 Pragmatic Evidence Based Review
The efficacy of acupuncture in the
management of musculoskeletal pain
Reviewer
Date Report Completed
August 2011
Important Note:
Pragmatic Evidence Based Review
The efficacy of acupuncture in the
management of musculoskeletal pain
Reviewer
Date Report Completed
August 2011
Important Note:
•
This report is not intended to replace clinical judgement, or be used as a clinical
protocol.
•
A robust evidence-based review of clinical guidelines, systematic reviews and high
quality primary evidence relevant to the focus of this report was carried out. This
does not however claim to be exhaustive.
•
The document has been prepared by the staff of the research team, ACC. The
content does not necessarily represent the official view of ACC or represent ACC
policy.
•
This report is based upon information supplied up to 31st July 2011
Purpose
The purpose of the report is to;
• Briefly describe traditional Chinese medicine (TCM) acupuncture and western
medical acupuncture
• Report the efficacy of acupuncture for the treatment of injury-related spine, shoulder,
knee & ankle conditions
• Report the comparative efficacy of acupuncture when considering alternative
conservative treatment interventions for the spine, shoulder, knee & ankle
• Report any adverse reactions cited in the literature.
Scope
This report will be restricted to acupuncture involving various modes of needling (including
electroacupuncture) for musculoskeletal pain from knee, spine, shoulder and ankle injuries.
Treatment modalities of TCM like cupping, scraping, Chinese massage, and herbalism will
not be addressed.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page 1
No distinction will be made between traditional Chinese medical acupuncture and western
medical acupuncture
Summary Message
The evidence for the effectiveness of acupuncture is most convincing for the
treatment of chronic neck and shoulder pain. In terms of other injuries, the evidence is
either inconclusive or insufficient. The state of the evidence on the effectiveness of
acupuncture is not dissimilar to other physical therapies such as physiotherapy,
chiropractic and osteopathy.
Key findings
General
• There is insufficient evidence to make a recommendation for the use of acupuncture
in the management of acute neck, back or shoulder pain
• There is emerging evidence that acupuncture may enhance/facilitate other
conventional therapies (including physiotherapy & exercise-based therapies)
• There is a paucity of research for the optimal dosage of acupuncture treatment for
treating shoulder, knee, neck and lower back pain
• Studies comparing effective conservative treatments (including simple analgesics,
physical therapy, exercise, heat & cold therapy) for (sub) acute and chronic non-
specific low back pain (LBP) have been largely inconclusive
Lower back
• The evidence for the use of acupuncture in (sub)acute LBP is inconclusive
• There is limited evidence to support the use of acupuncture for pain relief in chronic
LBP in the short term (up to 3 months)
• The evidence is inconclusive for the use of acupuncture for long term (beyond 3
months) pain relief in chronic LBP
• There is no evidence to recommend the use of acupuncture for lumbar disc herniation
related radiculopathy (LDHR)
Neck
• There is good evidence that acupuncture is effective for short term pain relief in the
treatment of chronic neck pain
• There is moderate evidence that real acupuncture is more effective than sham
acupuncture for the treatment of chronic neck pain
• There is limited evidence that acupuncture has a long term effect on chronic neck
pain
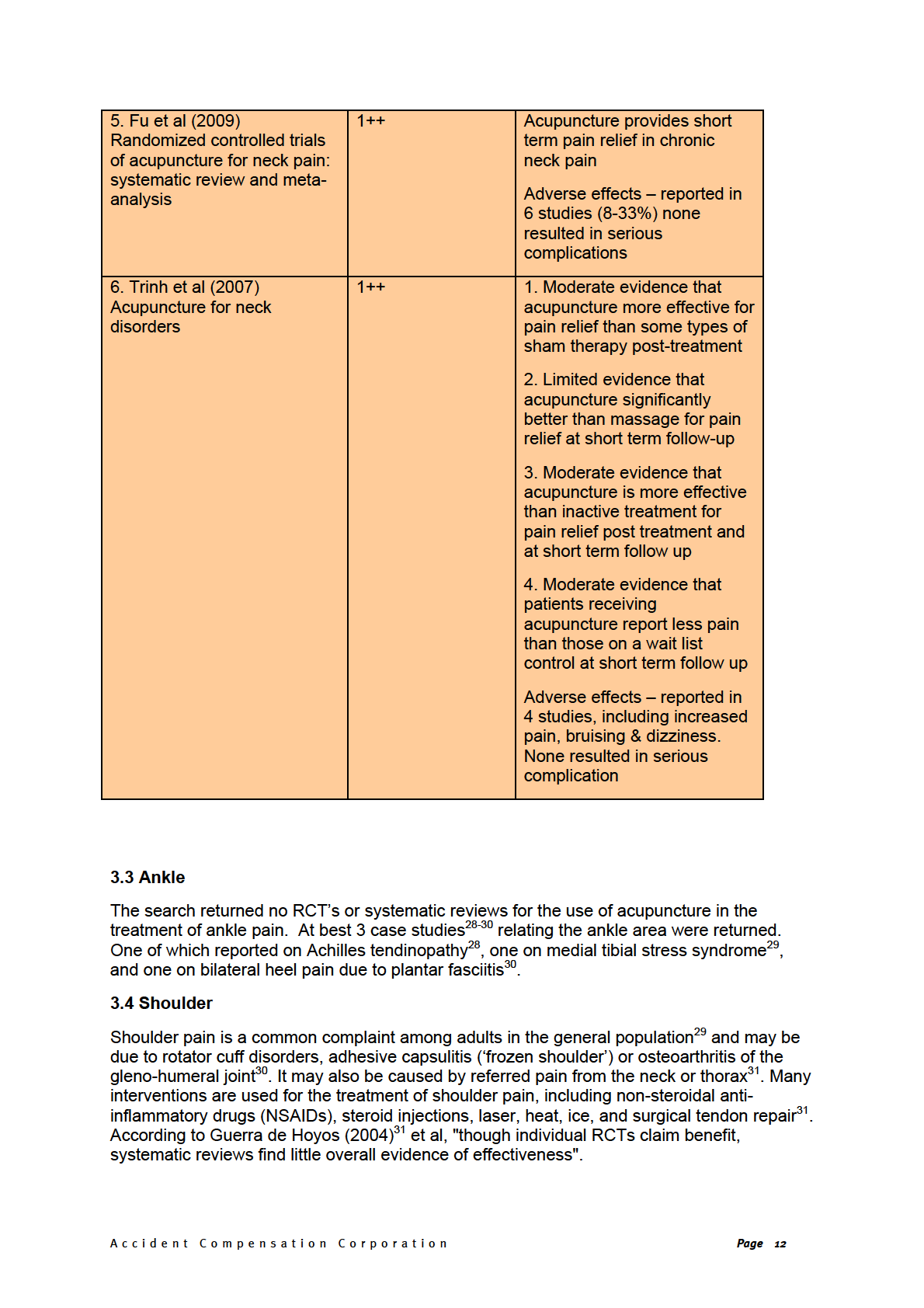
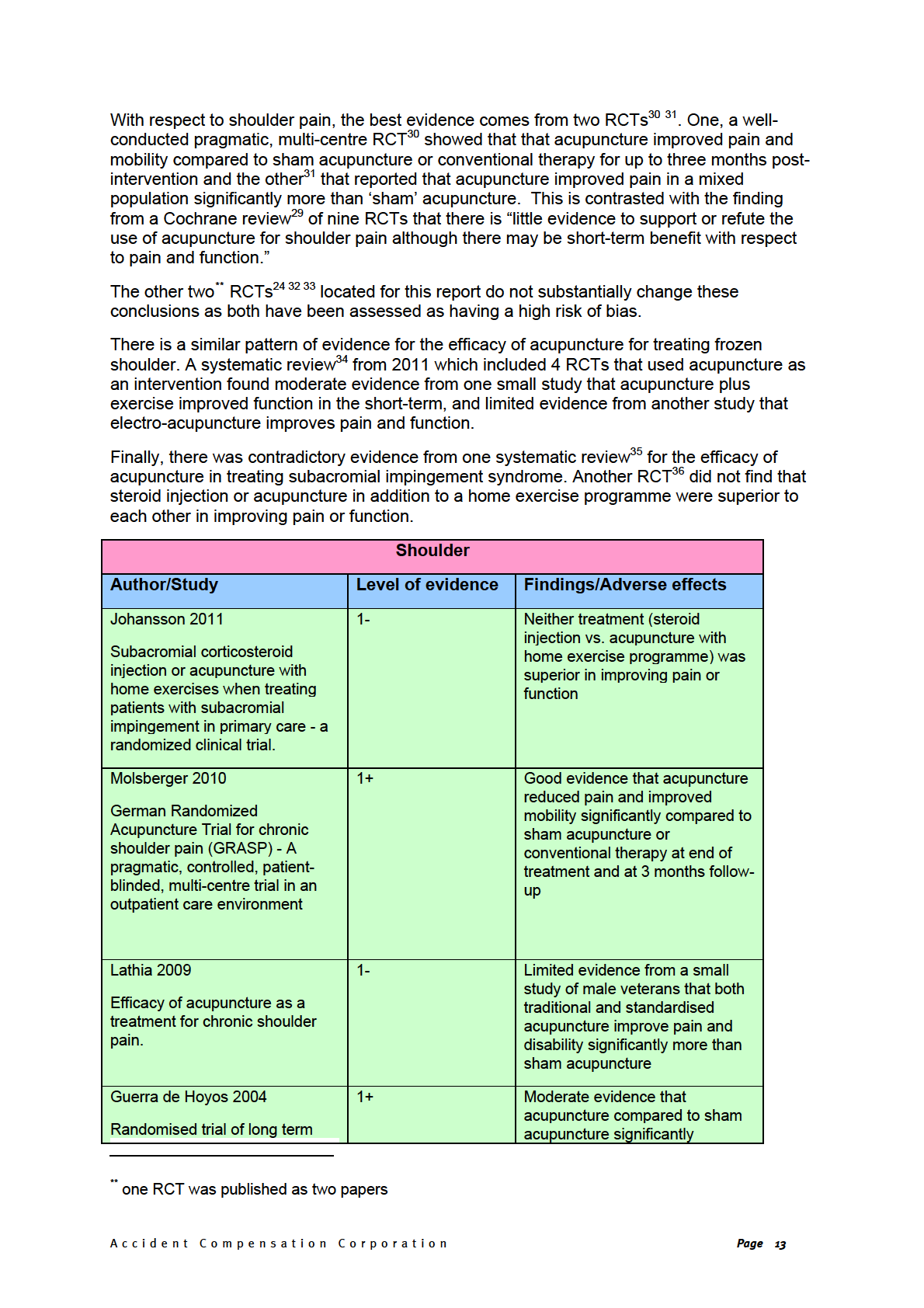
Shoulder
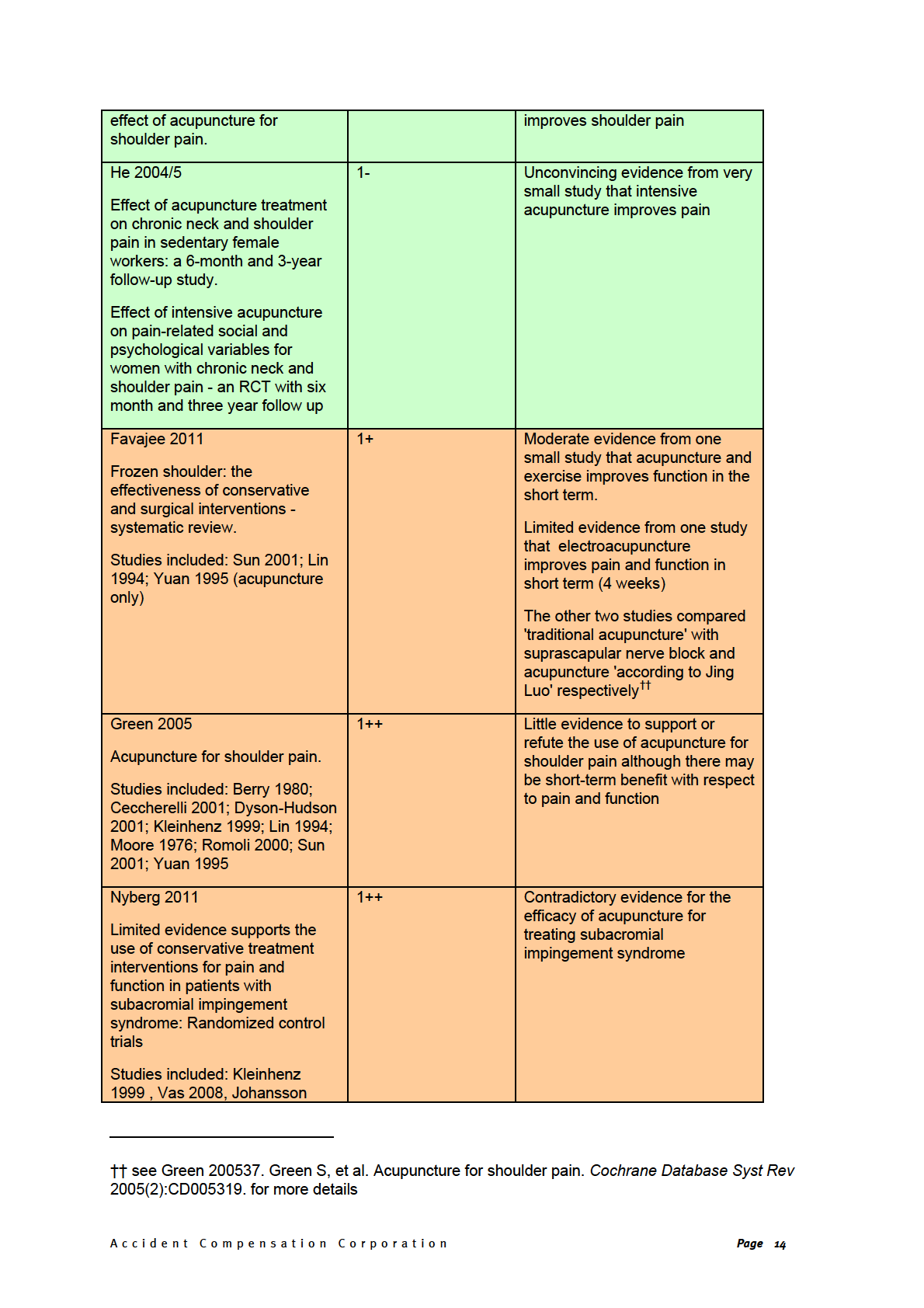
• There is good evidence from one pragmatic trial that acupuncture improves pain and
mobility in chronic shoulder pain
• There is limited evidence for the efficacy of acupuncture for frozen shoulder
• There is contradictory evidence for the efficacy of acupuncture for subacromial
impingement syndrome
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page 2
Knee
• There is no evidence to recommend the use of acupuncture for injury-related knee
pain
Ankle
• There is no evidence to recommend the use of acupuncture for ankle pain
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page 3
Background
Acupuncture has roots in ancient Chinese philosophy. Traditional Chinese Medicine (TCM)
acupuncture is based on a number of philosophical concepts, one of which is that any
manifestation of pain/dysfunction is a sign of imbalance of energy flow within the body. It is
in this context that the TCM acupuncturist uses a holistic treatment approach. TCM
acupuncture involves inserting needles into traditional meridian points with the intention on
influencing energy flow within that meridian1. Acupuncture has been adopted into western
medicine and treatments; many physicians currently practicing acupuncture reject such pre-
scientific notions described above, using unnamed tender or trigger points to stimulate
nerves or muscles1. Further to this acupuncture is also now regularly practiced globally by a
specialist sub-group of physiotherapists and some other health professionals. New Zealand
physiotherapists have been practicing acupuncture since 19722.
As a technique acupuncture includes the invasive or non-invasive stimulation of specific
anatomical locations by means of needles or other thermal, electrical, light, mechanical or
manual methods3. Acupuncture is most commonly used to treat chronic pain4 5 and is
currently used for a variety of conditions, including; spinal cord injury6, visceral dysfunction
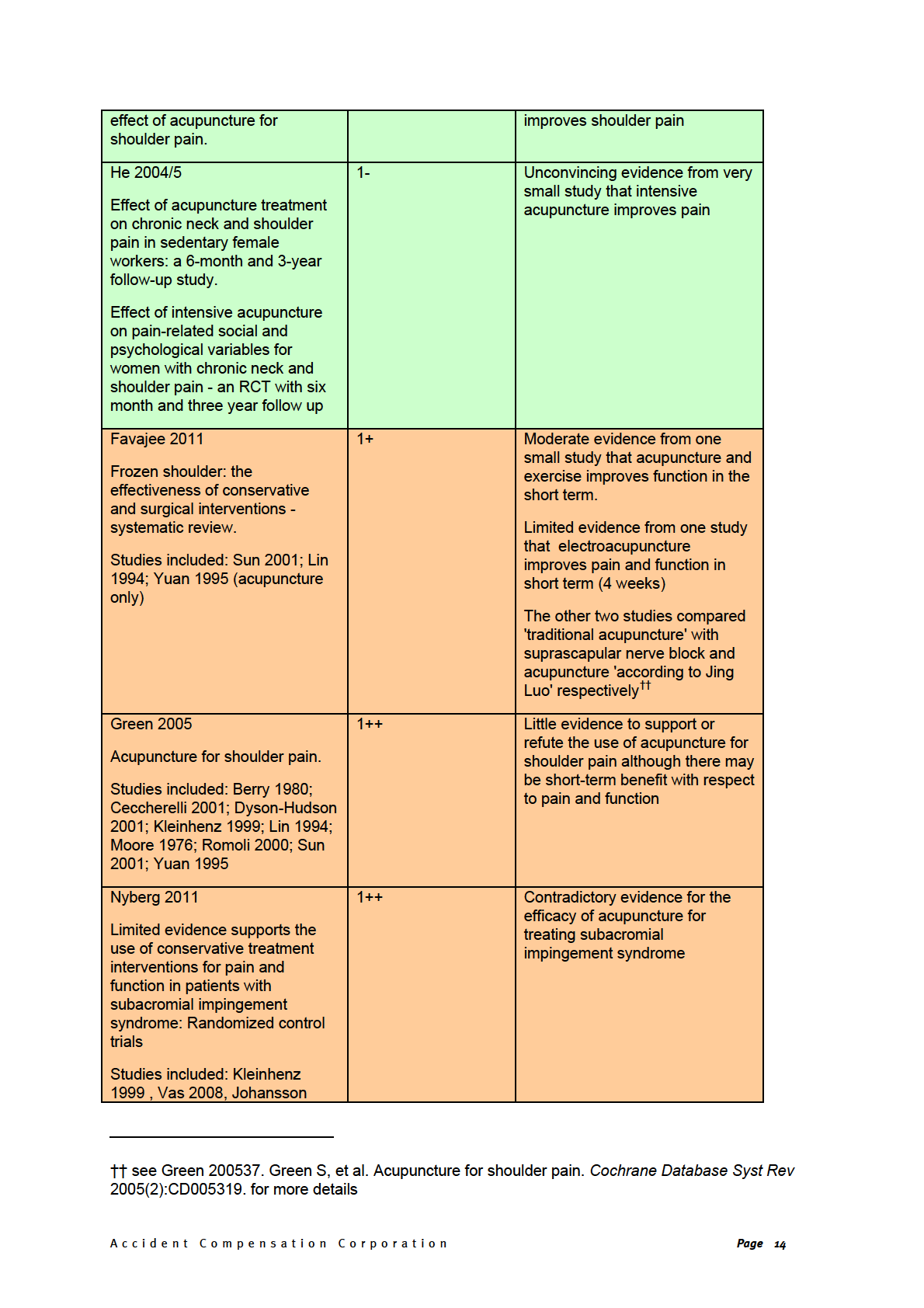
The other two studies compared 'traditional acupuncture' with suprascapular nerve block and
acupuncture 'according to Jing Luo' respectively
*6, headaches4, addictions6 emesis developing
after surgery or chemotherapy in adults The other two studies compared 'traditional acupuncture'
with suprascapular nerve block and acupuncture 'according to Jing Luo' respectively
†, nausea
associated with pregnancy6 and dental pain7; all of which fall outside the scope of this report.
Acupuncture is also used to treat a number of musculoskeletal conditions, including
shoulder6, wrist, and lower back pain4 6 7 The other two studies compared 'traditional acupuncture'
with suprascapular nerve block and acupuncture 'according to Jing Luo' respectively
‡, knee pain4 6,
neck pain, tennis/golfers elbow and ankle pain6.
Modern acupuncture includes manual stimulation of needles that are inserted into the skin.
Various adjuncts are often used including: electrical acupuncture (electrical stimulator
connected to acupuncture needle), injection acupuncture (herbal extracts injected into
acupuncture points), heat lamps, and moxibustion with acupuncture (the moxa herb,
Artemesia vulgaris, is burned at the end of a needle). Dry needling is a technique used to
treat myofascial pain in any part of the body8, by definition trigger point dry needling (TDN)
and Intramuscular manual therapy (IMT) are acupuncture techniques3. Dry needling involves
the insertion of a needle at specific trigger points, the needle being a solid acupuncture
needle or a dry injection needle.
1. Methodology
Comprehensive literature searching was carried out focused on the efficacy of acupuncture
for spine, knee, shoulder and ankle pain. The databases accessed for the search were,
Medline®, CINAHL, EMBASE, AMED, PsychINFO, PubMed and Medline-in-process and
Google. These databases will capture most, if not all, of the more robust clinical studies that
may have been reported in the TCM-specific databases. In addition, the databases used
here are used routinely in evidence-based research for complementary and alternative
medicines. Of note, the TCM-specific databases contain many case series studies and other
study designs that would be excluded from this report.
* see Green 200537. Green S, et al. Acupuncture for shoulder pain.
Cochrane Database Syst Rev 2005(2):CD005319. for more details
† see Green 200537. Green S, et al. Acupuncture for shoulder pain.
Cochrane Database Syst Rev 2005(2):CD005319. for more details
‡ see Green 200537. Green S, et al. Acupuncture for shoulder pain.
Cochrane Database Syst Rev 2005(2):CD005319. for more details
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page 4
The search was run on the 31st July 2011 for the period 2000 to present. Manual searching
of reference lists was also carried out. A pragmatic approach was taken initially searching
for randomised controlled trials (RCTs), systematic reviews and meta-analyses, as the
highest levels of evidence. RCT’s are also the trial design of choice when investigating
treatment efficacy.
The literature was critically appraised using SIGN9 (see below) grading system for systematic
reviews and RCTs.
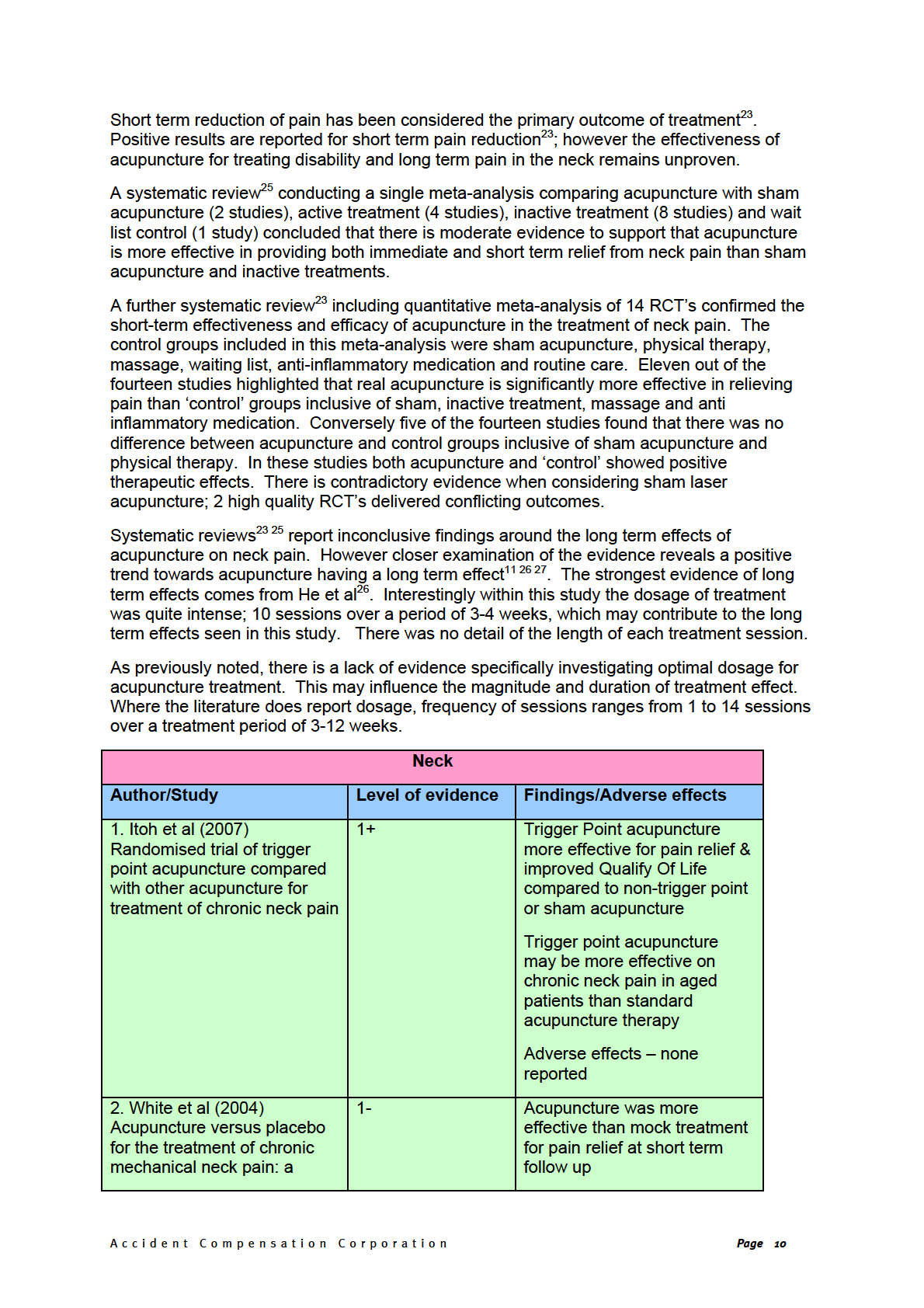
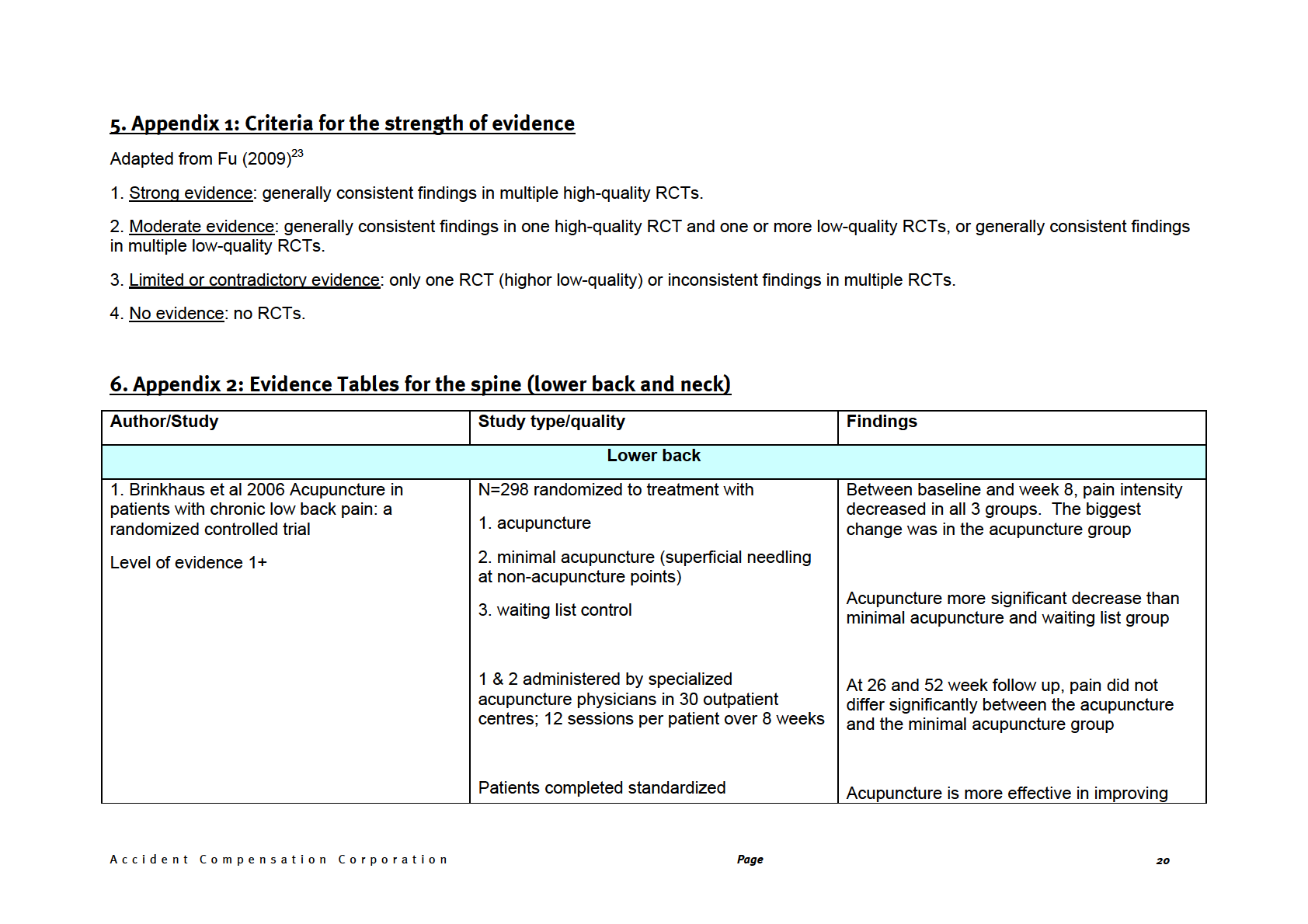
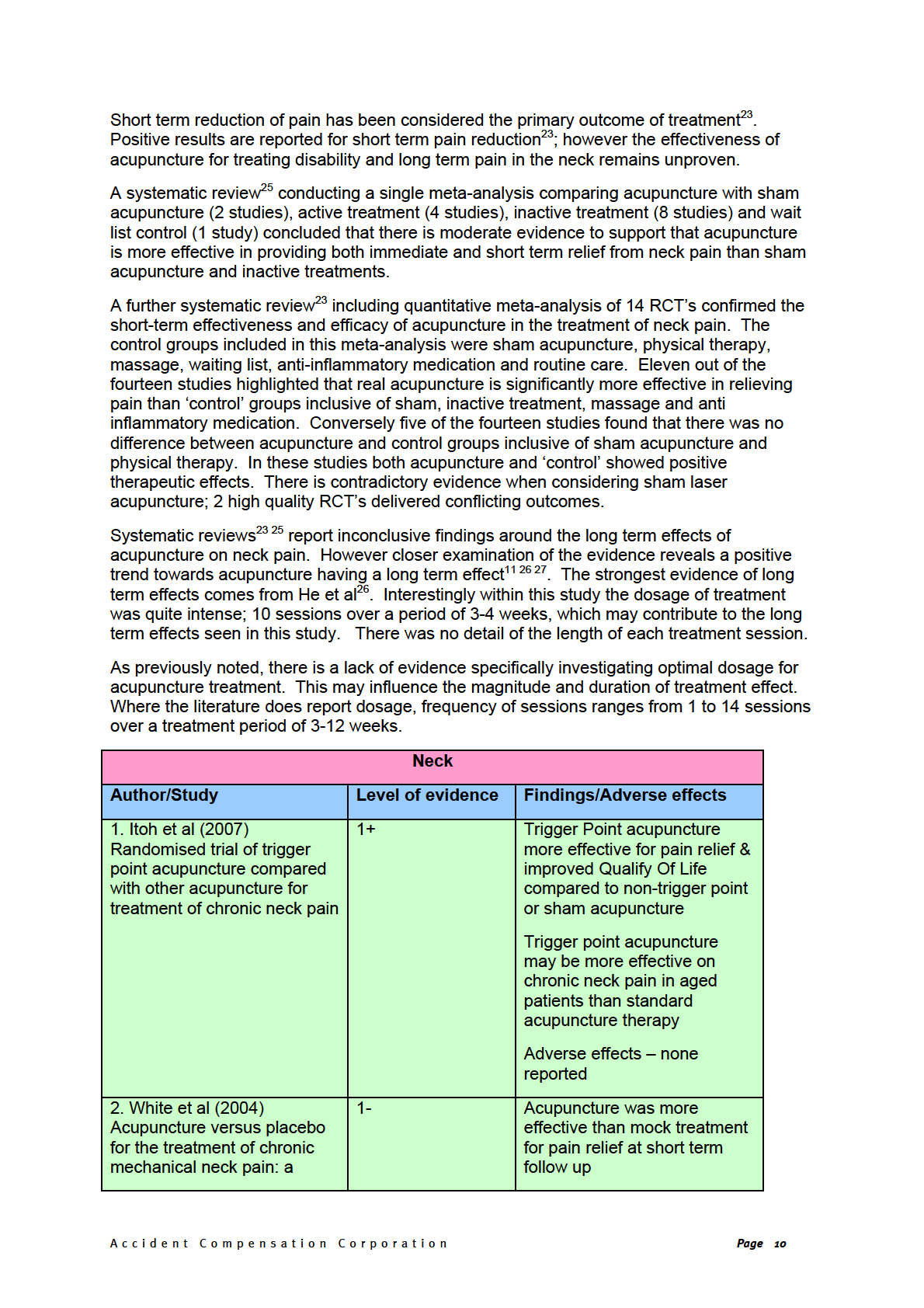
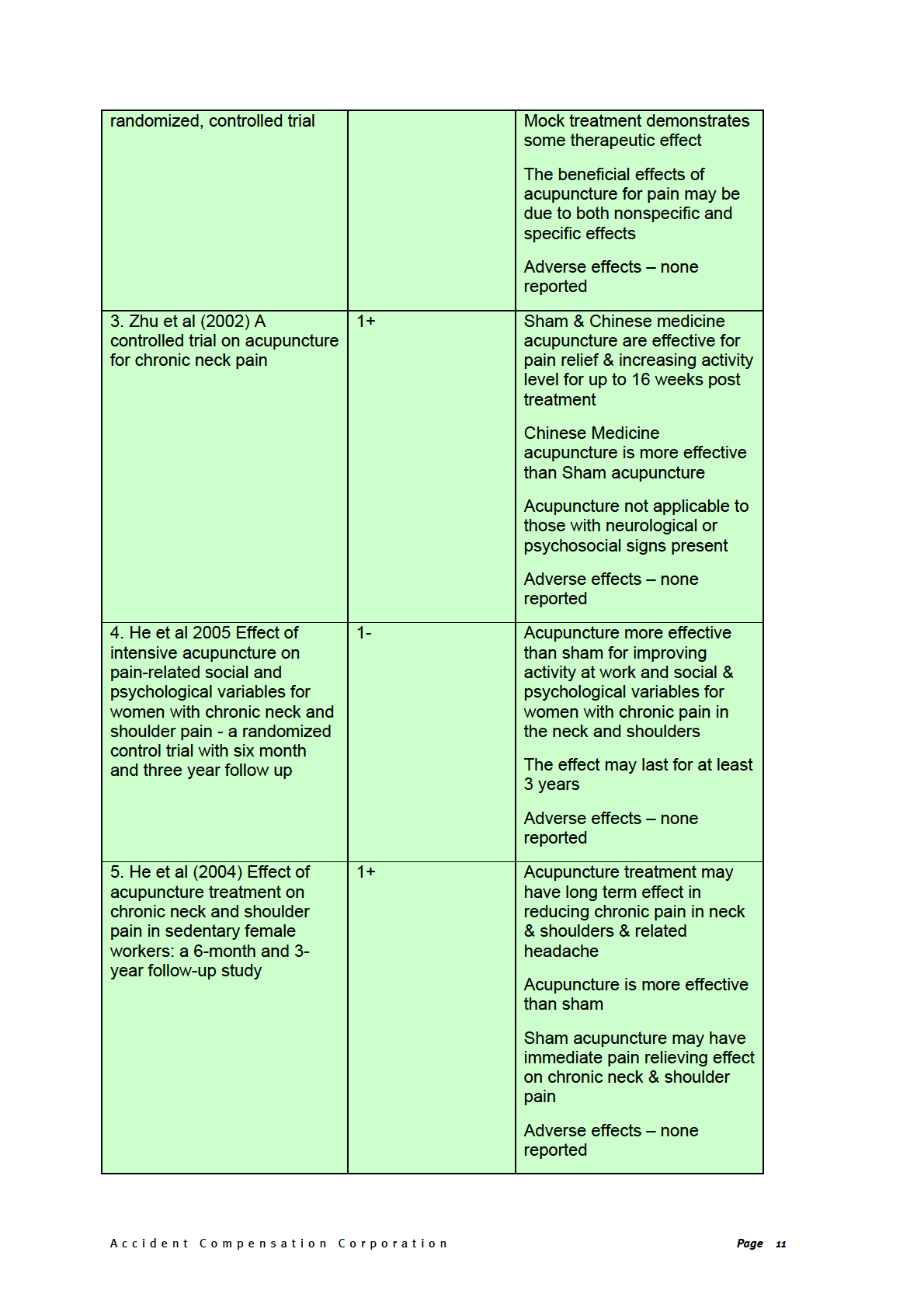
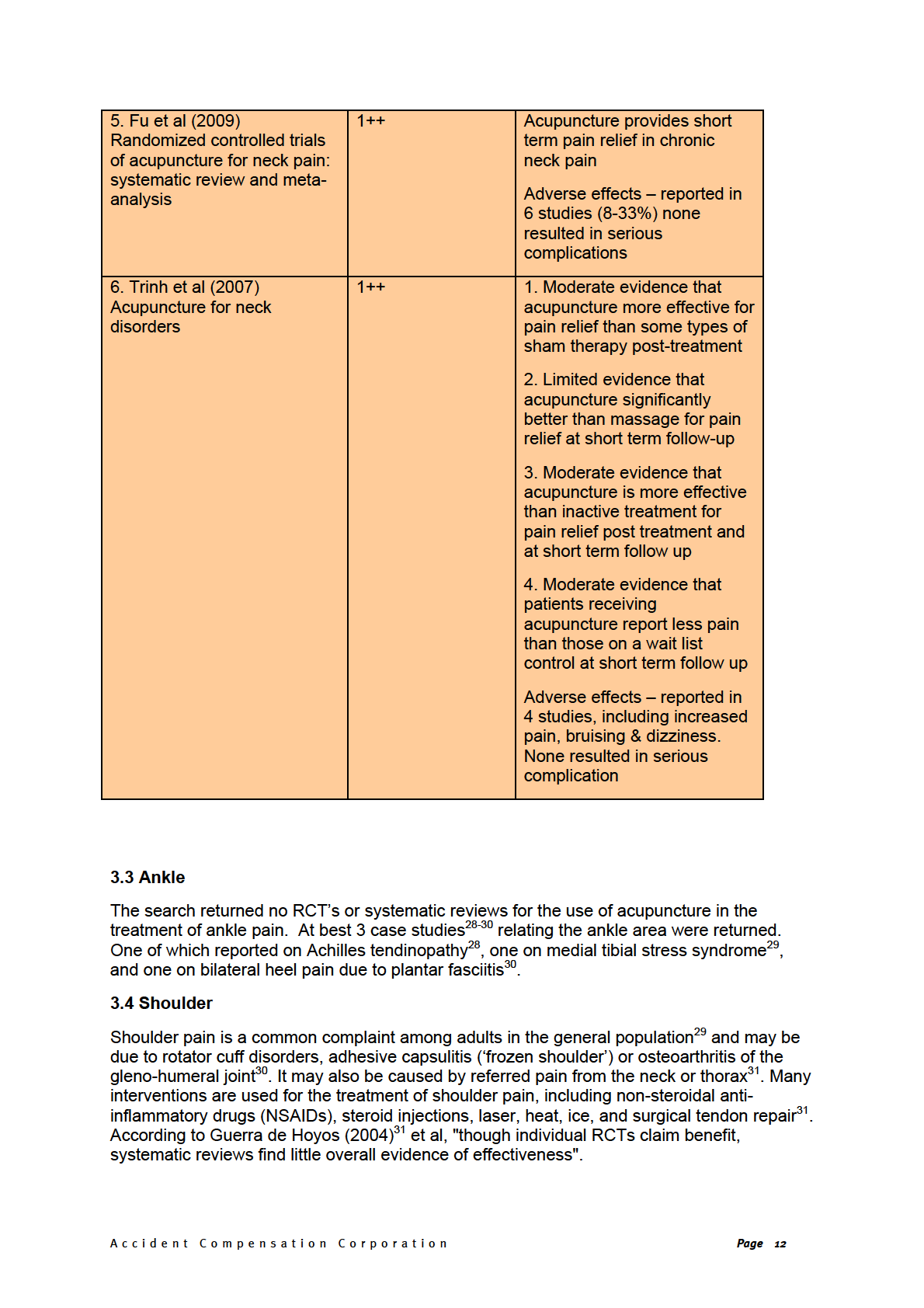
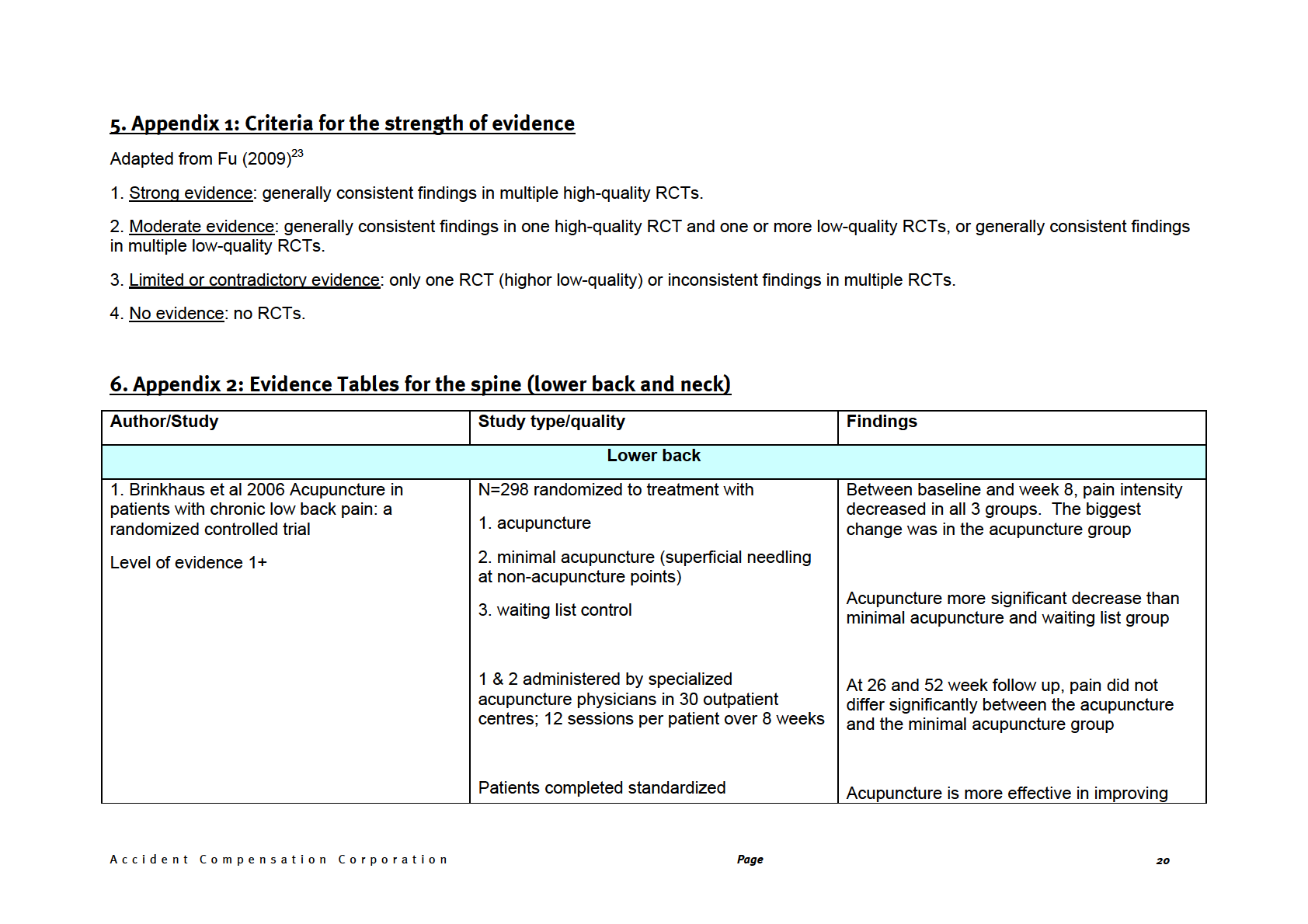
SIGN – LEVELS OF EVIDENCE
1++ High quality meta-analyses, systematic reviews of RCTs, or RCTs with a very low
risk of bias
1+ Well-conducted meta-analyses, systematic reviews, or RCTs with a low risk of bias
1-
Meta-analyses, systematic reviews, or RCTs with a high risk of bias
2++ High quality systematic reviews of case control or cohort or studies
High quality case control or cohort studies with a very low risk of confounding or
bias and a high probability that the relationship is causal
2+ Well-conducted case control or cohort studies with a low risk of confounding or
bias and a moderate probability that the relationship is causal
2-
Case control or cohort studies with a high risk of confounding or bias and a
significant risk that the relationship is not causal
3
Non-analytic studies, e.g. case reports, case series
4 Expert
opinion
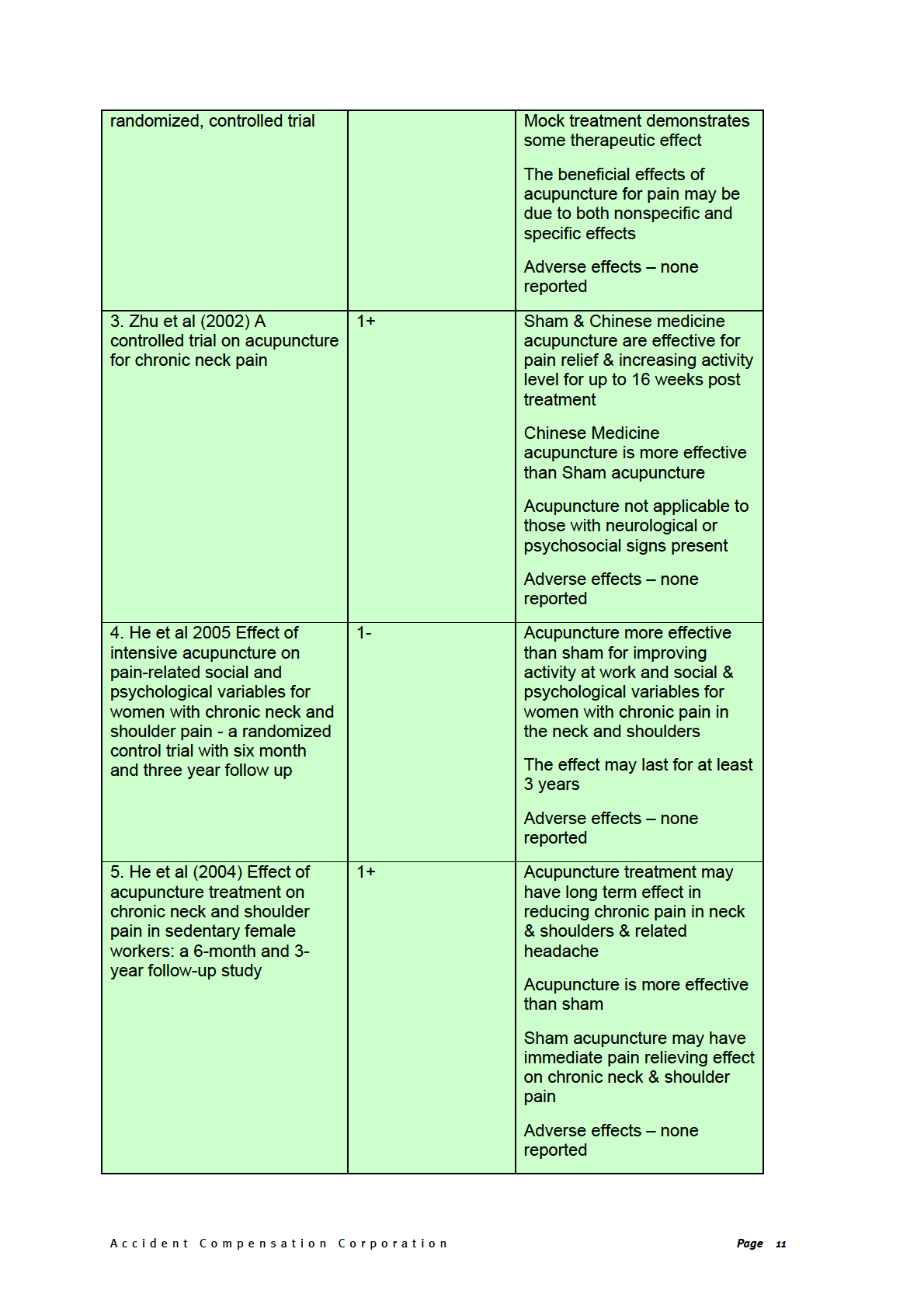
3. Review of the Literature
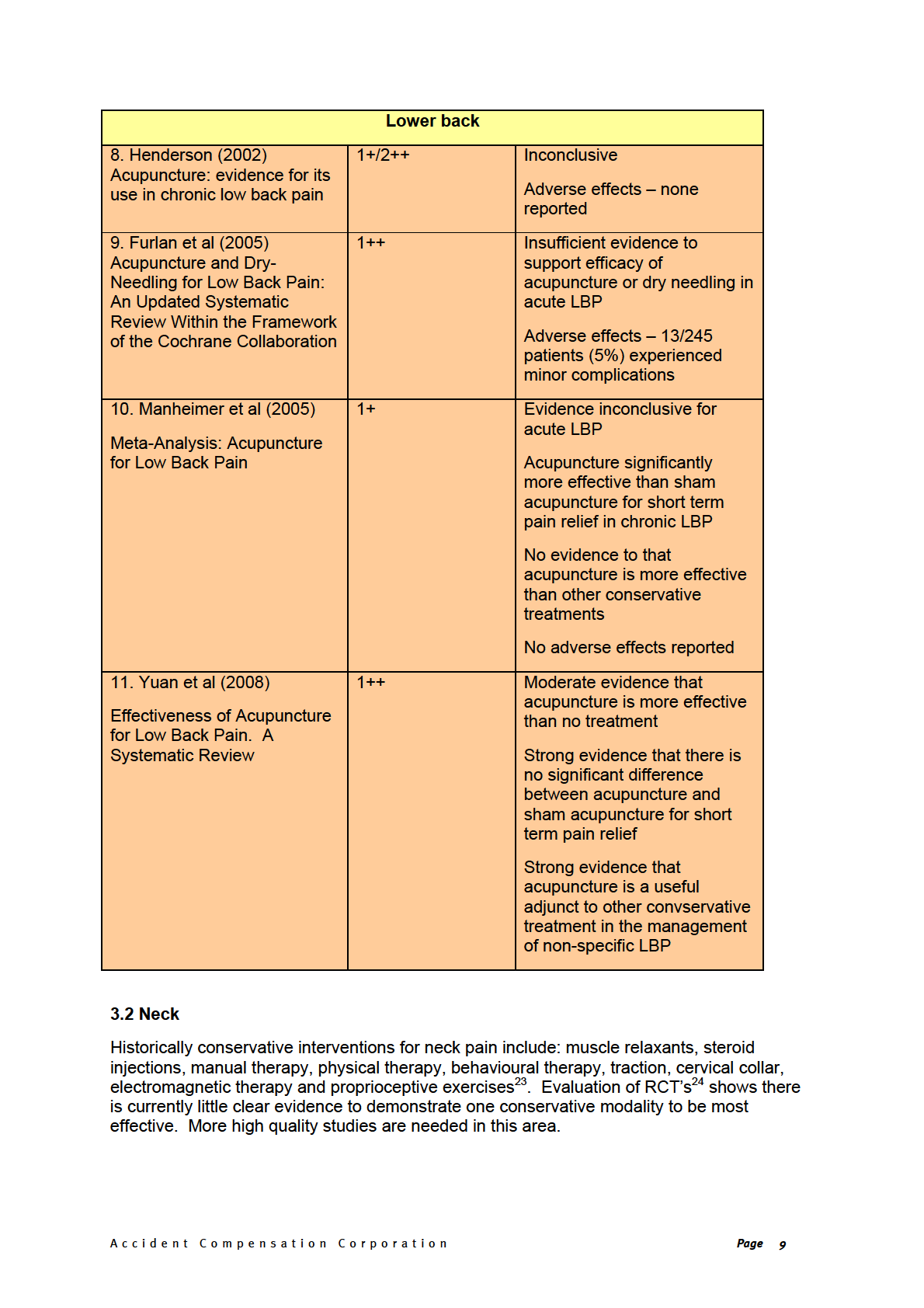
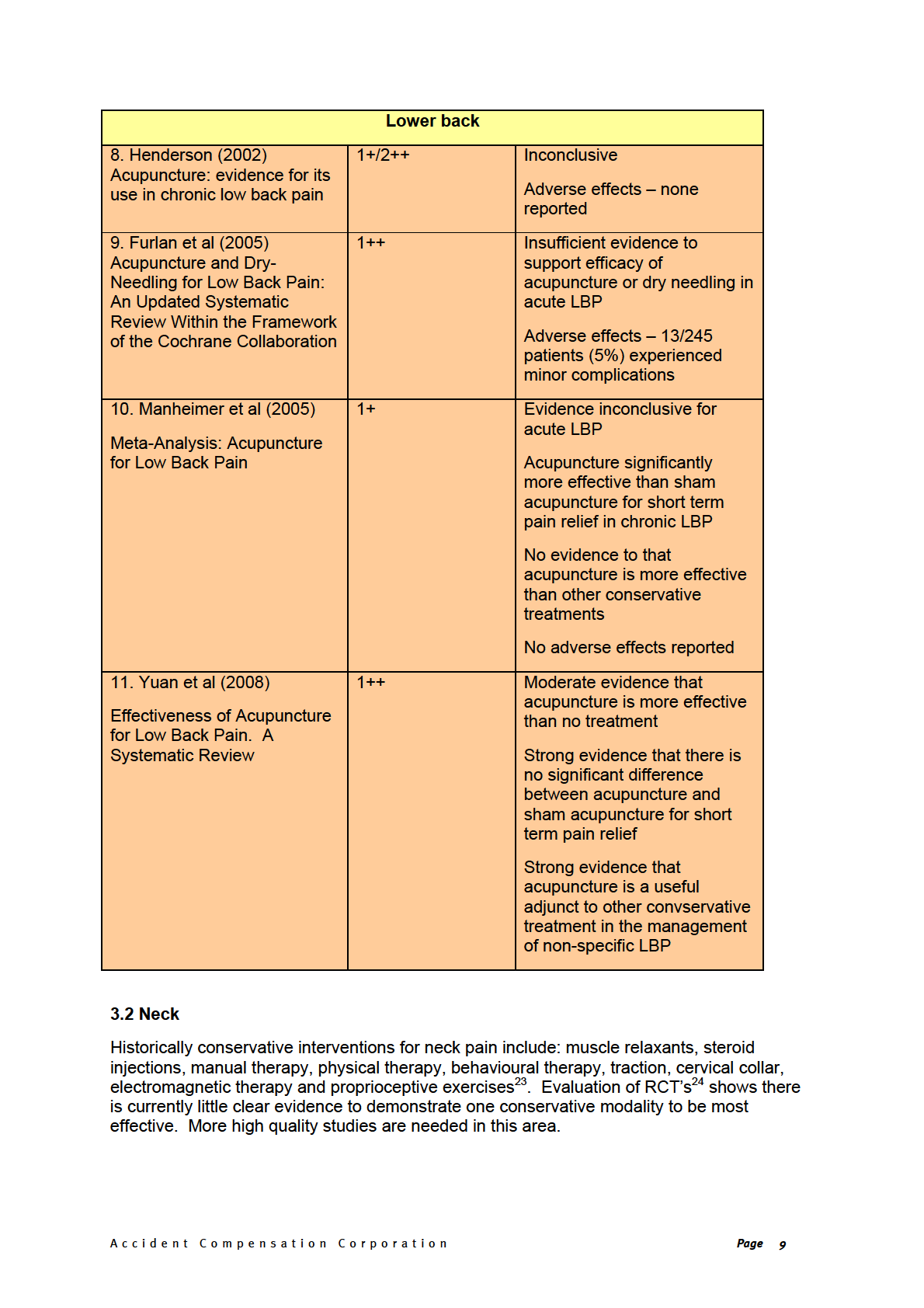
Neck pain and lower back pain (LBP) are two conditions that can be problematic to treat.
Studies examining effective conservative treatments for (sub)acute and chronic non-specific
low back pain have been largely inconclusive. This is also true of neck and thoracic spine
pain.
A lot of the literature focuses on chronic spinal pain; there are no high quality trials for the
treatment of acute spinal pain.
There is limited evidence to suggest that acupuncture is not an appropriate treatment for any
spinal condition with suspected neurological involvement10 11.
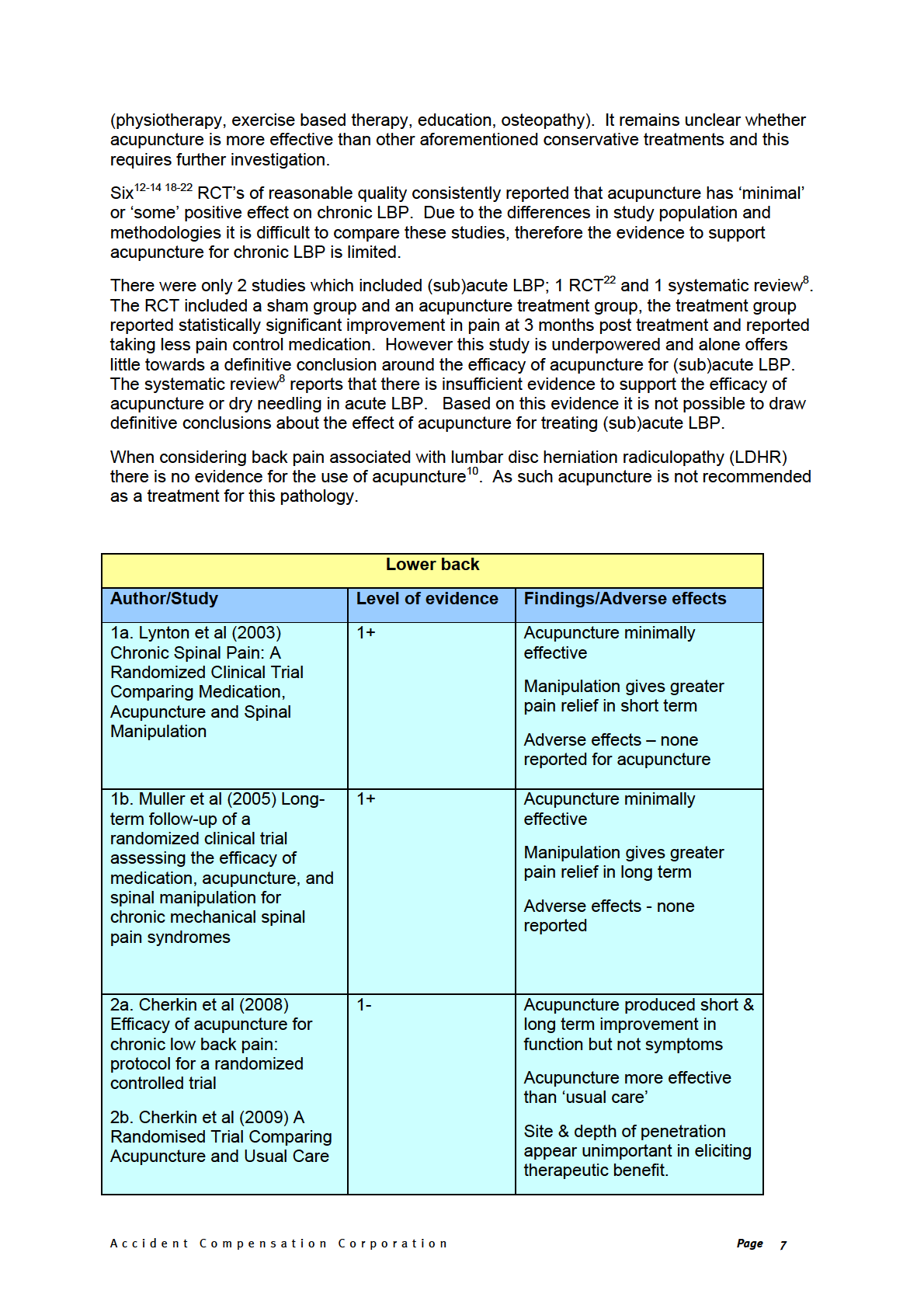
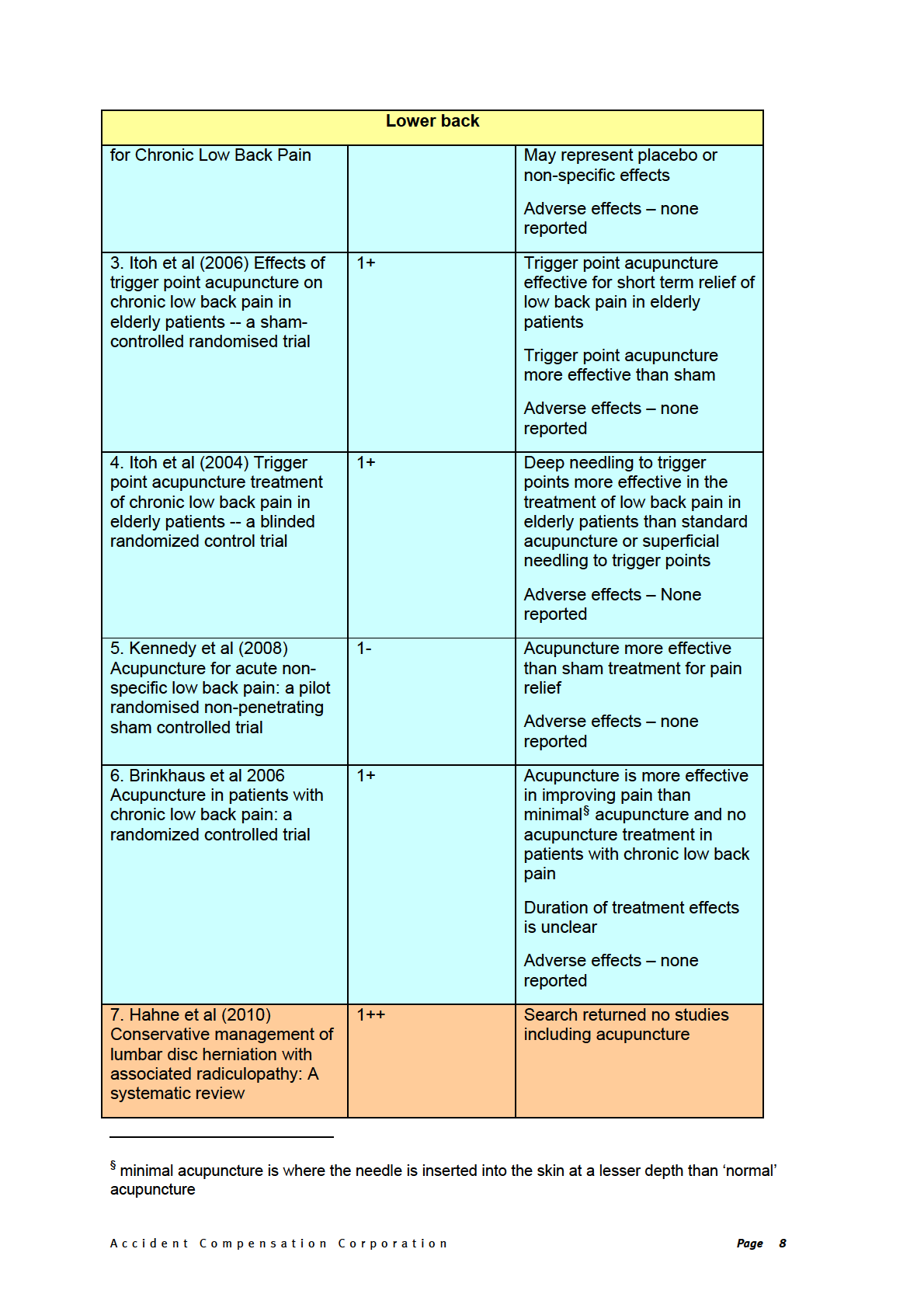
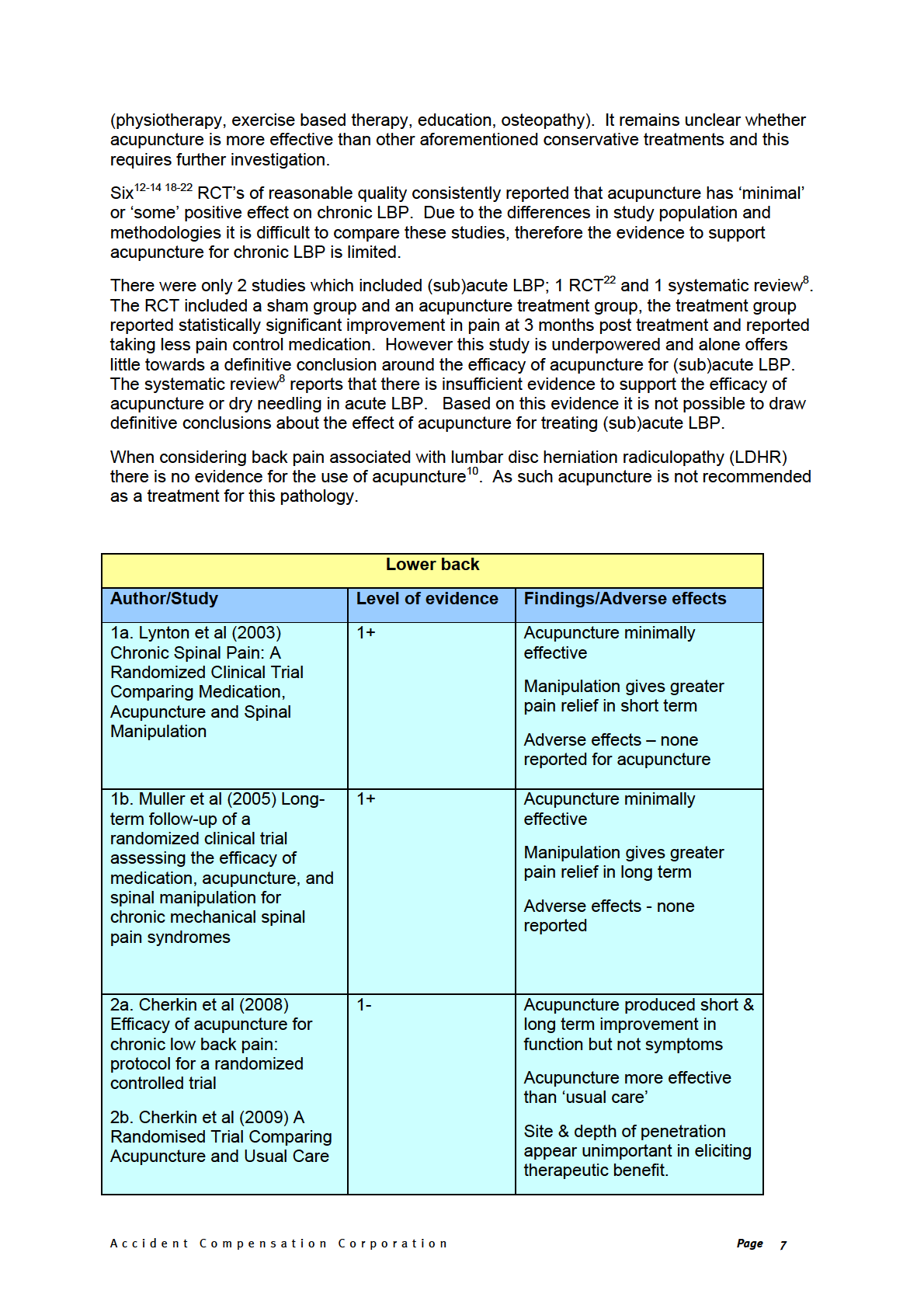
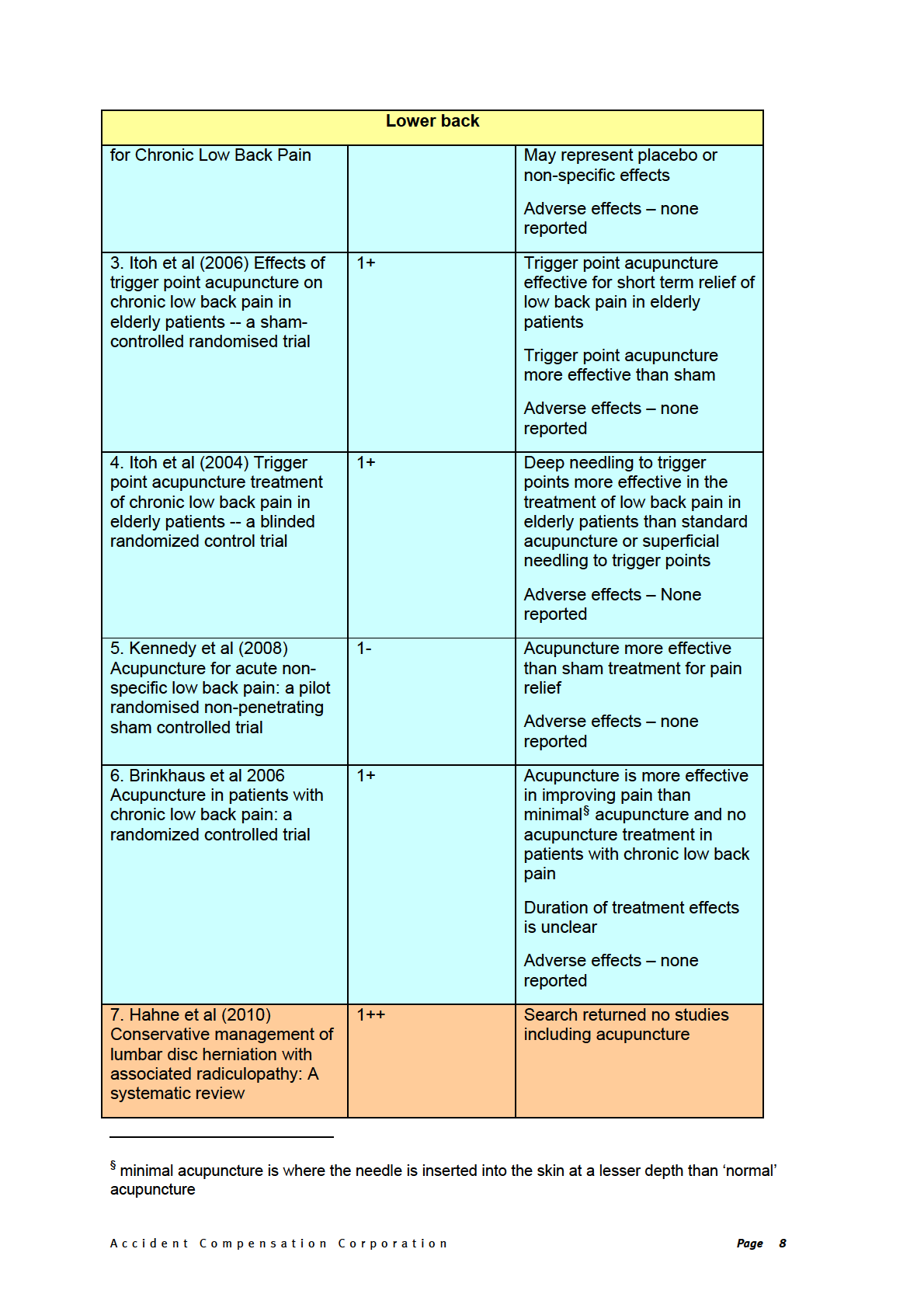
3.1 Lower Back Pain
Chronic spinal pain presents a diagnostic and treatment challenge ,reaching a specific
diagnosis is often difficult. Effective conservative treatments for (sub)acute and chronic non-
specific LBP have been largely inconclusive12. Differing patient populations and
methodologies make direct comparison of studies problematic often resulting in inconclusive
findings.
Studies comparing spinal manipulation, medication, and acupuncture for chronic spinal pain
revealed that spinal manipulation produced the greatest benefit both in the short13 and long
term 12; within these studies acupuncture produced ‘consistent’ improvement in outcomes
although this did not reach statistical significance. Outcome measures addressed both pain
and function (Oswestrey scale, Visual Analogue Scale (VAS), lumbar flexion in sitting and
standing); overall recovery was 27% of the patients receiving spinal manipulation, 9.4% of
those receiving acupuncture and only 5% of those receiving medication. It is noteworthy
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page 5
here that spinal manipulation is not appropriate for all LBP patients and a range of
conservative treatment options must always be considered. In this study it was not possible
to blind the patient and the therapist to the treatment allocation due to the ‘hands on’ nature
of manipulation and acupuncture, therefore the placebo effect cannot be discounted.
In a study14 comparing 3 different acupuncture approaches (individualised, standardised &
sham) to standard care (inclusive of medications, primary care and physical therapy, non-
study related), all groups treated with acupuncture demonstrated greater improvement in
dysfunction than standard care14. The acupuncture groups included in this study all used
different needle locations and depths, which suggests that this is unimportant in eliciting a
therapeutic effect and may in-fact represent a placebo or non-specific effect. This was the
only study reporting on function; the literature more frequently reports pain relieving effects.
Itoh et al15 reported that a study group receiving trigger point acupuncture recorded
significantly less pain (VAS) than a sham control group. This finding remained true when the
groups were crossed over following a 3 week washout period. As acknowledged by the
authors, the 3 week washout may have been insufficient and therefore a carry over treatment
effect could not be discounted. This study does however support the notion that both sham
and real acupuncture exert positive therapeutic effects on chronic LBP and that real
acupuncture is more effective than sham.
A systematic review of acupuncture for chronic LBP16 returned only 5 RCT’s. A meta-
analysis was not performed due to the wide disparities in design, groups, needling points,
control groups and how & when pain relief outcomes were measured in these studies. The
trials were examined individually, and did not provide definitive evidence to support or refute
acupuncture as an effective treatment for chronic LBP. Closer examination of the articles
included in the review reveals that the results of the RCT’s show a trend towards study
groups receiving some form of acupuncture intervention show improvement/positive
treatment effects. However in agreement with the review author there are some
methodological issues within the studies that prevent the drawing of definitive conclusions. A
systematic review8 concluded that in chronic LBP acupuncture is more effective than no
treatment or sham treatment at up to 3 month follow up. It was also reported that
acupuncture as an adjunct to conventional therapies is more effective than conventional
therapies alone. Dry needling is also considered in this review and reported as a useful
adjunct to other therapies for chronic LBP.
A larger systematic review 1 inclusive of both acute and chronic LBP focused on the primary
outcome of short term pain relief reports that acupuncture is described as statistically
significantly and clinically important and is more effective than sham acupuncture and
concludes that acupuncture effectively relieves chronic LBP. It is noteworthy that of the 33
RCTs included in the review only 22 could be included in the meta-analysis due to the
heterogeneity across the study samples and methodologies in the remaining 11 RCTs, 4 of
which were related to chronic LBP. The quality of the studies included in the meta-analysis
is variable, as such the findings from this review should only be considered as somewhat
preliminary. Future publication of larger trials would have an impact on the evidence overall.
A more recent systematic review17 inclusive of 6 RCTs not published when previous reviews1
8 were carried out reported that there is moderate evidence that acupuncture is more
effective than no treatment and strong evidence of no significant difference between
acupuncture and sham acupuncture for short term pain relief for chronic LBP.
Considering 3 systematic reviews1 8 17 of reasonable quality the evidence shows a trend
towards acupuncture being more effective than no treatment, however the evidence remains
limited. There are inconsistent findings for acupuncture versus sham acupuncture. There is
consistent evidence that acupuncture is a useful adjunct to other conservative treatments
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page 6

4. Hopton A, MacPherson, H.,. Acupuncture for chronic pain: Is acupuncture more than
an effective placebo? A systematic review of pooled data from meta-analyses.
Pain
Practice 2010;10(2):94-102.
5. Ernst E, Lee, M.S., Choi, T.Y., . Acupuncture: Does it alleviate pain and are there serious
risks? A review of reviews.
Pain 2011;152:755-64.
6. Harland S, Bleakley, C., McDonough, S. M.,. Acupuncture in soft tissue injury
management: a systematic review... Rehabilitation and Therapy Research Society
Third Annual Conference: Collaborative research... making it a reality, held on 26-
27 April 2007 at University of Ulster.
Physical Therapy Reviews 2008;13(2):121-22.
7. Kaptchuk TJ. Acupuncture: theory, efficacy, and practice.
Annals Of Internal Medicine
2002;136(5):374-83.
8. Furlan AD, van-Tulder, M., Cherkin, D., . Acupuncture and Dry-Needling for Low Back
Pain: An Updated Systematic Review Within the Framework of the Cochrane
Collaboration.
Spine 2005;2005(8):944-63.
9. Scottish Intercollegiate Guidelines Network. SIGN 50: Guideline Development.
10. Hahne AJ, Ford, J. J., McMeeken, J. M., . Conservative management of lumbar disc
herniation with associated radiculopathy: A systematic review.
Spine 2010;35(11):488-504.
11. Zhu XM, Polus, B.,. A controlled trial on acupuncture for chronic neck pain.
American
Journal of Chinese Medicine 2002;30(1):13-28.
12. Muller R, Giles, L. G. F.,. Long-term follow-up of a randomized clinical trial assessing
the efficacy of medication, acupuncture, and spinal manipulation for chronic
mechanical spinal pain syndromes.
Journal of Manipulative & Physiological
Therapeutics 2005;28(1):3-11.
13. Lynton GF, Giles, D.C., Muller, R.,. Chronic Spinal Pain:
A Randomized Clinical Trial
Comparing Medication, Acupuncture and Spinal Manipulation.
Spine 2003;28(14):1490-503.
14. Cherkin DC, Sherman, K.J., Avins, A.L., Erro, J.H., Ichikawa, L., Barlow, W.E.,
Delaney, K., Hawkes, R., Hamilton, L., Pressman, A., Khalsa, P.S., Deyo, R.A., . A
Randomised Trial Comparing Acupuncture and Usual Care for Chronic Low Back
Pain.
Archives of Internal Medicine 2009;169(9):838-66.
15. Itoh K, Katsumi, Y., Hirota, S., Kitakoji, H. Effects of trigger point acupuncture on
chronic low back pain in elderly patients -- a sham-controlled randomised trial.
Acupuncture in Medicine 2006;24(1):5-12.
16. Henderson H. Acupuncture: evidence for its use in chronic low back pain.
British
Journal of Nursing (BJN) 2002;11(21):1395-403.
17. Yuan J, Purepong, N., Kerr, D.P., Park, J., Bradbury, I., McDonough, S., . Effectiveness
of Acupuncture for Low Back Pain: A systematic review.
Spine 2008;33(23):E887-
900.
18. Brinkhaus B. WCM, Jena S., Linde K.,. Acupuncture in patients with chronic low back pain: a
randomized controlled trial. .
Archives of Internal Medicine 2006;166(4):450-57.
19. Cherkin DC, Sherman, K. J., Hogeboom, C. J., Erro, J. H., Barlow, W. E., Deyo, R. A.,
Avins, A. L.,. Efficacy of acupuncture for chronic low back pain: protocol for a
randomized controlled trial.
Trials 2008;9:10-10.
20. Itoh K, Katsumi, Y., Kitakoji, H. Trigger point acupuncture treatment of chronic low
back pain in elderly patients -- a blinded RCT.
Acupuncture in Medicine
2004;22(4):170-77.
21. Itoh K, Katsumi, Y., Hirota, S., Kitakoji, H. Randomised trial of trigger point
acupuncture compared with other acupuncture for treatment of chronic neck pain.
Complementary Therapies in Medicine 2007;15(3):172-79.
22. Kennedy S, Baxter, G. D., Kerr, D. P., Bradbury, I., Park, J., McDonough, S. M.
Acupuncture for acute non-specific low back pain: a pilot randomised non-
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page 16
penetrating sham controlled trial.
Complementary Therapies in Medicine
2008;16(3):139-46.
23. Fu L, Li, J., Wu, W.,. Randomized controlled trials of acupuncture for neck pain:
systematic review and meta-analysis.
Journal of Alternative & Complementary
Medicine 2009;15(2):133-45.
24. van Tulder MW, Goosens, M., Hoving, J., . Non-surgical treatment of chronic neck
pain In: Nachemson A, Jonsson, E., , editor.
Neck and Back pain. Philadelphia:
Lippincott, Williams and Wilkins, 2000.
25. Trinh K, Graham, N., Gross, A., Goldsmith, C., Wang, E., Cameron, I., Kay, T., .
Acupuncture for Neck Disorders.
Spine 2007;32(2):236-43.
26. He D, Hostmark, At., Veiersted, Kb., Medbo, Ji.,. Effect of intensive acupuncture on
pain-related social and psychological variables for women with chronic neck and
shoulder pain - an RCT with six month and three year follow up.
Acupuncture in
Medicine 2005;23(2):52-61.
27. White P, Lewith, G., Prescott, P., Conway, J.,. Acupuncture versus placebo for the
treatment of chronic mechanical neck pain: a randomized, controlled trial.
Annals
of Internal Medicine 2004;141(12):911-19.
28. Grainger R. Physiotherapy and acupuncture treatment for Achilles tendinopathy in a
high-level female rugby player.
Journal of the Acupuncture Association of Chartered
Physiotherapists 2009:67-76.
29. Knight RR. Integration of manual therapy, rehabilitation and acupuncture in the
treatment of a 17-year-old male professional football player with chronic medial
tibial stress syndrome.
Journal of the Acupuncture Association of Chartered
Physiotherapists:81-87.
30. Santha CC. Acupuncture treatment for bilateral heel pain caused by plantar fascitis.
Journal of the Acupuncture Association of Chartered Physiotherapists:67-74.
31. Green S, Buchbinder, R., Hetrick, S. E.,. Acupuncture for shoulder pain.
Cochrane
Database of Systematic Reviews 2005(2).
32. Molsberger AF, Schneider T, Gotthardt H, Drabik A. German Randomized
Acupuncture Trial for chronic shoulder pain (GRASP) - A pragmatic, controlled,
patient-blinded, multi-centre trial in an outpatient care environment.
Pain 2010;151(1):146-54.
33. Guerra de Hoyos JA, Andres Martin Mdel C, Bassas y Baena de Leon E, Vigara Lopez
M, Molina Lopez T, Verdugo Morilla FA, et al. Randomised trial of long term effect
of acupuncture for shoulder pain.
Pain 2004;112(3):289-98.
34. He D, Veiersted, Kb., Hostmark, At., Medbo, Ji.,. Effect of acupuncture treatment on
chronic neck and shoulder pain in sedentary female workers: a 6-month and 3-year
follow-up study.
Pain 2004;109(3):299-307.
35. Lathia AT, Jung, S. M., Chen, L. X.,. Efficacy of acupuncture as a treatment for chronic
shoulder pain.
Journal of Alternative & Complementary Medicine 2009;15(6):613-18.
36. Favejee MM, Huisstede BM, Koes BW, Huisstede BMA. Frozen shoulder: the
effectiveness of conservative and surgical interventions--systematic review.
BJSM
online 2011;45(1):49-56.
37. Nyberg A, Jonsson P, Sundelin G. Limited scientific evidence supports the use of
conservative treatment interventions for pain and function in patients with
subacromial impingement syndrome: Randomized control trials.
Physical
2010;15(6):436-52.
38. Johansson K, Bergstrom A, Schroder K, Foldevi M, Johansson K, Bergstrom A, et al.
Subacromial corticosteroid injection or acupuncture with home exercises when
treating patients with subacromial impingement in primary care--a randomized
clinical trial.
Fam Pract 2011;28(4):355-65.
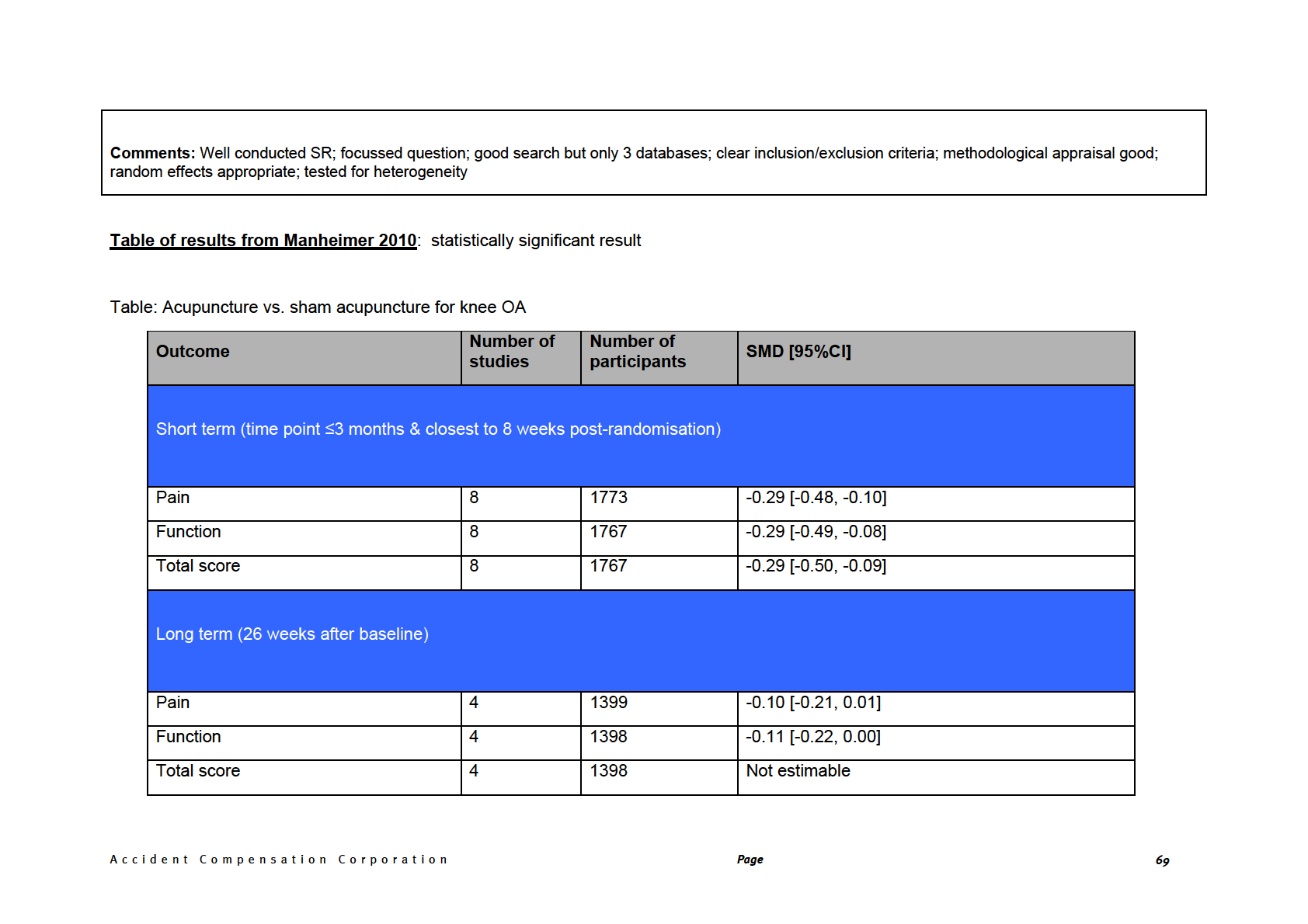
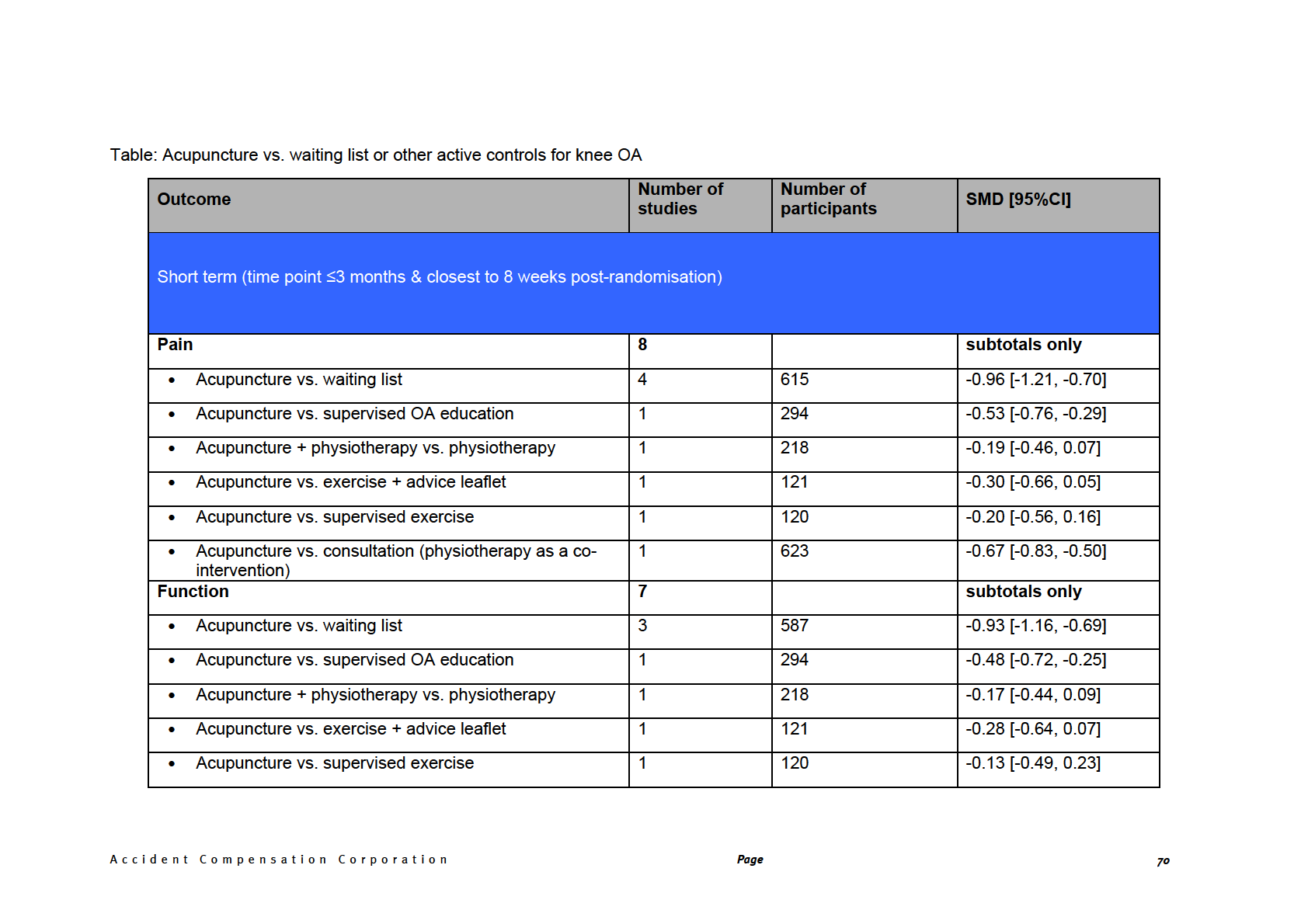
39. Manheimer E, Cheng K, Linde K, Lao L, Yoo J, Wieland S, et al. Acupuncture for
peripheral joint osteoarthritis.
Cochrane Database Syst Rev 2010(1):CD001977.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page 17
40. Kelly RB, Kelly RB. Acupuncture for pain.
Am Fam Physician 2009;80(5):481-4.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page 18
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page 19
questionnaires at baseline, 8, 26, and 52
pain than no acupuncture treatment in
weeks after randomization.
patients with chronic low back pain
There was no significant differences between
acupuncture and minimal acupuncture
Primary outcome variable was the change in
low back pain (VAS) intensity from baseline to
the end of week 8
2a. Lynton et al (2003) Chronic Spinal Pain:
A 3 armed RCT (includes full spine)
Earliest asymptomatic status:
Randomized Clinical Trial Comparing
Medication, Acupuncture and Spinal
1- medication
Manipulation (27%)
Manipulation
2–needle acupuncture
Acupuncture (9.4%)
Level of evidence 1+
3-spinal manipulation (chiropractic)
Medication (5%)
N=115
Outcome measures at 0,2,5,9 weeks
Best overall results from outcomes were for
treatment
manipulation
Patients with chronic spinal pain results in
greatest short term improvement. Data are
not strong
2b. Muller et al (2005) Long-term follow-up of
Extended follow-up (>1 year) of RCT
Comparisons of initial and extended follow-up
a randomized clinical trial assessing the
questionnaires to assess absolute efficacy
efficacy of medication, acupuncture, and
N=62/69
showed that only the application of spinal
spinal manipulation for chronic mechanical
N=40/62 patients who had received
manipulation revealed broad-based long-term
spinal pain syndromes
exclusively the randomly allocated treatment
benefit
Level of evidence 1+
for the whole observation period since
randomization
In patients with chronic spinal pain
syndromes, spinal manipulation, if not
contraindicated, may be the only treatment
modality of the assessed regimens that
provides broad and significant long-term
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
21
benefit
3a. Cherkin et al (2008) Efficacy of
4 arm RCT, n=640
Protocol detail only
acupuncture for chronic low back pain:
protocol for a randomized controlled trial
3b. Cherkin et al (2009) A Randomised Trial
4 arm RCT, n=638
At 8 weeks grps 1,2,3 improvement in function
Comparing Acupuncture and Usual Care for
Chronic Low Back Pain
1-Individualised acupuncture
At 1 year follow up grps 1,2,3 improved
function but not symptoms
Level of evidence 1-
2-Standardised acupuncture
3-Simulated acupuncture
Site and depth of penetration appear
4-Usual care
unimportant in eliciting therapeutic benefit.
Outcome measures at 0,8,26,52 weeks post
Raises question about physiological effect,
treatment onset
may represent placebo or non-specific effects
4. Hahne et al (2010) Conservative
Systematic review of randomized controlled
Search returned no studies including
management of lumbar disc herniation with
trials for specific diagnosis of LDHR
acupuncture
associated radiculopathy: A systematic review radiologically confirmed
Level of evidence 1++
5. Henderson (2002) Acupuncture: evidence
Systematic review on Western countries (11
No conclusive evidence to support or refute
for its use in chronic low back pain
articles; 3 case studies, 5 randomized
the use of acupuncture in Low back pain
controlled trials & 2 cross-over trials)
Level of evidence 1+/2++
Increasing number of patients suffering from
back pain seeking complementary therapies
to supplement traditional medical treatments
6. Itoh et al (2006) Effects of trigger point
RCT
At the end of the first treatment phase,
acupuncture on chronic low back pain in
elderly patients -- a sham-controlled
N=26 randomised to two groups
randomised trial
Each group received one phase of trigger
Group A receiving trigger point acupuncture
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
22
Level of evidence 1+
point acupuncture and one of sham
had significantly less pain than the sham
acupuncture with a three week washout
control group
period between them, over 12 weeks
Group A (n = 13) trigger point acupuncture in
first phase & sham acupuncture in the second There were significant within-group reductions
in pain in both groups during the trigger point
acupuncture phase but not in the sham
treatment phase
Group B (n = 13) received the same
interventions in the reverse order
Beneficial effects were not sustained
These results suggest that trigger point
acupuncture may have greater short term
effects on low back pain in elderly patients
than sham acupuncture
7. Itoh et al (2004) Trigger point acupuncture
Double blind crossover RCT
Deep resulted in less pain intensity and
treatment of chronic low back pain in elderly
improved QoL compared to standard
patients -- a blinded RCT
N=35 were randomised to 1 of 3 groups over
acupuncture or superficial needling to trigger
12 weeks
points
Level of evidence 1+
Each group received 2 phases of acupuncture
treatment with an interval between them
Reduction in pain intensity between the
1. Standard acupuncture group received
treatment & interval in the group that received
treatment at traditional acupuncture points for
deep needling (not the case in standard
low back pain
acupuncture or superficial needling to trigger
points
2. Superficial treatment on trigger points
Deep needling to trigger points may be more
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
23
effective in the treatment of low back pain in
elderly patients than standard acupuncture or
3. Deep treatment on trigger points
superficial needling to trigger points
8. Kennedy et al (2008) Acupuncture for acute A pilot patient and assessor blinded
For pain, the only statistically significant
non-specific low back pain: a pilot randomised randomized controlled trial
difference was at the 3 months follow up
non-penetrating sham controlled trial
N=48, 12 weeks treatment.
Level of evidence 1-
1. Placebo group with sham needle
At the end of treatment; verum acupuncture
group were taking significantly fewer tablets of
2. Verum acupuncture
pain control medication
Outcome measures at baseline, end of
treatment & 3 months follow up
This study has demonstrated 120 participants
would be required in a fully powered trial.
The placebo needle used in this study proved
to be a credible form of control
9. Furlan et al (2005) Acupuncture and Dry-
Systematic review of RCTs (1996-2003)
Insufficient evidence to support efficacy of
Needling for Low Back Pain: An Updated
acupuncture or dry needling in acute LBP
Systematic Review Within the Framework of
Acupuncture for (sub) acute & chronic non-
the Cochrane Collaboration
specific LBP
Level of evidence 1++
Dry needling for myofascial trigger points,
For chronic LBP Acupuncture more effective
compared to;
than no treatment or sham treatment up to 3
months.
- No treatment
For chronic LBP acupuncture is more effective
- Sham therapy
than no treatment for improving function in the
- Other therapy
short term
- Addition of acupuncture to other therapy
As an adjunct to other conventional therapies
acupuncture relieves pain and improves
function better than conventional therapies
alone
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
24
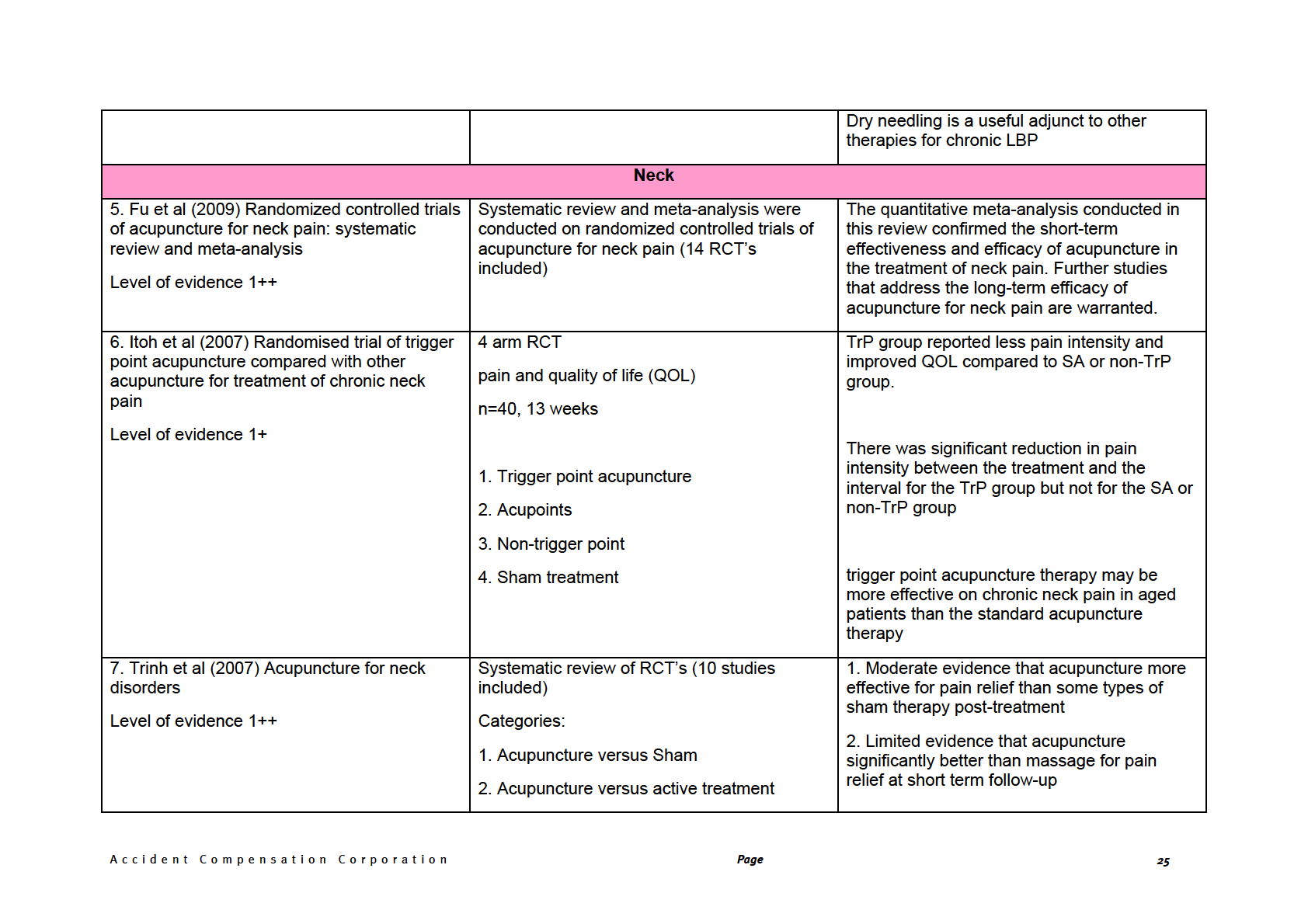
3. Acupuncture versus inactive treatment
3. Moderate evidence that acupuncture is
more effective than inactive treatment for pain
4. Acupuncture versus wait list control
relief post treatment and at short term follow
up
4. Moderate evidence that patients receiving
acupuncture report less pain than those on a
wait list control at short term follow up
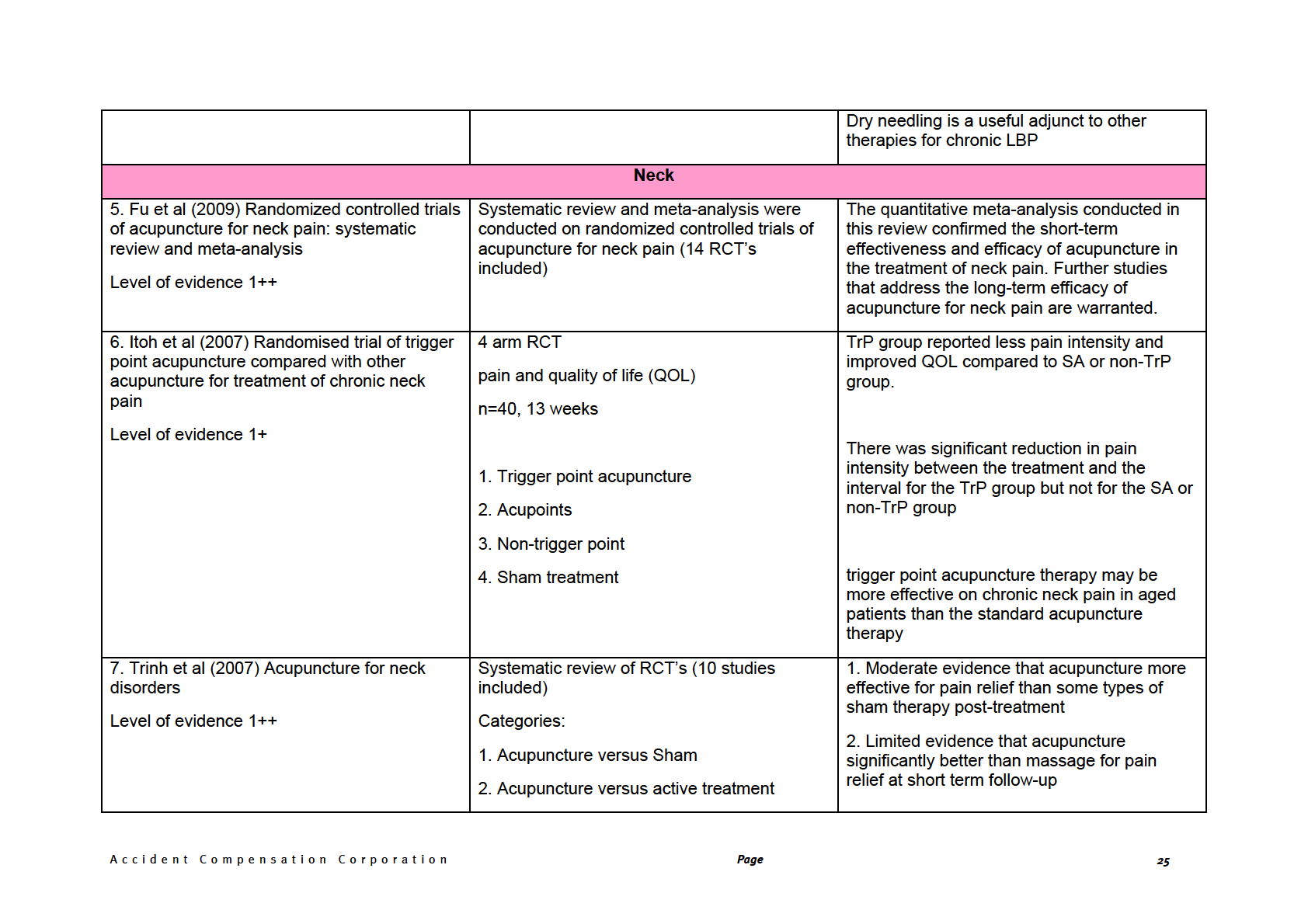
8. White et al (2004) Acupuncture versus
Randomized, single-blind, placebo-controlled, Both groups improved statistically from
placebo for the treatment of chronic
parallel-arm trial with 1-year follow-up
baseline
mechanical neck pain: a randomized,
controlled trial
n=135, 4 weeks, 8 treatments
Level of evidence 1-
1. acupuncture
Acupuncture was more effective than mock
treatment for pain relief at short term follow up
2. Mock transcutaneous electrical stimulation
of acupuncture points using a
decommissioned electroacupuncture
stimulation unit
However, this difference was not clinically
significant
Limitations All treatments were provided by 1
practitioner, control did not mimic the process
of needling, non-intervention group was not
present
Acupuncture reduced neck pain and produced
a statistically, but not clinically, significant
effect compared with placebo. The beneficial
effects of acupuncture for pain may be due to
both nonspecific and specific
9. Zhu et al (2002) A controlled trial on
Chinese medicine (CM) acupuncture for
Significant reduction in subjective pain
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
26
acupuncture for chronic neck pain
chronic neck pain (CNP)
intensity (VAS), pain hours per day, analgesic
pill consumption & increased activity level
Level of evidence 1+
Single blind, controlled, crossover, clinical trial following 9 session real CM acupuncture
n=29
2 groups received two phases of treatment
with a washout period between the two
The same for sham but to a lesser degree
phases
Sham acupuncture has a therapeutic effect
Group A - CM acupuncture, washout, sham
acupuncture Group B – Sham, washout, CM
Acupuncture may be a suitable intervention
acupuncture
for neck pain – not applicable to those with
neurological or psychosocial signs present
9 sessions over 3 weeks
Acupuncture and sham treatment have a long
term effect of neck pain lasting at least 16
weeks
Manual twisting of the needle was applied on
all points plus strong electrical stimulation of
distal points in CM acupuncture. Sham
acupoints (lateral to the real) and sham
Neither Sham or real CM acupuncture had
(weak) electrical stimulation was used in the
any significant effect on objective measures
control group.
Outcome measures at baseline, after each
phase of treatment, after washout, & at 16
week follow-up
He et al 2005 Effect of intensive acupuncture
This study examines whether intensive
The ‘pain-related activity impairment at work’
on pain-related social and psychological
acupuncture treatment can improve several
was significantly less in Acupuncture group
variables for women with chronic neck and
social and psychological variables for women
than sham (control) by the end of treatment
shoulder pain - an RCT with six month and
with chronic pain in the neck and shoulders,
three year follow up
and whether possible effects are long-lasting
There were significant differences between
the groups for; quality of sleep, anxiety,
Level of evidence 1-
depression & satisfaction with life
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
27
N=24 female office workers
Acupuncture was applied 10 times during 3-4
At 6 month & 3 year follow ups the
weeks
acupuncture group showed further
improvements in most variables and was
again significantly different from the control
1. Acupuncture points
group
2. Sham points (control group)
Intensive acupuncture treatment may improve;
activity at work and social & psychological
In addition, acupressure was given to patients variables for women with chronic pain in the
between treatments, at either real or sham
neck and shoulders
points. Questionnaires for social and
psychological variables were completed
The effect may last for at least 3 years
before treatment, just after the course, 6
months & 3 years follow up
He et al (2004) Effect of acupuncture
Randomized single blind controlled trial
The intensity & frequency of pain decreased
treatment on chronic neck and shoulder pain
more for TG than CG during treatment period
in sedentary female workers: a 6-month and
N= 24 female office workers
3-year follow-up study
randomly assigned to
Level of evidence 1+
At 3 year follow up, TG reported less pain
than pre treatment
1. Test Group (TG) - anti-pain acupoints
Headache decreased during treatment period
for both groups, but more for TG than for CG
2. Control Group (CG) - placebo-points
At 3 year follow up TG still had decrease in
Acupuncture was applied 10 times during 3-4
headaches
weeks
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
28
Outcome measures; pain threshold (PPT) in
In CG headache returned to pre-treatment
the neck and shoulders with algometry before level
first treatment, after the last treatment & at 6
month follow up. Questionnaires on muscle
pain and headache were answered at the
same time points & at 3 years follow up
PPT of some muscles increased during the
treatment period for TG & remained higher 6
months post treatment
Acupuncture treatment may have long term
effect in reducing chronic pain in neck &
shoulders & related headache
Acupuncture more effective than sham
Sham acupuncture may have immediate pain
relieving effect on chronic neck & shoulder
pain
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
29
7. Appendix 3: Evidence tables for shoulder, knee and pain
SHOULDERS
Reference and study
Studies
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
Favejee MM,
N = 5 Cochrane
Interventions: oral
Pain
Cheing 2008 (n=70)
In the short term,
Huisstede BM, Koes
reviews & 18 RCTs [1
medications, injection
moderate evidence
BW, Huisstede BMA.
Cochrane review and 1 therapy, physiotherapy,
• electroacupuncture from one small study
RCT for acupuncture]
acupuncture,
vs. interferential
was found for the
Function
arthrographic distension &
electrotherapy
effectiveness of
suprascapular nerve
vs.placebo.
acupuncture and
Frozen shoulder: the
block
• Significant
exercises with respect
effectiveness of
Total number of
differences were
to shoulder function
conservative and
patients in the studies:
found between
[Sun 2001]
surgical interventions--
not reported
Quality scores:
both treatment
systematic review.
Length of treatment:
groups and the
variable
Cheing 2008, 33%
control group, on
[low]
pain and function
Limited evidence for
Inclusion criteria:
(all p<0.001) at 4
effectiveness of
BJSM online
patients with frozen
Sun 2001, 55% [high]
weeks.
electroacupuncture
2011;45(1):49-56.
shoulder, not caused
Comparison (placebo):
compared to placebo
by acute trauma or
variable
Lin 1994, 36% [low]
on pain and function at
systemic disease; an
Sun 2001 (n=35)
Yuan 1995, 36% [low]
4 weeks [Cheing 2008]
Netherlands
intervention for treating
frozen shoulder; pain,
• acupuncture
+
Co-interventions: variable
exercises vs.
function or recovery
outcomes were
exercises alone
Included studies
•
reported; in English,
significant
looking at acupuncture:
difference in favour
French, German or
Cheing 2008, Sun
of acupuncture +
Dutch.
2001, Lin 1994, Yuan
exercises on
shoulder function
1995.
at 20 weeks
Exclusion criteria: none
• 9.40 WMD; 95%
reported
CI 0.52 to 18.28
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
30
Lin 1994 (n=100)
Databases used:
• suprascapular
Cochrane library,
nerve blocks
PubMed, EMBASE,
(SSNB) vs.
CINAHL, PeDro
acupuncture
• significant
differences in
favour of SSNB on
Description of the
pain and ROM 30
methodological
min after treatment
assessment of studies:
• WMD
(pain)
1.33;
score adapted from
95% CI 1.22 to
Cochrane review
1.44)
handbook
• WMD
(flexion)
−7.00; −11.17 to
−2.83)
No meta-analysis
Yuan 1995
• significant
Qualitative (‘best-
difference in favour
evidence’) analysis
of acupuncture
according to Jing
Luo over traditional
acupuncture on
recovery
• RR 1.50; 95% CI
1.08 to 2.09
• follow-up time not
reported
Study type: Systematic review with qualitative analysis
Quality: SIGN 1+
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
31
Comments: Wide range of interventions; good search and methodology appraisal; qualitative analysis appropriate; heterogeneity not formally reported; some
reporting not sufficient enough (due to inability to access online supplementary appendices)
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
32
Reference and study
Participants
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
Molsberger AF,
n=424 participants
1. Acupuncture:
15
Pain (VAS)
Primary end-point:
In people with chronic
Schneider T, Gotthardt
treatments (1-3 per
shoulder pain, ‘true’
H, Drabik A.
• 135 ‘sham’ group
week, lasting 20
acupuncture reduced
• 154
acupuncture
mins)
pain and improved
group
[‘Responder’ =
‘Responders’ at 3
mobility significantly
• 135 ‘COT’ group
reduction of pain by
months:
more than ‘sham’
German Randomized
2. ‘Sham”
acupuncture: ≥50% on VAS from
acupuncture or
Acupuncture Trial for
as above
initial score]
1. 64.9%
conventional therapy at
chronic shoulder pain
Inclusions: one-sided
2. 23.7%
6 weeks and 3 months.
(GRASP) - A
3. 37.0%
shoulder pain ≥6 weeks
pragmatic, controlled,
and up to two years; an 3. ‘COT’:
conventional
Shoulder mobility (Jobe
patient-blinded, multi-
average pain score of
orthopaedic therapy
test; degree of
1 vs. 2 p<0.01
centre trial in an
with 50mg diclofenac
≥50 mm on a VAS in
abduction; % full
outpatient care
daily and 15
the past week; age
elevation of arm
1 vs. 3 p<0.01
environment.
treatment sessions
between 25 and 65
individually selected
possible)
years; the ability to
from physiotherapy,
communicate
physical exercise,
OR (1 vs. 2 ) = 5.96
Pain 2010;151(1):146-
heat/cold therapy,
in German
[95%CI: 3.45-10.35]
54.
ultrasound and TENS
Exclusions: injections
Length of treatment: 6
OR (1 vs. 3) = 3.15
Germany
or cortisone of any kind; weeks
[95%CI: 1.90-5.23]
neurological disorders
causing shoulder pain;
Multicentre study
referred pain from the
Selection of acupuncture
cervical spine; OA of
points:
Secondary end-point:
the
1. Acupuncture:
gleno-humeral joint or
consensus agreement
systemic bone and joint
from experts to use
‘Responders’
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
33
disorder (e.g.
particular points ±
immediately after
rheumatoid arthritis);
others (5-10 needles)
treatment ended:
history of shoulder
2. ‘Sham’: 8 needles at
surgery; other
defined non-
1. 68.1%
acupuncture points
2. 39.3%
current therapy
near both tibia
3. 28.1%
involving analgesics;
overt psychiatric illness;
pregnancy; incapacity
1 vs. 2 p<0.001
for work >3 months
1 vs. 3 p<0.001
preceding
the trial, and pending
compensation
OR (1 vs. 2 ) = 2.30
procedure
[95%CI: 1.40-3.78]
Randomisation &
OR (1 vs. 3) = 3.77
allocation concealment
reported
[95%CI: 2.24-6.41]
Blinding:
• patients blinded to
Post hoc analyses of
whether in
shoulder mobility:
acupuncture or
sham group but
Acupuncture group all
not to COT group
significantly improved
• statisticians
at 6 weeks & 3 months
blinded to
compared to sham or
allocation group
COT (see full text for
• observers
not
details)
blinded
• those
administering
treatment not
blinded
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
34
Dropouts at 3 months:
• 61/135
(45%)
‘sham’ group
• 26/154
(17%)
acupuncture
group
• 29/135
(22%)
‘COT’ group
• overall
drop-out
rate ~ 27%
Follow-up: at end of
treatment and at 3
months after
Characteristics:
Mean age: 51 (sham);
50 (acupuncture); 51
(COT) years
% Male: 33; 43; 33%
Duration: 12; 11; 10
months
No significant
differences between
groups in any
characteristic reported
i.e. affected shoulder,
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
35
pain intensity
Secondary care
(outpatients)
Power calculation
ITT analysis
Mixed diagnoses: 40%
bursitis subacromialis,
29.4% bursitis calcarea,
3.9% frozen shoulder &
2.5% biceps tendinitis
Study type: multi-centre pragmatic RCT
Quality: 1+
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
36
Comments: Well conducted pragmatic, three-armed, patient-blinded, multi-centre RCT. Not observer blinded for acupuncture or sham & not blinded for COT
therefore possibility of bias present. At 3 months ~27% participants dropped out but ITT analysis i.e. drop-outs considered ‘non-responders’. ‘Mixed’
population.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
37
Reference and study
Participants
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
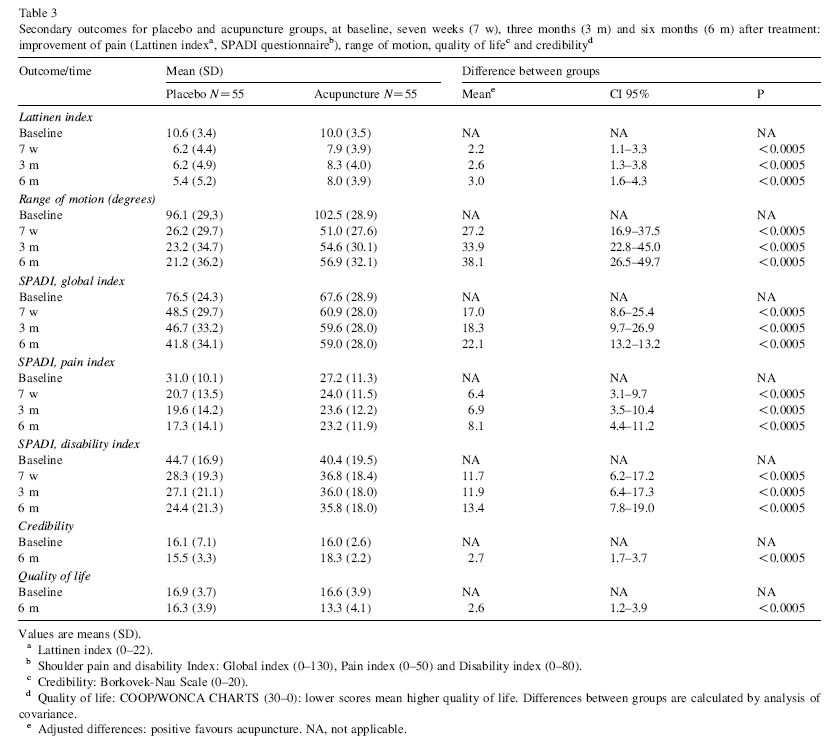
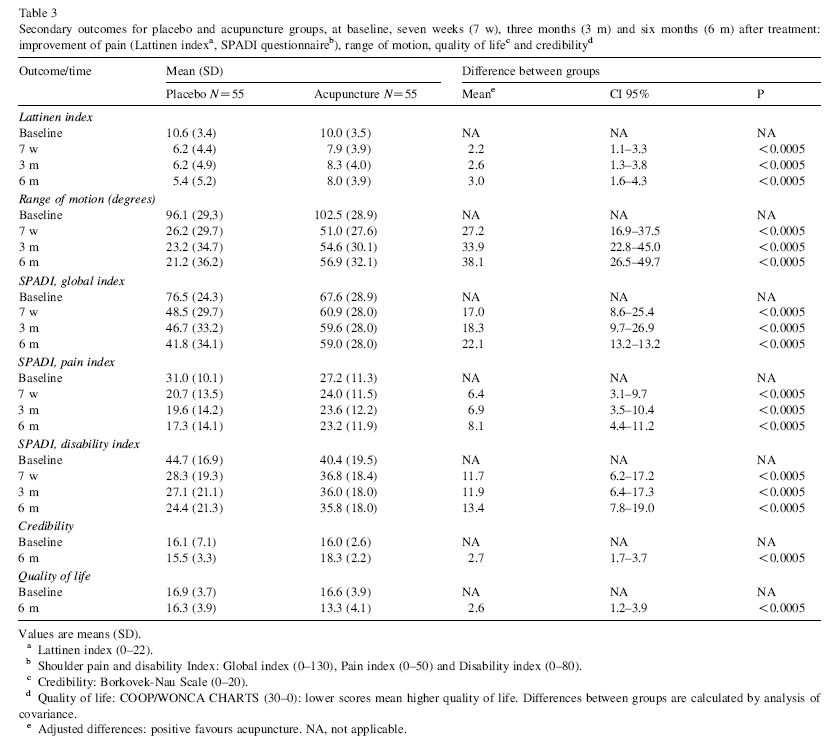
Guerra de Hoyos JA,
n=130
Treatment: “standardised” Primary outcome:
Mean difference VAS
“All results consistently
Andres Martin Mdel C,
electro-acupuncture i.e.
(95%CI):
suggested that real
Bassas y Baena de
• 65 in acupuncture all patients had same 4
Pain (VAS)
acupuncture is more
Leon E, Vigara Lopez
arm
acupuncture points used
effective than placebo-
M, Molina Lopez T,
• 65 in placebo
acupuncture to treat
7 weeks:
Verdugo Morilla FA, et
(“sham”) arm
Secondary outcomes:
pain and disability in
al.
patients with shoulder
Length of treatment: 8
• 1.5
(0.8-2.3)
Lattinen index (pain)
p<0.0005
pain from different
Inclusions: Clinical
weeks
causes, mainly rotator
diagnosis of soft tissue
ROM
cuff disease and
Randomised trial of
shoulder lesions; no
3 months:
capsulitis.”
long term effect of
swelling signs; no
SPADI (pain &
acupuncture for
recent trauma (previous Comparison: “sham”
disability)
• 1.5
(0.6-2.5)
shoulder pain.
3 months); no previous
acupuncture with needles
p<0.0005
acupuncture
not penetrating skin and
COOP/WONCA (quality
treatments; age of 18 or no electrical current
of life)
older
6 months:
Pain 2004;112(3):289-
98.
Co-interventions:
•
Adverse effects
2.0
(1.2-2.9)
p<0.0005
Exclusions: critical
diclofenac 50mg every 8
physical or mental
hours, if needed and
Spain
condition, febrile
famotidine 20mg every 12
Similar results for all
condition, systemic
hors if needed for
secondary outcomes
dermatological
dyspepsia
(see table 3 below)
conditions, neoplasms,
allergy to diclofenac,
referred pain from neck
ITT analysis
or thorax, rupture of
Adverse events:
tendons or bone
Intervention group:
fractures, pregnancy,
litigation, no intention to
2 fainted during
participate or follow
treatment; 3 reported
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
38
instructions.
dizziness; 5 bruising at
puncture site
Blinding: patient and
evaluators blinded to
5 reported dyspepsia (1
allocation
intervention , 4 in
control group)
Dropouts: 10 in both
groups i.e. 15% at 6
3 reported anxiety
months
reaction (1 intervention,
2 in control group)
Follow-up: weekly for
the 7 weeks of
treatment, then 3 and 6
months
Characteristics
(treatment/placebo):
Mean age: 60/ 59yrs
% Female: 49 /48%
Duration of symptoms:
5.7/6.8 months
Additional data: marital
status, education,
working, exercise,
diagnosis, location
pain…
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
39
Setting: primary care
Study type: RCT
Quality: SIGN 1+
Comments: Well conducted RCT. Randomisation method and allocation concealment good. Power calculation done.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
40
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
41
Reference and study
Participants
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
Lathia AT, Jung SM,
n= 31
1. Traditional
SPADI (Shoulder Pain Change from baseline
“Acupuncture may be
Chen LX.
acupuncture:
& Disability Index)
SPADI score (see
an alternative and
• 11
traditional
individualized
Table 2 below):
adjunctive treatment
acupuncture
acupuncture
reported that after 6
• 9
standardised
treatment according
weeks treatment the
to help improve pain
Efficacy of
acupuncture
to the approaches
traditional and
and function in
acupuncture as a
• 11 sham acupuncture
established by TCM;
standard groups
patients with chronic,
treatment for chronic
at each session, the
showed at clinically
non-rheumatologic
shoulder pain.
patient was
shoulder pain.”
Inclusion: ≥18 years old;
significant* change in
evaluated, and
SPADI score ≥30; shoulder
SPADI scores from
different treatment
pain ≥8 weeks;
baseline
points were chosen
J Altern Complement
acupuncture naïve; either
according to the
Reviewer’s conclusion:
Med 2009;15(6):613-8.
no previous treatment or
patient’s symptoms;
Statistically and
failed conventional
the points used varied
Treatment Effect (see
treatment ≥1 month prior to
between patients and
clinically significant
Table 3 below)
:
reduction in SPADI
USA
enrolment
between treatment
sessions for each
Difference in mean
score after 6 weeks
patient.
SPADI score (95%CI)
treatment for both the
from sham
traditional acupuncture
Exclusion: inflammatory or
acupuncture group:
group and standard
infectious arthritis; shoulder 2. Standardised
acupuncture group
fracture; stroke; pregnancy;
acupuncture:
compared to sham
any corticosteroid
treatment based on
acupuncture. The
injections in last 3 months
fixed, standard point
Pain
effect size was similar
protocols.; 7
for both the traditional
acupuncture points
1. -16.2 (-2.7, -29.7)
acupuncture group
relevant to shoulder
p=0.021
Blinding: subjects blind to
and standard
pain were used and
2. -17.2 (-4.9, -29.6)
intervention; SPADI
acupuncture groups.
remained the same
p=0.009
questionnaire investigator
for each session.
blind to allocation;
acupuncturists not blinded
Disability
3. Sham acupuncture:
1. -11.6 (-2.5, -20.6)
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
42
to allocation
carried out with sham
p=0.015
acupuncture needles
2. -10.6 (1.1, -22.3)
and the same points
p=0.073
as the standard point
Allocation concealment:
acupuncture group.
not reported
Total SPADI
Subjects in each group
1. -13.8 (-3.0, -24.7)
p=0.015
Drop-outs: 3 in sham group received the relevant
2. -13.9 (-3.3, -24.5)
failed to complete
acupuncture treatment
p=0.013
intervention because of
twice per week for 6
time constraints (2) or
weeks.
increased pain (1) i.e. 10%
Results from the 6
drop-out rate; only 8
month follow-up were
participants filled out
For the acupuncture,
only available foe 8
SPADI questionnaire at 6
subjects, of which,
months i.e. 74% ‘drop-out’
8–16 single-use,
only 2 reported
rate
disposable, sterile 36-
improvement in pain
gauge needles were
and disability since last
used and were left in
treatment (no figures
Follow-up: 6 weeks (end of place for 20 minutes.
reported)
treatment) and 6 months
Each session lasted
about 30 minutes.
*Clinically significant
Characteristics
worsening in shoulder
(traditional/standard/sham):
pain and function is an
Co-interventions: any
increase of ≥10 points.
Mean age: 62/65/59 yrs
medications were to be
continued and not
Men: 100/100/73%*
changed for 3 months
Duration pain: 48/28/51
prior and during study
months
Diabetes: 18/51/30%
Unilateral pain:
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
43
100/78/70%
Setting: Secondary care
*[p=0.05]
Study type: RCT
Quality: SIGN 1-
Comments: Small study in mainly male veterans with no power calculation. Long-term follow-up severely limited. Cannot entirely rule out bias from non-
blinding of acupuncturists to allocation group. The significance of a similar effect size for both the traditional and standard acupuncture groups is unclear.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
44
Reference and study
Studies
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
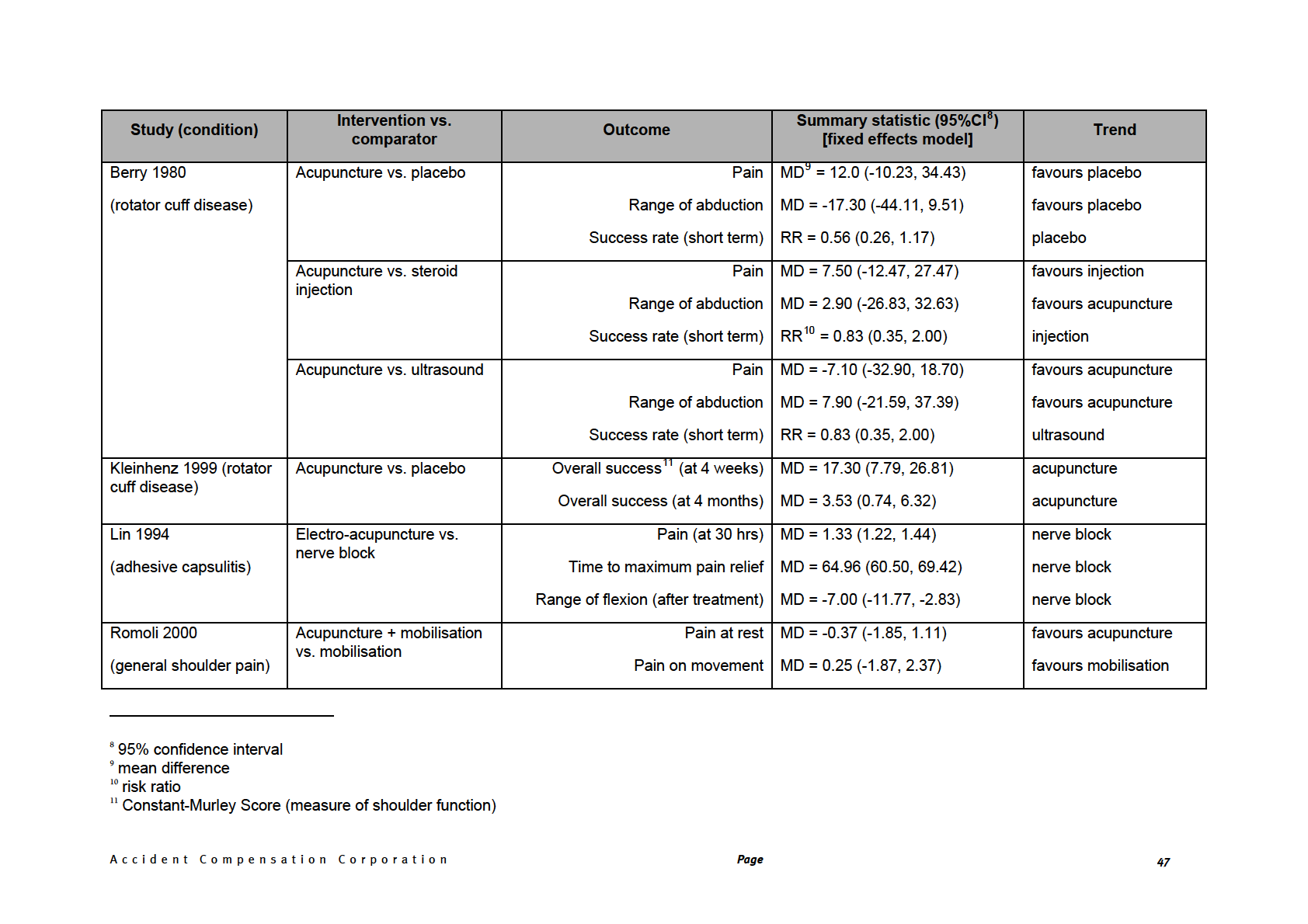
Green S, Buchbinder R, N=9 (
Intervention: ‘Traditional’
See Table below
See Table below for
“Due to a small number
Hetrick S.
or ‘classic’ acupuncture
summary of results
of clinical and
methodologically
diverse trials, little can
Inclusion: All RCTs or
be concluded from this
Acupuncture for
quasi-randomised
Length of treatment:
review. There is little
shoulder pain.
controlled trials; adults
variable
evidence to support or
>16yrs; shoulder pain
refute the use of
or disorder >3 weeks
acupuncture for
Cochrane Database
Comparison: Placebo
shoulder pain although
Syst Rev
(Berry 1980; Kleinhenz
there may be short-
2005(2):CD005319.
Exclusion criteria: a
1999; Moore 1976);
term benefit with
history of significant
ultrasound & steroid
respect to pain and
trauma or systemic
injection (Berry 1980);
function.”
Australia
inflammatory conditions nerve block (Lin 1994);
such as rheumatoid
mobilisation (Romali
arthritis, polymyalgia
2000); exercise (Sun
Reviewer’s conclusion:
rheumatica and
2001); Trager (Dyson-
Included studies: Berry
fracture, hemiplegic
Hudson 2001)
One small study (n=35)
1980 (n=60);
shoulders,
showed that exercise
Ceccherelli 2001
postoperative and peri-
and acupuncture
(n=44); Dyson-Hudson
operative shoulder pain
together was more
2001(n=20); Kleinhenz
and pain in the
NB: Ceccherelli 2001
efficacious than
1999 (n=52); Lin 1994
shoulder region as part
compared deep with
exercise alone for the
(n=150); Moore 1976
of a complex myofacial
shallow acupuncture, and
treatment of adhesive
(n=42); Romoli 2000
neck/shoulder/arm pain Yuan 1995 compared
capsulitis both post-
(n=24); Sun 2001
acupuncture with sites
intervention and at 20
(n=35); Yuan 1995
determined by TCM
weeks.
(n=98)
compared to the
Databases: MEDLINE,
distribution of Jing-Luo
The results from the
EMBASE, CINAHL,
rest of the studies are
Science Citation Index
conflicting or mixed, for
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
45
Co-interventions: see
example, One study
summary table below
(n=52) found that
Methodological
acupuncture was more
assessment:
efficacious than
descriptive (including
placebo in improving
appropriate
the Constant-Murley
randomisation,
score for rotator cuff
allocation concealment,
disease at 4 weeks and
blinding, number lost to
4 months. This is in
follow up and intention
contrast with another
to treat analysis),
study (n=60) that found
quantitative scoring for
that acupuncture was
allocation concealment
less efficacious than
only
placebo for rotator cuff
disease when
measuring treatment
No meta-analysis due
‘success’. However,
to clinical heterogeneity
because these two
studies used different
outcomes, they ability
to directly compare
Fixed effects model
them is limited, at least.
Study type: Systematic review
Quality: SIGN 1++
Comments: Well conducted SR with narrative synthesis. The paper by Moore (1976) was not used to construct forest plot. Nine studies of varying
methodological quality, most with small numbers of participants. Heterogeneity of populations, interventions, comparators and outcomes.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
46
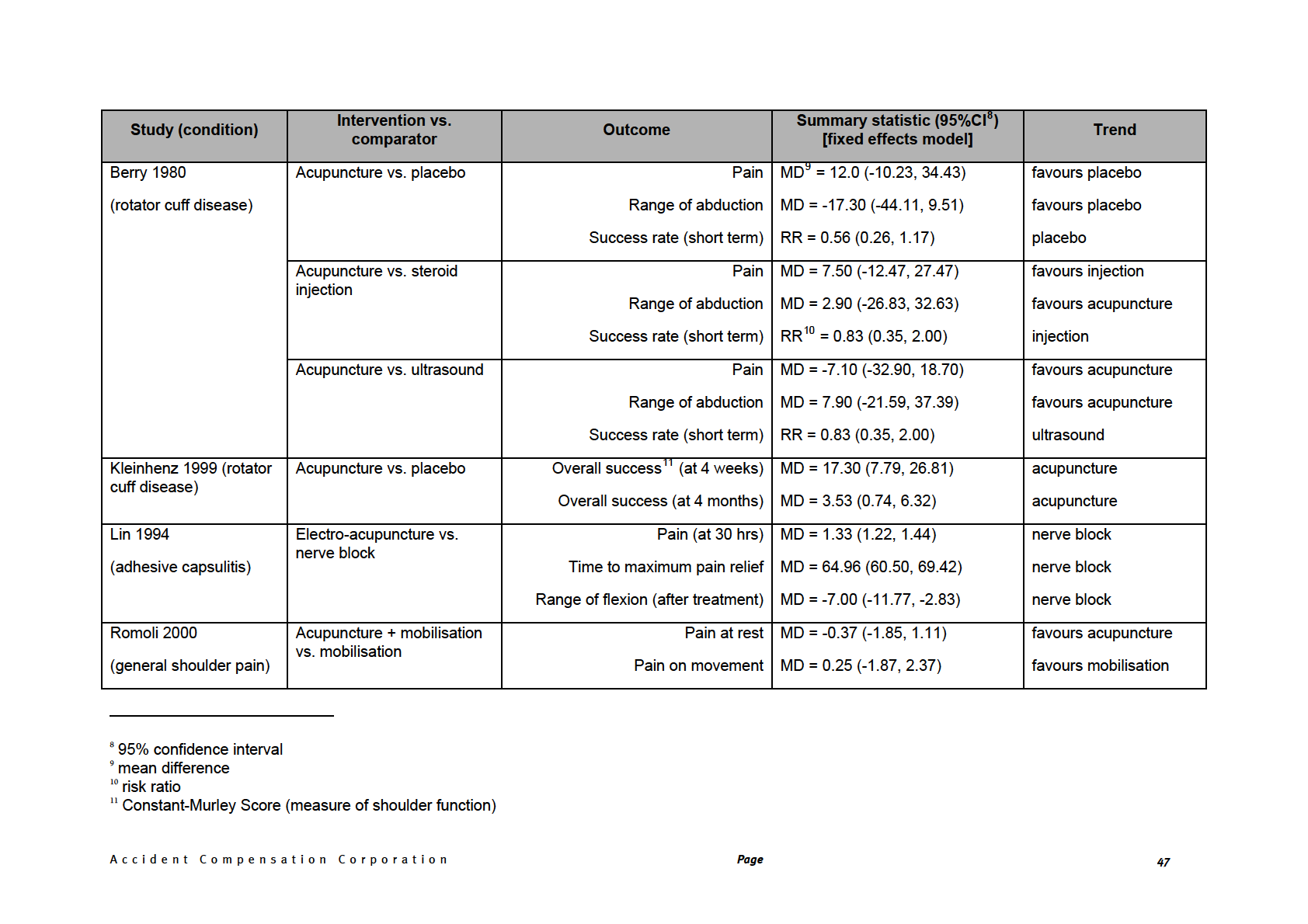
Active flexion MD = -13.13 (-39.79, 13.53)
favours mobilisation
Active abduction MD = -14.37 (-49.94, 21.20)
favours mobilisation
Sun 2001
Acupuncture vs. exercise
Constant
12 (post-intervention): MD = 9.20 (0.54, 17.86)
acupuncture
(adhesive capsulitis)
Constant (20 weeks): MD = 9.40 (0.52, 18.28)
acupuncture
Dyson-Hudson 2001
Acupuncture vs. Trager
Wheelchair index
13 (post- MD = 1.70 (-21.91, 25.31)
favours Trager
(general shoulder pain)
intervention): MD = 16.00 (-9.03, 41.03)
favours Trager
Wheelchair index (5 weeks):
Ceccherelli 2001
Deep vs. shallow
McGill Pain
14 (post-intervention): MD = -10.31 (-15.44, -5.18)
deep
(general shoulder pain)
acupuncture
McGill Pain (3 months): MD = -8.00 (-12.20, -3.80)
deep
Yuan 1995
Traditional vs. Jing Luo
Recovery: RR = 1.50 (1.08, 2.09)
Jing Luo
acupuncture
(peri-arthritis)
12 Constant-Murley Score (measure of shoulder function)
13 Wheelchair Users Shoulder Pain Index (WUSPI)
14 McGill Pain Questionnaire
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
48
Reference and study
Participants
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
Johansson K,
n=85
Intervention:
Constant-Murley Score Individual score
“The results suggest
Adolfsson L, Foldevi M.
‘standardised’
changes not reported
that acupuncture is
• 44 in acupuncture
acupuncture at 4 points
more efficacious than
group
(10 sessions)* + home
ultrasound in patients
• 41 in ultrasound
Adolfsson-Lysholm
exercise programme
with impingement
Effects of acupuncture
group
Shoulder score
Combined score
syndrome.”
versus ultrasound in
showed larger change
patients with
(p=0.045) at all 4 time
impingement
Inclusions: 30 - 60yrs of
Length of treatment: 5
points for acupuncture
UCLA End-Result
syndrome: randomized age; ‘typical’ history of
weeks
Reviewer’s conclusion:
Score
clinical trial.
shoulder impingement;
positive Neer
Acupuncture no more
No differences were
impingement test; ≥2
effective than
Comparison:
found across the 4 time
months duration; 3 of 4 of
Combined Score of all
ultrasound on ITT
Physical Therapy
standardised ultrasound
points when ITT
analysis.
2005;85(6):490-501.
Hawkins-Kennedy
above scales
analysis
impingement sign, Jobe
(10 sessions)* + home
supraspinatus test, Neer
exercise programme
impingement sign or
Sweden
painfull arc between 60
and 120° active
abduction
Co-interventions: unclear,
but “additional” pain
medication reported
Exclusions: X-ray
findings of malignancy,
G-H joint OA, bony
*twice weekly for 5 weeks
spurs/osteophytes
decreasing subacromial
space; polyarthritis,
rheumatoid arthritis,
fibromyalgia; history of
surgery, fracture or
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
49
dislocation in shoulder;
history/present instability
any shoulder joint;
suspicion of frozen
shoulder; cervical spine
problems; previous
ultrasound or
acupuncture for same
problem; steroid injection;
ruptured rotator cuff
clinically; acute
subacromial bursitis;
communication difficulty
Dropouts: none post-
treatment; 3.5% (2
acupuncture group/1
ultrasound group) at 3
months; 5.9% (0/2) at 6
months; 12.9% (2/4) at
12 months
Follow-up: immediately
post-intervention; 3, 6 &
12 months
Blinding: observer
blinded
Characteristics
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
50
(acupuncture/ultrasound):
Mean age: 49/49 yrs
% Male: 27/34%
No significant differeence
in duration, occupation,
sick leave taken,
analgesic use, exercise
frequency or smoking
status
Setting: Primary care
Study type: RCT
Quality: SIGN 1-
Comments: Smallish study with inappropriate analysis showing a (barely) significant result. Complicated selection criteria. Reported “concealed”
randomisation but only observers blinded. Comparator of dubious therapeutic value. Power calculation done. ITT analysis.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
51
Reference and study
Participants
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
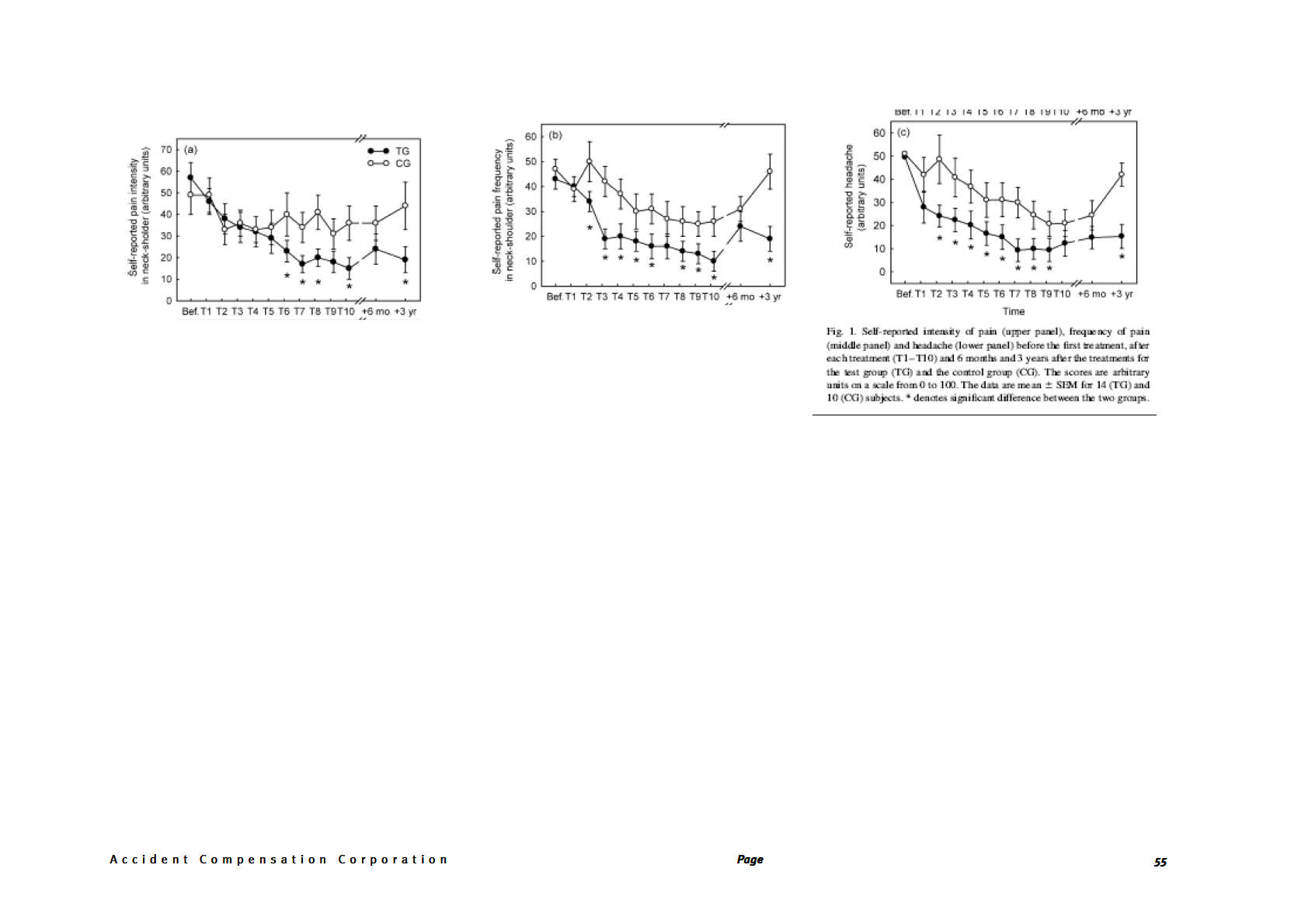
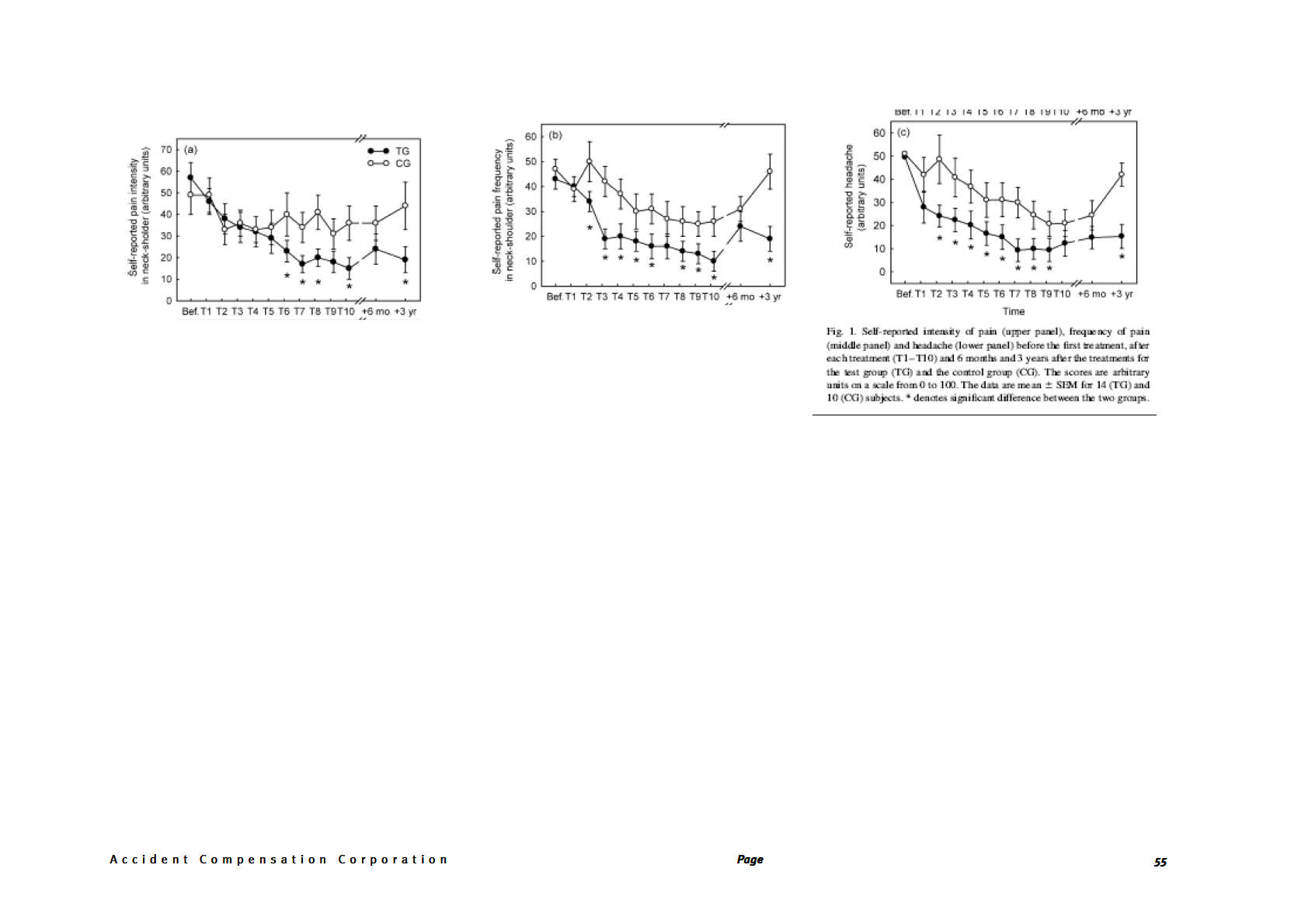
(see fig 1 below)
He D, Veiersted K,
N=24
Intervention:
Pain (intensity,
Pain intensity (mean
“The main finding in
Hostmark A, Medbo J.
electroacupuncture,
frequency)
intervention vs. mean
this study was that
• 14 in acupuncture acupuncture, & ear
control group)
adequate acupuncture
group
acupressure of
treatment reduced the
• 10 in control
standardised points*
intensity and frequency
Effect of acupuncture
group
Pain threshold
of muscle pain, the
treatment on chronic
At end of treatment:
degree of headaches,
neck and shoulder pain
and a number of trigger
in sedentary female
Inclusions: Women
Length of treatment: 3
15 vs. 36 units; p=0.02
points became less
workers: a 6-month and office workers with
treatments per week with
Headache
tender.”
3-year follow-up study. chronic (≥3 months in
a total of 10 treatments
previous year) pain in
over 2-4 weeks; each
At 6 months:
the shoulder and neck
treatment lasted 45 min
Blood variables
region; 20-50yrs of age;
24 vs. 36; p=0.15
Pain 2004;109(3):299-
307.
pain was severe
enough to interfere with
Reviewer’s conclusion:
Comparison:
work/spare time
electroacupuncture
At three years:
Some statistically
activities;
without any voltage
significant differences
Norway
19 vs. 44; p<0.04
applied, acupuncture 10-
in outcomes in favour
40mm distal to actual
of intervention at
Exclusions: diabetes,
points, & ear acupressure
differing timepoints.
neurological,
4-6mm below actual
Frequency of pain:
However, due to this
rheumatological or
points
being a very small
other diseases;
(intervention vs. control study and questions
pregnancy, breast-
group)
about validity of
feeding
outcome measures and
Co-interventions: none
variation in results, the
reviewer cannot
At end of treatment:
exclude that the results
Dropouts: none
*16 body acu-points, 6
not reported
seen are due largely to
ear acu-points
bias.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
52
Blinding: Participants
At 6 months:
and examiner blinded to
allocation;
24 vs. 31; p=0.18
acupuncturist not
blinded
At three years:
19 vs. 46; p=0.003
Follow-up: 6 months, 3
yrs
Pain threshold (PPT)
Characteristics
used algometry on
(acupuncture/control):
particular trigger points
(13); unclear but
Mean age: 49/45 yrs
reported “ several
Sex: all women
improvements but no
impairments in the PPT
Pain duration: 12/12 yrs
for the [treatment
group] during the
Total days pain: 4.3/4.5
study.” The control
days per week
group showed no
improvements.
All other variables
similar
Headache
Setting: secondary care
no significant difference
at end of treatment or 6
months; significant
difference at 3 years
Blood variables
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
53
blood platelet
concentration
increased by 15% just
after treatment in
intervention group; no
change in control
group; no change in
any other measured
blood variable
Study type: RCT
Quality: 1-
Comments: Small study in women office workers from Norway. Acupuncture carried out by one of the authors. Unsure of validity of questionnaires although
VAS well accepted. Complex acupuncture intervention. Utility of trigger point pain threshold uncertain. Three subjects (21%) in the intervention group and 5
(50%) in the control group had other treatments during the 3 year follow-up period.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
54
Reference and study
Participants
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
He D, Hostmark A,
N=24
Intervention:
Pain-related activity
Pain-related activity
“Intensive acupuncture
Veiersted K, Medbo J.
electroacupuncture,
impairment at home
impairment
treatment may improve
• 14 in acupuncture acupuncture, & ear
and work
activity at work and
group
acupressure of
Work: significant
several relevant social
• 10 in control
standardised points*
difference after 6th &
and psychological
Effect of intensive
group
10th treatment [p
variables for women
acupuncture on pain-
Quality of sleep
values not reported],
with chronic pain in the
related social and
and at 3 years [p=0.04]
neck and shoulders.
psychological variables Inclusions: Women
Length of treatment: 3
The effect may last for
for women with chronic
office workers with
treatments per week with
Degree of irritability &
at least three years.”
neck and shoulder pain chronic (≥3 months in
a total of 10 treatments
anxiety
- an RCT with six
previous year) pain in
over 2-4 weeks; each
Home: significant
month and three year
the shoulder and neck
treatment lasted 45 min
differeence at 3 years
follow up.
region; 20-50yrs of age;
[p=0.03]
pain was severe
Degree of satisfaction
enough to interfere with
with life
Reviewer’s conclusion:
Comparison:
work/spare time
Acupuncture in
electroacupuncture
Quality of sleep
activities;
Some statistically
Medicine
without any voltage
Significant difference
significant differences
2005;23(2):52-61.
applied, acupuncture 10-
Frequency of
after 9th treatment and
in outcomes in favour
40mm distal to actual
depression
of intervention at
6 months and 3 years
Exclusions: diabetes,
points, & ear acupressure
[p<0.01; p<0.03;
differing timepoints.
4-6mm below actual
Norway
neurological,
p<0.03]
However, due to this
rheumatological or
points
being a very small
other diseases;
study and questions
pregnancy, breast-
about validity of
feeding
Degree of irritability &
outcome measures and
Co-interventions: none
anxiety
variation in results, the
reviewer cannot
significant difference
exclude that the results
Dropouts: none
between groups after
*16 body acu-points, 6
seen are due largely to
6th treatment and at 6
ear acu-points
bias.
months and 3 years
follow-up [p<0.02;
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
56
Blinding: Participants
p=0.02; p=0.02]
and examiner blinded to
allocation;
acupuncturist not
blinded
Degree of satisfaction
with life
significant difference
Follow-up: 6 months, 3
between groups after
yrs
the 8th treatment [p
value not reported] and
at 6 months [p<0.01]
and 3 years [p value
Characteristics
not reported] follow-up
(acupuncture/control):
Mean age: 49/45 yrs
Frequency of
Sex: all women
depression
Pain duration: 12/12 yrs
significant difference
between groups after
Total days pain: 4.3/4.5
the 5th-9th treatments
days per week
and at 6 months and 3
All other variables
years follow-up [all
similar
p=0.04]
Setting: secondary care
Study type: RCT
Quality: 1-
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
57
Comments: as He 2004 above
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
58
Reference and study
Participants
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
Johansson K,
n=117
Intervention: injection
Pain & shoulder
No significant
“Neither treatment was
Bergstrom A, Schroder
methylprednisolone +
function (Adolfsson-
differences between
superior in decreasing
K, Foldevi M.
• 65
in
local anaesthetic (if
Lysholm shoulder
two groups with respect pain and improving
corticosteroid
requested they could get
assessment score)
to pain and function as
shoulder function”
group
another injection)
measured by the
• 58 in acupuncture
Adolfsson-Lysholm
Subacromial
group
shoulder assessment
corticosteroid injection
Health-related quality
score
Reviewers’ conclusion:
or acupuncture with
Comparator: manual
of life (EQ-5D)
Neither treatment was
home exercises when
Inclusions: 30-65 yrs
acupuncture
superior, however,
treating patients with
old; presented at one of (standardised acu-points)
cannot exclude
subacromial
5 primary health care
+ home exercise
No significant
Patients’ global
selection bias and/or
impingement in primary centres with shoulder
programme
differences between
assessment of change
performance bias i.e.
care--a randomized
pain and a ‘typical’
two groups with respect baseline characteristics
clinical trial.
history of shoulder
to other secondary
dissimilar, no blinding
impingement; positive
outcomes (QoL; global
to allocation
Neer impingement test;
Length of treatment:
assessment)
≥2 months duration; 3
acupuncture treatment
Fam Pract
was 2x weekly for 5
2011;28(4):355-65.
of 4 of Hawkins-
Kennedy impingement
weeks (30 min session);
sign, Jobe
supraspinatus test,
Sweden
Neer impingement sign
Co-interventions: none
or painfull arc between
reported
60 and 120° active
abduction
Acupuncture administered
by 3 physiotherapists;
Exclusions: X-ray
corticosteroid injection by
findings of malignancy,
3 GPS
G-H joint OA, bony
spurs/osteophytes
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
59
decreasing subacromial
space; polyarthritis,
rheumatoid arthritis,
fibromyalgia; history of
surgery, fracture or
dislocation in shoulder;
history/present
instability any shoulder
joint; suspicion of
frozen shoulder;
cervical spine
problems; previous
ultrasound or
acupuncture for same
problem; steroid
injection; ruptured
rotator cuff clinically;
acute subacromial
bursitis; communication
difficulty
Dropouts: 123
participants randomised
but 6 developed frozen
shoulder and were
excluded, therefore 117
participants; 26 (22%)
of theses 117 were lost
to follow-up
Follow-up: 12 months
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
60
Blinding: treatment
practitioners (3 GPs
and 3 physiotherapists)
ITT analysis: those who
changed treatment
groups but still
continued assessments
as per protocol
Relevant characteristics
(steroid vs.
acupuncture):
Mean age: 50 vs. 51
yrs
% women: 27 vs. 26%
Duration 2-3 months:
24 vs. 48%
Setting: Primary care
Study type: RCT
Quality: 1-
Comments: Multi-centre pragmatic RCT; patients and treatment providers not blinded to allocation; 22% lost to follow-up; ITT analysis included those who
had changed treatment groups but not other ‘drop-outs’; sample size estimation done; 8 participants changed treatment groups (6 from steroid group; 2 from
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
61
acupuncture group)
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
62
Reference and study
Studies
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
Nyberg A, Jonsson P,
N = 20 studies
Interventions:
Pain
Kleinhenz 1999
“The result of this
Sundelin G.
acupuncture,
(n=52)
systematic review
electrotherapy modalities,
indicates contradictory
exercises, mixed
• acupuncture
vs.
scientific evidence to
Total number of
Function
modalities, changing
placebo
support the use of
Limited scientific
patients in the studies:
posture, functional brace
acupuncture
acupuncture for pain
evidence supports the
not reported
• Constant-Murley and function in SAIS
use of conservative
score significantly
patients.”
treatment interventions
improved in
for pain and function in
Length of treatment:
Quality scores:
treatment group
patients with
Inclusion criteria: RCTs variable
post-intervention
subacromial
of patients diagnosed
Kleinhenz 1999, 9/10
[p<0.014]; pain
impingement
with subacromial
[high]
intensity
syndrome:
impingement syndrome
significantly higher
Randomized control
(SAIS) and/or
Comparison (placebo):
Vas 2008, 8/10 [high]
in placebo group at
trials.
established signs and
variable
3 months follow-up
symptoms consistent
Johansson 2005, 8/10
[p<0.05]
with SAIS;
[high]
conservative
Physical Therapy
treatment* (alone or in
Co-interventions: variable
Reviews
combination) vs.
2010;15(6):436-52.
any/placebo/no
Vas 2008 (n=425)
intervention;
• single
point
acupuncture +
Sweden
physiotherapy vs.
mock-TENS +
physiotherapy
*interventions other
Studies included that
• Constant-Murley
than surgery,
were investigating
score significantly
pharmacological
acupuncture: Kleinhenz
improved
treatment and steroid
et al. (1999) , Vas et al.
[p<0.001] in
injections
(2008), Johansson et
treatment group
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
63
al. (2005),
post-intervention
and at 3 month
Exclusion criteria:
follow-up
shoulder diagnoses
other than SAIS;
multiple diagnoses
Johansson 2005 (n=85)
Databases used:
Cochrane library,
• acupuncture
+
PubMed, CINAHL;
home exercise
English only
programme vs.
ultrasound + home
exercise
programme
Description of the
• no significant
methodological
differences
assessment of studies:
between groups on
as per PEDro scale
ITT analysis; per
protocol analysis
acupuncture group
No meta-analysis
better [p=0.045]
Qualitative (‘best-
evidence’) analysis
Study type: Systematic review with qualitative analysis
Quality: SIGN 1++
Comments: Wide range of interventions; good search and methodology appraisal; qualitative analysis appropriate; heterogeneity not formally reported
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
64
KNEES
Reference and study
Studies
Intervention/comparison
Outcome measure
Results/effect size
Notes
design
Manheimer, E., K.
N =16 studies (n =
Treatment/procedure:
Pain
Acupuncture vs.
Sham-controlled trials
Cheng, et al. (2010).
3498 subjects)
traditional (needle)
Sham acupuncture
show statistically
"Acupuncture for
acupuncture
Function
(all joints):
significant benefits;
peripheral joint
however, these
Symptom severity
osteoarthritis."
benefits are small, do
Cochrane Database of
Inclusion: RCTs in any
not meet our pre-
Systematic Reviews(1): language of at least 6
Length of treatment:
Pain
defined thresholds for
CD001977.
weeks observation;
clinical relevance, and
people with
Short-term = 8 weeks
Short-term:
are probably due at
osteoarthritis (OA) of 1
Long-term = 26 weeks
Standardized mean
least partially to
or more peripheral
placebo effects from
US, UK, Netherlands,
difference (SMD)
joints i.e. knee, hip, or
incomplete blinding.
China, Korea, Germany hand; traditional
= -0.28
acupuncture compared Description of comparison
to a sham, other active
(placebo): sham, other
95% confidence
Waiting list-controlled
Included studies:
treatment or waiting list active treatment or
interval (95%CI): -0.45
control group
waiting list control group
to -0.11
trials of acupuncture for
16 RCTs (Christensen
peripheral joint
1992; Molsberger 1994;
9 trials; 1773 subjects
osteoarthritis suggest
statistically significant
Takeda 1994; Berman
Exclusions: only OA of
Co-interventions:
I2 = 64%
and clinically relevant
1999; Fink 2001;
spine; dry
diclofenac or placebo
benefits, much of which
Haslam 2001; Sangdee needling/trigger point
tablet in one study
may be due to
therapy; laser or
Long-term (6 months)
expectation or placebo
2002; Berman 2004;
electro-acupuncture
effects.
Stener-Victorin 2004;
with no needle
SMD = -0.10
Tukmachi 2004;
insertion; comparison
of one form of
95%CI: -0.21 to 0.01
Vas 2004; Witt 2005;
acupuncture with
Scharf 2006; Witt 2006; another
4 trials; 1399 subjects
Foster 2007;
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
65
Williamson 2007)
I2 = 0%
Databases: Cochrane
Central Register of
Controlled trials,
Function
MEDLINE, and
Short-term:
EMBASE
SMD = -0.28
95%CI: -0.46 to -0.09
Methodological
assessment: used the
9 trials; 1829 subjects
following criteria
(adequate sequence
I2 = 69%
generation, allocation
concealment, blinding,
incomplete outcome
Long-term:
data addressed, free of
selective reporting)
SMD = -0.11
plus prognostic factors
similar at baseline, co-
95%CI: -0.22 to 0.00
interventions avoided
or similar, compliance
4 trials; 1398 subjects
acceptable in all
I2 = 6%
groups, timing of
outcome assessment
Symptom severity
similar, and intention to
treat analysis.
Short-term:
SMD = -0.29
Random effects model
95%CI: -0.50 to -0.09
9 trials; 1767 subjects
I2 = 74%
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
66
Long-term:
SMD = -0.11
95%CI: -0.22 to 0.00
4 trials; 1398 subjects
I2 = 2%
Acupuncture vs.
Sham acupuncture
(Knee OA only)
Pain
Short-term:
SMD = -0.29
95%CI: -0.48 to -0.10
8 trials; 1773 subjects
Long-term:
SMD = -0.10
95%CI: -0.21 to 0.01
4 trials; 1399 subjects
Function
Short-term:
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
67
SMD = -0.29
95%CI: -0.49 to -0.08
8 trials; 1767 subjects
Long-term:
SMD = -0.11
95%CI: -0.21 to 0.00
4 trials; 1398 subjects
Symptom severity
Short-term:
SMD = -0.29
95%CI: -0.50 to -0.09
8 trials; 1767 subjects
Long-term:
SMD = not estimable
4 trials; 1398 subjects
Study type: systematic review with meta-analysis
Quality: SIGN 1++
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
68
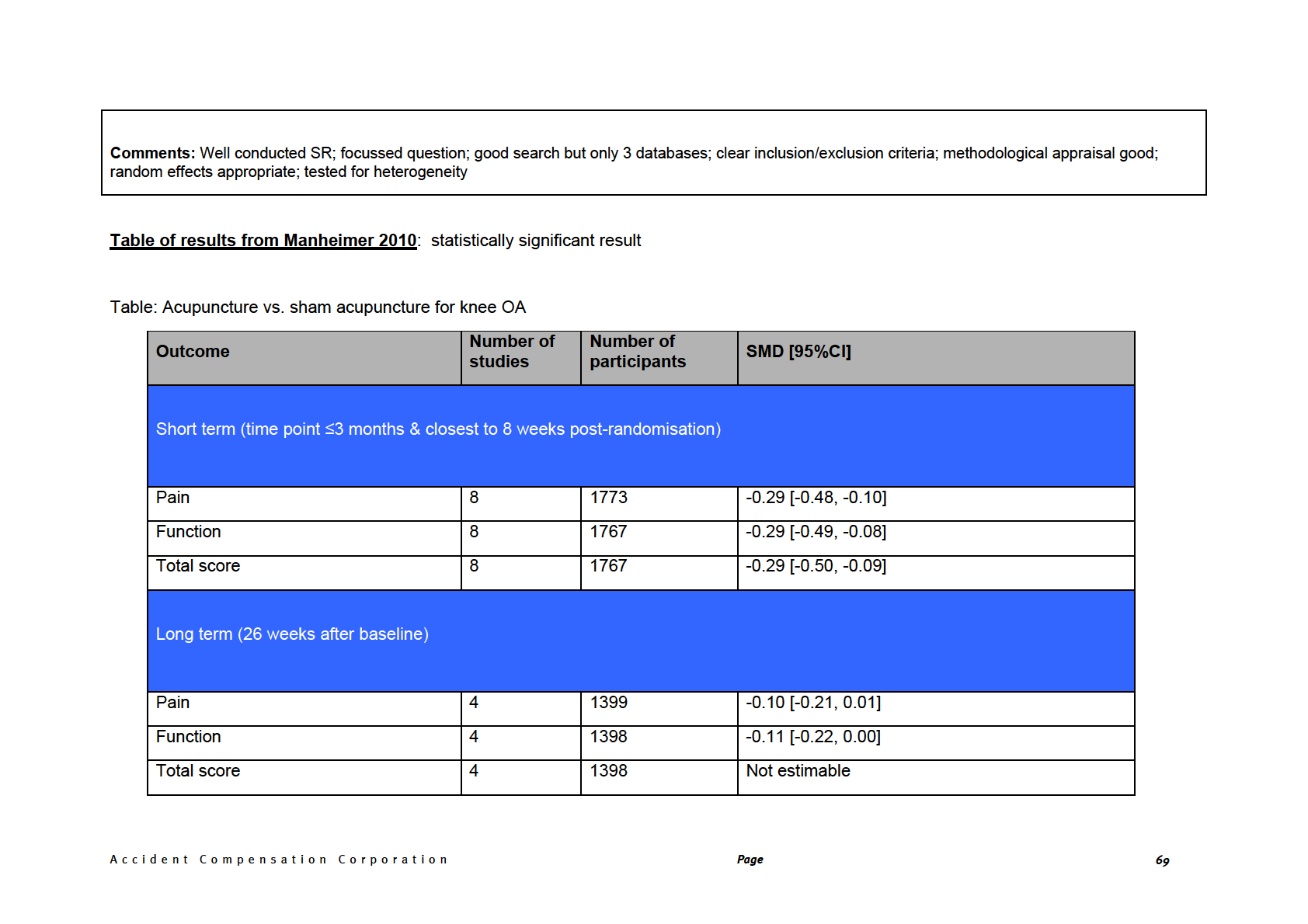
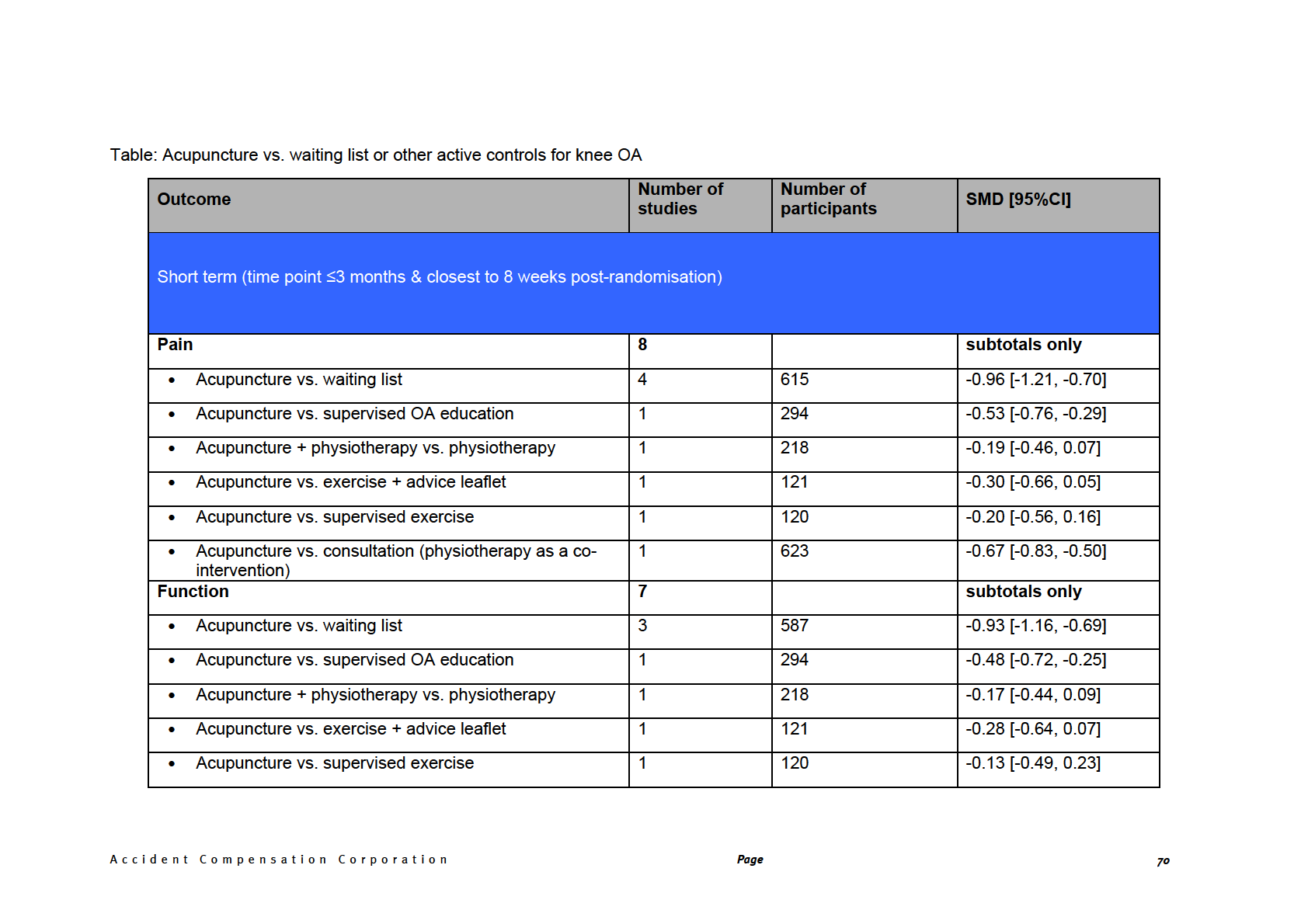
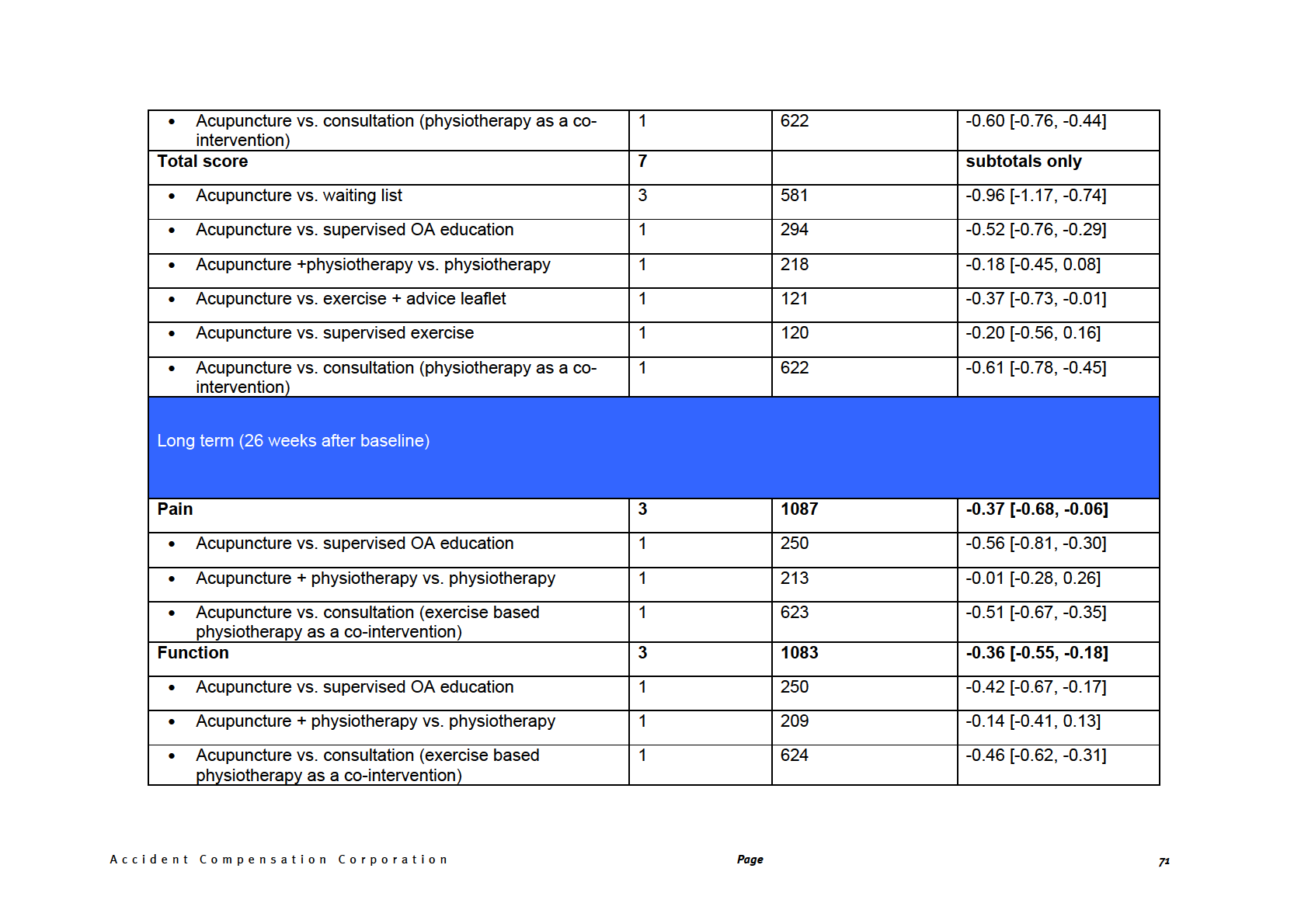
Total score
3
1083
-0.38 [-0.62, -0.15]
• Acupuncture vs. supervised OA education
1
250
-0.46 [-0.71, -0.20]
• Acupuncture + physiotherapy vs. physiotherapy
1
209
-0.12 [-0.39, 0.15]
• Acupuncture vs. consultation (exercise based
1
624
-0.52 [-0.68, -0.36]
physiotherapy as a co-intervention)
Reference and study
Participants
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
Miller E, Maimon Y,
55 participants
Intervention: acupuncture
Knee Society Score
8 weeks:
“Adjunctive
Rosenblatt Y, Mendler
needles placed in points
(KSS) [acupuncture vs.
acupuncture seems to
A, Hasner A, Barad A,
•
treatment arm =
selected by team of TCM
sham]
61.6 vs. 56.8; p=0.15
provide some added
et al. Delayed Effect of
28
practitioners (see full
improvement to
23.7 vs. 24.4; p=0.7
Acupuncture Treatment
•
control arm = 27
paper for details); needles
• total
score
standard care in elderly
in OA of the Knee: A
in place for 20mins and
• pain
score
65 vs. 59.7; p=0.23
patients with OA of the
Blinded, Randomized,
• function
score
knee.”
Inclusions: ≥45 yrs;
manually manipulated
Controlled Trial.
Evid
diagnosis of OA knee
every 5mins
Based Complement
≥6 months; moderate-
Alternat Med 2009.
12 weeks:
severe pain most days
Reviewer’s conclusion:
in last month for which
Comparison: sham
63.54 vs. 53.6; p=0.036 Acupuncture added to
analgesics were used
acupuncture (no insertion
“standard care” may
Israel
for at least 1 month
into skin) at same points
24.0 vs. 21.1; p=0.31
improve total knee
as in treatment group at
score and knee function
67.4 vs. 54.7; p=0.01
same frequency
at 12 weeks after
Patient satisfaction
commencement of
Exclusions: intra-
[acupuncture vs. sham]
therapy but not at 8
articular steroid
weeks. However,
injection into knee(s)
Length of treatment: twice
cannot rule out bias or
within 4 weeks; severe
weekly for 8 weeks
4.87 vs. 3.75; p=0.005
the effect of co-
unstable chronic illness
intervention, as this is
e.g. CHF, CRF, cancer
poorly reported.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
72
Co-interventions:
Adverse effects
“standard therapy (e.g.
Dropouts: 25%
NSAIDs)
10 during treatment
None reported
(18%)
[4 in acupuncture group
& 6 in control]
4 lost during follow-up
(7.7%)
[3 in acupuncture group
& 1 in control]
Follow-up: 12 weeks
Blinding: reported as
being “applied
successfully”
Relevant
characteristics: Mean
age: 70.3yrs
[acupuncture], 72.2yrs
[control]
Sex: 75% women
[acupuncture], 63%
[control] Stage of
disease: not reported
Co-morbidity: not
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
73
reported
Secondary care
Study type: RCT
Quality: SIGN 1-
Comments: Small study; possible confounders not reported; co-intervention not reported clearly; no controls of therapist behaviour e.g. time spent,
communication; high drop-out rate; drop-outs may be different from completers i.e. KSS function score lower
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
74
PAIN
Reference and study
Studies
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
Hopton A, MacPherson N= 8 systematic
Intervention: Acupuncture Pain
Knee pain only
“The meta-analyses of
H. Acupuncture for
reviews
all recent systematic
chronic pain: is
reviews of acupuncture
acupuncture more than
for the most commonly
Comparison: “Sham”
an effective placebo? A
Kwon 2006
occurring chronic pain
See table below for
acupuncture (variable
systematic review of
conditions show that
more details
methods
15)
• Short-term
pooled data from meta-
• N=2 studies (264
there is consistent
analyses. Pain pract
subjects)
evidence that
2010;10(2):94-102.
• SMD = 0.24, 95% acupuncture is more
Inclusion: systematic
Length of treatment: for
CI: 0.01 to 0.47
effective than sham
reviews of acupuncture this review, defined as:
acupuncture for chronic
and chronic pain (knee,
osteoarthritis of the
UK
back, head) in English
Short-term = <3 months
Bjordal 2007
knee and headache in
with meta-analyses and
both the short term and
Long-term = ≥3 months
statistically pooled data
All short-term
longer term.”
Studies included:
Manual acupuncture
Furlan 2005;
Manheimer 2005; Kwon
No co-interventions
Exclusion: reviews of
• N=4 studies (746
“However, the results
2006; Bjordal 2007;
reported
shoulder, neck, elbow
subjects)
for back pain are
Manheimer 2007; White or leg pain, myofascial
• WMD = 1.3, 95%
mixed.”
2007; Davis 2008; Sun
trigger point pain,
CI: -2.7 to 4.7
2008
chronic pain from RA,
Electroacupuncture
circulatory disorders,
• N=3 studies (242
Reviewer’s conclusion:
cancer or other
subjects)
terminal illness;
• WMD = 21.9,
Overall, the evidence
injection of substances
95% CI: 17.3 to
from 4 good quality
alone e.g. bee venom
25.3
systematic reviews
show that acupuncture
reduces pain compared
15 including superficial insertion of needles at inappropriate sites and the use of blunt devices to apply pressure without penetration of skin
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
75
Databases: Medline,
Manheimer 2007
to ‘sham’ acupuncture
Allied &
both in the short- and
Complementary
Short-term
long-term [NB: except
Medicine database,
•
for the manual
N=6
(1636
Cochrane library, Web
acupuncture ‘arm’ of
subjects)
of Science, authors’
•
the Bjordal study].
SMD = 0.35, 95%
database and
CI: 0.15 to 0.55
reference list (2005-
Long-term
2008).
However, the effect
• N=3
(1304
size is small with lower
subjects)
confidence limits near
Methodological
• SMD = 0.13, 95% zero.
assessment: based on
CI: 0.01 to 0.24
14 questions derived
from the Oxman and
White 2007
Guyatt index and the
AMSTAR tool
Short-term
• N=5
(1334
subjects)
• WMD = 1.54,
No pooling of results
95% CI 0.49 to
from individual
2.60
systematic reviews
Long-term
• N=3
(1178
subjects)
• WMD = 0.54,
95% CI 0.05 to
1.04
Study type: Systematic review of systematic reviews
Quality: 1++
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
76
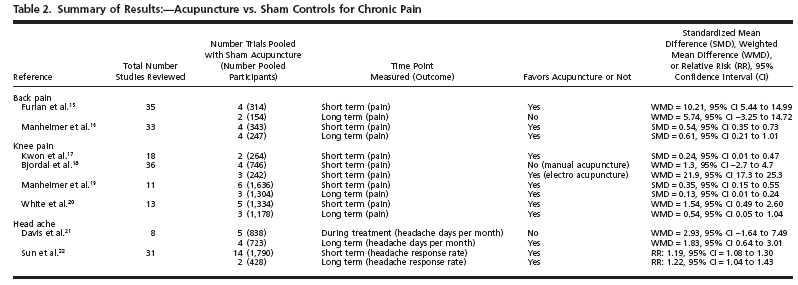 Comments:
Comments: Selected reviews that contained pooled data for meta-analyses from
high-quality trials that compare sham and true acupuncture for specific,
common pain conditions. Well conducted search and methodological assessment. Qualitative analysis of results appropriate. Each SR formally assessed the
internal validity of each study, applied strict inclusion & exclusion criteria, and tested for heterogeneity. Three of the 4 knee studies conducted a sensitivity
analysis and considered publication bias.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
77
Reference and study
Studies
Intervention/comparison
Outcome measure
Results/effect size
Conclusions
design
Madsen MV, Gotzsche
N=13 studies (3025
Intervention: acupuncture
Pain
Pooled results
“We found a small
PC, Hrobjartsson A.
subjects)
analgesic effect of
Acupuncture treatment
acupuncture that
for pain: systematic
seems to lack clinical
Acupuncture vs.
review of randomised
Length of treatment: 1
relevance and cannot
placebo acupuncture
clinical trials with
Inclusion criteria: all
day to 12 weeks
be clearly distinguished
(see fig 1 below):
acupuncture, placebo
trials labelled
from bias. Whether
acupuncture, and no
“acupuncture”; any
needling at
acupuncture groups.
placebo interventions
Comparison: both a
acupuncture points, or
Bmj 2009;338:a3115.
used by authors e.g.
SMD = -0.17
at any site, reduces
non-penetrating
placebo acupuncture and
a no acupuncture control
pain independently of
needles, insertion into
(95%CI: -0.26 to -0.08)
the psychological
non-acupuncture
group
impact of the treatment
Denmark
points; pain measured
13 trials*; 3025
ritual is unclear.”
by VAS or another
subjects
scale; two control
Co-interventions: all
groups (placebo and no
I2 = 36%
Included studies:
patients were supplied
acupuncture)
Reviewer’s
Melchart 2005; Linde
with standard care which
Funnel plot:
conclusions: Both
2005; Lin 2002; Sprott
was analgesics in 13 trials
symmetrical with clear
meta-analyses show a
1993; Fanti 2003;
and physiotherapy in 5
peak (data not
statistically significant
Wang 1997; Witt 2005;
Exclusion criteria:
reported)
benefit with regards to
Scharf 2006; Foster
TENS, manual
pain and moderate
2007; Molsberger 2002; acupressure; different
degree of
Brinkhaus 2006;
co-interventions in each
*one trial excluded as
heterogeneity. Whether
Leibing 2002; Kotani
group
an outlier [Kotani 2001] this effect is clinically
2001
i.e. % weight = 0
significant is debatable,
however, if it reflects a
Databases: Cochrane
true effect then it is
Relevant to report: Witt
library, Medline,
small.
Placebo acupuncture
2005 (OA knee); Scarf
EMBASE, Biological
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
78
2006 (OA knee); Foster Abstracts, and PsycLit
vs. no acupuncture
2007 (OA knee)
(see fig 2 below)
Assessment of bias:
adequate allocation
SMD = -0.42
concealment; patients
were blinded; drop-outs
(95%CI: -0.60 to -0.23)
<15% [if all 3 present
12 trials; 3025 subjects
then low risk of bias];
funnel plot to assess
I2 = 66%
small sample size bias
Funnel plot: broad peak
as large trials reported
both large and small
Meta-analysis
effects of placebo;
small trials tended to
report small effects
Fixed or variable
effects: “used a random
effects model if
Individual results (All
heterogeneity
OA knee)
existed (P<0.10) and a
Acupuncture vs.
fixed effect model
placebo acupuncture
otherwise.”
Witt 2005
-0.52 (-0.80 to -0.23)
Scharf 2006
-0.13 (-0.28 to 0.02)
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
79
Foster 2007
-1.66 (-2.34 to -0.98)
Placebo acupuncture
vs. no acupuncture
Witt 2005
-0.68 (-1.02 to -0.34)
Scharf 2006
-0.42 (-0.58 to -0.27)
Foster 2007
-0.21 (-0.47 to 0.06)
Study type: Systematic review with meta-analysis
Quality: SIGN 1-
Comments: Due to moderate levels of statistical heterogeneity i.e. I2 = 25-75%, probably not appropriate to conduct a meta-analysis. In addition, considerable
heterogeneity is present in the populations, treatments and outcome measures. The results need to be interpreted in this light.
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
80
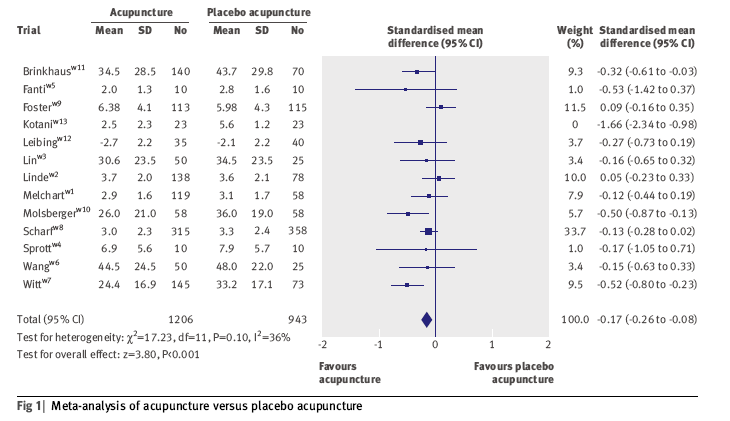
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
81
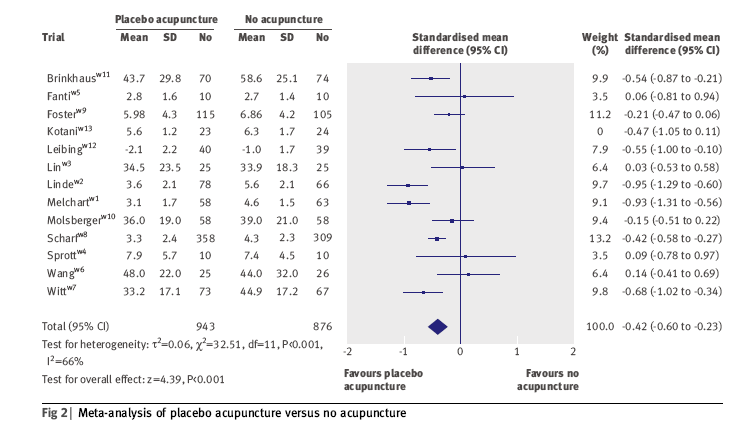
A c c i d e n t C o m p e n s a t i o n C o r p o r a t i o n
Page
82