/CFS seriously. Given the
prevalence of LC in our communities it is essential that we address the inadequate support available
for those living with long-term disability as a result of illness. The government has an opportunity
now to rectify the situation and ensure that their poor treatment of those with ME/CFS does not
continue, and is not repeated in the LC community.
2022
6
Document 8
Recognising the impending healthcare crisis and the need for improved support starts with
reclassification. Reclassification to disability enables access to the support services required. Those
support services need significant investment, recruitment of qualified staff, and timely due process of
case considerations. New Zealand has well established, nonprofit organisations providing important
support services and education to people living with ME/CFS and their whānau, including home help
and nursing care. However, to provide these services to the growing membership, including people
with LC, these groups need government funding. ANZMES is the national advisory body for these
organisations and has the ability to assist in the facilitation of increased support.
Support required
ME/CFS is a condition that requires long-term support. Support can remove barriers and improve
quality of life increasing the ability to take part in family, social and community life. Providing
adequate support can lead to relief and restoration of dignity.
ANZMES supports the 2019 WEAG report recommendations that seek to provide equity and fairness
for people living with disability and disabling illness through financial support, including carers
allowance, and changing Supported Living Payments to NZ Superannuation. We believe that the
ministry needs to consider implementing these recommendations.23
Home Help Services
Many people who are diagnosed with ME/CFS require assistance with basic activities such as
dressing, eating, and hygiene.
A survey conducted by ANZMES, identified 33% of 456 respondents
with diagnosed ME/CFS required a caregiver. Quality of life and emotional wellbeing is impacted for
lay caregivers for people with ME/CFS,24 demonstrating this debilitating condition can not only
burden those diagnosed but also family members. Quality of life is significantly lower compared with
conditions such as cancer, depression, heart disease, diabetes, and rheumatoid arthritis.25 Many of
these conditions have larger funding pools and patients can often more easily access home help.
Those who suffer from ME/CFS or LC have limited energy for tasks including dressing and preparing
meals, and ‘basic’ household chores can exacerbate fatigue. With the current classification it is very
difficult for individuals with ME/CFS to receive home help services as there is a very high threshold
under the criteria for Long-Term Support for Chronic Health Conditions. Classing ME/CFS as a
disability will improve access to home help for themselves and their families, and access to benefits
that can help improve quality of life. Providing home help may improve recovery and prevent further
disability.
Buddy programmes have previously been successful in providing support to people with ME/CFS,
by significantly reducing fatigue severity.26 Models focusing on volunteer caregiving, with regular
assistance to daily chores can prevent overexertion and support individuals with daily life activities. A
government funded volunteer network could significantly improve lives of individuals with ME/CFS,
ANZMES and regional nonprofits can help coordinate this.
2022
7
Document 8
Housing / Accommodations to housing
Due to the significant impact ME/CFS has on activities, those who suffer are at a greater risk for
housing insecurity. Every New Zealander needs access to safe and healthy homes. Those with
significant mobility disabilities require adequate home environments that meet their health needs
and do not place undue burden on their family members or further contribute to social isolation or
exclusion.
As 25-29% of ME/CFS patients are either house-bound or bed-bound,8 it is vital for dignity-enabling
homes to be available to them. ME/CFS patients may have special housing needs, such as a
requirement for a home to accommodate wheelchair use, which can pose significant problems due
to the lack of accessible homes. According to Statistics New Zealand, people with a disability or
chronic condition are more likely to be in rental homes and 24% are in homes that are cold and
damp, compared to 15% of non-disabled.15
Around 20-25% of people with ME/CFS may experience such a severity of illness that they lack the
strength to walk and are bed-bound and often require a wheelchair.10 For these people the cost of
accommodating modifications for accessibility and mobility can be high (estimated up to $8,000) and
government financial assistance is only available to those classified with the term “disability.”11
Financial Support
In New Zealand currently, ACC is declining to cover support for LC if individuals cannot prove that
COVID-19 was caught in the workplace. For people with LC who remain unwell and unable to work,
consideration should be given to fall under disability classification, to provide eligibility for
government support.
Overseas research indicates that people with ME/CFS are significantly more likely to be living on a
low income, with 75% being unable to work and have substantially higher medical costs than other
individuals - paying annually, on average over $1000 for prescriptions alone.27 Symptom severity
varies significantly for ME/CFS patients, however 60% of those with ME/CFS are unable to maintain
work and school due to fluctuating and debilitating illness. Another 20% are likely to only be able to
manage part-time work.28
In a survey conducted by ANZMES of 585 respondents with diagnosed ME/CFS, only 8.5% of
respondents reported they were able to work full time (
Figure 1). The best kind of work for a person
with ME/CFS is freelance contracts where the individual can choose their hours and work from
home. Only 20% may be able to return to work/school, and lead relatively ‘normal’ lives after a
period of unwellness.
With numbers of new ME/CFS diagnosis following LC predicted to be around 30% of individuals, this
group of unsupported people may be forced into poverty due to increased medical and support bills
and lost income, without a change in classification.29
Chronically ill people often struggle to navigate the systems for support, and jump through hoops, to
only be turned down or provided inadequate support. Disability classification will allow better access
to financial support to those who need it.
2022
8
Document 8
Social Support
ME/CFS is an illness which has been tarnished with controversies and dismissal from many in the
medical community, wrongly deemed to be psychosomatic in nature.30 There is a stigma around
ME/CFS and other chronic illnesses. Often individuals who experience symptoms struggle to have
their illnesses validated and recognised, when prejudiced opinions of the condition continue to this
day.9 ME/CFS patients require better access to online, qualified counselling professionals.
Nonprofits throughout New Zealand provide online and face-to-face support, including educational
and informational presentations/resources, youth support, social gatherings, and support for carers.
With increasing prevalence, resources will become progressively stretched.
Government funding for
services facilitated by ANZMES and similar nonprofits will be vital for continued support.
Healthcare Equity
The right to experience good health is a fundamental human right that should be “enjoyed without
discrimination on the grounds of race, age, ethnicity or any other status.”31 Health equity for the
ME/CFS community is an area of concern; there is a disparity between the incidence of diagnosis of
ME/CFS in the Māori population compared to other ethnicities, which does not correlate to expected
levels based on overseas demographic studies.32
Reclassification of ME/CFS to disability may aid in
addressing inequity by removing barriers to support and improving pathways to healthcare.
Education of Ministry and Medical Staff/Students
The current health system approach, in New Zealand, for managing ME/CFS lacks consistency and
continuity of care. ANZMES are concerned that some DHB’s are using outdated UK guidelines (with
detrimental disease management advice) despite these being superseded by current guidelines from
the US Centers for Disease Control (CDC)33, NICE (October 2021),34 and evidence presented in 2015
by the Institute of Medicine.3 We propose that all agencies (MoH, MSD, ACC) adopt the same
evidence-based guidelines relating to ME/CFS as a disabling chronic neurological disease. This way
those affected have a chance in improving their health, receiving access to necessary ministry
services, and finding suitable education/employment. Dr. Vallings, one of NZ’s leading authorities on
ME/CFS, formalised the Health Pathways guidelines with Dr. Chung. ANZMES endorses these as the
preferred evidence-based option. Consensus of staff recognising ME/CFS as the medically
understood neurological disease that it is will help streamline care and this means discontinuing all
publications that refer to it as a psychological condition. This also includes no longer using medical
professionals that have this outdated stance, as external experts on cases. ANZMES’ medical team is
available for education and training.
Enabling Good Lives Initiative
Enabling good lives is a partnership between the disability sector and government agencies to ensure
people with disabilities have greater control over their lives.35 The initiative was created in 2011 with
the intent to improve quality of life by empowering individuals with disabilities; enhancing Mana
through greater recognition and respect for them and their whānau. Those with ME/CFS were shown
to experience the lowest quality of life when compared to 20 other debilitating health conditions.25
2022
9
Document 8
The inclusion of the ME/CFS and LC community in this important initiative, through reclassification
will help to address this issue of inequity.
Conclusions
There is insufficient access to support services under the current classification of ME/CFS
and LC. It is vital for ME/CFS and LC that this access is improved. This growing community of
chronically ill people deserve better treatment and urgently need more access to financial
support and health services with acknowledgment that their illness is disabling. As the new
ministry is currently still under development, now is the time to reclassify ME/CFS to
disability, to seize the opportunity to develop new pathways of support. ANZMES is able to
advise and help develop programmes needed to support people living with ME/CFS and LC.
2022
10
Document 8
References
1. Jason, L. A.
et al. A community-based study of chronic fatigue syndrome.
Arch Intern
Med 159, 2129–2137 (1999).
2. Lim, E.-J.
et al. Systematic review and meta-analysis of the prevalence of chronic fatigue
syndrome/myalgic encephalomyelitis (CFS/ME).
Journal of Translational Medicine 18,
100 (2020).
3. National Academy of Sciences. Beyond Myalgic Encephalomyelitis/ Chronic Fatigue
Syndrome. Redefining illness.
Institute of Medicine of the National Academies. (2015)
https://nap.nationalacademies.org/resource/19012/MECFS_ReportBrief.pdf
4. ANZMES. ME/CFS Awareness Day 2021, How you can help. (2021).
https://anzmes.org.nz/me-cfs-awareness-day-2021-how-you-can-help/
5. Institute of Medicine. IOM 2015 Diagnostic Criteria | Diagnosis | Healthcare Providers |
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) | CDC. (2021).
https://www.cdc.gov/me-cfs/healthcare-providers/diagnosis/iom-2015-diagnostic-criteria.h
tml .
6. Bested, A. C. & Marshall, L. M. Review of Myalgic Encephalomyelitis/Chronic Fatigue
Syndrome: an evidence-based approach to diagnosis and management by clinicians.
Rev
Environ Health 30, 223–249 (2015).
7. Nacul, L.
et al. How Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)
Progresses: The Natural History of ME/CFS.
Front Neurol 11, 826 (2020).
8. Carruthers, B. M.
et al. Myalgic encephalomyelitis: International Consensus Criteria.
Journal of Internal Medicine 270, 327–338 (2011).
2022
11
Document 8
9. Carruthers, B. M.
et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome.
Journal of
Chronic Fatigue Syndrome 11, 7–115 (2003).
10.Pendergrast, T.
et al. Housebound versus nonhousebound patients with myalgic
encephalomyelitis and chronic fatigue syndrome.
Chronic Illn 12, 292–307 (2016).
11.Boulazreg, S. & Rokach, A. The Lonely, Isolating, and Alienating Implications of Myalgic
Encephalomyelitis/Chronic Fatigue Syndrome.
Healthcare (Basel) 8, 413 (2020).
12. NICE Guideline Development Group. Myalgic Encephalomyelitis (or
Encephalopathy)/Chronic Fatigue Syndrome:diagnosis and management. NICE guideline.
National Institute for Health and Care Excellence. (2021).
https://www.nice.org.uk/guidance/ng206/documents/draft-guideline
13. Ministry of Health. Housing Modifications for Disabled People. (2022).
https://www.health.govt.nz/your-health/services-and-support/disability-services/types-disa
bility-support/equipment-and-modifications-disabled-people/housing-modifications-disabl
ed-people
14. Ministry of Health NZ. Disability. (2021).
https://www.health.govt.nz/our-work/populations/maori-health/tatau-kahukura-maori-healt
h-statistics/nga-mana-hauora-tutohu-health-status-indicators/disability.
15. Statistics New Zealand. Disability Survey: 2013. (2013).
https://www.stats.govt.nz/information-releases/disability-survey-2013
16. Human Rights Act 1993 No 82 (as at 10 May 2022), Public Act 21 Prohibited grounds of
discrimination – New Zealand Legislation.
https://legislation.govt.nz/act/public/1993/0082/latest/DLM304475.html.
2022
12
Document 8
17. World Health Organisation. (2021). Disability and health.
https://www.who.int/news-room/fact-sheets/detail/disability-and-health
18. United Nations. UN Enable : First 50 Years : Chapter II - What is a disability?. (2003-04).
https://www.un.org/esa/socdev/enable/dis50y10.htm.
19. New Zealand Government. Disability
Allowance.(2021).https://www.govt.nz/browse/health/financial-help/disability-allowance/.
20. Lopez-Leon, S.
et al. More than 50 long-term effects of COVID-19: a systematic review
and meta-analysis.
Sci Rep 11, 16144. (2021).
21. Komaroff AL, Bateman L. Will COVID-19 lead to myalgic encephalomyelitis / chronic
fatigue syndrome?
Frontiers Med. (2021). DOI:
https://doi.org/10.3389/fmed.2020.606824
22. Groff, D.
et al. Short-term and Long-term Rates of Postacute Sequelae of SARS-CoV-2
Infection: A Systematic Review.
JAMA Netw Open 4, e2128568 (2021).
23. Welfare Expert Advisory Group (2019). Creating a fairer deal for people with health
conditions or disabilities and carers. Recommendations - key and detailed.
http://www.weag.govt.nz/weag-report/whakamana-tangata/creating-a-fairer-deal-for-peopl
e-with-health-conditions-or-disabilities-and-carers/recommendations-key-and-detailed/
24. Nacul, L. C.
et al. The functional status and well being of people with myalgic
encephalomyelitis/chronic fatigue syndrome and their carers.
BMC Public Health 11, 402
(2011).DOI: 10.1186/1471-2458-11-402
25. Falk Hvidberg, M., Brinth, L. S., Olesen, A. V., Petersen, K. D. & Ehlers, L. The
Health-Related Quality of Life for Patients with Myalgic Encephalomyelitis / Chronic
2022
13
Document 8
Fatigue Syndrome (ME/CFS).
PLoS One 10, e0132421 (2015).doi:
10.1371/journal.pone.0132421..
26. Jason, L. A.
et al. Provision of Social Support to Individuals With Chronic Fatigue
Syndrome.
J Clin Psychol 66, 249–258 (2010).DOI: 10.1002/jclp.20648
27. Jason, L. A., Benton, M. C., Valentine, L., Johnson, A. & Torres-Harding, S. The
Economic impact of ME/CFS: Individual and societal costs.
Dyn Med 7, 6 (2008).
https://doi.org/10.1186/1476-5918-7-6
28. Close, S.
et al. The Economic Impacts of Myalgic Encephalomyelitis/Chronic Fatigue
Syndrome in an Australian Cohort.
Front Public Health 8, 420 (2020). DOI:
10.3389/fpubh.2020.00420
29. Arthur, A. Mirin, Mary, E. Dimmock, & Leonard, A. Jason. (2022). Updated ME/CFS
prevalence estimates reflecting post-COVID increases and associated economic costs and
funding implications, Fatigue: Biomedicine, Health & Behavior, 10:2, 83-93, DOI:
10.1080/21641846.2022.2062169
30. Neu, D.
et al. Dimensions of pure chronic fatigue: psychophysical, cognitive and
biological correlates in the chronic fatigue syndrome.
Eur J Appl Physiol 114, 1841–1851
(2014).
31. World Health Organisation. Human Rights and Health.
(2022).https://www.who.int/news-room/fact-sheets/detail/human-rights-and-health
32. Jason L.A., Richman J.A., Rademaker A.W., et al. A Community-Based Study of
Chronic Fatigue Syndrome. Arch Intern Med. (1999). doi:10.1001/archinte.159.18.2129
2022
14
Document 8
33. Centers for Disease Control and Prevention (CDC). (2022). Myalgic
encephalomyelitis/Chronic Fatigue Syndrome. https://www.cdc.gov/me-cfs/index.html
34. National Institute for Health and Care Excellence (2021). Myalgic encephalomyelitis (or
encephalopathy)/chronic fatigue syndrome: diagnosis and management (NG206).
https://www.nice.org.uk/guidance/ng206
35. Enabling Good Lives Toolbox.
Enabling Good Lives. (2022).
https://www.enablinggoodlives.co.nz/about-egl/resources/provider-resources/enabling-goo
d-lives-toolbox/.
36. Jason, L.A., Ohanian, D., Brown, A., Sunnquist, M., Klebek, L., Fox P., Sorenson, M.
(2017). Differentiating Multiple Sclerosis from Myalgic Encephalomyelitis and Chronic
Fatigue Syndrome.
Insights Biomedical, 2(2), doi:10.21767/2572-5610.10027.
33. New Zealand Health and Disability System Review - Interim Report (2019). Hauora
Manaaki ki Aotearoa Whānui – Pūrongo mō Tēnei Wā.Wellington: HDSR.
2022
15



Document 9
Reclassification of ME/CFS as a “disability”
- Outlining the issues, solutions, frameworks and benefits
Compiled for: Minister for Disability Issues, COVID-19 Response Minister,
Te Whatu Ora and Te Aka Whai Ora
Compiled by: Associated Myalgic Encephalomyelitis Society Incorporated (ANZMES)
© September 2022

Document 9
Report
Reclassification of ME/CFS as a “disability”
- Outlining the issues, solutions, frameworks and benefits
Contents
Summary
3
Who are ANZMES?
3
What is ME/CFS?
4
Who does it affect?
4
ME/CFS in New Zealand
4
Issues
5
Expert opinion
6
Solution
6
Benefits
7
Framework
7
Recommendation One - unique coding
8
Recommendation Two - one national model
8
Recommendation Three - modified NASC eligibility criteria
8
Recommendation Four - subsidised medication
10
Recommendation Five - government contract
10
Recommendation Six - pilot programme for healthcare
11
Recommendation Seven - pilot programme for mentorship
12
Conclusions
14
Appendix A
15
Appendix B
17
2022
2
Document 9
Summary
The purpose of this report is to outline the issues surrounding current classification, provide
solutions, a workable framework, and benefits to reclassifying Myalgic Encephalomyelitis/Chronic
Fatigue Syndrome (ME/CFS) as a disability.
Problem Summary
People with ME/CFS experience barriers to support and access inequity under the current
classification; due to inconsistent service delivery and management with complicated assessment
processes, disparity across regions and no dedicated funding. People with ME/CFS need consistent
access to a team of diverse health and support professionals that understand their condition and this
is currently not available. An estimated ten percent of people with Long COVID (LC) will fall into the
ME/CFS category and there is currently insufficient resources to accommodate increasing prevalence.
Proposed Solutions Summary
● Reclassification of ME/CFS from a chronic illness to a disability to improve access and support
through the existing framework for disabilities.
● Streamline the needs assessment process accounting for the fluctuating nature of ME/CFS.
● Partner with ANZMES for the delivery of educational programmes for all relevant staff.
● Work with ANZMES to develop a multidisciplinary pilot program that aligns with the latest
research and recommendations ensuring access to the right support and care, utilising LC
dedicated funding for a one stop shop approach to health care.
● Offer a mentor training program, working with ANZMES, to create a pathway for people with
ME/CFS to gradually return to work and those in need to be supported by their own
community, improving living conditions.
The government must commit to a fair financial contribution to provide improved services for people
with ME/CFS and LC - a growing community of people with significant needs.
Value/Benefits
Equitable access to health care will improve health outcomes, reduce future financial burden, offer
quality statistical data for planning of future care, and improve quality of life for people with ME/CFS.
New Zealand has the opportunity to create world-leading care and support and recognition for
people with this disabling condition.
Who are ANZMES?
The Associated New Zealand Society for ME/CFS (ANZMES) has been providing information, building
awareness, funding research, and advocating for people with ME/CFS for the past 42 years (since
1980). As the national advisory body for ME/CFS in New Zealand, ANZMES disseminates
evidence-based information nationally, and represents the ME/CFS voice, globally as a founding
member of the World ME Alliance. ANZMES acts as the voice of all people living with this disabling
disease through advocacy and leadership.
ANZMES is a member of: The World ME Alliance, Long COVID Alliance, NZ Neurological Alliance, NZ
Disability Support Network, Access Matters, and NZ Carers Alliance.
2022
3

Document 9
What is ME/CFS?
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is often triggered by a viral illness
and involves overwhelming fatigue and other symptoms that range in severity as it affects many
body systems, such as the immune, neuroendocrine and autonomic nervous system.
The key characteristic of ME/CFS is post exertional malaise (PEM) which presents 12-48 hours after
exertion, and can result in days to weeks of exacerbated symptoms. For the very severe, this exertion
can be simply trying to speak or eat.
Who does it affect?
Anyone. ME/CFS is indiscriminate – it strikes people of all ages, ethnicity, and socio-economic status.
affects immune,
neuroendocrine
and autonomic
nervous systems.
ME/CFS in New Zealand (NZ)
In New Zealand, it is estimated that there are at least 25,000 sufferers. This equates to 1 in 250
adults and 1 in 134 youth. This number is likely to increase to an estimated 45,000 due to some with
Long COVID also fitting diagnostic criteria for ME/CFS as a post-viral syndrome. The incidence is
6.25-11.25 times higher than Multiple Sclerosis, and considerably higher than a woman’s lifetime risk
of developing lung cancer. The economic cost to each family with a sufferer has been estimated to be
in the region of NZ$35-45,000 per year (2017 data).
ME/CFS is thought to afflict around 150,000 in the UK, and over one million in the US.
2022
4
Document 9
Issues
The current system creates access inequity due to complicated assessment processes and policies
and disparity between regions.
Please also refer to the extensive report produced by ANZMES and sent to Ministers in July 2022.
ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome) is currently classified as a chronic
illness and this means access to support is limited to people who require daily, full-time care because
the funding for Long Term Support - Chronic Health Conditions (LTS-CHC) is targeted towards those
with very high needs.
In 2010 funding LTS-CHC was transferred from the Ministry of Health (MoH) to the individual DHB’s
and this has led to inconsistencies between regions and access inequity (see
Appendix A). Each DHB
manages their funding and support differently, some use National Assessment Service Coordination
(NASC) to assess LTS-CHC others do not. This lack of a universal process leads to inconsistency of care
and support across the country.
Currently, there is no dedicated funding for ME/CFS within the MoH. Long Term conditions such as
diabetes and obesity are the core focus of LTS-CHC funding. Multiple Sclerosis has access to Need
Assessment Service Coordination despite significantly less prevalence and burden of disease. Yet
ME/CFS has a higher disease burden in regards to functionality. With the estimated ME/CFS and LC
patients in NZ being as high as 45,000, that is 1.2% of the population currently not catered for. Māori
and Pasifika are under-diagnosed with ME/CFS and are disproportionately affected by negative
COVID-19 outcomes.
Causes of inequity of access to health services
Complicated assessment
Service disparity
No dedicated funding
processes
across regions
for services
With changes being made within the healthcare system through the
formation of Te Whatu Ora and Te Aka Whai Ora there is an opportunity to
create better pathways and funding to care and support people with ME/CFS.
2022
5
Document 9
Expert opinion
"ME/CFS is significantly under-diagnosed and this is more a reflection of inequity in healthcare
than ME/CFS prevalence. People do not seek support because they are trying to get an easy dollar
out of the system. They do it because living with chronic illnesses and experiencing disability is
hard. It seems to me that the petition to reclassify ME/CFS as a disability is a no-brainer for a
compassionate and equity-focused society."
Dr. Tanisha Jowsey - Senior Lecturer in Medical Education, Centre for Medical and Health Sciences
Education, University of Auckland.
"Those with ME/CFS who move to a chronic phase (~75%) live fragile lives with frequent relapses
and most are not able to work, but they can have limited interactions with their communities. They
still need financial support, and sometimes support from social services. Reclassifying ME/CFS as a
disability rather than a chronic illness will give due recognition to ME/CFS as a serious disabling
illness."
Emeritus Professor Warren Tate, Department of Biochemistry, University of Otago.
"I would hope that attention to this issue also encourages discussion on improving experiences
of healthcare for those with ME/CFS. Historically the medical profession has paid limited attention
to conditions such as ME/CFS."
Kate Waterworth, Lecturer, School of Clinical Sciences, Auckland University of Technology.
Solution
The solution begins with reclassification of ME/CFS to disability; all ME/CFS patients will then be
supported under the existing framework of the Disability Support Services. Referrals for patients
would come under disability criteria.
Reclassification of ME/CFS to disability would result in:
●
legitimisation and validation of a person living with ME/CFS as a disabled
person, and a protection of their rights as a disabled person,
●
easier access to governmental financial support and ministry services,
●
increased access to social services,
●
access to need assessments as a recognised disabled person,
●
access to home-help support and services, including mobility aids, and grants
for home modifications for wheelchair use (estimated 25% are likely to require
this),
●
access to free immunisations on a voluntary basis,
●
assistance with returning to work (estimated 20% are likely to require this),
●
increased level of care and support through social services and educational
institutions.
2022
6
Document 9
Benefits
This government has the opportunity to be the global leaders of change. The UK and USA are
investigating reclassification. Australia is developing a pilot programme run by a nonprofit.
NZ could become the world's first government to recognise and validate ME/CFS by reclassifying it
as a disability. They could be the first government to fund a dedicated health pilot programme, using
the expertise of ME/CFS nonprofit organisations.
The data produced by the coding and pilot programmes would be recognised worldwide. They would
also enable a deeper understanding of the healthcare needs and treatments of ME/CFS and LC.
Reclassifying ME/CFS to disability will ensure that The United Nations September 2022 report is
adhered to, in which they recommend that: people with ME/CFS should have access to the
disability support system and be included in disability policies and programs (53c).
● Leading change - world first reclassification
● Improve health outcomes through equitable access to health services
● Reduce inequity of access
● Reduce long term burden on healthcare system by providing wraparound
services that improve outcomes (less people developing severe ME through
support)
● Real statistical data (tracking, monitoring through coding and pilot
programmes)
● Adherence with The UN recommendations
● ME/CFS economy - more in employment, less on government allowances
Framework
On the following pages a framework is outlined as recommendations for how the solution may
operate within Whaikaha Ministry of Disabled People. This includes a universal referral process with
appropriate eligibility criteria used throughout NZ by Te Whatu Ora and Te Aka Whai Ora in all
regions.
How the solution may operate:
● Unique code for tracking
● One nationwide model
● Modified NASC eligibility criteria
● Subsidised medication
● Government contract - dedicated funding
● Pilot programme for healthcare
● Pilot programme for mentorship
2022
7
Document 9
Recommendation One
- unique coding
There is a Long COVID (LC) code and it is understood that there is a code for ME/CFS at MSD but not
in the healthcare system. A unique code for ME/CFS will enable real time tracking of diagnoses and
treatment plans. This would enable more accurate data for funding purposes and better
understanding of prevalence, in NZ, so that future healthcare plans can be modified accordingly.
Currently prevalence is estimated based on overseas data. This would mean this government could
obtain accurate data that can be used to monitor long term health outcomes and equity of access.
Current prevalence is estimated up to 25,000 (45,000 with
people with Long COVID fitting ME/CFS diagnostic criteria).
Recommendation Two
- one nationwide model
With the formation of Te Whatu Ora and Te Aka Whai Ora as the national health services there is an
opportunity to use one exemplary model and roll it out nationwide.
The Wairarapa District Health Board provides an access service for support that could be a model for
providing a consistent service nationwide. Their service, known as FOCUS, offers a single point of
entry for support referrals and people are paired with a community coordinator who assesses their
needs and assists them in accessing services. Anyone can refer to them for support and their criteria
is more open, flexible, and patient-centred. This centralised approach to care simplifies the process
improving access for people who may struggle to navigate a complicated system alone. It offers a one
stop shop approach that streamlines access to health care services. ANZMES recommends that a
patient-experience survey is conducted to assess the success of this programme for people with
ME/CFS, and if it proves efficient, then there is potential for FOCUS to be adopted as the nationwide
model for disability/long term conditions support, with ME/CFS included.
Recommendation Three
- modified NASC eligibility criteria
Eligibility for access to Needs Assessment Service Coordination (NASC) should not be subject to age.
See
Appendix A for current examples. Criteria, nationwide, should be based on the definition of
disability released by the NZ government:
A disability is an impairment — physical, intellectual or sensory — that lasts for more
than 6 months and limits your ability to carry out day-to-day activities. This can
include psychiatric illness.
2022
8
Document 9
The United Nations refer to barriers to participation which is especially poignant for people with
ME/CFS who can be so disabled by the disease that they are bedbound or housebound (25-29% of all
people with ME/CFS):
Any restriction or lack (resulting from an impairment) of ability to perform an activity in the
manner of or within the range considered normal for a human being. Persons with disabilities
include those who have long-term physical, mental, intellectual or sensory impairments
which in interaction with various barriers may hinder their full and effective participation in
society on an equal basis with others.
Please refer to page 4 "Burden of ME/CFS" in the ANZMES report entitled "Reclassification of ME/CFS
to “disability” Addressing the needs of people with ME/CFS" sent to Ministers in July 2022 for more
information on barriers to participation, and page 8 "Housing/Financial Support" for an
understanding of employment barriers and effects.
The Health Select Committee report 2012
supported the notion of ME/CFS as a disability.
This refined eligibility criteria ensures that ALL people with ME/CFS are eligible for access to support
services as required.
At an operational level, within the disability framework, this would improve equity of access to the
health system and its vital services for people with ME/CFS and LC. Which in turn may improve
health outcomes.
Of the estimated 25,000 (potentially 45,000 with those with LC fitting diagnostic criteria for ME/CFS)
15% may be classed as mild-moderate, 60% moderate-severe, and 25% severe-very severe.
Broadening the eligibility criteria for support services would make it easier for mild-moderate and
moderate-severe patients to access disability services under the new model as a first and second tier
approach. Mild-moderate patients need very little support, if any, but they do need the recognition
of ME/CFS as a disability in order to access workplace accommodations as required when living with
a long term illness.
Moderate-severe patients may require some home help services at certain times, or for 3-4 days per
week. Severe-very severe patients may require ongoing home help services, 7 days per week, and in
a certain smaller number of cases, 24/7 care. Currently only the latter category is eligible for NASC
and therefore support such as: home help with housework, personal care, meals, and
accommodation modification.
15%
60%
25%
mild-moderate
moderate-severe
severe-very severe
ME/CFS is a fluctuating disease with cycles of relapse and remission of severe symptoms; during an
illness journey a person with ME/CFS could be classed as having moderate-severe ME, move into the
2022
9
Document 9
severe-very severe category for several months, requiring additional support, only to move back to
moderate-severe again. More than one needs assessment may be required for an individual patient
based on their fluctuating needs.
The paired relationship between patient and community coordinator used by FOCUS enables
continuity of care. With one coordinator overseeing all service referrals they will learn more about
the individual patient's needs and these relapse and remission cycles, making it easier to justify more
than one NASC assessment over the course of the chronic illness duration.
Recommendation Four
- subsidised medication
Overseas research indicates that people with ME/CFS have substantially higher medical costs than
other individuals and subsidising medications may reduce this burden.
Low Dose Naltrexone has been shown to benefit chronic pain experienced with ME/CFS however
here in New Zealand, it is a prescription drug that is not funded. It may need to be made up by a
specialised compounding pharmacy, which creates added costs.
A 6-week course of B12 injections is also recommended for ME/CFS.
Some antivirals help to deactivate the Epstein Barr virus (and others) which are known to reactivate
when the immune system is under stress.
Antihistamines are also an effective treatment for some people with ME/CFS who have high levels of
mast cells activated in their body.
Most people with ME/CFS use supplements such as: Co-enzyme Q10, MitoQ, and electrolytes. It
would be helpful to have subsidisation at local pharmacies to reduce the burden of ongoing costs.
Recommendation Five
- government contract
ANZMES and its regional member support groups and organisations throughout NZ have been
subsidising the healthcare system for decades by providing a wraparound service of support to
people with ME/CFS and now recently, LC. These services are provided efficiently and cost-effectively.
Primary care is short-term, however, people with chronic conditions require ongoing support
services, which currently exist through all the regional members and ANZMES as the national
advisory body. Time is long overdue for the government to provide fair contribution through a
contract that enables increased resources for proper support of those with LC, and continue the vital
service for pwME.
Given there is no dedicated funding for ME/CFS currently, there will be an outlay to provide this
service, but this investment will improve long term outcomes through equity of access, universal
support, accurate information dissemination and education of relevant parties. ANZMES is offering to
partner with relevant agencies so that these agencies gain access to 42 years of experience.
2022
10
Document 9
A contract with ANZMES would ensure that all people living with ME/CFS and LC have access to wrap
around services locally, through the many support groups currently operating, and through liaison
with the community coordinator in charge of their care (e.g. FOCUS model). Currently ANZMES and
its member organisations (ME/CFS Support Auckland, ME/CFS Canterbury, MEISS, Rest Assured
Respite Trust, and Complex Chronic Illness Support) are heavily reliant on grants, donations, and
sponsorship to deliver its services, which is becoming increasingly difficult to obtain and sustain.
ANZMES provides some start-up funding for small non-registered regional support groups, and
funding to the member organisations for specific expenses related to education of the community
and medical professionals. Government funding would enable continuity of care throughout New
Zealand, improving equity of access to health and support services.
A contract with ANZMES would ensure that Te Whatu Ora and Te Aka Whai Ora have access to the
most up-to-date evidence-based research, resources, information, and experts through the networks
and relationships already established by, and with, ANZMES and its member organisations.
It would enable ANZMES to deliver a nationwide education programme to medical professionals
within Te Whatu Ora, Te Aka Whai Ora, and ministry staff (e.g. MSD, MoH, Whaikaha) to reduce the
inconsistencies still observed in the attitude and care of patients presenting with this condition.
A contract would enable ANZMES to deliver a nationwide education programme to insurers in the
health system to ensure they are operating with the correct information and not outdated treatment
recommendations, which we know is currently occuring.
A contract would enable the organisations and healthcare team to support graduated return to work
if appropriate, and increase services to more people living with these conditions.
Partnerships with Māori and Pasifika healthcare providers, trained by ANZMES on ME/CFS diagnostic
criteria and symptom management, may improve equity in healthcare for these groups.
A fair contribution, through a formal contract with government to deliver services in partnership with
Whaikaha and Ministry of Health and Ministry for Social Development, would potentially be $5
million per year given to ANZMES to redistribute amongst the regional entities and ensure delivery of
the above educational programmes.
Recommendation Six
- pilot programme for healthcare
Multidisciplinary health pilot programmes have been used successfully for other health conditions
overseas such as heart disease. See
Appendix B for pilot programmes being trialled globally.
The World Health Organisation (WHO) recognises that ME/CFS needs a multidisciplinary healthcare
approach. A pilot programme involving specialised care for people with ME/CFS could be created
with ANZMES, allied health, such as specialist physiotherapists, nurse practitioners, nutritionists and
GP’s familiar with the condition. A team of specialists providing individualised support plans has been
outlined as best practice care set out in the National Institute for Health and Care Excellence (NICE)
2021 Guidelines for treatment of ME/CFS.
2022
11
Document 9
South Australia has an example of a unique one stop shop for care and research for ME/CFS. The
charity Bridges and Pathways is creating the ME/CFS Multidisciplinary Clinical and Research Centre
with the goal of improving services for people with ME/CFS, which is a central point for specialist
care teams to work together with research creating a source of validated patient centred care
approaches.
An early diagnosis and correct management of symptoms can lead to a better prognosis. By bringing
in care earlier, it may save care costs long term. Investment in treatment now may lessen the burden
for the future, as appropriate support offers the potential to reduce the number of people who fall
into a severe category due to lack of home help services.
The most defining feature of ME/CFS and LC is Post Exertion Malaise, which means that the ability to
exert energy is limited due to malfunction of energy production, and the consequences are long
periods of rest.
The energy envelope describes the first aid approach to managing the body's functional capacity for
activities. Teaching patients to stay within their energy envelope can help reduce symptom
exacerbation and can be managed with functional measures such as monitoring heart rate and
breathing rate.
With LC the severity varies, however some people are reporting that even with very little exertion
they have a significant increase in their symptoms and become bedbound for days.
If people are able to operate now within energy envelopes due to help with chores
at home, over time their bodies may heal enough that they can manage it
themselves, or return to work.
Recommendation Seven
- pilot programme for mentorship
A pilot programme for mentorship and vocational opportunities may reduce inequity for people with
ME/CFS.
Often, ME/CFS hits well-educated, working professionals, who when unable to work full time due to
symptom severity, experience reduction in income or unemployment, increased medical costs, and a
lowering of their social economic status.
This means people with ME/CFS are often living in poverty and reliant on government financial
support.
Overseas models of buddy programmes have seen success in using trained mentors to provide
support to people with ME/CFS, significantly reducing fatigue severity. Models focused on regular
assistance with daily chores can prevent overexertion and support individuals with daily life activities.
2022
12
Document 9
These mentors, made up of people with ME/CFS could be trained to provide peer support, liaise with
wraparound service providers and community nurse practitioners, and report on the ongoing needs
of people with ME/CFS and LC. This fosters self-empowerment of the mentors and mentees. This
model will enable real time statistics to be established to better understand the diseases.
This pilot would enable the beginning of training and creation of part-time work opportunities for
people with ME/CFS and LC. More people with ME/CFS and LC could then return to the workforce
with less reliance on government benefits. Rest Assured Respite Charitable Trust have reintegrated
people with ME/CFS into part-time employment through their charitable shops in Auckland. Two
testimonials for this trial follow:
“I started volunteering at The Charity Boutique in Howick in June. It was hard at first, but it did feel
great being out and helping people in the community. I love helping others and meeting new people,
so volunteering was a great start. It was nice to help with a charity/trust that helps people in the
community that deals with what you are living through daily. I was [then] offered a job at their new
store. Having a job after so many years, it has given me a more positive look on life and my illnesses.
After so many years spent at home and in so much pain, I honestly thought this was my life till the
end. Every day is still a challenge and I need to take one day at a time. Having the support from Rest
Assured Respite Charitable Trust, I was given the opportunity to return to part time work.” TL
“We asked about the chance for an afternoon once a week volunteering. We were absolutely
delighted to be able to help in this way. We were new to the area, and I was pleased to have a chance
to meet people from the community, AND to feel we were being productive and “giving back” a little,
it was brilliant. The fact it was volunteering meant that we could start on just a few hours, and test
out our health. When you have been housebound for a long time it is hard to know what standing for
a few hours would be like!” NH
Currently and estimated 60% of people with ME/CFS are unable to maintain work and school outside
of the home due to fluctuating symptoms and symptom severity. A percentage of these may manage
home-based work where they can choose their hours, and conduct the work on a computer, in bed,
if necessary.
Mentorship could be conducted virtually through online video conferencing.
There is an opportunity for this government to pilot this idea and thus create a ME/CFS economy,
and in the future introduce the model to other disability and long term condition patient groups.
2022
13
Document 9
Conclusions
Reclassification will legitimise ME/CFS as a disability and with broadened eligibility criteria using the
government definition for disability will enable all patients with ME/CFS to access NASC and relevant
home help services.
This will be a world first, and this NZ government could lead global change.
ANZMES believes that diagnosis, treatment, and patient experience will be more easily tracked for
accurate prevalence data with the creation of a unique code within the health system. Subsidised
medications and supplements will provide an affordable option for people with ME/CFS to manage
their symptoms.
The government should commit to a fair financial contribution to provide improved services for
people with ME/CFS and Long COVID - a growing community of people with significant needs.
ANZMES will then be in the position, with 42 years experience, to provide training to agencies,
medical professionals, and partner with Te Whatu Ora and Te Aka Whai Ora to ensure continuity and
consistency of care nationwide, using FOCUS as an exemplary model.
A multidisciplinary health and mentorship pilot programme will also enable necessary patient
centred approaches, and initiate the development of an ME/CFS economy, where people with the
disease can mentor others and perhaps obtain gainful part-time employment, thus reducing reliance
on government benefits.
Equitable access to health care will improve health outcomes, reduce future financial burden, offer
quality statistical data for planning of future care and improve quality of life for people with ME/CFS.
2022
14
Document 9
Appendix A
Differing accessibility and services at the various DHBs.
Auckland - DHB has funding for ME/CFS through the NASC, but under 65s must be very high needs
(24 hr care) to access these services.
Central Auckland - under 65s come under Taikura Trust who do needs assessment. Criteria: very high
needs, must be lifelong, having depression as part of illness may exclude people from care. Most
people with ME/CFS would not fit criteria. They do not take self-referrals like the other regions.
Counties Manukau - uses Community Central for all needs assessment - however the messaging
around this is very ambiguous because they also state that “0-64 years of age with an on-going
disability who require support will be assessed by Taikura Trust for needs assessment and facilitation
of services” but Taikura is for very high needs as above. People may be passed around these services
resulting in eventually no help.
Bay of Plenty - SUPPORT NET - does needs assessment and coordination and anyone can refer - even
family or self referral.
Capital Coast and Hutt Valley - CAPITAL SUPPORT - does both needs assessment and coordination,
eligibility is for high needs and states that it doesn’t generally cover chronic health conditions or
fatigue, so most people with ME/CFS can’t access what they offer, although anyone can refer and
they will decide individually whether to assess. They also list behavioural support which no other
DHB mentions.
Hawkes Bay - has Long Term Conditions Framework based on Four Aka (roots);
Person-Family-Whanau Centred Care, Person centred systems and processes, Workforce
development and enablement, and Risk identification and mitigation. The framework is not disease
specific, and has its own review system.
Hutt Valley - information no longer available.
Lakes (Rotorua/Taupo) - NASC assess and coordinate. Criteria: vague and for over 65. “This service is
for people over 65 years of age, who have long term loss of independent function and require
assistance with normal daily tasks. Excluded are people who are: Covered under the Accident
Compensation Act (ACC) may not be eligible. People who require assessment solely as a result of a
personal health need (e.g. they require ongoing supervision by a health professional) this usually
means asthma and diabetes but not necessarily ME/CFS. People who are not a resident of New
Zealand” This is different to most other DHB listed exclusions.
Midcentral - have Kaituhono/connectors mainly targeted at disability defined conditions but no clear
rules for who might use this service. 2019 Policy document to address inconsistency - “The
Supportlinks NASC service will ensure the population eligible for LTS-CHC services, do receive the
services that they are entitled to. Every effort will be made to consider which services have District
Health Board contracts and appropriate discussion elevated to NASC Management where necessary.”
2022
15
Document 9
Nelson Marlborough - DHB does needs assessment service but have no real coordination service for
long term health conditions they simply refer people to other groups - physio, Supported
Independent Living. It is mostly targeted to those classified as a disability.
Northland - their website has great information about ME that has been reviewed by Dr. Ros Vallings.
Northable - dedicated disability support services, unclear if ME/CFS fits the criteria.
Southern - extremely difficult to find anything that caters for ME/CFS. DHB Needs assessment is for
over 65 or those with very high needs.
South Canterbury - their information is generally unhelpful and would be hard to navigate if you
were looking for ME/CFS support. Services of NASC are only for over 65 and classified as disability. It
appears some responsibility to assess chronic illness support is given to primary health - GPs and
hospital occupational therapists.
Tairawhiti - information no longer available.
Taranaki - runs care manager community support service - Needs assessment is mainly for over 65
and for short term disability but will take very high needs referrals of complex long term conditions
needing support. This is however not obvious to the public only mentioned in a pdf.
Waikato - Health of Older People (HOP) team run all needs assessment. ME/CFS would come under
their DSS Disability Support Services (DSS) 0 to 65. Any person can make a referral to the disability
support link for assessment but falls under high needs category for long term conditions.
Wairarapa - FOCUS - a one stop shop for referrals for long term conditions and disabilities. A patient
is provided with a community coordinator who conducts needs assessments and helps with
everything including supporting carers.
Criteria: A long-term impairment is one that lasts longer than 6 months, has reduced your ability to
be independent, and means you require some form of support.
Waitemata - NASC geared towards older persons, does include younger persons with chronic health
conditions, but limited detail.
West Coast - comes under older persons support called Complex Clinical Care Network - they do
assessment and then a tailored care plan.
Whanganui - has been criticised in the media for dangerous wait times for needs assessment.
Contracted out to Life Unlimited and Access Ability who do the assessment and coordination. People
with ME/CFS may be eligible for a needs assessment and some support based on this vague criteria “
To be eligible for a Needs Assessment, your disability must last longer than six months and you must
need support in some parts of your life because of your disability.”
2022
16
Document 9
Appendix B
Examples of healthcare pilot programmes from around the world.
New Zealand - Mana Whaikaha - based in MidCentral under Enabling Good Lives National concept. A
single point of contact - Kaituhono/Connectors - build “Good life plan” for disabled. Funding from
MoH and community initiative.
Australia - They are looking at creating a pilot multidisciplinary Clinic and Research Centre that feeds
info to GP’s and other care providers. Funding is donations and fee based, will be a non-government
health service, based on a business model where staff salaries will need to be covered. Services are
consistent with Australian Medicare and private health funding schedules, which means there will be
a fee-for-service to cover gaps.
USA - Clinician Coalition - a group of experts working together for ME/CFS education of medical
professionals and to inform research. They make online CME courses, which is something that could
be added to the Pilot programme.
UK - Multidisciplinary organisation of clinicians working with ME/CFS called BACME. Health
professionals join it and receive centralised education.
Funding - comes from Lottery and Community Funds and from health professionals membership and
a conference that GPs pay to go to.
Buddy program: Undergraduate students of psychology and social work, received course credits not
payment. Provision of social support to individuals with chronic fatigue syndrome.
Existing multidisciplinary pilot programs for other health conditions:
Pelvic health pilot - aiming for more cohesive, seamless care. Uses nurses as navigators as single
point of contact. Funding - Advent Health is a Christian fund - community and church enterprise
Fibromyalgia - small multidisciplinary pilot study - treatment from doctor, dietitian, physio
collaboration. Funding - Physiotherapist foundation and Rheumatologist research
Heart failure - Cost analysis for heart failure using a multidisciplinary program - showed more cost
effectiveness.
2022
17
Document 10 and 11
Excerpt from Minutes of DSS Advisory Group second meeting 4 December 2023
4.9.4 ME/CFS and long covid could fit into the option on gaps, young people’s
approach, and UNCRPD option. Long term conditions aren’t well covered in other
options. Options that focus on one single disability pit disability groups against
each other and do not align with the social model or meet our UNCRPD
obligations.
Excerpt from Minutes of DSS Advisory Group second meeting 14 February 2024
4.1.1 ME/CFS and similar conditions should be eligible but aren’t based on
impact to someone’s life. This is due to exclusion criteria.

Document 12
From:
Fiona Charlton
To:
Helen Walter; Amber Coyle
Subject:
Re: Advisory Group Workshop - Review of Eligibility for Disability Support Services (DSS)
Date:
Wednesday, 14 February 2024 5:38:05 pm
Attachments:
image001.png
BIM Infographic ANZMES.png
Reclassification Report ANZMES July 2022.pdf
Reclassification of ME CFS - issues, solutions, frameworks and benefits.docx.pdf
Petition Written Submission ANZMES Oct2022.pdf
Neurological Alliance BIM - Health - Feb 2024.pdf
Neurological Alliance Feb 2024 Infographic.pdf
HSC 2022 Final report (Petition of ANZMES).pdf
Hi Helen and Amber
I have attached:
Report titled "Reclassification of ME/CFS - addressing the needs" which provides some
information about burden, costs.
The cost of doing nothing highlighted in the attached infographic. I can send our full BIM
when it is completed.
The written submission for our petition which outlines the various discrepancies for NASC vs
LTC-CHC.
Appendix A of the Report titled "Reclassification of ME/CFS - outlining the issues, solutions,
frameworks, benefits" provides the different NASC eligibility criteria around the country.
The oral submission and rebuttals: https://anzmes.org.nz/anzmes-speaks-to-parliament/
and https://anzmes.org.nz/anzmes-speaks-on-rnz-about-reclassification/ provides
simple conclusions around what is and isn't working.
Health Select Committee Report that states that ME/CFS should be eligible for Whaikaha.
Neurological Alliance BIM Report February 2024 and infographic.
To get an idea for your costings. It is estimated that at least 25,000 people live with ME/CFS. Of
all COVID-19 cases, 10% will meet the diagnostic criteria for ME/CFS. We could
conservatively increase the number then to around 70,000. But it may be higher. As coding is not
routinely used in primary and secondary care and not tracking or reporting is conducted. This
does not mean that all these people require Whaikaha services.
ME/CFS exists on a spectrum like many conditions, from mild to very severe. The very severe
usually require 24/7 care and are entitled to NASC as "very high needs." However one example to
highlight what happens there, is a 22 year old is cared for by her mother, she requires feeding,
toileting, bathing etc. Her mother was granted 22 hours per week and due to staff shortage on 11
hours was given in reality. So technically we could say that the very-severe meet the criteria.
They account for about 2-5% of all people with ME/CFS.
However those in the moderate and severe categories, are not deemed severe enough, even
though the majority are bedbound or housebound, unable to work or exert energy for simple
tasks like housework. They are meant to get NASC through the DHBs / Te Whatu Ora under LTC-
CHC but do not fit the criteria. Given that the conditions fit the criteria for disability, it should be
included in Whaikaha. Moderate-severe account for approx 60-75% of all people with ME/CFS.
I am a chronically ill (but capable) volunteer who checks these emails intermittently. Thank you for your patience in
awaiting my reply.
Angela, our National Coordinator is our first point of contact for all communications: [email address].
Ngā mihi maioha / Thank you with appreciation
Kind Regards
Fiona Charlton
President
ANZMES
Associated NZ Myalgic Encephalomyelitis Society Inc
9(2)(a)
9(2)(a)
@anzmes.org.nz
www.anzmes.org.nz