

ACC
TREATMENT
PROVIDER
HANDBOOK
This is a living document and will be updated as required
link to page 4 link to page 4 link to page 5 link to page 6 link to page 7 link to page 7 link to page 8 link to page 9 link to page 11 link to page 13 link to page 14 link to page 18 link to page 22 link to page 23 link to page 25 link to page 25 link to page 25 link to page 26 link to page 29 link to page 31 link to page 31 link to page 33 link to page 34 link to page 37 link to page 37 link to page 41 link to page 42 link to page 42 link to page 43 link to page 44 link to page 48 link to page 49 link to page 51 link to page 54 link to page 58 link to page 59 link to page 63 link to page 63 link to page 64 link to page 67
ACC Treatment Provider Handbook 2016
Contents
1. Overview ...................................................................................................................... 4
Welcome....................................................................................................................... 4
How ACC cover works at a glance ............................................................................... 5
Key ACC contacts for treatment providers ................................................................... 6
2. How the Scheme works and working with us .......................................................... 7
About the ACC Scheme ............................................................................................... 7
Your partnership with ACC ........................................................................................... 8
What ACC covers ......................................................................................................... 9
Who ACC covers ........................................................................................................ 11
Cultural services ......................................................................................................... 13
Treatment and rehabilitation entitlements – overview ................................................. 14
How ACC pays ........................................................................................................... 18
Privacy ........................................................................................................................ 22
Health, safety and security ......................................................................................... 23
3. Supporting quality .................................................................................................... 25
Resources for providers and clients ........................................................................... 25
Research .................................................................................................................... 25
Clinical records ........................................................................................................... 26
Monitoring providers and fraud control ....................................................................... 29
4. Provider registration ................................................................................................ 31
Registering to become an ACC provider .................................................................... 31
Individual registration .................................................................................................. 33
Counsellor registration ................................................................................................ 34
5. Lodging claims ......................................................................................................... 37
Lodging a claim with ACC or an Accredited Employer ............................................... 37
Lodging Accredited Employer claims .......................................................................... 41
6. Treatment .................................................................................................................. 42
Acute treatment .......................................................................................................... 42
Nursing services ......................................................................................................... 43
Requesting further treatment ...................................................................................... 44
Adding or changing a diagnosis .................................................................................. 48
Work-related gradual process, disease or infection .................................................... 49
Treatment injury .......................................................................................................... 51
Mental injuries, sensitive claims and counselling ........................................................ 54
Dealing with challenging behaviour ............................................................................ 58
Pharmaceuticals ......................................................................................................... 59
7. Rehabilitation ............................................................................................................ 63
ew
Work and rehabilitation ............................................................................................... 63
Rehabilitation and you ................................................................................................ 64
erviv
Medical certificates (ACC18s) .................................................................................... 67
O
link to page 70 link to page 73 link to page 78 link to page 78 link to page 79 link to page 81 link to page 82 link to page 83 link to page 85 link to page 88 link to page 89 link to page 90 link to page 92 link to page 92 link to page 92 link to page 93 link to page 95 link to page 96 link to page 98 link to page 98 link to page 99 link to page 101 link to page 103 link to page 108 link to page 110 link to page 112 link to page 115 link to page 115 link to page 115
ACC Treatment Provider Handbook 2016
Sustained return to work ............................................................................................. 70
Referral and rehabilitation services ............................................................................ 73
8. Invoicing and payments ........................................................................................... 78
Our legislation and policies ......................................................................................... 78
Consultations/Visits .................................................................................................... 79
Medical practitioners’ treatment costs ........................................................................ 81
Nurses’ treatment costs .............................................................................................. 82
Joint medical practitioner and nurse treatment costs .................................................. 83
Specified treatment providers ..................................................................................... 85
Payment for counsellors ............................................................................................. 88
Services and reports ................................................................................................... 89
Invoicing correctly ....................................................................................................... 90
9. Working electronically with ACC ............................................................................. 92
Digital certificates ....................................................................................................... 92
Online claim lodgement: eLodgement ........................................................................ 92
Electronic invoicing: eSchedule .................................................................................. 93
Online eBusiness Gateway queries ............................................................................ 95
Working online FAQs .................................................................................................. 96
10. Consultation/Visit and procedure costs and codes .............................................. 98
Guide to invoicing for medical practitioners and nurses ............................................. 98
Burns and abrasions ................................................................................................... 99
Dislocations .............................................................................................................. 101
Fractures .................................................................................................................. 103
Miscellaneous ........................................................................................................... 108
Open wounds ........................................................................................................... 110
Soft tissue injuries .................................................................................................... 112
11. Glossary .................................................................................................................. 115
Introduction ............................................................................................................... 115
Definitions ................................................................................................................. 115
While ACC has endeavoured to see that it’s correct, the legal information contained in this
document is a summary only. For any legal purpose, see the applicable legislation and
regulations.
ew
ervivO
link to page 6
ACC Treatment Provider Handbook 2016
1.
Overview
Welcome
ACC’s role and our partnership with you
ACC’s role is to ensure that people in New Zealand receive the rehabilitation they need to
return to work or everyday life after injury.
Of course this isn’t a role that we perform alone, but one that we carry out in partnership
with you and other health professionals who provide treatment and rehabilitation services.
It’s your expertise and dedication that are the main drivers of your patients’ recovery.
However, the funding and support available through ACC play an integral role in creating
successful rehabilitation outcomes. Our partnership is therefore an important one, and it’s
vital to the wellbeing of the clients we serve.
This handbook has been created to help us work together as effectively as possible in this
partnership. It gives you a thorough overview of what ACC is, how it works and, most
importantly, the processes that need to be followed to ensure we work together in the best
interests of our clients.
The handbook covers everything from your responsibilities as an ACC-registered
treatment provider to details on how to lodge claims, order ACC resources and invoice us
for your services. It also talks about the importance of our clients’ rights to privacy and
your role in this.
If you’re not familiar with any of the terms used in the handbook, please refer to the
Glossary. You can also get more information by calling one of our toll-free enquiry
numbers or sending us an email
(see our contact details), or visiting ou
r website.
I trust you’ll find the handbook both helpful and easy to use, and I wish you well as we
begin this important partnership together.
Scott Pickering
Chief Executive
ACC
ew
ervivO
Accident Compensation Corporation
Page 4 of 128
ACC Treatment Provider Handbook 2016
How ACC cover works at a glance
g
n
m
i
i
a
Injured person visits
Injured person & provider or hospital
g
l
d
c
treatment provider or hospital
complete & lodge ACC45 Injury Claim form
o
e
L
ht
ACC receives claim & decides on cover
Decisions for specialised claims are referred to the:
• Gradual Process team
re
• Treatment Injury Centre
v
o
• Sensitive Claims Unit
c
• Dental team
g
n
• Hearing Loss team
i
m
• Accidental Death team
rifno
Cover is declined:
C
see review and appeal process,
or consider other care options
Cover is accepted
Simple claims
Low-complexity
High-complexity
(medical fees only)
(managed claim)
(managed claim)
im
Provider helps client recover
Client is supported by:
e cla
ACC partial reimbursement
Client is supported
• ACC case manager, or
th
g
of medical costs
by ACC case
• national serious injury
coordinator
in
coordinator
g
a
n
a
M
Provider helps client recover
Treatment and/or rehabilitation can include:
s
f
t
o
n
• acute treatment • Public Health Acute Services • elective surgery
e
e
m
• pharmaceuticals • imaging • transport • weekly compensation
p
o
el
• home-based rehabilitation • house or vehicle modifications
c
ti
S
t
• rehabilitation programmes (e.g. Stay at Work, social rehabilitation)
n
e
ACC may review ongoing cover and/or entitlements at any time
ew
ervivO
Accident Compensation Corporation
Page 5 of 128
ACC Treatment Provider Handbook 2016
Key ACC contacts for treatment providers
Provider Contact Centre
0800 222 070
[email address]
Client Helpline
0800 101 996
[email address]
Urgent home help (fax
Hamilton: 0800 222 891
Christchurch: 0800 222 359
numbers during ACC
Wellington: 0800 181 306
Dunedin: 0800 633 632
office hours)
Provider eBusiness
0800 222 994 option 1
[email address]
Support
Provider Registration
0800 222 070
[email address]
04 560 5213 (fax)
ACC, PO Box 30823
Lower Hutt 5040
Fraud Helpline
0800 222 372
[email address]
(0508 ACC FRAUD)
ACC, PO Box 1426,
ACC online reporting fraud
Wellington 6140
portal
Medical Fees units for invoices, schedules, ACC32
[email address]
treatment requests
Waikato Mail Centre
North: for regions north of New Plymouth, Gisborne and
Taupo
PO Box 952, Hamilton 3240
Medical Fees units for invoices, schedules, ACC32
[email address]
treatment requests
Elective Service Centre
South: for regions south of New Plymouth, Gisborne and
the South Island
PO Box 408, Dunedin 9054
Stationery Order Line (forms and brochures)
0800 802 444
Dental stationery
0800 226 440
Sensitive Claims Unit (sexual assault)
0800 735 566 option 1
Treatment Injury Centre
0800 735 566
Health procurement
(for service contracts)
0800 400 503
ACC website
www.acc.co.nz
ew
ervivO
Accident Compensation Corporation
Page 6 of 128
link to page 115 link to page 14
ACC Treatment Provider Handbook 2016
2.
How the Scheme works and
working with us
About the ACC Scheme
The ACC Scheme provides comprehensive, 24-hour, no-fault cover for all New Zealand
citizens, residents and temporary visitors who sustain certain types of personal injury in
New Zealand, generally those resulting from accidents. The Scheme is mandated by law,
in particular by the
Accident Compensation Act 2001 (the AC Act).
ACC is responsible for:
helping to prevent the circumstances that lead to injuries at work, at home, during
sport and recreation, and on the road
providing cover for personal injuries, no matter who’s at fault
reducing the physical, emotional and social impacts of people’s injuries by funding
timely treatment and rehabilitation that gets them back to work or independence as
safely and quickly as possible
minimising personal financial loss by paying contributions to treatment costs, paying
lump sum compensation and providing weekly compensation to injured people who
can’t work because of their injuries.
This handbook will help you work within the parameters of the Scheme and understand the
legislation and regulations that govern what we do. The
Glossary explains the terms we
use in our policies and procedures for claims and treatment, and with providers. We
haven’t set out everything here and ask that, if in doubt and for legal purposes, you refer to
our governing
legislation and regulations that apply.
th us
ACC’s governing legislation
The
AC Act is ACC’s governing legislation. It sets out what we’re able to cover and
ng wi
ensures that our help to clients is of the required quality.
rki
ACC’s policy requirements
ACC has a number of policies and procedures to help us deliver the outcomes required by
our legislation and ensure appropriate treatment and rehabilitation for our clients.
and wo
Our policies and procedures include:
works
promoting current treatment protocols, guidelines and evidence-based practice
encouraging providers to stay up to date with the latest developments in ACC policy
requiring providers’ clinical records to be of a standard acceptable to their relevant
heme
practitioner bodies and/or the Health Practitioners Competence Assurance Act 2003
c
(HPCA Act)
expecting providers to deliver services that are culturally responsive to the needs of
Māori and that recognise the Treaty of Waitangi by taking into account the social,
economic and political values of Māori (see
Services to Māori)
promoting the
Guidelines on Māori Cultural Competencies for Providers as a best-
How the S
practice model when working with Māori
monitoring appropriate outcomes for Māori
Accident Compensation Corporation
Page 7 of 128
ACC Treatment Provider Handbook 2016
requiring providers to deliver services in ways that are culturally appropriate and
responsive for Pacific, Asian and other ethnic groups
monitoring health care services
assessing provider claims, both random and targeted
investigating any concerns about the need for treatments, or the appropriate number,
length or quality of treatments
taking legal action if dishonest claims are made
recovering any funding for claims that are charged for inappropriately.
Legislative and policy requirements for providers
When we ask providers to assist in the treatment of clients we’re guided by three things:
1. Legislation and policy
2. Standards set by professional bodies
3. Major health sector frameworks such as the
HPCA Act. The HPCA Act protects the
public’s health and safety by ensuring the competence of health practitioners for the
duration of their professional lives. Having one legislative framework allows for
consistent procedures and terminology across the many professions now regulated
by the HPCA Act.
For more information, see t
he HPCA Act online or the
Ministry of Health commentary on
the Act.
Your partnership with ACC
Your role in our partnership
We work with injured people and their families/whānau in an extended partnership with
you, our treatment providers, as well as other health sector professionals, employers and
supporting groups.
Some of you will have occasional contact with patients who become ACC clients, while
ng with us
others of you may work with our clients daily.
rki
As a health services provider seeking funding to treat clients with ACC-covered injuries,
you’ll have certain responsibilities. These include:
and wo
complying with the
AC Act, our policies and procedures and your professional
sk
standards when treating and making claims for ACC clients
providing our clients with clinical treatment that meets the requirements of best
practice and the standards of your professional body
wor
providing treatment and advice that assist ACC clients to return to work and/or
independence
heme
following the ACC
treatment profiles
maintaining appropriate
clinical records
invoicing appropriately, especially if you are registered with more than one
professional body.
ow the Sc
We encourage you to get to know us. Feel free to make personal contact with us locally,
H
e.g. through your loca
l Supplier Manager or you
r local branch.
Accident Compensation Corporation
Page 8 of 128
link to page 9 link to page 10
ACC Treatment Provider Handbook 2016
Supplier Managers – key contacts
Supplier Managers work in the community with our contracted and non-contracted
suppliers in the following ways:
providing education and support to treatment providers
helping treatment providers work within ACC’s policies and processes
managing performance as well as relationships.
For more information about Supplier Managers, see
Supplier Manager contact details.
What ACC covers
ACC cover
ACC receives about 1.9 million claims a year fo
r personal injuries including
mental injuries.
The most common injuries we cover are caused by:
accidents at work, at home and on the road
work-related gradual processes, diseases or infections
treatment injuries
sexual assault or abuse.
Advice on cover criteria
If you’re unsure about advising patients on possible ACC cover, phone the Provider
Contact Centre on
0800 222 070 or email
[email address]. Alternatively, ask your
patient to get in touch through the Client Helpline on
0800 101 996 or by emailing
[email address].
th us
Personal injuries
Personal injuries cover:
ng wi
physical injuries (including fatal injuries), which typically include:
rki
o wounds
o lacerations
o sprains
o strains
and wo
o fractures
o amputations
o dislocations
works
o some dental injuries
work-related gradual process injuries, diseases and infections, which cover a range
of physical deteriorations caused over time by work or the work environment.
heme
Examples include:
c
o asbestosis
o work-related hearing loss
treatment injuries, i.e. physical injuries sustained while receiving treatment from
registered health practitioners.
How the S
Accident Compensation Corporation
Page 9 of 128
link to page 115 link to page 54
ACC Treatment Provider Handbook 2016
Mental injuries
Cover for a mental injury is provided if it was caused by:
a physical injury
a specific event in the workplace
sexual assault or abuse.
Mental injuries caused by physical injuries
Some mental injuries are caused by physical injuries already covered by claims with ACC.
If a person suffers a mental injury of this kind that can be covered by ACC, it’s treated as
part of the original physical injury claim, with the same injury date as the physical injury.
Mental injuries caused by witnessing a traumatic event at work
ACC provides cover for mental injuries caused by traumatic events in the workplace if
certain conditions set out in the
AC Act are met.
Mental injuries caused by sexual assault or abuse
Mental injuries arising from this type of criminal offence are called sensitive claims. For
more information, see
Schedule 3 of the AC Act 2001 or the
Glossary.
Mental injury is a complex area and it can sometimes be difficult to determine cover.
Decisions are made in each case on the basis of diagnosis and evidence provided by a
psychiatrist or psychologist in their report to us. In order to receive cover, the information
provided in the report needs to prove that the patient’s physical injury, the traumatic event
at work or the sexual assault or abuse was a direct and significant cause of the mental
injury.
For more details about the assessments used to determine treatment options for mental
th us
injuries, see
Mental injuries, sensitive claims and counselling.
ng wi
What ACC is unable to cover
rki
ACC isn’t able to cover:
injuries to teeth arising from their natural use, e.g. biting a boiled sweet
cardiovascular or cerebrovascular diseases, unless they’re a result of treatment
and wo
injuries or work injuries involving effort that is ‘abnormally applied’ or ‘excessively
intense’
gradual process injuries that are not caused wholly or substantially by work-related
works
gradual processes, diseases or infections
personal injuries caused wholly or substantially by the ageing process (if medical
opinion confirms that the injuries wouldn’t have happened without the ageing process)
heme
personal injuries caused by illness
c
the emotional effects of injuries such as hurt feelings, stress or loss of enjoyment,
unless they result from mental injuries
injuries caused by coughing or sneezing, or other internal forces.
How the S
Accident Compensation Corporation
Page 10 of 128
link to page 125 link to page 119 link to page 13
ACC Treatment Provider Handbook 2016
Limitations to entitlements
In some cases a person’s injury will be covered but we’ll be unable to provide some
entitlements, e.g. in some instances o
f self-inflicted injury o
r criminal disentitlement. If
you’re treating a patient with a claim of this nature, please encourage them to contact the
Client Helpline as soon as possible on
0800 101 996.
Who ACC covers
Three categories of people are covered by ACC:
all New Zealanders, 24 hours a day, whether or not they’re earning an income
New Zealanders who are injured overseas (with certain criteria)
visitors to New Zealand (with certain criteria).
Code of ACC Claimants’ Rights
All ACC claims are managed under the Code of ACC Claimants’ Rights. These rights are
covered in the pamphle
t ACC2393 Working together to resolve issues.
The pamphlet explains what clients can do if they’re unhappy with the service they receive
and outlines what they can expect from ACC in their dealings with us.
For more information, see
Code of ACC Claimants’ Rights: respect, culture and values.
Cover for Kiwis injured overseas
New Zealanders may also be able to receive support
back in New Zealand if they were injured overseas. They
just need to meet ACC
’s ‘ordinarily resident’ criteria.
th us
Eligible New Zealanders may also receive payment for
overseas treatment if they’ve suffered work-related
personal injuries overseas. ACC isn’t able to reimburse
ng wi
New Zealand providers for treatment given overseas (e.g.
rki
when accompanying sports tours). Providers can only
receive payments when they’re working in New Zealand.
See the information shee
t ACC593 Getting help if you’ve
and wo
been injured while travelling overseas. You can order this
online or by phoning the Stationery Order Line on
0800
802 444 option 0, and quoting the ACC number in the title
(ACC593).
works
hemec
How the S
Accident Compensation Corporation
Page 11 of 128
link to page 123 link to page 123
ACC Treatment Provider Handbook 2016
Cover for visitors to New Zealand
Visitors to New Zealand are covered fo
r personal
injuries, and ACC can help to pay for treatment while
they’re in New Zealand once their claims have been
accepted. We’re not able to reimburse visitors for
rehabilitation or treatment costs in their home countries,
or for loss of income.
The information shee
t ACC592 Getting help if you’re
injured visiting our country can be ordered
online or by
phoning the Stationery Order Line on
0800 802 444 option 0, and quoting the ACC number in the title
(ACC592).
The brochure is also available in Māori, Samoan,
Tongan, Cook Island Māori, Chinese, Hindi and Korean.
You can select the brochure in the language you want at
our
website.
Cover for Kiwis in New Zealand
The information shee
t ACC583 Help for injuries explains
for clients how the claim process works in New Zealand.
You can order th
is online or by phoning the Stationery
Order Line on
0800 802 444 option 0, and quoting the
ACC number in the title (ACC583).
th us
ng wi
rki
and wo
works
Terminology: clients and patients
heme
ACC uses the word ‘clients’ to describe patients whose claims have been accepted for
c
cover and have therefore become ACC clients. The term is used throughout this handbook
to reinforce the importance of lodging claims in order to access entitlements for people.
We recognise, however, that you may prefer to use alternative terms.
How the S
Accident Compensation Corporation
Page 12 of 128
ACC Treatment Provider Handbook 2016
Cultural services
The Cultural Services team
ACC’s Cultural Services team is a group of cultural case advisors including Pae Ᾱrahi
(Māori cultural case advisors), Pacific cultural case advisors and Asian cultural case
advisors. You can contact these advisors through case owners and other frontline staff in
ACC.
Code of ACC Claimants’ Rights: respect, culture and values
All ACC claims are managed under the Code of ACC Claimants’ Rights.
The pamphlet
ACC2393 Working together to resolve issues explains what clients can do if
they’re unhappy with the service they receive and outlines what they can expect from ACC
in their dealings with us.
You can order th
is online or by phoning the Stationery Order Line on
0800 802 444 option
0, and quoting the ACC number in the title (ACC2393).
For more information, see the
legislation covering ACC claimants’ rights.
Māori cultural guidelines
The ACC booklet
ACC1625 Guidelines on
Māori Cultural Competencies for Providers
can be viewed online. It was created to help
you give appropriate advice, care and
treatment to Māori clients.
You can order th
is online or by phoning the
th us
Stationery Order Line on
0800 802 444 option 0, and quoting the ACC number in
the title (ACC1625).
ng wi
rki
The booklet comes with a DVD and is
available as:
an A4-size document with the code
and wo
number ACC1625, or
a shorter version with the code number
ACC1626.
works
Please quote the ACC number and your
provider number when ordering.
hemec
Treaty of Waitangi
In line with our Treaty of Waitangi obligations for Māori and recognising the cultural and
ethnic diversity of New Zealand, ACC obtains input from Cultural Services for appropriate
How the S
service delivery and to ensure these clients have positive experiences of our service.
Accident Compensation Corporation
Page 13 of 128
link to page 63 link to page 18
ACC Treatment Provider Handbook 2016
Services to Māori
ACC is committed to ensuring that appropriate services are delivered to all who meet our
entitlement criteria. However, we know that Māori make significantly fewer claims than
New Zealand Europeans.
You can play a key role in helping to address disparities. For example, if you’re filling out
the
ACC24 Application for ACC Health Provider Registration form, you can indicate both
your capacity to offer services in a range of languages and your ability to work respectfully
with clients whose cultural backgrounds might make extra demands of providers. This lets
us offer your treatment services to clients in need of such providers.
Alternatively, you can contact the ACC Provider Registration team by phoning
0800 222
070, emailing
[email address] or writing to ACC Provider Registration, PO Box
30823, Lower Hutt 5040.
For our contracted services, ACC
’s Standard Terms and Conditions include clauses that
outline suppliers’ obligations to provide services that comply with the Treaty of Waitangi
and will meet the cultural needs of Māori, Pacific and Asian clients and clients of other
ethnicities.
Treatment and rehabilitation entitlements – overview
Managing rehabilitation
The aim of rehabilitation is to help restore a client’s pre-injury health, independence and
participation in society as much as possible. Returning injured people to work and
independence is ACC’s role and we engage with a range of providers to enable
rehabilitation.
If a client’s rehabilitation requirements are complex, their claim is managed in a branch by
th us
a case owner who has access to a panel of experts. Typically these will be a clinical
advisor, a branch psychologist, a technical advisor and a team manager with a
ng wi
rehabilitation focus. These experts will help the case owner to direct rehabilitation.
rki
For more information on rehabilitation, se
e Rehabilitation.
Managing treatment
and wo
Treatment includes:
physical rehabilitation
works
cognitive rehabilitation
examinations or assessments for the purpose of providing a certificate to ACC (such
as a medical certificate for time off work, or assessments to help determine treatment
heme
plans).
c
ACC supports clients’ treatment by contributing to:
client consultations/visits and procedures delivered by treatment providers, according
to the
Accident Compensation (Liability to Pay or Contribute to Cost of Treatment)
How the S
Regulations 2003 and amendments (the
Regulations). See a
lso How ACC pays
treatment services such as elective surgery and hand therapy, usually under contract
Accident Compensation Corporation
Page 14 of 128
link to page 59 link to page 67
ACC Treatment Provider Handbook 2016
pharmaceuticals prescribed for ACC-covered injuries (see also
Pharmaceuticals) bulk funding to the Crown for emergency department, acute inpatient and follow-up
medical outpatient services, and some associated ancillary services.
Increasingly, multiple interventions are used alongside treatment, including ‘non-clinical’
tools such as exercise programmes and education for clients.
We encourage you to participate in early planning and discussions with clients, and may
also pay for you to attend case conferences where multiple parties, including
families/whānau and employers, can be represented.
What help clients can receive
ACC clients can receive a range of treatment and rehabilitation services and may also be
eligible for compensation. The
AC Act forms the legislative base for most of ACC’s
activities and outlines what clients with approved cover may be entitled to receive.
This includes:
weekly compensation while a client is unable to work
lump sum compensation for permanent impairment
support for survivors in the event of accidental death
rehabilitation, which covers:
o treatment
o social rehabilitation (support in everyday activities)
o specialised rehabilitation
o vocational rehabilitation (support in maintaining or obtaining employment)
o pain management services
o associated ancillary services.
Details of these entitlements follow in the sections below.
th us
Weekly compensation
ng wi
Clients may be eligible for compensation for lost earnings if they need to take time off work
rki
because of their injuries.
Only medical practitioners and nurse practitioners can certify time off work for ACC clients.
The exception is for the first week off work after a work-related personal injury. In this case
and wo
the client’s employer can nominate and pay a registered health professional, such as a
nurse, occupational therapist or physiotherapist, to complete the certificate.
For more information, see
Medical certificates (ACC18s).
works
Lump sum compensation
heme
Lump sum compensation is generally available for clients whose injuries lead to
c
permanent impairment. The type of compensation available is based on claim type.
You can get more information through the Provider Contact Centre on
0800 222 070 or by
emailing
[email address]. Your patient can get more information by calling the
Client Helpline on
0800 101 996.
How the S
Accident Compensation Corporation
Page 15 of 128
ACC Treatment Provider Handbook 2016
The information shee
t LSIAIS01 All about lump sum payments and independence
allowances also gives details on lump sum compensation calculation procedures.
Social rehabilitation
The aim of social rehabilitation is to help clients achieve as much independence as
possible. Social rehabilitation is available to support clients whose injuries have moderate
or significant impacts on their lives. It supports the clients’ rehabilitation through the
provision of:
home and community support services, e.g. home help, child care and attendant care
equipment based on the clients’ assessed needs, e.g. wheelchairs, shower stools and
walking frames
modifications to clients’ homes or vehicles
needs assessment services
post-acute rehabilitation delivered by district health boards (DHBs) and some trust
hospitals.
For details on the assessment criteria for social rehabilitation, see
Social rehabilitation
assessment.
Specialised rehabilitation
The aim of specialised rehabilitation is to help clients achieve the best possible outcomes
by providing early, intensive rehabilitation and community support. Specialised
rehabilitation is available to support clients whose injuries have significant long-term (or
lifelong) impacts on their lives. It supports the clients’ rehabilitation through services such
as:
‘training for independence’ programmes
community-based services
th us
disability support services
education support
ng wi
residential rehabilitation services
transition services.
rki
For details on specialised rehabilitation, see ACC’s
Contracts and services.
Vocational rehabilitation
and wo
Vocational rehabilitation is available to help clients recovering from significant injuries to
maintain or obtain work, or to regain vocational independence. Generally it’s best for
clients to stay in their pre-injury jobs where possible. Together with suppliers and
works
providers, we can help them to do this by:
heme
reviewing their working environment and discussing ways to help them do all or some
c
of their work tasks as their rehabilitation progresses
providing equipment to help them at work.
In some cases clients start in Stay at Work (SAW) programmes before they return to work
and while they’re rehabilitating. Employers are asked to take all practical steps to help
How the S
injured employees to rehabilitate, including when their injuries aren’t work related.
Accident Compensation Corporation
Page 16 of 128
link to page 63 link to page 76
ACC Treatment Provider Handbook 2016
We have a range of tools to help clients who are unable to return to their pre-injury jobs.
These include:
initial occupational assessments, which identify the types of work that may be suitable
for them
initial medical assessments, which identify whether those types of work are medically
sustainable and if any further rehabilitation is required
Work Readiness programmes, which include pre-employment preparation and/or
strengthening programmes and can include work trials.
Following rehabilitation, we may ask a client to have their vocational independence
assessed by an occupational assessor and a medical assessor. This is to ensure that the
full extent of rehabilitation has been provided and we’ve addressed any injury-related
barriers to employment or vocational independence. The assessments help to determine
whether the client can return to work full time or whether further alternative rehabilitation is
necessary.
For details on vocational rehabilitation se
e Work and rehabilitation.
Pain management services
Pain management services aim to reduce clients’ pain through exercise activities and
education. Early screening can determine when a client will need further assessments to
establish if they have an increased risk of disability.
A pain management programme works best for the client when the programme clearly and
specifically targets getting the client back to independence. This means:
the programme sets client-specific goals to restore independence for pre-injury
activities, e.g. vacuuming and getting in and out of a truck
the client can continue the programme once the formal supervision has finished, if
th us
they choose to do so
the client must be confident that there are no other reasons for their pain, i.e. red flags
have been dismissed.
ng wi
rki
ACC has a range of tools to help clients identify, manage and recover from pain. These
include:
Functional Reactivation Programme
and wo
Progressive Goal Attainment Programme
Pain Management Psychological Service
Pain Disability Prevention Programme
works
Comprehensive Pain Assessment
Activity Focus Programme
Multi-disciplinary Persistent Pain Programme
hemec
Interventional Pain Management
For details on vocational rehabilitation, see
Pain management services.
Accidental death – help for families/whānau
How the S
When we accept a claim for entitlements arising from fatal injuries, we can help with:
Accident Compensation Corporation
Page 17 of 128
link to page 42 link to page 78 link to page 92
ACC Treatment Provider Handbook 2016
a funeral grant (to the maximum amount set by the
Regulations) a grant (for the spouse, children and other dependants)
weekly compensation for the dependants if the deceased person was in employment
at the time they died (the spouse can apply to convert this into a lump sum)
payments to cover child care for the deceased’s children.
Ancillary services
Ancillary services help clients to access treatment and rehabilitation. They include:
pharmaceuticals and laboratory services
emergency transport by ambulance, and transport to treatment
transport to and from certain types of vocational and social rehabilitation
travel for support people in specific situations
help with accommodation for clients and/or their support people.
When a client’s care is being funded under the
Public Health Acute Services (PHAS)
agreement, the DHB provides their ancillary services.
Helping clients understand what help they can receive
Our clients often ask their treatment providers about
what help they can get from ACC and how ACC works.
While we don’t expect treatment providers to understand
all the ins and outs of the Scheme, the brochure
ACC2399 Getting help after an injury covers the basics
of how we can help.
You can order free
online or by phoning the Stationery
Order Line on
0800 802 444 option 0, and quoting the
ACC number in the title (ACC2399).
th us
For detailed information you can direct clients to
www.acc.co.nz. Under ‘Making a claim’, they can click
ng wi
on What support can I get? They can also call the Client
rki
Helpline on
0800 101 996.
If you have any questions about entitlements, please
contact the Provider Contact Centre on
0800 222 070 or
and wo
email
[email address].
works
How ACC pays
heme
Criteria for covering costs
c
ACC pays for, or contributes to, the costs of treating covered personal injuries. See also
Invoicing and payments and
Online claims lodgement: eLodgement.
ACC makes decisions according to the
AC Act and the
Regulations, which state that
treatment must:
How the S
Accident Compensation Corporation
Page 18 of 128
ACC Treatment Provider Handbook 2016
be necessary and appropriate
meet the quality required
be given the appropriate number of times, and ‘in person’
be given at the appropriate time and place
be reasonably required to facilitate treatment (for ancillary services)
normally be provided by your type of treatment provider, and you must be qualified to
provide that treatment
have prior approval (if required).
In deciding whether these points apply to a client’s treatment, the
AC Act says that ACC
must take into account:
the nature and severity of the injury
generally accepted treatment for the injury in New Zealand
other treatment options available in New Zealand for such an injury
the cost in New Zealand of both the generally accepted treatment and the other
options, compared with the benefit to the client of the treatment.
Requirements for providers seeking payment
Providers seeking payment from ACC for services or treatment must ensure that:
the services provided and invoiced for include clinical records that meet ACC’s
recommendations
their clinical records meet their professional bodies’ standards
their clinical records demonstrate that the treatments provided meet the legislative
requirements (listed above)
the treatments provided and the clinical records can withstand scrutiny through peer
review, an audit (medical or financial) or a medico-legal challenge
the dates of appointments are the same on the invoices as recorded in any clinical
th us
notes.
Our policy on treating yourself or your family
ng wi
rki
ACC agrees with the Medical Council of New Zealand, which states that “other than in
exceptional circumstances you shouldn’t provide medical care to yourself or anyone with
whom you have a close personal relationship”. ACC considers this to be relevant to all
types of treatment provider and includes the treatment of work colleagues.
and wo
We generally consider it unacceptable and unethical for providers to claim payments from
ACC for treating those who are close to them. In these cases we’ll only consider paying for
treatment in exceptional circumstances.
works
Exceptional circumstances include:
heme
acute treatment provided in an emergency situation where, in your reasonable
c
judgement, the need for treatment is urgent given the likely clinical effect on the
person of any delay in treatment
situations in rural areas where there is no other appropriately qualified treatment
provider available to give the required treatment.
How the S
We’re unable to fund:
Accident Compensation Corporation
Page 19 of 128
link to page 37 link to page 37 link to page 37
ACC Treatment Provider Handbook 2016
treatment provided in a non-emergency situation
emergency treatment that would ordinarily be provided by a family member who isn’t
a provider.
The provider claim lodgement framework
To enable us to verify claims lodged on behalf of patients, we’ve worked with professional
bodies to incorporate ‘scopes of practice’ into our frameworks.
The ‘provider claim lodgement framework’ covers various injury types. It refers to common
Read Codes to show those injuries for which a provider may complete an
ACC45 Injury
Claim form and provide initial treatment. If an injury is within a provider’s scope of practice
we can decide to cover it.
If an injury isn’t within a provider’s scope of practice (as defined in the provider claim
lodgement framework), the provider can give initial treatment and initiate the completion of
an ACC45 Injury Claim form. They must then refer the client to a medical practitioner for
confirmation of diagnosis before we can determine cover.
This means the patient will see two providers before their claim is considered. ACC will
pay for the consultation/visit to confirm the diagnosis, but won’t be able to pay for the initial
consultation/visit and any subsequent treatment until the diagnosis has been confirmed
and the claim accepted. The types of provider to which this rule applies include
acupuncturists, osteopaths and speech therapists.
For more information on lodging claims, see the online documents:
Provider claim lodgement framework
Lodge a claim electronically
Lodging a claim with ACC or an Accredited Employer.
th us
How ACC funds providers in training
ACC only pays for treatment given by qualified treatment providers who take full
ng wi
responsibility for the treatment provided to clients.
rki
If you’re a provider in training (e.g. an intern or a university or polytechnic student
undertaking practical work for study) we can offer funding provided you’re:
and wo
already a qualified practitioner undertaking further study
unqualified but have gained consent from the client and are supervised by a qualified
practitioner who:
o is personally present throughout the treatment delivery
works
o takes responsibility for assuring its standard.
Note: An important exception is that sexual abuse counselling must always be provided by
hemec
a fully qualified counsellor.
Three ways to provide services to ACC
the S
There are three ways to provide services to ACC:
How
service contracts
Accident Compensation Corporation
Page 20 of 128
link to page 79
ACC Treatment Provider Handbook 2016
Every ACC contract for services includes details of the invoicing and payment
arrangements that apply to those who sign it. Contract terms can differ from the
Regulations – when this happens the contracted terms take precedence over the
Regulations
payments under agreed costs
These comprise agreements between ACC and providers based on treatment costs.
If an ACC case owner requests services at an agreed cost, you’ll need to request a
seven-digit purchase order number from ACC. This needs to be included on every
invoice. For more information, phone the Provider Contact Centre on
0800 222 070 or
email
[email address]
Regulations. These comprise, for example, the:
o Accident Compensation (Liability to Pay or Contribute to Cost of Treatment)
Regulations 2003
o
Accident Compensation (Ancillary Services) Regulations 2002
o Injury Prevention, Rehabilitation, and Compensation (Public Health Acute
Services) Regulations 2002
o any later amendments.
Payments under the Regulations
The
Regulations cover a large number of treatment providers, including:
acupuncturists
audiologists
chiropractors
counsellors
dentists
hyperbaric oxygen treatment providers
medical practitioners
th us
nurses and nurse practitioners
occupational therapists
ng wi
osteopaths
rki
physiotherapists
podiatrists
radiologists
registered specialists
and wo
speech therapists.
ACC contributes to treatment costs at the rates/amounts specified in the Regulations. The
Regulations cover basic treatment provider costs, while the
Schedule of the Regulations
works
specifies amounts for treatments and procedures.
These include rates and amounts:
hemec
per consultation/visit, as long as you examined, assessed and/or treated the client in
person, for an injury or condition covered by ACC (for details see
Consultations/Visits)
per treatment/procedure given to a client during a consultation/visit as long as the
Schedule includes an amount for that treatment/procedure for your type of provider.
How the S
Accident Compensation Corporation
Page 21 of 128
link to page 85 link to page 98 link to page 98
ACC Treatment Provider Handbook 2016
Providers’ payment options
If you’re a ‘specified treatment provider’ (or ‘allied provider’) working under the Regulations
you have the choice of being paid on a per-treatment basis or on an hourly rate. Hourly
rates are specified in the
Regulations. For details see
Specified treatment providers.
Treatment/Procedure guide for medical practitioners and nurses
For guidance on items in the Regulations for medical practitioners and nurses, see
Guide
to invoicing for medical practitioners and nurses.
Privacy
We take privacy seriously
ACC deals with the personal and health information of a large number of people. We often
request that you provide us with information and sometimes you’ll need access to this
information to carry out services for ACC. It’s important that we each do our part and work
together to protect this information.
What to expect
If you have access to personal or health information we would like you to:
work with us in a transparent way
notify us of potential risks
notify us of breaches and near-misses
resolve issues as they arise
maintain a privacy register that includes breaches, near-misses and remedial action
plans.
th us
What do we mean by ‘breach’ and ‘near-miss’?
A
breach is when personal information is disclosed to an external party when it shouldn’t
ng wi
be, whether by error, mistake or without legal authority.
rki
A
near-miss is when you can identify something that would have led to a privacy breach
but didn’t because the information wasn’t disclosed.
Not only does maintaining a privacy register help us to meet the requirements of the
and wo
Privacy Act 1993 and
Health Information Privacy Code 1994, it also enables us to work
with an enhanced level of transparency on breaches and near-misses. To achieve a high
level of transparency we expect all providers to have effective preventive measures in
works
place to avoid breaches and near-misses.
If you have a privacy breach, contact your loca
l Supplier Manager, who will work with you,
hemec
or call the Provider Contact Centre on
0800 222 070, who will direct you to your local
Supplier Manager.
Obligations
Every organisation has obligations under the
Privacy Act 1993. When dealing with
How the S
personal information you need to ensure that you comply with the 12
information privacy
principles that cover the collection, handling and use of personal information, set out in the
Accident Compensation Corporation
Page 22 of 128
ACC Treatment Provider Handbook 2016
Act. The Act also requires every organisation to have a Privacy Officer to oversee its
compliance with the Act and investigate any complaints when they arise.
A privacy pack has been developed to help you manage the privacy of your clients’
personal information. It’s available from ou
r website and was developed with information
from the Office of the Privacy Commissioner.
Further information can be obtained by contacting the Office of the Privacy Commissioner
either a
t its website or through its helpline on 09 302 8655 (or
0800 803 909). You can
also refer to the privacy management section on ou
r website.
Health, safety and security
Keeping people safe and healthy at work
ACC fully supports the Government’s 2020 goal of a 25% reduction in serious harm and
fatalities in New Zealand workplaces. We want to be a responsible leader by
demonstrating our Safe Kiwis and Good Partner strategic directions with everyone with
whom we interact, including the health providers who deliver services on our behalf to our
clients.
The health and safety risks in each health service category will vary greatly, from low to
very high. We expect our providers to have appropriate health, safety and security
procedures and policies in place to keep staff and subcontractors’ staff safe and healthy.
ACC’s website provides guidance for businesses on managing hazards, training and
supervision and health and safety, including workplace safety programmes. If you require
more information, go to ou
r website. WorkSafe New Zealand also has resources available
on its
website.
To meet our responsibilities for health and safety, we need you to tell us about health and
th us
safety events, including close calls and personal threats that arise while you’re providing
services to us or our clients. We’ll work with you to protect others from harm by eliminating
ng wi
or minimising the risks wherever possible.
rki
What you need to do
If you provide services to ACC via a service contract or as payments under agreed costs
then you need to report incidents to us using the Health and Safety Incident Reporting
and wo
Procedure on ou
r website. We need to know about any of the following that occur while
you’re delivering services on our behalf:
works
notifiable events
close calls/near-misses
non-notifiable injuries
heme
personal or organisational threats.
c
This requirement does not apply if you provide services to ACC v
ia Regulations.
Obligations
How the S
The
Health and Safety at Work Act 2015 applies to nearly all businesses in New Zealand.
Accident Compensation Corporation
Page 23 of 128
ACC Treatment Provider Handbook 2016
To learn more about the new Act and your obligations, and to subscribe to receive
email
alerts, please visit the
WorkSafe website. You can also contact WorkSafe at
0800 030 040 or email
[email address].
Definitions
Notifiable event
Under the Health and Safety at Work Act, a notifiable event is:
the death of a person
a notifiable injury or illness, or
a notifiable incident
that arises from work.
Refer to the
legislation.
Notifiable incident An unplanned or uncontrolled incident in relation to a workplace
that exposes a worker or any other person to a serious risk to that
person’s health and safety arising from an immediate or imminent
exposure to one of the incidents listed in the legislation – for
example:
the fall or release from a height of any plant, substance or
thing
an implosion, explosion or fire
an electric shock.
Refer to the
legislation for a full list of notifiable incidents.
Notifiable injury
an injury or illness listed in the legislation that requires the
or illness
person to have immediate treatment (other than first aid), or
an injury or illness that requires admission to hospital for
immediate treatment, or
th us
an injury or illness that requires medical treatment within 48
hours, or
ng wi
any serious infection where the carrying out of work is a
rki
significant contributing factor as listed in the legislation, or
any other injury or illness declared to be notifiable by
regulations.
and wo
Refer to the
legislation.
Close call/near-
Any incident that could potentially have resulted in a notifiable
miss
event.
works
Personal threat
Any written or verbal threat made to a staff member either in
person or remotely, for example by telephone or email.
hemec
Organisational
Any written or verbal threat made to your organisation, for
threat
example a bomb threat or damage to the organisation’s property.
How the S
Accident Compensation Corporation
Page 24 of 128
ACC Treatment Provider Handbook 2016
3.
Supporting quality
Resources for providers and clients
Resources to help you
ACC produces a range of resources to inform, encourage and support the use of best
clinical practice. These are available on ou
r website. Although some of the information
may be dated, the page is under constant review and we encourage you to check it
regularly.
Resources include:
Case studies
Treatment injury case studies are produced by ACC’s Treatment Injury Centre to provide
health professionals with:
an overview of the factors leading to treatment injury
expert commentary on how similar injuries may be avoided in the future.
Feedback reports
ACC produces annual
National Service Reports that contain high-level data that can be
compared to individual practice data and used for professional discussion. The content is
developed using the Results Based Accountability framework, which measures how much
we’ve done, how well we’ve done it, and whether anyone is better off.
ACC reviews
ACC reviews summarise the latest best-practice injury management and rehabilitation
from a clinical perspective, drawing on recent available evidence and clinical guidelines.
The reviews are developed by clinical subject matter experts in conjunction with ACC staff
and relevant peer review groups.
Resources for clients
You can help your patients to understand their injuries by giving them information from the
Caring for your… leaflet series. This series gives clients tips on how to look after their
injuries.
These leaflets are available to order from our website through the
Publications section.
y ti
Research
ual
Research involvement
ACC invests in ongoing research as part of our commitment to ensuring the most
orting q
appropriate treatment and rehabilitation for clients. This is often done in collaboration with
partners in the broader clinical and health sectors.
Supp
Our Research team conducts research in-house and manages ACC-funded research that
is contracted to external agencies. We also work in partnership with other areas of the
Accident Compensation Corporation
Page 25 of 128
ACC Treatment Provider Handbook 2016
organisation where our research expertise is required for initiatives including consensus
guidelines, evidence-based health care (EBH), programme evaluation, customer insights
and innovations in treatment and rehabilitation.
Research advice
The Research team is committed to the principles of EBH. This enables a multifaceted
approach to inform decision-making and guide health purchasing and supports best
practice among treatment providers. The team’s objectives include:
developing impartial, evidence-informed purchasing recommendations to assist ACC
in making appropriate purchasing decisions
promoting best practice in injury management and rehabilitation
evaluating new ACC services and primary health care initiatives
consulting and collaborating with health care providers
seeking feedback from providers and other partners through surveys and market
research to analyse new and emerging issues that might affect ACC in the future.
Research partnerships
For purchasing recommendations the team uses internationally standardised EBH
methods to summarise and evaluate existing clinical research on effectiveness and safety.
In partnership with subject matter experts and a purchasing advisory group, the team
provides recommendations on whether the treatments, products or services in question
should be purchased by ACC. Recommendations are formed through the analysis of
research articles from peer-reviewed journals. These recommendations are then put
forward for ratification by the ACC Clinical Governance Committee before becoming
policy.
EBH reports written by the Research team can be found on ou
r website. The Considered
Judgement Forms (which facilitate the purchasing advisory group discussions) can also be
found there.
Clinical records
ACC’s emphasis on clinical records
Each of your clinical records should show the history you obtained, the examination you
undertook, how you formulated your diagnosis, and how you planned the client’s
treatment. Reviewing your records will help ACC and others to see how you reached your
conclusions.
y ti
It can be easy to forget details of a client’s presentation or what you said and did in the
consultation/visit. Good clinical note-taking can help you to review your practice and avoid
ual
uncertainties.
In the unlikely event of a complaint from or an adverse event for a client, good records
orting q
help to demonstrate your standard of care and document your decisions and advice. It’s
therefore vital that you keep full and accurate clinical records, for your own and the clients’
protection and support.
Supp
Accident Compensation Corporation
Page 26 of 128
link to page 27 link to page 27 link to page 44 link to page 44
ACC Treatment Provider Handbook 2016
All professional bodies endorse the responsibility of professionals to regard record-keeping
as a key area of competence, and most have processes to support and encourage this.
Each profession also has its own standards for record-keeping, so check what your
professional body suggests.
All services that you provide and for which you invoice us must be supported by clinical
records that meet your profession’s standards and ACC’s recommendations. See
What we
recommend for all clinical records.
Requesting your clinical records
People wanting to lodge claims for injuries can have complex or confusing presentations.
ACC has a legislated right to view your clinical records at any time. Your clinical records
provide us with the necessary clinical evidence to determine whether your patients’ injuries
meet the legislative requirements for different types of cover and that your treatment was
necessary and appropriate.
If a patient’s injury is covered, they may be given treatment and other support as their
‘entitlement’. Normally, primary care consultations/visits receive automatic financial
contributions under the
Regulations, but for special services such as surgery, pain
management, weekly compensation and home help we’re obliged to check that the
requested support is directly related to the clients’ injuries. Your records can be crucial in
helping us to determine entitlements and overall rehabilitation plans.
We’ll require copies of relevant clinical records when you submit an
ACC32 Request for
Prior Approval of Treatment form.
Your clinical records might also be requested:
by other agencies for other reasons, such as an adverse patient outcome or patient
complaint
for certain invoiced services to ensure these are clinically justified
by other treatment providers (you’ll need patient consent for this)
by your patients
if your practice undergoes one of our periodic audits.
What we recommend for all clinical records
Your clinical records for each patient need to:
provide client identifiers such as name, date of birth and ethnicity
provide your name, a legible signature (if on paper) and the date and time of each
consultation/visit
y ti
be written at the time of the consultation/visit or shortly afterwards and have any later
records dated and countersigned
qual
be written in English on a permanent electronic record or, if on paper, be legible and
in pen, not pencil
record any tests or communication that influenced your diagnosis or treatment
orting
record any prescribed medications the patient is taking
provide clinical reasons to justify any consultation/visit or ongoing treatment
provide a provisional diagnosis and supporting rationale if there is a differential
Supp
diagnosis
identify a treatment plan and rehabilitation expectations, as discussed with the patient
Accident Compensation Corporation
Page 27 of 128
link to page 22
ACC Treatment Provider Handbook 2016
record any referrals made
show consistency between your appointment record and invoice dates
be stored securely for a minimum of 10 years after the final consultation/visit
be transported (physically or electronically) only when essential, taking all steps
necessary to protect that information. See
Privacy
withstand scrutiny of the treatment provided in the event of peer review, audit
(medical or financial) or medico-legal challenge.
What to avoid in your clinical records
Make sure you don’t:
use ambiguous abbreviations
make offensive or humorous comments
alter notes or disguise additions.
Our recommendations for the initial consultation/visit
To help us make appropriate decisions as swiftly as possible, we ask that in the initial
consultation/visit you record details of the:
accident, how it occurred and any mechanisms of injury
injury symptoms and clinical significance
reason for the presentation, or the main reason if the consultation/visit involves more
than one condition
history and examination findings, including important negatives
relevant past history, including medications
initial working diagnosis
pain and effect on sleep, work and other activities of daily life
employment history – current employment, the physical, perceptual and mental
demands of work as it relates to the patient’s functional limitations, and the
willingness of the employer to make workplace accommodations
initial advice you’ve given the patient, e.g. about work fitness or injury-related
restrictions
treatment undertaken and tests and investigations required
management and follow-up plan.
Our recommendations for follow-up consultations/visits
Your records for any follow-up consultations/visits should demonstrate that your treatment
meets the legislative requirements of being necessary and appropriate. We ask that you
detail:
y ti
the patient’s progress
ual
your evaluation of the effectiveness of previous treatment
new aspects of history and examination, and the results of any new tests or
investigations
any restated or revised diagnosis
orting q
any subsequent advice given to the patient
any treatment provided
Supp
the reason for any change to an earlier treatment plan
work capacity and return-to-work barriers
Accident Compensation Corporation
Page 28 of 128
ACC Treatment Provider Handbook 2016
any reports or communication relating to the injury.
Peer reviews
To ensure that we have the best possible information, we may sometimes approach peers
in your clinical area for independent advice. Peer reviewers may be clinical advisors
employed by ACC or external advisors nominated by your professional body.
Monitoring providers and fraud control
ACC requires assurance that providers are supplying services that match ACC’s
requirements, and that the invoices you submit are valid and correct.
The legal basis for any monitoring is set out in:
any service contracts agreed between providers and ACC, and/or
the
Regulations, which cover invoicing and payments under the
AC Act.
ACC guides providers towards best-practice behaviour and contract compliance to help
improve client services and relationships.
The assistance we offer includes:
working with providers in an educative and supportive way
monitoring the activities of providers whose invoicing patterns cause concern, in
accordance with ACC’s performance and monitoring framework
helping to develop, negotiate and implement improvement plans for providers
managing and resolving provider issues that affect client outcomes.
We’ve developed a suite of provider indicator reports. These reports have been developed
to enable ACC to monitor provider service variations regularly within and across provider
types, monitor provider billing behaviour, manage the risks involved in provider services,
and identify and prioritise areas/groups where quality improvement/education is required.
How ACC investigates and controls fraud, wastage and abuse
In respect of fraud ACC understands that:
“Any person who commits an act or omission that is dishonest and without claim of right
and for the purpose of obtaining a pecuniary advantage (money) or other valuable
consideration (e.g. an entitlement) for oneself or any other person, commits fraud”.
ACC has a dedicated team focused on minimising fraud, wastage and abuse to preserve
y ti
the value and sustainability of the Scheme and keep it fair for those who need it most.
ual
This is implemented through ACC’s three lines of defence approach. The first line is the
primary identification and management of risks through Supplier Manager monitoring. The
second line is Integrity Services’ data-led detection insights. The third line is independent
reviews.
orting q
Supp
Accident Compensation Corporation
Page 29 of 128
ACC Treatment Provider Handbook 2016
Integrity Services
Our Integrity Services team utilises a range of methodologies to achieve its planned
objectives, including a prevention-first philosophy to minimise fraud occurring in the first
place and, when it’s discovered, intervening early to prevent further loss.
The remedies we consider when we detect fraud include:
formal warnings
recovering money that’s been unlawfully or inappropriately obtained
billing restrictions
complaints to professional bodies
prosecution
penalties under legislation
civil court action.
Integrity Services provides national support and advice to the ACC business while also
engaging through appropriate channels with professional bodies and peer agencies across
the sector. This ensures that optimal strategies are adopted to manage fraud risk.
Situations requiring Integrity Services intervention include:
claiming for treatments and services not provided
intentional over-servicing for financial gain
falsifying billing schedules and treatment invoices.
Contacting Integrity Services
If you have concerns that you believe may require ACC Integrity Services’ attention,
please contact the team on
0508 222 37283 or by email at
[email address]. You can also
report fraud via our
website.
y ti
ual
orting q
Supp
Accident Compensation Corporation
Page 30 of 128
ACC Treatment Provider Handbook 2016
4.
Provider registration
Registering to become an ACC provider
Why become a registered ACC provider?
Registration with ACC enables you to:
lodge claims for cover on your patients’ behalf
provide treatment for ACC clients within your scope of practice
invoice us for the services you provide to our clients
order stationery such as ACC claim forms
receive important communications.
Who can register?
Any treatment providers seeking payment for services to ACC clients need to register with
ACC. Registration is open to all those identified under the
AC Act as treatment providers.
This table shows the vocations that qualify, noting the groups that are identified under the
Act as ‘registered health professionals’ and under the
Regulations as ‘specified treatment
providers’.
Specified
Treatment
Registered health
Vocational classification
treatment
provider
professional
provider
Acupuncturist
Audiologist
Chiropractor
Clinical dental technician
Counsellor
Dental technician
Dentist
Medical laboratory technologist
oni
Medical practitioner
trats
Medical radiation technologist
egi
Midwife
der ri
Nurse
Nurse practitioner
Prov
Accident Compensation Corporation
Page 31 of 128
link to page 78 link to page 85 link to page 88
ACC Treatment Provider Handbook 2016
Occupational therapist
Optometrist
Osteopath
Pharmacist
Physiotherapist
Podiatrist
Speech therapist
Note: Acupuncturists must be members of either the
New Zealand Register of
Acupuncturists or the
New Zealand Acupuncture Standards Authority at the time of
delivering treatment.
ACC’s registration requirements
The qualification, registration and certification requirements that treatment providers must
meet differ slightly between groups. For details of the different invoicing arrangements, see
Invoicing and payments.
Registered health professionals
Providers categorised as ‘registered health professionals’ are asked to demonstrate
qualifications in a way that directly reflects the registration and professional standards
required of them by the
HPCA Act.
Registered health professionals can include those holding interim practising certificates,
but only when they’re acting in accordance with any conditions of their certification, as
stated in the HPCA Act.
Nurses and nurse practitioners
Under the
AC Act nurses and nurse practitioners are those who are registered as such in
terms of the
HPCA Act and hold current annual practising certificates. These categories
don’t therefore include enrolled nurses or nurse assistants.
Specified treatment providers
‘Specified treatment providers’ are designated in the
Regulations. Their registration
on
process is similar to that followed by registered health professionals.
i
trat
Specified treatment providers have special arrangements for invoicing and payment that
s
include the option of hourly rates or fixed rates per treatment. This reflects the way they
egi
provide treatment. For details, see
Specified treatment providers.
Counsellors
der ri
Counsellors work with ACC in a slightly different way. To reflect these differences,
counsellors have a separate registration process. See
Counsellor registration.
Prov
Accident Compensation Corporation
Page 32 of 128
ACC Treatment Provider Handbook 2016
Registering to provide contracted services
While some services can be provided under the
Regulations, others can only be provided
under contract. If you’re interested in registering as an ACC health provider and want to
take up a contract, your key initial contact will be the Provider Service Delivery team. This
team negotiates and manages ACC contracting opportunities.
ACC’s contracted services govern client assessment, planning and
treatment/rehabilitation. We contract directly with treatment and rehabilitation providers to
connect our clients with a wide range of services. Those services are summarised on our
website.
For more information about applying for a contract you can:
contact the Health Procurement and Contracting team on
0800 400 503 or by
emailing
[email address]
visit ou
r website.
Individual registration
How to register as an individual treatment provider
If the organisation (vendor) for which you work has a contract with ACC you may not be
required to go through a registration process for yourself. For example, clinics or practices
holding Accident and Medical contracts or Rural General Practice Services contracts
register in a different way.
If you do need to register as an individual, you’ll need to supply:
a completed
ACC024 Application for ACC Health Provider Registration form
a copy of your current annual practising certificate
your bank account details, either on a pre-printed bank deposit slip or via bank
verification.
For more information and registration forms, visit ou
r website.
Alternatively, you can call the Provider Contact Centre on
0800 222 070 or email
[email address] and we can fax, post or email the relevant application form to you.
Once you’ve completed the form and attached all additional information required, please
send it to:
oni
ACC Provider Registration
PO Box 30823
trat
Lower Hutt 5040
s
egi
Alternatively, you can fax your form to
04 560 5213 or email scanned images of the signed
form to
[email address].
der ri
The Health Practitioner Index
The Health Practitioner Index (HPI) is a Ministry of Health initiative that ACC supports. The
Prov
HPI is an identification system that replaces the:
Accident Compensation Corporation
Page 33 of 128
ACC Treatment Provider Handbook 2016
ACC provider number with an HPI person number
ACC vendor number with an HPI organisation number
ACC facility number with an HPI facility number.
ACC will register you with your HPI-Common Person Number (HPI-CPN). If this isn’t
possible, you’ll be allocated your own ACC provider number. We may contact you directly
to change from an ACC number to an HPI number. Individual providers may already be
using HPI-CPN, issued by their regulatory authorities.
Receiving your registration number
We’ll let you know in writing that we’ve accepted your application for registration, and
confirm your provider number within five working days of receiving the application.
ACC uses provider numbers to identify who’s provided treatment, track payments and
monitor treatment provider performance. Your provider number is therefore specific to you
and mustn’t be shared with other health professionals. Please use it whenever you can in
communications and transactions with us.
If you’re employed at more than one practice, you may need a separate provider number
for each practice. This is due to restrictions with the electronic schedule and the invoice
payment systems used by some practices. Please contact the ACC Provider Registration
team on
04 560 5211 to find the best solution.
Keeping your details up to date
It’s important that we hold up-to-date contact details for you, and we ask that you contact
us if you’ve changed your name, postal or email address, or phone or fax number. You
can update your details with us by phoning the Provider Contact Centre on
0800 222 070 or emailing
[email address] (please make sure you include your provider number
in the email).
We’ll update your records, send you confirmation of the change, and give your new details
directly to our printing and distribution partners, so they have the correct details in their
databases when you order stationery.
All bank account changes require either a pre-printed bank deposit slip or bank
verification. We can also accept faxed or emailed copies if they’re received via a
previously verified email address or fax number.
To check the details we currently have recorded for you, please get in touch with the
Provider Contact Centre on
0800 222 070 or email
[email address].
oni
Counsellor registration
trats
Who can be an ACC counsellor?
egi
ACC accepts applications from suitably qualified and experienced counsellors, including
social workers, psychotherapists, psychologists and psychiatrists.
der ri
Prov
Accident Compensation Corporation
Page 34 of 128
link to page 37 link to page 88 link to page 54
ACC Treatment Provider Handbook 2016
Benefits of being an ACC counsellor
Counsellors registered with ACC can lodge
ACC45 Injury Claim forms on behalf of clients,
which can make it faster and easier for the clients to receive our services.
We’ll pay for your counselling services at published rates in accordance with the
Regulations. The rates differ slightly according to whether treatment is given by a
counsellor or a psychiatrist (a medical practitioner).
See a
lso Payment for counsellors.
Counselling services purchased by ACC
ACC purchases counselling services for clients with:
sensitive claims
mental injuries from physical injuries or work-related events.
ACC also has a Sensitive Claims Unit that specialises in helping people to rehabilitate and
recover from mental and physical trauma caused by criminal acts such as sexual violation,
indecent assault and unlawful sexual connection. Counselling services are key to the
recovery of these clients.
We also help people to recover from mental injuries that are the direct result of covered
physical injuries or traumatic work-related events.
For more information see
Mental injuries, sensitive claims and counselling.
If you have any questions about our counselling work, please contact the Provider
Registration team on
04 560 5211 or email
[email address].
Required qualifications, skills and experience
To be registered as an ACC-approved counsellor, psychologist, psychotherapist or
psychiatrist, you need specific qualifications, skills and experience.
The requirements include:
membership of an appropriate professional body
qualifications that reflect your nominated area of expertise
previous and ongoing supervision arrangements
cultural competency
proof of relevant ongoing training or experience in sexual abuse or physical injury
oni
counselling.
trats
You’ll need to include other supporting documents:
egi
a completed application form
two case studies
der ri
consent for a police check
a copy of your current annual practising certificate.
Prov
Accident Compensation Corporation
Page 35 of 128
ACC Treatment Provider Handbook 2016
If you belong to another profession you’ll need to provide additional items, including
certified copies of your academic qualifications. You’ll also need to arrange for your
supervisor to provide details about you and about their own membership of an appropriate
professional body.
You can get more information on the required qualifications by:
phoning the ACC Provider Registration team on
04 560 5211 emailing
[email address].
Applying for registration
To find out how to apply to become an ACC-approved counsellor, we recommend that you
visit ou
r website.
How we assess your application
All applications are reviewed by an external evaluation panel made up of nominated
representatives from various New Zealand counselling bodies.
The panel will assess your qualifications and experience against the ACC criteria and
make its recommendation to us. We’ll make the final decision.
The application process includes a Police check to find out if New Zealand Police holds
any information about you. This includes details of criminal convictions, except those
covered by section 7 of the
Criminal Records (Clean Slate) Act 2004.
Letting you know
We aim to advise you of our decision within six weeks of receiving your completed
application.
oni
trats
egi
der ri
Prov
Accident Compensation Corporation
Page 36 of 128
link to page 38 link to page 38 link to page 51 link to page 67 link to page 67 link to page 48 link to page 48 link to page 44 link to page 48 link to page 48
ACC Treatment Provider Handbook 2016
5.
Lodging claims
Lodging a claim with ACC or an Accredited Employer
Forms used to lodge claims
There are five main forms used to lodge claims, and most can be lodged electronically:
ACC45 Injury Claim form
The ACC45 Injury Claim form is the primary form used to lodge claims for cover, and
should be used wherever possible. This is because it has a unique number for security
reasons, which we also use to monitor claims, and provides sufficient prompts within the
form to ensure that all the necessary information is provided. See
Completing the ACC45
Injury Claim form for more information. If your patient requires further time off work, you’ll
also need to complete an ACC18 Medical Certificate form.
ACC2152 Treatment Injury Claim form
Use this form in addition to the ACC45 Injury Claim form when lodging a treatment injury
claim. For more information, see
Treatment injury.
ACC18 Medical Certificate form
Use the ACC18 Medical Certificate if you’re a medical practitioner or a nurse practitioner
and you need to describe a person’s ability to work. This is the only certificate we accept
for compensating clients for time off work. For more information see
Medical certificates
(ACC18s). An ACC18 Medical Certificate form can also be used to request ACC
to change
or add a new diagnosis to an existing claim.
ACC42 Dental Injury Claim form
The ACC42 Dental Injury Claim form is a specialised form of the ACC45 Injury Claim form
that dentists use to provide more specific details about clients’ dental injuries.
ACC32 Request for Prior Approval of Treatment form
The ACC32 Request for Prior Approval of Treatment form can be used for several
purposes (refer to
ACC32) – such as when your patient’s injury is covered and you:
anticipate that you’ll need prior approval from ACC for additional treatment funding
want to add or change a diagnosis (see also
What information does ACC need?) want additional splinting costs.
Ordering new forms
ms
ail
The easiest way to access and submit order forms is electronically; however, if you don’t
have access to a computer, printed forms can be requested. To order new forms, reply-
paid envelopes and other ACC supplies, phone the Stationery Order Line on
0800 802
ng c
444.
Lodgi
Accident Compensation Corporation
Page 37 of 128
link to page 90 link to page 31 link to page 67 link to page 41 link to page 41 link to page 40 link to page 40 link to page 92
ACC Treatment Provider Handbook 2016
The claim lodgement process
When you lodge a claim using the ACC45 Injury Claim form you’re asking us to cover a
patient’s personal injury.
Please complete the form with your patient and send it to ACC either as a paper form or
electronically. The fastest way to lodge a claim is electronically. For more information on
electronic lodgement, visit ou
r website or see
Working electronically with ACC.
Each ACC45 Injury Claim form has a unique, secure reference number that identifies the
patient’s claim once it’s been lodged. The form is used for many injuries and conditions
and enables you to provide important information that can help start the treatment,
rehabilitation and/or entitlements process.
Only treatment providers defined by legislation can lodge claims on behalf of patients. See
Who can register? for a list of accepted providers, and visit ou
r website for more
information. If you’re an acupuncturist you may lodge a claim but you’ll need the patient to
have the diagnosis confirmed by another provider. Claims won’t be considered for
treatment or entitlements until a confirmed diagnosis has been received and cover
approved.
Only medical practitioners and nurse practitioners can certify incapacity for work. For more
information see
Medical certificates (ACC18).
Lodging a claim with an Accredited Employer is slightly different. For more information se
e
Lodging Accredited Employer claims.
The processes for lodging specific claims can differ. Visit ou
r website for details on how to
lodge:
claims for mental injury caused by sexual abuse
claims for treatment injury
claims for work-related gradual processes, diseases and infections
late lodgement claims.
If you’re not sure how to lodge a claim with ACC we encourage you to check out the
information on ou
r website, or give us a call. This will make sure everything goes smoothly
for you and your patient. If you have a question about lodging a claim or a claim already
submitted, please get in touch with the Provider Contact Centre on
0800 222 070 or email
[email address].
Completing the ACC45 Injury Claim form
There is information about how to complete, sign and lodge a claim on ou
r website. See
a
lso Where to send the claim forms.
ms
ail
Things to note when completing the form and before you submit it:
If you want to check whether a claim has already been submitted
ng c
If you need help in finding out about a claim already submitted, call the Provider Contact
Centre on
0800 222 070 or email
[email address] with the patient and injury
Lodgi
details. You can also check on a claim’s status through the
eLodgement system.
Accident Compensation Corporation
Page 38 of 128
ACC Treatment Provider Handbook 2016
If your patient has claimed for their injury before
Quote the ACC45 number for their original claim. The number will be on the referral form
or the first ACC45 Injury Claim form.
Check the client’s personal details (Part A) and employer details (Part B) and, if
necessary, update them.
Include previous surnames if they’ve changed within the previous few years.
If your patient is in paid employment
Employers’ names and addresses must be included for all claims where your patients are
in paid employment, regardless of whether their injuries are work related.
If you think your patient needs help beyond ACC’s contribution to treatment costs
For example, if you think your patient needs further treatment, personal support or weekly
compensation, there are several places on the ACC45 Injury Claim form where you can
specify their additional needs.
You can also give them your professional assessment of these needs and encourage
them to contact the Client Helpline on
0800 101 996 as soon as possible. In most cases
they can apply for entitlements over the phone. However, entitlements aren’t granted until
cover has been accepted, so it’s still essential that you lodge the ACC45 Injury Claim form
promptly.
If your patient presents with a sexual abuse injury
It’s important that you also ask them whether they want mail from ACC and providers to be
sent to a different address from the one in your records.
Before submitting the form
Add NHI (National Health Index) numbers if you know them.
Be sure to go over the Patient Declaration and Consent section on the back of the ACC45
Injury Claim form with the patient to ensure they understand what they’re signing.
Using Read Codes
Read Codes are a hierarchical coding system for injury types, with each level giving a
more specific diagnosis. Each Read Code has five characters. If a Read Code only has
four numbers it will end in a dot, which becomes its fifth character.
Primary care providers are required to record Read Codes for all diagnosed injuries for
ACC claims. Hospitals and secondary care providers can use ‘International Classification
ms
of Diseases: 10’ (ICD-10) codes instead, although they can and often do also provide
ail
Read Codes. Having the correct Read Code helps to ensure that we cover the correct
injury and provide the client with the most appropriate support, treatment and
ng c
rehabilitation.
Lodgi
Accident Compensation Corporation
Page 39 of 128
link to page 37 link to page 37 link to page 37 link to page 44 link to page 39 link to page 92
ACC Treatment Provider Handbook 2016
Recording a Read Code
When completing an ACC form, e.
g. the ACC45 Injury Claim form, the
ACC18 Medical
Certificate or the
ACC32 Request for Prior Approval of Treatments please:
record the Read Code that best corresponds to your diagnosis of your patient’s injury
record the lowest relevant level of Read Code
use a separate Read Code for each injury for a client with multiple injuries in the order
of severity/complexity
ensure that each Read Code includes the dot, if necessary, for the most accurate
injury diagnosis
use Code Z (unspecified condition) if there’s no Read Code to match your diagnosis,
and provide a detailed written diagnosis. An ACC staff member will complete the
Read Code field and may contact you if they need to clarify anything.
If you don’t have access to the full Read Code directory via Read Code software, refer to
the
ACC6343 Read Code reference list which is sorted by type and location of injury. You
can also access the Read Codes commonly used in
physiotherapy, osteopathy and
chiropractic.
For more information, see
Using Read Codes.
Where to send the claim forms
If you’re sending claim forms using eLodgement, do so regularly during the day. Most
claim forms can be sent electronically.
Visit our website for more information on
lodging a claim electronically and working online
with ACC.
If you’re sending claim forms by post or fax, visit ou
r website for a list of offices that deal
with specific and general claims.
Work-related injury claim forms and documentation for employees who work for Accredited
Employers must be sent directly to the employers.
What happens next?
For details on how we process a lodged claim, visit ou
r website.
When cover has been accepted we advise the client by letter. If you want to find out
whether cover has been accepted, call the Provider Contact Centre on
0800 222 070 and
quote the ACC45 claim number or email
[email address]. You can also check via
the
eLodgement system.
ms
It’s important that we have all the information we need to make a decision. If we don’t have
ail
enough information the claim can be put on hold, or declined pending further information.
We don’t usually pay for claims with insufficient information to make a decision unless they
ng c
are work-related gradual process claims or sensitive claims.
Invoicing
Lodgi
Accident Compensation Corporation
Page 40 of 128
link to page 79 link to page 79
ACC Treatment Provider Handbook 2016
For information on invoicing ACC and Accredited Employers, see
Invoicing ACC or
Accredited Employers or visit ou
r website.
Lodging Accredited Employer claims
About Accredited Employers
An Accredited Employer is a business that’s signed a ‘Partnership Programme’ contract
with ACC. This allows it to deal directly with staff workplace claims and health providers on
behalf of ACC.
Accredited Employers pay lower ACC levies than other employers and are expected to
provide the same cost contributions and quality of service as ACC. Some Accredited
Employers also choose, at their discretion, to refund co-payments for their employees.
They manage their own:
workplace health and safety
employee injuries, including rehabilitation
employee workplace (but not non-workplace) injury claims.
Over a quarter of New Zealand’s full-time employees work for Accredited Employers. If
your patient isn’t sure whether they work for an Accredited Employer, you can find out by
calling the Provider Contact Centre on
0800 222 070.
Third-party administrators
An Accredited Employer may contract a ‘third-party administrator’ (TPA) to deliver injury
and claim management services to its injured employees. TPAs include Gallagher Bassett,
Wellnz and WorkAon.
TPAs can only act as payment agents and day-to-day points of contact, while Accredited
Employers remain responsible for managing their injured employees’ claims and injuries.
How to lodge an Accredited Employer claim
Send all documentation for your Accredited Employer patients (i.e. the initial ACC45 Injury
Claim forms, treatment and rehabilitation plans, and invoices) to the Accredited Employers
or their nominated TPAs, rather than ACC.
Visit our website for more information
on lodging a claim with an Accredited Employer and
for the
answers to frequently asked questions on Accredited Employers and the ACC
Partnership Programme.
ms
ail
ng c
Lodgi
Accident Compensation Corporation
Page 41 of 128
link to page 115
ACC Treatment Provider Handbook 2016
6.
Treatment
Acute treatment
Definitions: acute treatment and acute admission
The
AC Act describes
acute treatment as:
the first visit to a treatment provider to get treatment for an ACC-covered personal
injury
if, in the treatment provider’s judgement, the need is urgent (given the likely clinical
effects on the client of any delay in treatment):
o any subsequent visit to that treatment provider for the covered injury
o any referral by that treatment provider to any other treatment provider, for the
covered injury.
The Act describes
acute admission as an admission to a publicly funded or agreed facility
within seven days of the decision being made to admit, unless otherwise specified in the
Regulations. See
Accident Services – A guide for DHB and ACC Staff (see a
lso Glossary).
Deciding if acute treatment/admission is needed
You need to be appropriately qualified to decide whether an injury needs acute treatment;
otherwise you need to refer the client to a treatment provider who’s qualified. The referred
visit to another treatment provider is also regarded as acute treatment. The applicable
qualification is described in the
Provider claim lodgement framework.
If you determine that the client’s injury is outside the scope of a primary care provider and
that acute specialist assessment/treatment and/or acute hospital admission is required,
you must ensure that the treatment is provided by:
a publicly funded provider, or
a provider that isn’t publicly funded, if:
o ACC agrees beforehand (prior approval), or
o for reasons of clinical safety, treatment by a publicly funded provider isn’t
practicable.
Funding Public Health Acute Services (PHAS)
PHAS are funded by a bulk payment from ACC to the Crown. The Crown then funds the
Ministry of Health to purchase these services from DHBs on behalf of ACC. You can find
more details in the publication
Accident Services – A guide for DHB and ACC staff.
Referring for other acute services
Radiology
nt
For X-ray referrals we recommend that you complete your practice radiology referral form
and remember to enclose a copy of it with the ACC45 Injury Claim form. If your patient is
eatme
likely to need acute treatment outside the scope of a primary care provider, in addition to
radiology for their injury, refer them to the nearest public hospital.
Tr
Accident Compensation Corporation
Page 42 of 128
link to page 18
ACC Treatment Provider Handbook 2016
High-tech imaging
Acute high-tech imaging, such as MRIs and CT scans for ACC clients, is provided as part
of PHAS. If your patient needs high-tech imaging as part of their acute treatment, please
refer them to the nearest DHB.
Non-acute MRIs are funded separately by ACC under contract. For more information on
how to access this service, phone the Provider Contact Centre on
0800 222 070 or email
[email address].
Surgery and specialist treatment
Acute surgery and specialist treatment is provided under PHAS. If your patient needs
these services, refer them to the nearest DHB.
Elective surgery and specialist treatment are paid for by ACC through both the
Regulations
and contracts. You can refer your patient to a specialist directly. The specialist will request
funding for treatment from ACC as required.
Nursing services
Nursing services
Nursing services can be provided in two ways to ACC clients who have covered injuries:
under the
Regulations (see
How ACC pays)
through contracted nursing services (community-based service delivery within the
clients’ homes, a clinic or any other appropriate community location).
Contracted nursing services
These are services to patients whose nursing needs can’t be met by their primary care
teams. There could be many reasons for this, including:
the patient has reduced mobility
the patient has little or no natural support, making it unsafe or impractical for them to
attend a medical centre
the injury-related needs of a seriously injured patient
the patient needs care outside normal practice hours
the patient has complex injuries – for example ulcers, wounds with heavy exudate, a
large bacterial burden, pressure wounds or skin grafts
the patient needs specialised treatment – for example stoma care, compression
therapy or negative-pressure wound therapy
the patient has a history of leg ulcers, slow-healing wounds, immuno-compromise,
heart disease or diabetes
the patient is a student with a complex wound and can’t be managed by their primary
health care team or school nurse. The supplier can provide services at the school,
nt
home or clinic
the patient has made a full or partial return to work and their individual rehabilitation
plan states the treatment is to occur at the workplace. This requires prior approval
eatme
from ACC.
Tr
Accident Compensation Corporation
Page 43 of 128
link to page 48 link to page 48 link to page 48 link to page 48 link to page 48
ACC Treatment Provider Handbook 2016
Please note, however, that eligibility for entry to this service isn’t influenced by patient
preference or convenience.
Entry to this service is by referral only, including for any subsequent injuries. Referrals can
be generated by:
the primary health care team (e.g. GP, nurse practitioner or practice nurse)
patient self-referral (if the patient lives in a remote or rural area at least 50 kilometres
or 30 minutes’ drive from the nearest medical centre that has a doctor in regular
attendance).
To satisfy the nursing supplier that there is a covered injury requiring the input of nursing
services, your referral should include:
the patient’s personal details
injury diagnosis
treatments to date
nursing needs
rationale for requiring services outside what can be provided by the primary health
care team.
Requesting further treatment
Using the ACC32 Request for Prior Approval Treatment form
The ACC32 Request for Prior Approval of Treatment form can be used for different
purposes by specified treatment providers – for example when your patient’s injury is
covered and you:
anticipate that you’ll need ACC prior approval for additional treatment funding or are
requesting additional splinting costs
want to
add a diagnosis to a covered injury (see also
What information does ACC
need?)
want to
change a diagnosis (see also
What information does ACC need?)
want to recommend another treatment provider in addition to completing another
referral.
Further treatment and costs
Prior approval for further treatment
Prior approval is required from ACC when:
it has been more than 12 months since the client last received treatment from a
specified treatment provider, or
nt
a client first presents for management of an injury more than one year after the date
of that injury, or
the treatment trigger number for the covered injury has been (or is about to be)
eatme
reached and your client requires more treatment.
Tr
Accident Compensation Corporation
Page 44 of 128
link to page 27 link to page 27
ACC Treatment Provider Handbook 2016
Each Read Code identifies the number of treatments (trigger numbers) you can provide
before you need ACC prior approval to fund further treatment. Trigger points are a guide to
expected recovery timeframes only, and all decisions are based on individual clinical need.
ACC will consider each request on a case-by-case basis and will advise whether ongoing
treatment has been approved or declined. It’s important to include all available clinical
information at the time of seeking prior approval. No payments will be made until prior
approval has been granted.
When completing an ACC32 Request for Prior Approval of Treatment form it’s important to
specify the date of the injury, details of the covered injury and the treatment given to date.
If this information isn’t available from the client, call the Provider Contact Centre on
0800
222 070 or email
[email address].
What treatment profile trigger applies if you’re registered with ACC for more
than one treatment modality?
If you choose to move between different treatment modalities in the management of your
patient, the treatment profile trigger relating to the primary modality applies, regardless of
the type or combination of modalities used.
Example: A provider is registered with ACC as a physiotherapist and also as an
acupuncturist. The client’s injury is primarily treated with physiotherapy, but the provider
determines that acupuncture is also required at the same presentation. Only the
physiotherapy treatment profile trigger would apply.
A dual-registered provider can’t refer to themselves for their second modality without first
seeking prior approval by:
completing an ACC32 Request for Prior Approval of Treatment form
supplying clinical records that demonstrate the need for the change in treatment
modality.
The treatment profile trigger numbers for multiple modalities can’t be added up or used
one after the other for ongoing treatments. The services should be invoiced under the
provider’s primary vocational scope.
What to include in the ACC32 form
The information we need in the ACC32 Request for Prior Approval of Treatment form will
depend on what type of provider you are. It is important to send ACC your request well
before your last treatment so that continuity of treatment can be assured.
Physiotherapists
If you’re a physiotherapist or hand therapist you’ll need to include both an ‘outcome
measure’ report and the client’s clinical notes with each ACC32 application.
nt
Other specified treatment provider groups
Other specified treatment providers only need to submit clinical records with ACC32
eatme
applications. The clinical records should be dated, legible and in English (see
What we
Tr
recommend for all clinical records).
Accident Compensation Corporation
Page 45 of 128
ACC Treatment Provider Handbook 2016
If the information you submit is incomplete, we’ll return the form straight away and ask for
the missing information.
If the treatment required is post-operative and within 12 months of the date of ACC-funded
surgery, please note this on the ACC32 Request for Prior Approval of Treatment form
along with the date of surgery. Alternatively, you can call the Provider Contact Centre on
0800 222 070 and obtain approval.
Outcome measures for physiotherapy
Outcome measures are a tool for measuring the effects of physiotherapy interventions
over time. They give all parties a better understanding of the outcomes achieved from
purchasing physiotherapy services for clients. They also enable physiotherapists to reflect
on their clinical practice and quality of service.
Physiotherapists are required to use evidence-based outcome measures. We recommend
either:
the Patient Specific Functional Scale (PSFS) outcome measure, or
the Numeric Pain Rating Scale (NPRS).
However, an alternative standardised, evidence-based outcome measure can be used if
it’s more appropriate to a client’s condition.
For guidance on using evidence-based outcome measures see the ACC
Guide to
Outcome Measure Reporting. This document focuses on the PSFS and NPRS because of
their widespread acceptance among physiotherapists and other clinicians.
Please record a validated outcome measure for every ACC client:
at the initial consultation/visit
after six treatments
on discharge.
When patients are referred by other types of provider
Approval for treatment is discipline specific. Using the ACC32 Request for Prior Approval
of Treatment form to refer a client to a different provider type isn’t the same as using it to
request ACC prior approval for further treatment.
If a provider of another discipline recommends referral to your discipline on an ACC32
form that they have submitted to ACC, or uses an ACC32 form to refer a client directly to
you, you’ll still need to determine if your treatment requires prior approval and submit an
ACC32 form yourself. Please attach the other provider’s referral letter or ACC32 form
when you submit your ACC32 request.
If a client has been referred to you by another provider of the same discipline as yourself,
nt
you’ll need to confirm how many treatments the client has received, and complete another
ACC32 form if the treatment profile triggers have been reached.
Our decision process
eatme
Tr
Once you’ve completed the ACC32 Request for Prior Approval of Treatment form and
included all relevant information, please send it to your nearest service centre. We aim to
Accident Compensation Corporation
Page 46 of 128
ACC Treatment Provider Handbook 2016
issue a decision or advise you of any delay within five working days of receiving the
documents.
The requests are assessed by clinical advisors as necessary and we’ll write to both you
and the client with our decision. If we decline the request we’ll also try to contact the client
to talk them through our decision.
What to do if you disagree with our decision
If we decline your request for funding additional treatment, you can seek clarification from
an ACC clinical advisor. The client can also formally dispute the decision, as all decisions
are issued with review rights, meaning the client can have the decision independently
reviewed. A request for review needs to be submitted within three months of the date of
our decision, although this can be extended if a situation beyond their control prevents the
client applying within that timeframe.
Criteria for approving requests
If we approve your request for treatment we’ll fund up to six treatments in addition to the
treatment profile trigger, as long as you invoice ACC in the order that the services are
delivered.
If it’s a request for a serious injury client we can approve more than six treatments if it’s
clinically justified. Please ensure that you include all supporting information.
Criteria for declining requests
We’re unable to approve an ACC32 treatment request if:
there’s no causal link
There needs to be a clear link between the client’s ongoing condition and the covered
injury in order to receive funding. This link must be supported by medical evidence, as
a condition may be similar to, but not caused by, an injury.
it’s not injury related
If the request is for a condition not related to the injury, we’re not able to cover it.
it’s not considered necessary or appropriate
If clinical records show that there hasn’t been any significant improvement as a result
of treatment, further requests for treatment can’t be justified.
the injury site doesn’t match the covered injury
We can only approve requests for covered injuries. If you’re unsure about whether
your patient’s injury is covered, please contact the Provider Contact Centre on
0800
222 070.
the surgery wasn’t funded by ACC
If we haven’t funded the surgery we’re unable to fund post-operative rehabilitation
nt
treatment.
it’s a gradual process injury
Unless it’s a covered work-related gradual process condition we’re unable to fund
eatme
treatment.
Tr
it’s for treatment plus cover, or cover only
Accident Compensation Corporation
Page 47 of 128
link to page 48 link to page 48 link to page 37 link to page 37 link to page 44
ACC Treatment Provider Handbook 2016
Cover and entitlement are two different decisions. If you submit an ACC32 Request
for Prior Approval of Treatment form to add an injury, we need supporting clinical
information. We may or may not approve cover while determining treatment. See
Adding or changing a diagnosis and
What information does ACC need?
it’s a new claim
If, as a result of a patient assessment, you believe that their current condition doesn’t
relate to the initial accident, you should inform the patient and not submit an ACC32
Request for Prior Approval of Treatment form.
If during your assessment you find there has been a clear new event causing
personal injury, your patient may want to submit a new ACC45 Injury Claim form.
Adding or changing a diagnosis
Adding a diagnosis to a covered injury
If, when you’re treating your patient, you discover an additional injury(s) related to the
injury we’ve covered, you’ll need to request an ‘additional diagnosis’ before we can provide
assistance for that injury.
Example: A patient falls and sustains a shoulder injury. A claim has been lodged and
accepted for the shoulder injury. However, you find out that the patient also sustained a
knee injury in the fall and you want to treat the knee injury under this claim.
Changing a diagnosis
We’ll consider a request to change a diagnosis if:
there’s been an administrative error, e.g. a claim was lodged for the incorrect body
site
there’s been a change from an ICD-10 code to a Read Code
the initial diagnosis of the injury was incorrect.
Example: A claim was lodged with the lumber sprain Read Code S572. However, there’s
now a confirmed diagnosis that the client has a lumbar disc prolapse with the
radiculopathy Read Code N12C2.
How to add or change a diagnosis
To request that ACC add an injury or change a diagnosis, please submit an
ACC18
Medical Certificate form o
r ACC32 Request for Prior Approval of Treatment form. When
making your request it’s very important that you provide sufficient information for a timely
decision to be made. If we don’t have enough information the claim will be put on hold or
declined pending further information. We don’t usually pay for claims with insufficient
information to make a decision unless they’re work-related gradual process claims or
sensitive claims.
nt
What information does ACC need?
When requesting to add or change a diagnosis you’ll need to provide your clinical
eatme
justification and any supporting documentation.
Tr
Accident Compensation Corporation
Page 48 of 128
ACC Treatment Provider Handbook 2016
Where possible, please include the following information to support the additional injury or
the change in diagnosis:
the date of the original event
the original injury diagnosis
a description of how the new or additional injury has been caused by the original
event
the body site of the new injury
the Read Code for the new/additional diagnosis
medical evidence, e.g. clinical notes, reports, correspondence and X-ray, MRI or
other scan results.
What happens next?
An ACC case owner will review the information you provide and consider your request.
They may also seek further internal clinical advice, for example from an ACC branch
medical advisor.
If we need to clarify anything with you, an ACC case owner will get in touch with you prior
to a decision being made. They’ll contact you and the client when a decision has been
made.
Work-related gradual process, disease or infection
Cover under legislation
ACC covers a range of gradually arising process injuries, diseases and infections if they
involve a personal injury as defined in section 26 of the
AC Act, and there is a causal link
between the injury and the person’s employment.
Eligibility criteria
To be eligible for this cover, clients must meet either of two criteria.
1. The client’s work environment shows that:
there is a particular property or characteristic in a work task or the work
environment that can be identified as having caused the condition
the property or characteristic isn’t materially present outside the person’s work
activities or environment
those performing the work task or employed in that work environment are at
significantly greater risk of developing the condition than those who don’t.
The more common musculoskeletal injuries that can develop over an extended period
of time through work are epicondylitis (lateral or medial), tenosynovitis (e.g. de
Quervain’s), prepatellar bursitis and rotator cuff syndrome. Claims for these need to
satisfy the three-part test above, which reflects section 30 of the
AC Act.
nt
If your patient has noise-induced hearing loss
eatme
Patients with noise-induced hearing loss may be covered if they’ve been exposed to
Tr
hazardous noise levels while working in New Zealand and meet the above criteria. In
Accident Compensation Corporation
Page 49 of 128
link to page 37
ACC Treatment Provider Handbook 2016
addition, the amount of occupational noise-induced hearing loss (i.e. ‘net of age’
corrections and an allowance for other otological conditions) must be at least 6%.
2. The injury is on the list of occupational diseases, with their causative agents, in
Schedule 2 of the AC Act. Common Schedule 2 diseases include occupational asthma,
allergic contact dermatitis, mesothelioma, leptospirosis and lead poisoning. This list
enables an injured person to be granted ACC cover more quickly and easily than the
above criteria.
A person will be covered for a listed disease if evidence shows that they have the
disease and were exposed to contributing factors while working in New Zealand. If it’s
unclear that the disease is linked to employment, ACC must establish that the
Schedule 2 disease isn’t work related.
Lodging a gradual process injury claim
Work-related gradual process injury claims can only be lodged by medical practitioners
and nurse practitioners. Any other provider who believes a person has a gradual process
disease or injury should refer them to a GP to complete an
ACC45 Injury Claim form as
quickly as possible. Any treatments given for the injury (e.g. by a physiotherapist) before
the patient has seen a GP or medical specialist won’t qualify for payment.
When we receive the ACC45 Injury Claim form we send three questionnaires to the
patient. The patient must fill in their questionnaire and ensure that their employer and GP
fill in theirs. All the questionnaires must be returned to ACC so that a cover decision can
be made. As the patient will only be able to receive their entitlement (e.g. weekly
compensation for incapacity) once we’ve accepted their claim, it’s important that you fill in
your questionnaire promptly.
For more information on gradual process claims, see
Work-related gradual process,
disease or infection.
We may ask for a copy of your clinical notes
As we require evidence of actual damage, including a specific diagnosis of the gradual
process injury, disease or infection, we may ask for a copy of your clinical notes and
require test results. Providing details of the patient’s clinical history and your examination
findings at the time you lodge the claim will speed up the cover decision process for them.
If the cause is work task or workplace related
If you’re documenting aspects of work task or workplace cause (to help establish plausible
consequence, an absence of non-work factors and epidemiological evidence), please give
details of where the causative agent is present. This means accurately identifying the
specific property or characteristic in the task or workplace that has caused, or contributed
to, the person’s condition. We may also request a workplace assessment to clarify these
factors.
nt
You might also need to get information on the person’s non-work activities.
eatme
Tr
Accident Compensation Corporation
Page 50 of 128
ACC Treatment Provider Handbook 2016
Treatment injury
How ACC defines treatment injury
Treatment injury is a personal injury suffered by a person seeking or receiving treatment
from a registered health professional and caused by treatment and not a necessary part or
ordinary consequence of the treatment
(section 32 of the AC Act).
Before July 2005 medical misadventure legislation covered treatment injuries. Claims
lodged before this date continue to be managed under the previous legislation.
What treatment injury covers
If a patient is injured as a result of treatment, they may be able to make a claim and get
help through ACC. However, we don’t cover all treatment outcomes that don’t turn out as
expected, so we encourage you and your patient to contact us before lodging a claim to
discuss whether a treatment injury has occurred.
Treatment needs to be provided by a covered registered professional
The covered registered health professionals are:
chiropractors
clinical dental technicians
dental technicians
dentists
medical laboratory technologists
medical practitioners – doctors, surgeons, anaesthetists, etc
medical radiation technologists
midwives
nurse practitioners
nurses
occupational therapists
optometrists
pharmacists
physiotherapists
podiatrists.
Several other provider groups qualify as ACC treatment providers but their treatment can’t
be the subject of treatment injury claims.
However, patients who receive injuries from these treatment providers may still be covered
under the wider ACC personal injury claim provisions. There treatment providers are:
acupuncturists
audiologists
nt
counsellors
osteopaths
speech therapists.
eatme
Tr
Accident Compensation Corporation
Page 51 of 128
link to page 37 link to page 37 link to page 37
ACC Treatment Provider Handbook 2016
Lodging a treatment injury claim
Treatment injury claims are lodged using the
ACC45 Injury Claim form, o
r ACC42 Dental
Injury Claim form, along with a completed
ACC2152 Treatment Injury Claim form. The
ACC2152 form provides additional information that may be sufficient for ACC to determine
cover.
The
ACC2152 form is available on ou
r website. Payment for the consultation/visit when an
ACC45/42 form is submitted is made separately.
For more information on treatment injuries and how to lodge claims, visit our website or
phone the Treatment Injury Centre on
0800 735 566.
Who can complete the ACC45 and ACC2152 forms?
The best person to complete the forms is the registered health professional involved in the
treatment that caused the injury.
The forms can also be completed if you’re a treatment provider who wasn’t involved in the
treatment injury (e.g. if you’re helping a patient) as long as you have enough information.
If you don’t have enough information you should only complete the ACC45 Injury Claim
form and:
tick the ‘Treatment Injury Box’
provide the place of treatment
provide the name(s) of the person(s) involved in the treatment that caused injury
provide any relevant clinical information.
We’ll contact the health professional who provided the treatment for more information.
If you’re helping a patient to complete a claim form, you don’t need to ascertain the cause
of the injury being treated. We understand that you may not have access to this
information (e.g. for older injuries, or when records are incomplete).
Who can’t complete the form?
Some health professionals can’t lodge a treatment injury claim even if they were involved
in the treatment that caused the injury.
These include:
clinical dental technicians
dental technicians
medical radiation therapists
midwives
pharmacists.
What to say to your patients
nt
If possible, you should let your patient know that we’ll assess the claim and we may ask for
more information about the injury and the events that led to it, including from other
treatment providers involved. This means it could take a few weeks or more to reach a
eatme
decision on their claim.
Tr
Accident Compensation Corporation
Page 52 of 128
ACC Treatment Provider Handbook 2016
Legislation gives us up to nine months to make a decision after a treatment injury claim
has been lodged. However, we aim to determine cover as quickly as possible.
Eligibility criteria for clients
A patient may qualify for cover if they’re injured as a result of treatment by a registered
health professional and the treatment, not the patient’s health condition or some other
factor, is the cause of the injury.
The
treatment from which the injury may stem includes the treatment itself, either given or
directed by the health professional, or a lack of treatment that should have been provided.
Under special conditions we’ll consider a claim from someone who was part of an
approved
clinical trial and suffered complications. We’re unable to accept claims resulting
from trials that are mainly for the benefit of the maker or distributor of the item being
tested.
Assessing treatment injury claims
ACC’s Treatment Injury Centre assesses all treatment injury claims. It also assesses
claims for any potential risk of harm to the public.
The Centre starts the claim assessment process as soon as the ACC45 Injury Claim form,
the ACC2152 Treatment Injury Claim form and/or supporting medical records are received.
If only an ACC45 Injury Claim form is received, we’ll need to obtain the ACC2152 form and
other records before we can process the claim.
Each claim is allocated to one of the Centre’s clinical advisors with clinical experience in
nursing, midwifery, pharmacy, physiotherapy and medicine. Their role is to make decisions
on whether to accept claims by assessing the individual facts of the claims and applying
the legislative criteria.
Once a cover decision has been made, the Centre informs the client and advises them to
let their health professional know about it (it doesn’t contact the health professional
directly). For an accepted claim, we either pay the relevant invoices (if no further help is
needed) or transfer the claim to be managed by the client’s local branch (if the client still
needs help).
Assessing the potential public harm
The Treatment Injury Centre analyses treatment injury data to assess the potential risk of
harm to the public.
The results are shared through monthly treatment injury case studies, which can be found
on our website unde
r Clinical best practice, and at presentations to clinical meetings,
conferences and seminars. Notifications are also made monthly to authorities such as the
Director-General of Health, Medsafe and, in some circumstances, registration councils and
nt
boards.
eatme
Tr
Accident Compensation Corporation
Page 53 of 128
ACC Treatment Provider Handbook 2016
Mental injuries, sensitive claims and counselling
Definition of mental injury
A mental injury is defined as a “clinically significant behavioural, cognitive, or psychological
dysfunction”. ACC covers the effects of a mental injury from an event rather than the event
itself.
Client eligibility
ACC funds counselling under the
Regulations for:
mental injuries arising from physical injuries or workplace events
sensitive claims, i.e. mental injuries arising from certain criminal acts listed in
Schedule 3 of the
AC Act.
When a person’s mental injury has been caused by sexual abuse, they can lodge their
claim through a medical practitioner, an ACC-registered counsellor or a provider who
delivers services via the Integrated Services for Sensitive Claims (ISSC) contract.
Immediate help can be accessed through ISSC by self-referral. The Find Support
website
provides information about providers who deliver ISSC services and their locations.
Sensitive claims counsellors can choose to work under:
an ISSC contract with a supplier, and/or
the
Regulations.
What are the differences between the Regulations and the ISSC contract?
The Regulations and the ISSC contract refer to ways that ACC can purchase sensitive
claims counselling services. The differences between the Regulations and the ISSC
contract are particularly important for providers treating clients with sensitive claims.
The table below explains some of the key differences between the two purchasing
methods.
The Regulations
ISSC contract
Consolidation of
The Regulations were introduced This contract was introduced on
services
in 1999 and replaced in 2003.
24 November 2014. It ties
Along with the
Accident
together all the services that
Insurance (“Counsellor”)
were in different sensitive claims
Regulations 1999, they
contracts, and for the first time
determine who can deliver
includes counselling services
services and how much ACC can and social work.
pay for them.
nt
Client payments
May require co-payments from
A client co-payment can’t be
and co-payments
clients.
charged by a provider (ACC
funds sessions to the amount
eatme
specified in the contract).
Tr
Accident Compensation Corporation
Page 54 of 128
ACC Treatment Provider Handbook 2016
The Regulations
ISSC contract
ACC provider
Providers are paid by the hour
Providers are paid at a new rate.
payments
and only for face-to-face time
with clients.
The rate incorporates things
such as administration and time
There are no separate payments spent on client referrals. There is
for clients who don’t attend their
some partial compensation for
appointments or for
client sessions where clients
administration, referrals or
don’t attend and for providers to
contacting other agencies on
travel to see clients.
clients’ behalf.
Clients accessing
For a counsellor accepted to
For a counsellor accepted to
support for the first deliver counselling services
deliver counselling services
time
under the
Regulations, ACC
under the ISSC contract there is
provides a one-off lodgement fee the ability to offer pre-cover,
for the first session when they
treatment and additional support
submit an ACC45 Injury Claim
services that are fully funded for
form on behalf of a new client.
clients.
This client will then be referred to
the ISSC contract. If a client with
an accepted claim returns for
further counselling the counsellor
will be able to offer treatment
services.
Mental injury caused by physical injury and work-related mental injury
In making a cover decision for a person who has a mental injury caused by a physical
injury or through a traumatic event at work, we need at least two medical reports:
a report from the person’s treating practitioner
a comprehensive assessment by a registered psychiatrist or clinical psychologist,
usually contracted to ACC.
After receiving the treating medical practitioner’s report, we may make a referral for an
assessment from a psychiatrist or a clinical psychologist. The assessment is designed to
help us understand more about the injury’s clinical significance and the causal link to the
event. We may also seek appropriate treatment recommendations.
Exception
The only exception to this process is when a treating practitioner advises that there is no
nt
clinically significant mental condition.
In this case we may decline the claim without a psychiatric report as long as we have
eatme
confirmation from an ACC medical advisor that it’s appropriate to do so. The decision will
Tr
depend on the facts of each situation. For example, when the advice is from a GP, a claim
will likely only be declined if they have had recent and regular contact with the client.
Accident Compensation Corporation
Page 55 of 128
link to page 88
ACC Treatment Provider Handbook 2016
Treatment options
The recommended treatment options outlined in the psychiatric report can include referral
to a counsellor, psychotherapist, psychiatrist or psychologist for treatment or counselling.
We can contribute to the funding of treatment if the provider is registered with us to provide
counselling services under the
Regulations or the ISSC contract. We’re unable to fund
services for non-registered providers.
For a full list of ACC-registered counsellors, call the Provider Contact Centre on
0800 222
070.
For a full list of ISSC suppliers, go to Find Suppo
rt website.
To find out more about registering as an ACC counsellor, see
Counsellor registration or
contact the Provider Registration team on
04 560 5211 or by emailing
[email address].
To find out more about how to become a contracted ISSC-named provider, please email
[email address].
Sensitive claim injuries
A sensitive claim is a mental and/or physical injury caused by a sexual abuse crime such
as sexual violation, indecent assault and unlawful sexual connection.
Because these claims are confidential and personal in nature, we have a special Sensitive
Claims Unit to help people with these injuries. The claims can often be complicated. ACC
staff may need to gather more information than what’s collected on an ACC45 Injury Claim
form or the Engagement form completed when a person accesses ISSC. As a result it can
take longer to determine cover for these claims, so the legislation makes allowances for
this.
Sexual abuse crimes considered by ACC are listed in
Schedule 3 of the AC Act. ACC staff
may refer to the ‘event’ as a ‘Schedule 3 event’.
If you have any questions about a claim like this or wish to direct a patient to ACC for
confidential advice, phone the Sensitive Claims Unit on
0800 735 566 option 1.
Crisis care and early intervention
If your patient is distressed and there are serious concerns for their safety, contact the
Crisis Assessment and Treatment Team (CATT) at your regional DHB. Each DHB has its
own team and details are available on all DHB websites.
The CATTs provide 24-hour, seven-day assessment and short-term treatment services for
people experiencing serious mental health crises who have urgent safety issues.
ACC also funds early medical and forensic assessments and follow-up treatment through
nt
the Sexual Abuse Assessment and Treatment Service (SAATS). This service is delivered
by Doctors for Sexual Abuse Care (DSAC) doctors and nurses under local DHBs. DSAC
doctors and nurses are specifically trained in managing sexual assault cases. You can
eatme
refer patients to SAATS by contacting the local DHB or Police.
Tr
Accident Compensation Corporation
Page 56 of 128
link to page 37
ACC Treatment Provider Handbook 2016
Lodging a sensitive claim
Medical practitioners and ACC-registered counsellors can lodge sensitive claims on an
ACC45 Injury Claim form. ISSC-named providers can lodge sensitive claims by completing
an Engagement form.
GPs and counsellors can get help with lodging sensitive claims from two ACC guides:
ACC1149 GPs’ Guide to Completing the ACC45 Injury Claim Form For a Sensitive
Claim
ACC1363 Counsellors’ Guide to Completing the ACC45 Injury Claim Form For a
Sensitive Claim.
You’ll find them in the ‘Forms & fact sheets’ sidebar in the ‘Lodge a claim’ section of our
website.
When describing a criminal act
Important: When lodging a sensitive claim, describe the criminal act and/or the relevant
section listed in
Schedule 3 of the AC Act. The cover decision process is likely to be
delayed if you use simplified wording such as ‘sexual abuse’, fail to describe the criminal
act or give unclear details of a mental injury diagnosis.
When providing a preliminary mental injury diagnosis:
if you’re unsure about identifying a preliminary mental injury diagnosis, or are not
qualified to provide one, please use clinically relevant terms to the best of your ability
if in doubt, over-describe the symptoms, as this is likely to provide the most useful
information to help us determine cover. Use a DSM-IV diagnosis, an ICD code, a
Read Code or any other relevant diagnostic classification tool
at the various stages of seeing the patient, you should always check whether their
contact details need updating.
Ensuring client safety and privacy
Given the nature of these claims, ask your patient for a safe address, which may be
different from the one you have on record.
This is particularly important for clients aged between 13 and 16; we prefer a
caregiver/guardian and/or family/whānau to be involved if possible.
Who can sign the ACC45 Injury Claim form?
Only the patient or their legal representative can sign the ACC45 Injury Claim form.
If your patient is under 16, their parent or guardian must sign for them.
If any other person signs, or there’s no signature, we won’t be able to register the claim
nt
and will return the form to you.
Before sending us the form
eatme
To avoid any delays it’s really important to double-check that all mandatory sections have
Tr
been completed (e.g. whether the patient is working).
Accident Compensation Corporation
Page 57 of 128
link to page 64
ACC Treatment Provider Handbook 2016
Dealing with challenging behaviour
Dealing with an aggressive patient
Patient violence against providers is uncommon in New Zealand. However, some
providers may find themselves on the receiving end of verbal abuse and, on rare
occasions, physical assault. Dealing with an aggressive or violent patient can be a huge
challenge for you and your practice colleagues.
In most cases patients are keen to get back to everyday life or work. Others, owing to
injury or debilitation, take out their frustrations on treatment providers and may blame the
broader accident compensation and rehabilitation system.
There may or may not be a direct connection between a patient’s behaviour and their
presenting condition. Abusive or threatening behaviour can also stem from compensation
issues such as entitlement, eligibility for treatment or investigation, the legitimisation of a
claim, and issues of cooperation in rehabilitation.
How we can help
It’s important that you let us know about any violent and/or aggressive patient who’s also
our client. We can help you to assess the situation and determine whether other known
factors are contributing to the hostility.
If mental injury is a factor
If a patient has developed a mental illness post-injury, and this appears to contribute
significantly to their aggression or violence, we can help by providing a psychiatric
evaluation and therapy or a psychologist referral. In this case our staff can be crucial in
working with you to rehabilitate the patient and help with your patient relationship.
If pain is a factor
If chronic pain resulting from an injury is central to a patient’s frustration and escalating
hostility, we can offer pain management options. This type of support could help you with
returning your patient to everyday life and work. For more information see
Managing pain.
We also train our client service staff to deal with difficult and hostile clients, so they can
support you in getting information from these patients. ACC staff usually hold interviews in
rooms that offer some protection and security for participants.
Preventing or handling attacks
Sudden, violent attacks are rare; most incidents are preceded by mounting tension and
frustration or escalating threats. To help you recognise the warning signs and take
appropriate action, practical guides are available through many professional bodies,
including the
New Zealand Medical Association and the
Royal New Zealand College of
nt
General Practitioners. Working and communicating with a patient, their family/whānau,
associated staff and other providers can go a long way to reducing or eliminating the
patient’s hostility.
eatme
Tr
Accident Compensation Corporation
Page 58 of 128
ACC Treatment Provider Handbook 2016
For example, there are steps that you can take before a patient arrives, when they make
appointments, when they’re on your premises, while the consultation/visit is underway, and
if they become violent.
Here are some essential points to remember and develop in assessing the risks of and
managing these situations:
Anticipate
Make sure you and your colleagues are always aware that you could
encounter an aggressive or violent patient, and have mechanisms in place
to deal with them.
Detect
Detecting high-risk patients early and implementing harm-reduction
measures can stop threatening behaviour escalating into full-blown
violence.
Analyse
Try to identify the factors that promote or encourage aggressive or violent
tendencies in a patient. A careful analysis of patient, practice and provider
features may identify the cause of the problem and enable management
strategies that benefit you and your patients.
Team
Take a team approach to planning and managing aggressive and violent
patients.
Support
Get appropriate support if a patient becomes aggressive or threatens
violence, e.g. from the Police, ACC, the New Zealand Medical Association,
the Medical Council of New Zealand or other provider bodies.
Prevent and
Effective prevention and appropriate action are crucial when dealing with
act
violent and aggressive patients.
Practise and
Develop and practise strategies to make sure you and your staff know how
be prepared
to respond and keep yourselves safe.
Contact us
Call the Provider Contact Centre on
0800 222 070 as soon as possible to
let us know what’s happened. Make sure you speak directly to one of our
staff.
Pharmaceuticals
ACC’s definition
Pharmaceuticals are described in the
AC Act as:
prescription medicines, restricted medicines or pharmacy-only medicines, as listed in
Parts 1, 2 and 3 of
Schedule 1 of the Medicines Regulations 1984
nt
controlled drugs as defined in the
Misuse of Drugs Act 1975.
Helping with costs
eatme
ACC may be able to contribute to prescription costs for clients who are prescribed
Tr
medication to help them recover and rehabilitate after injury.
Accident Compensation Corporation
Page 59 of 128
ACC Treatment Provider Handbook 2016
To be eligible for assistance your patients will need to complete the
ACC249 Request for
Reimbursement of Pharmaceutical Costs form.
This comes with an information sheet explaining what reimbursement we offer, and what
we need to be able to reimburse costs, e.g. the receipts and invoices that need to be sent
with the form.
How we decide to reimburse
ACC will consider helping with the cost of pharmaceuticals if a claim has been accepted
and the item prescribed:
is reasonably required to help the client’s treatment or rehabilitation based on their
injury and clinical information
is prescribed within the scope of practice of the prescribing provider
is classified as a prescription medicine, restricted medicine, pharmacy-only medicine
or controlled drug
follows best-practice prescribing protocols
follows best-practice rehabilitation pathways.
We’ll also consider the availability of similar pharmaceuticals and generic alternatives
listed in the
Pharmaceutical Schedule.
If there isn’t enough information to support a reimbursement request, we may ask for more
information.
What we’re unable to reimburse
We’re not able to reimburse any administration charges added by the prescriber or
dispensing pharmacy, or the cost of substances not considered pharmaceuticals, such as
herbal remedies and complementary medications
How we contribute to costs
We pay for clients’ pharmaceuticals in several ways.
By contract
If the contract includes providing pharmaceuticals, we’ll pay the contracted price. Clients
shouldn’t be charged pharmaceutical costs if the contract price covers pharmaceuticals.
By reimbursement
We reimburse clients or pharmacies:
for co-payments on community pharmaceuticals
as a contribution towards part-charges for partly subsidised community
pharmaceuticals
nt
as a contribution towards pharmaceuticals that aren’t on the
Pharmaceutical
Schedule or that don’t meet its subsidy criteria, as long as we’ve pre-approved them.
eatme
Tr
Accident Compensation Corporation
Page 60 of 128
ACC Treatment Provider Handbook 2016
Via Public Health Acute Services (PHAS)
The bulk amount that we pay to the Crown via the PHAS agreement covers
pharmaceuticals that are:
required by clients during acute hospital admissions or emergency department visits
given as part of the treatment associated with clients’ outpatient follow-ups for up to
six weeks from discharge or treatment
used during treatment given by medical practitioners less than seven days after
referrals by other medical practitioners
listed on the
Pharmaceutical Schedule, meet its subsidy criteria and are used in the
community.
Pharmacies, clients and other providers don’t need to invoice ACC for these
pharmaceutical costs as they’re already paid for under the PHAS agreement.
When you’re prescribing medicines
When prescribing medicines please record:
the ACC45 Injury Claim form number against each item
a Ministry of Health identifier for all medical illness scripts to distinguish between
accident and medical cases.
When to seek prior approval
Prior approval is needed for all non-subsidised pharmaceuticals
If a patient needs non-subsidised pharmaceuticals not already covered by the PHAS time
period or under another ACC contract, we may be able to reimburse the costs partially.
You’ll need to seek funding approval from us before prescribing the pharmaceuticals. If
you prescribe them without our prior approval, we ask that you let the patient know that we
may not be able to contribute to the cost.
Requesting funding for non-subsidised pharmaceuticals
To apply for prior approval, complete
an ACC1171 Request for pharmaceutical funding
form with your patient.
We’ll need to know how the non-subsidised medication will help treat the injury and why
other subsidised medication is unsuitable. This type of approval is for a limited time only.
Things to note when prescribing
When prescribing please ensure that you:
prescribe subsidised pharmaceuticals that meet the
Pharmaceutical Schedule criteria
nt
for community pharmaceutical use
always apply for PHARMAC special authority when this is available
code prescriptions as A4 – all our clients are eligible people in New Zealand, including
eatme
non-residents whose injuries are covered by ACC.
Note: You’ll need to change the code on the script if it’s computer generated and
Tr
you’ve categorised the client as non-resident in your practice management system
Accident Compensation Corporation
Page 61 of 128
ACC Treatment Provider Handbook 2016
(PMS)
prescribe generic names rather than brand names, e.g. diclofenac tablets, not
Voltaren tablets. If this means your client needs a new generic brand, you may need
to support their changeover. Information is available from the PHARMA
C website
support patient adherence – use the tool at the National Institute for Health and Care
Excellence
website
prescribe small quantities when trialling new medicines
report adverse reactions to the Centre for Adverse Reactions Monitoring, PO Box
913, Dunedin 9054.
nt
eatme
Tr
Accident Compensation Corporation
Page 62 of 128
ACC Treatment Provider Handbook 2016
7.
Rehabilitation
Work and rehabilitation
ACC’s definition of rehabilitation
Rehabilitation is the term we use to cover the overall process of helping clients to return to
work or, if they weren’t working at the time of their injuries, to independence in their daily
lives as much as possible.
Rehabilitation can involve combinations of:
treatment for the effects of an injury
specialised inpatient rehabilitation
support to maintain employment
support to obtain employment
education support
support to regain independence
support in everyday living activities.
It’s a dynamic process in which we involve treatment providers and help make connections
to other providers. It recognises that one clinician or organisation can seldom meet a
client’s total needs in isolation.
Our rehabilitation framework
Our clients’ circumstances vary greatly according to injury, health, work and other factors.
We’ve created a range of pathways to make it easier to tailor the best support for each
person and help them to achieve the results that will be of the most benefit to them.
Together, the pathways fit into an overall rehabilitation framework. The table below
summarises the core concepts as developed in conjunction with stakeholders and staff:
Intent
Rehabilitation framework principles
An inclusive relationship of Rehabilitation is based on listening to, and understanding,
support
the person in the context of their personal circumstances and
community.
A service approach based
ACC works with the person and their family, employer and
on client need
provider to plan and deliver the agreed rehabilitation tailored
to the individual.
ACC acts as a partner and We mobilise existing support and provide any additional
on
facilitates the expertise of
support and services needed to help people return to
others
productive lives.
tatiil
Rehabi
Accident Compensation Corporation
Page 63 of 128
link to page 65
ACC Treatment Provider Handbook 2016
Rehabilitation and you
Your involvement in helping our clients to rehabilitate
As a treatment provider you may be involved with our clients at various stages of their
rehabilitation.
You may initiate rehabilitation yourself by treating an injury or make a referral to elective
surgery or other specialists.
The clients might also need social and vocational rehabilitation services. Through your
understanding of their needs you can help us to identify where support in their
environment could help them.
Managing pain
At all stages of rehabilitation you should consider whether there are any pain-related
disability factors that could inhibit the client’s progress. We have a number of pain
management services to which you can refer patients, or you can let us know your
concerns so we can help you to choose the best option.
For more information, see ou
r website and
ACC4467 Pain management quick reference
guide to our services.
Vocational rehabilitation
Vocational rehabilitation aims to help clients to maintain or obtain employment. The range
of tools and programmes spans:
helping clients to rehabilitate at work, e.g. via the
SAW service
helping clients to rehabilitate who have to consider different work
re-training clients when necessary to help them to find different work.
When clients have some capacity to work and are at low risk of re-injury, we can work with
employers to arrange alternative work duties or hours.
Clients might need ongoing help to return to work, including: return-to-work monitoring; a
graduated return-to-work programme; work trials; agreed recovery initiatives such as
lifestyle changes, help with workplace access or adaptation; and other equipment to
enable their independence.
ACC, or sometimes another contracted provider, may ask you to verify that a client is
medically fit for a vocational rehabilitation programme.
If a client’s return to work isn’t progressing as expected, discuss it with us. There may be
other options such as pain management services.
on
tati
Assessing a client’s work capacity – overview
il
As part of a client’s rehabilitation we’ll ask an appropriately skilled treatment provider to
assess their capacity to work. We might also ask them to assess any medical grounds on
which we can compensate the client while they’re unable to work.
Rehabi
Accident Compensation Corporation
Page 64 of 128
ACC Treatment Provider Handbook 2016
The Stay at Work service
The Stay at Work (SAW) service aims to help ACC clients to recover from injury in the
workplace.
SAW service providers visit clients and employers at their workplaces and review the work
tasks and environment. Their aim is to establish a clear picture of the tasks the clients can
and can’t do safely, and whether there are barriers preventing their recovery at work.
A good early intervention is the SAW level 1 service, in which SAW service providers help
clients and employers to develop suitable return-to-work plans, including possible short-
term modifications to the employees’ work tasks.
SAW level 2-4 services are longer term, cover more complex needs and require progress
reports from providers. Levels 3 and 4 are multidisciplinary programmes that include both
functional and vocational rehabilitation components and monitoring of clients’ returns to
work.
SAW service providers
SAW service providers have a range of backgrounds. They’re registered or certified
members of their chosen fields, have ergonomic and health and safety expertise and are
skilled in working with injured people in the workplace.
Assessing a client’s disability duration – resources
Tools to help you assess the duration of incapacity include:
treatment profiles for some primary care professions
the
ACC14191 Return to Work Guide first published in May 2006.
These help to summarise the current best practice for common injuries and provide a
starting point for managing a client’s rehabilitation at work or their return to work with ‘time
off work’ certification.
They should be used when possible. If you’d like paper copies, please phone the
Stationery Order Line on
0800 802 444 option 0.
Factors that influence disability duration
The duration of a disability can be affected by factors such as dominant versus non-
dominant arm, work requirements (use of wrist, forearm), conservative versus surgical
treatment, and compliance with the rehabilitation programme.
There is a minimum recovery time that most people will need to return to work at the same
performance levels as before their injuries. Clients may be fit to return to work in shorter
on
timeframes, particularly if there are suitable selected or modified duties or other support.
tatiil
Likewise there is the time identified when most people are likely to be able to return to
work, subject to good health care and no significant complications and/or co-morbid
medical conditions.
Rehabi
Accident Compensation Corporation
Page 65 of 128
ACC Treatment Provider Handbook 2016
There is a time at which additional reviews and evaluations should occur to determine
when (and if) clients may be able to return to work and whether there are specific factors,
including psychosocial, that need to be addressed.
Definitions for degree of work
For details on work types see ou
r website. The work types are listed at the bottom of that
page.
Work type
Definition
Sedentary
Exerting up to 4.5 kilograms (kg) of force occasionally and/or a negligible
amount of force frequently or constantly to lift, carry, push, pull or
otherwise move objects, including the human body. Involves sitting most
of the time, but may involve walking or standing for brief periods.
Light
Exerting up to 9kg of force occasionally and/or up to 4.5kg of force
frequently, and/or negligible amount of force constantly to move objects.
Physical demand requirements exceed those for sedentary work.
Usually requires walking or standing to a significant degree. However, if
the use of any arm and/or leg controls requires exertion of forces greater
than those for sedentary work, and the worker sits most of the time, the
job is rated light work.
Medium
Exerting up to 22.5kg of force occasionally and/or up to 9kg of force
frequently and/or up to 4.5kg of force constantly to move objects.
Heavy
Exerting up to 45kg of force occasionally and/or up to 22.5kg of force
frequently and/or up to 9kg of force constantly to move objects.
Very heavy
Exerting over 45kg of force occasionally and/or over 22.5kg of force
frequently and/or over 9kg of force constantly to move objects.
Frequency scale for degree of work example
This table gives an example of how often the degree of work can apply to a client when
their work type work capacity and disability duration are being assessed.
Frequency
% of an 8-hour day
Example
Occasional
0-33
One lift every 30 minutes
Frequent
34-66
One lift every two minutes
on
tatii
Constant
67-100
One lift every 15 seconds
l
Rehabi
Accident Compensation Corporation
Page 66 of 128
link to page 67 link to page 48 link to page 37
ACC Treatment Provider Handbook 2016
Medical certificates (ACC18s)
Why medical certificates are important
Medical certificates (ACC18s) are important because they verify that clients are entitled to
ongoing ACC weekly compensation while they’re off work recovering.
Following your clinical assessment you can use an
ACC18 Medical Certificate form to:
alert us early that a client might need extra rehabilitation support so we can look at
the options
recommend home help, personal care, a second opinion or an assessment for the
client
change a diagnosis or add a diagnosis to a covered injury
make changes or corrections to the origina
l ACC45 Injury Claim form.
We encourage you to use the spaces provided on the form, as well as other
communication methods, to give us your views on a client’s needs. If you’re unsure about
specifics, please still pass on any general concerns to our case owners.
Confidential discussions
If you’d like to talk to us about matters that you’re not comfortable writing in a client’s
ACC18 Medical Certificate form, please tick the option ‘I would like to discuss this with the
client’s case owner’.
In complex cases it can be in the client’s interests for you to meet our staff, rehabilitation
experts, the client, their family and others in a case conference facilitated by ACC.
How medical certificates work
When clients need time off work to recover from their injuries, the medical certificates
validate this and specify
tasks or exposures the clients should avoid while recovering.
They also allow us to provide workers with compensation for lost income while they’re off
work. Please emphasise to clients that the sooner they send us their ACC18 Medical
Certificate forms, the sooner we can process their applications for compensation.
Only a medical practitioner (e.g. GP, specialist or emergency department doctor) or nurse
practitioner can complete an ACC18 Medical Certificate form. The practitioner records the
client’s incapacity details on the required form:
the ACC45 Injury Claim form if this is the client’s first visit. This can be used to certify
incapacity for up to 14 days
the ACC18 Medical Certificate form if an ACC45 Injury Claim form has already been
lodged. The ACC18 form provides a detailed description of how the client’s injury
on
affects their capacity for work and their prospects for rehabilitation.
tatii
The ACC18 Medical Certificate form must show:
l
that the client’s examination was done in person, not by phone or based on third-party
reports
Rehabi
your clinical assessment following the examination – this should be in line with the
relevant treatment profile, including your diagnosis, comments and recommendations
Accident Compensation Corporation
Page 67 of 128
link to page 48 link to page 48 link to page 40 link to page 48 link to page 48
ACC Treatment Provider Handbook 2016
to meet the overarching needs of care.
How to fill in an ACC18 Medical Certificate form
Give a confirmed diagnosis
After you’ve examined the client, enter a Read Code and/or a diagnosis (preferably both)
on the form. You can also use the ACC18 Medical Certificate form to
add or change a
diagnosis. If you do, you’ll need to
record a new Read Code along with the
supporting
clinical evidence.
Get work information
Find out:
the type of work the client does and the tasks involved
key facts about their work history (tasks, skills)
what their work environment is like
any problems or injuries they had before the accident
any concerns or fears they have about returning to work
what tasks they can still do.
An ACC18 Medical Certificate form can help you to gather this information. It provides you
with an early opportunity to advise us about possible risk factors in the client’s work that
could affect their rehabilitation.
Indicate a client’s capacity for work
If a client can’t do the job they had before their accident they may still have other work
options, so it’s important to indicate whether they have a capacity for work.
Marking that they have some capacity (i.e. are fit for selected part-time or alternative work)
enables us to negotiate with all parties for the client to return to other available duties
within the medical limitations imposed by the injury. This doesn’t mean that we’ll stop their
weekly compensation payments. When negotiating a partial return to work we’ll need to
ensure that payment levels are appropriate and in line with the client’s entitlement.
If the client doesn’t think there are light duties available, contact us so that we can discuss
this with their employer and look at alternatives.
Determine fitness for work
To be fully unfit for work the client must be unable to:
travel to and from work
be at the workplace
on
do specified tasks at the workplace.
tatii
If you identify only one or two of these points we can look at ways to help the client
l
overcome these barriers. It’s important that we know their functional limitations, e.g. if they
can’t lift more than 10 kilograms, lift above shoulder height or stretch etc.
Rehabi
Important: We recommend that you and the client each keep a signed copy for your
records.
Accident Compensation Corporation
Page 68 of 128
link to page 73
ACC Treatment Provider Handbook 2016
Specify the time off work
Time off work is usually certified from when the client first presents with an injury until the
next scheduled consultation/visit, usually two weeks or less.
If they have a severe or chronic condition you may need to certify a longer period, usually
a maximum of 13 weeks. However, in some cases – such as if the client has a serious
injury – they may need medical certificates at intervals of more than 13 weeks, e.g. at six-
or 12-monthly intervals. The case owner will let you know if the client meets the criteria.
A client can have a medical certificate for more than 13 weeks (up to a maximum of 12
months) if:
their functional restrictions have stabilised and are likely to remain unchanged
these restrictions mean they can’t perform any work
their eligibility for long-term entitlements isn’t in doubt.
Highlight next steps towards a return to work
Estimate when you expect the client to be fit for normal work. This helps us to negotiate
with their employer and develop appropriate rehabilitation and return-to-work programmes.
The client’s return to work should always focus first on their pre-injury employment role,
tasks and hours. If the client can’t do their usual tasks or hours, options include part-time
wo
rk, vocational rehabilitation services and temporary alternative duties.
See the
certification page on our website for more information.
Submitting the ACC18 Medical Certificate form online
1. You can send us the form through a BPAC (Best Practice Advocacy Centre) module
in your PMS
2. If you don’t have a PMS, you can access the eACC18 via the stand-alone form
hosted by BPAC
3. To set up either, please contact BPAC directly on
0800 633 236; they will be able to
arrange access for you.
When you use the eACC18 online, the form is received immediately after you press
‘Submit’.
Three documents are produced for you:
1. ACC/Patient copy
2. Employer copy
3. Patient declaration.
To print a copy for the client and their employer, go to the stored documents and print as
on
you would any document.
tatiil
ACC doesn’t require you to keep paper copies with written signatures; however, there is a
mandatory tick-box in the Declarations tab that has to be checked before you can submit
the eACC18.
Rehabi
Accident Compensation Corporation
Page 69 of 128
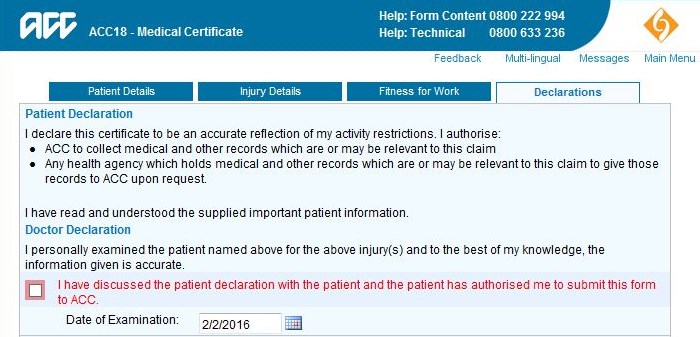
ACC Treatment Provider Handbook 2016
The patient declaration is available in 14 languages from the ‘Multi-lingual’ link at the top of
the eACC18.
If you’d like any more information on the eACC18, please contact our eBusiness Support
team on
0800 222 994 option 1 or email
[email address].
Using the paper ACC18 Medical Certificate form
Give the paper form to the client to either post or deliver to us. Emphasise to them that the
sooner they get the form to us, the sooner we can process their application and begin any
compensation payments. You can also give them a copy to keep.
When using a paper copy the client must sign the consent section, declaring that the
information they have given is true and correct and authorising us to collect all relevant
information. We recommend that, for audit purposes, you keep a signed copy of this form
in paper or image format.
Sustained return to work
Helping your patients to return to work
The benefits of early return to work are recognised by health professionals and employers.
Modern practice supports safe and sustainable work that quickly integrates people back
into their workplaces and their normal lives.
Informed
work fitness certification is vital to opening the doors to the range of vocational
rehabilitation services that ACC can deliver to your patients.
on
Returning to work after an injury has to be sustainable if it’s to be successful. To establish
your patient’s work capacity there are a few things you can do:
tatiil
1. Get in touch with their employer to:
understand the specific demands of their job
Rehabi
identify any barriers to returning to work
troubleshoot the barriers
Accident Compensation Corporation
Page 70 of 128
link to page 72 link to page 72
ACC Treatment Provider Handbook 2016
2. Let us know if barriers are identified
3. Let the case owner looking after your patient know if you’re unable to make contact
with the employer.
There’s a lot of good information on supporting and coordinating an effective return to work
in the
ACC2360 Return to Work Guide, which was developed by both ACC and treatment
providers. It includes best-practice information and practical help for managing
rehabilitation and supporting your decisions.
Understanding the demands of your patient’s job
The first step in assessing your patient’s ability to return to work involves identifying their
work tasks. These might include things like sitting, standing, climbing a ladder, lifting heavy
loads or working on a keyboard most of the day.
‘Work type detail sheets’ are available to help you. They specify tasks for various work
categories and can be found on ou
r website (scroll to the bottom of the page).
Check if the patient can complete any of their employer’s minimum requirements.
Observing directly is the most accurate way to do this.
How to identify return-to-work barriers
A number of barriers can affect a patient’s fitness to return to full, partial or graduated work
activities. A vocational/occupational provider may need to be involved. They will consult
you and any rehabilitation providers involved in your patient’s care on the following:
Disability and physical impairment
Residual impairments can stop a client returning to work fully. It’s important to diagnose
these and seek the help of providers with appropriate expertise to manage the
rehabilitation.
Injury factors
Injury factors include safety, biomechanical, cognitive, perceptual and functional
limitations. Pain itself isn’t a contraindication to activity and work. If you identify specific
safety concerns they may apply to only part of the job. Identifying the part(s) of the job that
the client can still do is an important starting point for returning them to work part time or
using a graduated approach.
Individual factors
Individual factors include the client’s beliefs about their injury and symptoms, e.g. their
fear
of pain from movement. A client may believe that pain intensity signals significant damage
to the body and that all activity and work must be avoided until the problem is completely
on
fixed. This means they often respond to the anticipation of pain, which engenders a ‘fear-
and-avoidance cycle’.
tatiil
In these cases you should consider prescribing appropriate pharmaceuticals as part of
your response and ensure they’re being used correctly.
Rehabi
Accident Compensation Corporation
Page 71 of 128
link to page 72
ACC Treatment Provider Handbook 2016
Workplace factors
Workplace factors include job satisfaction, work organisation issues and relationships with
managers and co-workers. An employer’s willingness and/or ability to offer temporary
modifications to work tasks are critical.
For an example of how to complete a return-to-work plan with your patient, see Appendix 3
of the
ACC2360 Return to Work Guide.
Advising us of barriers preventing return to work
If your patient has ongoing restrictions or specific limitations, please let us know so we can
get in touch with their employer to arrange duties and a phased return to work as
appropriate.
A phased programme may involve:
selected or alternative duties, meaning the tasks they can still do become the
temporary focus of their work
a graduated return to work, where they undertake full or selected duties for part of the
day and steadily increase these over a few weeks. With this option it’s important to
keep to the usual work starting time
a programme that provides an individual return-to-work plan containing physical and
vocational rehabilitation targets
part-time work, which is considered a temporary last resort and only used in
exceptional circumstances, such as when the patient is suffering significant fatigue or
serious medication side-effects. See
Lifestyle substitution.
Our main focus is to return your patient to a full day of selected duties and activity rather
than a limited day of full duties.
Dealing with return-to-work barriers
Fear of pain from movement
If there are no specific safety concerns your patient’s activity levels should be based on
time rather than pain. They should be given clear guidelines on steadily increasing their
activity level to avoid the risk of ‘disuse or inactivity syndrome’ developing from a long-term
withdrawal from activity. Reassurance, motivation and encouragement can often help to
counter this problem.
Lifestyle substitution
A graduated return to work may not advance beyond, for example, a four-hour day, but it
enables your patient to experience the benefits of work while avoiding the lifestyle
pressures associated with working longer hours.
on
To change this pattern, ask them to work a full day followed by a short day, then steadily
tatiil
move towards every day being a full day.
Workplace barriers
Rehabi
An ergonomic review of the organisation and processes of the workplace might be
needed. These might not have caused the injury but could be barriers to a full and
Accident Compensation Corporation
Page 72 of 128
ACC Treatment Provider Handbook 2016
sustainable return to work. Health professionals who specialise in the work environment
will usually conduct these reviews. You can contact your patient’s case owner to discuss a
workplace assessment.
Please watch carefully for other return-to-work barriers. Anecdotal evidence indicates that
highly motivated people (such as the self-employed) return to work more quickly than other
groups of workers. However, some of these may need close monitoring to ensure they
modify their workloads temporarily and don’t end up prolonging their recovery.
Support is important within the first few days, as this is when most return-to-work problems
occur. Many concerns can be resolved by contacting your patient’s ACC case owner
and/or their employer (manager or supervisor). If this fails, you might consider a referral to
a health professional specialising in the work environment.
Referral and rehabilitation services
Other health professionals involved
A number of health professionals specialise in the work environment, including:
occupational health nurses
occupational physicians
occupational physiotherapists
occupational therapists
vocational rehabilitation providers.
Your patient’s problems will indicate which provider is the most appropriate. Please
contact their case owner to discuss any referral, as you might need prior ACC approval.
Vocational rehabilitation services
Some of the most common assessment, service and/or rehabilitation programmes
available to ACC clients are described in the table below. In almost all cases these are
provided by contracted providers. The provider criteria in the table indicate the contract
types.
Service
Purpose
Provider criteria
Initial Occupational
Assesses clients’ education, training
Occupational assessor
Assessment
and work experience and identifies
suitable work types.
Initial Medical
Follows an initial occupational
Medical assessor
Assessment
assessment and helps to determine
clients’ vocational rehabilitation
on
needs. It assesses the clients’
medical and injury-related conditions
tatiil
and any non-injury-related barriers to
ensure they can sustain rehabilitation
medically and with safety.
Rehabi
SAW 1 and 2
Evaluate and review workplaces,
Rehabilitation
then implement supervised increases
Accident Compensation Corporation
Page 73 of 128
ACC Treatment Provider Handbook 2016
in hours with the clients via
professional
documented plans, including
troubleshooting.
SAW 3 and 4
Evaluate clients’ workplaces and
Rehabilitation
involve key work contacts in
professional
identifying changes needed to make
the environments safe, or for the
clients to return to work. They are
multidisciplinary services where
functional rehabilitation is provided
alongside monitoring of the clients’
return to work.
Vocational Medical
Allows certifying practitioners and
Medical practitioner
Review
claim managers to request expert
with vocational training
medical views of clients’ fitness for
work. The service helps clients to
return to work quickly and safely
following injury. The vocational
medical review provider consults all
parties to ensure agreement on
fitness for work.
Work Readiness
Helps clients to become work ready,
Vocational practitioner
Programme
even if they’re not expected to return
to their pre-injury jobs or can’t
maintain their current jobs due to
injury-related factors after all
practicable rehabilitation has been
completed.
Social rehabilitation services
Some of the most common assessment, service and/or social rehabilitation programmes
available to ACC clients are described in the table below. In almost all cases these are
provided by contracted providers. The provider criteria in the table indicate the contract
types.
Service
Purpose
Provider criteria
Equipment
Provides equipment, aids and
Contracted provider
appliances based on clients’
assessed needs to support their
on
rehabilitation.
tatiil
Home and Community
Provides high-quality, flexible support Contracted provider or
Support Services
services in clients’ homes and
personal carer
communities to support rehabilitation
and help them return to ‘everyday
Rehabi
life’. Services include home help,
Accident Compensation Corporation
Page 74 of 128
ACC Treatment Provider Handbook 2016
attendant care and child care.
Housing modifications
Provide project management and
Contracted consultant
advice for housing modifications
approved by ACC, such as the
removal of structural barriers or
addition of fixed features that are
based on clients’ assessed injury-
related needs.
Inpatient non-acute
A service for clients who, as a result
DHBs and some trust
rehabilitation
of personal injury, require fast-stream hospitals
inpatient rehabilitation in a
rehabilitation unit.
Social rehabilitation
Recommends to ACC the most
Contracted provider
assessment
appropriate and cost-effective
combination of social rehabilitation
services to enable clients to achieve
the expected outcomes in the most
rapid and durable manner.
Specialised rehabilitation services
Some of the most common assessment, service and/or specialised rehabilitation
programmes available to ACC clients are described in the table below. In almost all cases
these are provided by contracted providers. The provider criteria in the table indicate the
contract types.
Service
Purpose
Provider criteria
Concussion service
An interdisciplinary traumatic brain
Multidisciplinary
injury (TBI) service. The service aims providers
to prevent long-term consequences,
such as post-concussion syndrome
(PCS) by identifying clients at risk of
PCS and giving them effective
interventions and education.
Spinal cord injury
The spinal cord injury rehabilitation
Multidisciplinary
rehabilitation service and service provides non-acute, inpatient providers
spinal reassessment
rehabilitation services for clients
service
who’ve sustained spinal cord injuries
to assist them to return to acute
on
participation in their homes, work,
leisure and community in a planned
tatiil
and timely manner.
Regular and routine reassessments
are performed under the spinal
Rehabi
reassessment service. This supports
clients to maintain their health and
Accident Compensation Corporation
Page 75 of 128
ACC Treatment Provider Handbook 2016
wellbeing and prevent secondary
complications.
Visual impairment
Provide clients who are visually
Multidisciplinary
services
impaired as a result of their injuries
providers
with the support they need to regain
the skills they need in everyday life.
Education support
Aims to meet the short- and long-
Education support
term injury-related learning support
worker
needs of children and young people
attending early childhood education
centres and primary and secondary
institutions, and the long-term injury-
related learning support needs of
students in tertiary education.
TBI residential
Support clients who’ve sustained
Multidisciplinary
rehabilitation services
moderate-to-severe TBI to return to
providers
active and meaningful participation in
their communities and, if appropriate,
support clients to return to work in a
planned, timely, supported and
sustainable manner.
Child and adolescent
Specialist inpatient, community
Multidisciplinary
rehabilitation services
rehabilitation and follow-up services
providers
for children and young people aged
0-16. They aim to enable these
children to achieve and maintain their
optimal level of functioning and
participate in developmentally
appropriate activities, prevent further
injury and provide advice on
appropriate rehabilitation planning.
Training for
Trains and coaches clients as they
Multidisciplinary
independence
adapt to the impacts of their injuries
providers
and helps maximise their
participation in home and community
activities.
Residential support
Provide slow-stream rehabilitation or Contracted or
services
‘home for life’ environments for
designated provider
clients who’ve suffered serious
on
injuries.
tatiil
Pain management services
Some of the most common pain management services available to ACC clients are
Rehabi
described in the table below. In almost all cases these are provided by contracted
providers. The provider criteria in the table indicate the contract types.
Accident Compensation Corporation
Page 76 of 128
ACC Treatment Provider Handbook 2016
Service
Purpose
Provider criteria
Pain
Uses psychological assessments and
Clinical
Management
interventions to help clients cope with and
psychologist/psychiatrist
Psychological
adapt to their injuries.
Service
Functional
An individualised exercise programme that
Registered
Reactivation
incorporates education in pain
physiotherapist and/or
Programme
management and the practical applications occupational therapist
of self-management principles.
Comprehensive
A comprehensive, fully integrated and
Multidisciplinary
Pain
independent clinical assessment. The
providers
Assessment
emphasis is on determining functional
goals for clients’ rehabilitation.
The comprehensive pain assessment
consists of three separate clinical
assessments (medical, functional and
psychological) followed by a team
discussion. The team produces a combined
‘formulation’ with recommendations.
Activity Focus
For clients who have persistent pain-related Multidisciplinary
Programme
disabilities with significant functional
providers
problems due to injury. The purpose of this
programme is to help clients adopt a self-
management approach to independent
functioning both at work and at home,
despite pain.
Multi-disciplinary A three-week residential programme that
Multidisciplinary
Persistent Pain
primarily focuses on helping to modify
providers
Programme
clients’ responses to pain, rather than
removing the pain stimulus.
Interventional
Provides specialised assessments and
Contracted specialised
Pain
treatment for ACC clients. Pain is a
medical practitioners
Management
complex phenomenon and best treated
using an integrated approach.
Interventional Pain Management
procedures should be undertaken within
the wider context of clients’ rehabilitation
on
(i.e. it’s not appropriate for a client to be
receiving the procedures in isolation, with
tatiil
no concurrent rehabilitation).
Rehabi
Accident Compensation Corporation
Page 77 of 128
link to page 29 link to page 93
ACC Treatment Provider Handbook 2016
8.
Invoicing and payments
Our legislation and policies
Payment criteria
ACC pays providers for the costs of treating patients with personal injuries that are
covered by the Scheme.
Legislation and policies specify that the treatment provided must be for the purpose of
restoring clients’ health to the maximum extent practicable. That means treatment needs
to be:
necessary and appropriate
of the quality required
given at the appropriate time and place, with only the necessary number of treatments
given prior approval if required
provided by an appropriately qualified treatment provider holding a current annual
practising certificate
clearly documented.
In deciding whether the points above apply to a client’s treatment, the legislation also says
that ACC must take into account the:
nature and severity of the injury
generally accepted treatment for the injury in New Zealand
other treatment options available in New Zealand for such an injury
New Zealand cost of both the generally accepted treatment and the other options,
compared with the likely benefit to the client of the treatment.
Your provider responsibilities are significant. In making payments for your services we may
need to query and verify aspects of your treatment or approach. This is to ensure that the
treatment meets the criteria, including ‘necessary’, ‘appropriate’ and ‘of the quality
required’, and that you’re supporting the treatment given with auditable clinical records.
For more information on monitoring, see
Monitoring providers and fraud control.
Invoicing
You can invoice ACC:
under the
Regulations
mentsy
through a contract arrangement (see your particular contract for details of the
invoicing process)
by agreement with ACC against a purchase order.
If you’re providing services under an ACC contract, you need to follow the invoicing or
ng and pa
payment arrangements in the contract, as these will supersede the Regulations.
icoi
For more information, visit ou
r website, phone the Provider Contact Centre on
0800 222
070 or email
[email address].
Inv
See a
lso Electronic invoicing: eSchedule.
Accident Compensation Corporation
Page 78 of 128
link to page 98 link to page 41
ACC Treatment Provider Handbook 2016
Invoicing under the Regulations – key points
ACC and Accredited Employers pay, or contribute to, costs at the rates and/or amounts
specified in the
Regulations. Contributions go towards basic consultation/visit costs and
additional costs for specific treatment and procedure types. For details of the contributions
see the
Schedule of the Regulations.
The Regulations allow invoicing for:
a consultation/visit relating to an injury or condition covered by ACC. The price of the
consultation/visit includes any procedures not specified in the
Regulations
a treatment or procedure carried out during the consultation/visit if it has an amount
specified in the Schedule. The amount we pay includes the cost of the most effective
treatment materials for the client’s injury. Procedures that don’t have specified prices
in the Schedule are included in the price for the consultation/visit and can’t be
invoiced separately.
You can only invoice us for payments if your client is eligible for the service you provide.
Our policy is to recover any money paid through incorrect invoicing.
For more details about inclusions and exclusions for invoicing treatments and procedures,
see
Consultation/Visit and procedure costs and codes.
Invoicing ACC and Accredited Employers
ACC
We pay you once we’ve accepted a claim and received your invoice for services, usually
on an ACC40 schedule (for medical practitioners) or ACC47 schedule (for other treatment
providers), or electronically through your PMS.
Accredited Employers
If your patient works for an Accredited Employer you’ll need to send your invoices directly
to the Accredited Employer. If you have any queries about invoice payments, prior
approval or injury management when treating an employee of an Accredited Employer,
please discuss these with the employer’s contact person or their nominated TPA. For more
information see
Lodging Accredited Employer claims.
Consultations/Visits
Definition of a consultation/visit
mentsy
For ACC to pay for a consultation/visit, it must be a necessary and appropriate face-to-
face assessment, treatment or service relating to a covered injury.
This includes providing injury-related advice, completing prescriptions, making referrals,
issuing any certificate to ACC and all relevant documentation that may result from the
ng and pa
consultation/visit. It doesn’t include insubstantial medical services for which clients
ic
wouldn’t normally pay, e.g. phone consultations and informal encounters.
oi
For billing purposes a consultation/visit includes:
Inv
removing sutures
Accident Compensation Corporation
Page 79 of 128
link to page 98
ACC Treatment Provider Handbook 2016
removing a non-embedded foreign body from an eye, mouth, auditory canal or other
site (excluding rectum or vagina) without incision
dressing minor single burns or abrasions
re-dressing wounds that don’t need significant dressings
checking a plaster cast
removing casts or splinting
removing packing of the nose, an abscess or haematoma
cleaning of, and minor dressings for (e.g. small gauze and non-stick dressings), small
burns or abrasions
cleaning of, and minor dressings for (e.g. plaster strips), small, open wounds
managing minor sprains that don’t need significant splinting.
For more details about inclusions and exclusions for invoicing consultations/visits, see
Consultation/Visit and procedure costs and codes.
When appointments are missed
You can invoice us for missed appointments or cancellations only if:
we made the appointment and agreed to pay a non-attendance fee
your contract with us covers payments for non-attendance by clients.
Paying for more than one consultation/visit per day
Generally, we only pay for one consultation/visit per day per client, for all provider types.
However, we consider each case individually and if clinically justified we may pay for a
second consultation/visit.
Criteria for more than one payment
Paying for two consultations/visits in one day may be clinically justified if:
you need to reassess the client for a second time later in the day e.g. if you need to
change a dressing or check a client whose condition may deteriorate or be likely to
deteriorate
the client initiates the second consultation/visit because of concerns about their
condition
the client is treated for one injury then leaves the consultation/visit and has a second,
separate accident that day.
We’re unable to pay for more than one consultation/visit in a day when:
ments
a client is referred for X-ray and returns for a consultation/visit afterwards to discuss
y
the outcome
more than one covered injury is managed at the same presentation.
If you have any queries, please call the Provider Contact Centre on
0800 222 070 or email
[email address].
ng and paic
To help us make quick decisions on invoices for additional same-day consultations/visits,
oi
you must explain why they were necessary. If you use manual invoices or a bulk-billing
Inv
schedule, note your reasons on the invoice. If you invoice electronically, phone the
Provider Contact Centre on
0800 222 070 or email
[email address].
Accident Compensation Corporation
Page 80 of 128
ACC Treatment Provider Handbook 2016
Medical practitioners’ treatment costs
Our contribution to medical practitioners’ costs
We contribute to two aspects of a medical practitioner’s treatment costs:
a consultation rate for a covered injury. The rate we pay depends on the client’s
age and is specified in the
Regulations. We pay a higher rate for clients under 13
years old than for other clients. The higher rate is to compensate medical practitioners
for providing free visits to under 13s.
specific treatments or procedures a client receives during a consultation/visit.
ACC only contributes to the cost of treatments or procedures listed under the heading
‘Medical practitioners’, nurses’ and nurse practitioners’ costs’. We pay the amounts
stated in the
Schedule of the Regulations.
How to invoice when different injuries need different treatments
If a client has more than one injury and needs procedures for more than one injury at the
same consultation/visit, the rates we pay are scaled.
We contribute:
the full amount stated in the Schedule for the most expensive treatment or procedure
the client receives
50% of the amount stated in the Schedule for any other treatment or procedure the
client receives.
Example 1: An adult client needs three treatments or procedures for more than one injury.
Example 1
Regulated amount
Invoice shows
Treatment/Procedure A
$34.83
@ 50% = $17.42
Treatment/Procedure B
$75.44 (highest-cost
@ 100% = $75.44
procedure overall)
Treatment/Procedure C
$40.35
@ 50% = $20.18
Consultation/Visit
$29.90
$29.90
Invoice total
$142.94
mentsy
Note: This example is based on indicative
rates and isn’t intended to reflect any amounts
specified in the
Regulations o
r Schedule.
How to invoice when the same injury needs different treatments
ng and paic
If a client receives a basic treatment or procedure and a more comprehensive treatment or
oi
procedure during the same consultation/visit, we pay only the rate for the more
comprehensive procedure.
Inv
Accident Compensation Corporation
Page 81 of 128
link to page 81
ACC Treatment Provider Handbook 2016
If you need help clarifying whether the rules for dual treatments apply, contact the Provider
Contact Centre on
0800 222 070 or email
[email address]. We also recommend
using the list of treatments and procedures from the
Schedule of the Regulations to find
the most appropriate category.
Nurses’ treatment costs
‘Nurse’ defined for invoicing
For ACC’s purposes a ‘nurse’ means a registered nurse (including a nurse practitioner) but
not an enrolled nurse or nurse assistant.
Our contribution to nurses’ costs
We contribute to two aspects of a nurse’s treatment costs:
a consultation rate for a covered injury. The rate we pay depends on whether
you’re a registered nurse or a nurse practitioner. We pay a higher rate for clients
under 13 years old than for other clients. The higher rate is to compensate medical
practitioners for providing free visits to under 13s.
specific treatments or procedures a client receives during a consultation/visit.
The treatment or procedure must be listed under the heading
‘Medical practitioners’,
nurses’ and nurse practitioners’ costs’. We pay the amounts stated in the
Schedule of
the Regulations.
These payments apply to nurses, or providers of nursing services, who don’t have
contracts with ACC. Nurses and nurse practitioners wanting to claim under the
Regulations need to be registered with us as individual treatment providers.
How to invoice when different injuries need different treatments
If a client has more than one injury and needs two or more treatments or procedures at the
same consultation/visit, the rates we pay are scaled – see
Example 1.
We contribute:
the full amount stated in the
Schedule for the most expensive treatment or procedure
the client receives
50% of the amount stated in the
Schedule for any other treatment or procedure the
client receives.
ments
How to invoice when the same injury needs different treatments
y
If a client receives a basic treatment or procedure and a more comprehensive treatment or
procedure during the same consultation/visit, we pay only the rate for the most expensive
procedure.
ng and pa
If you need help clarifying whether the rules for dual treatments apply, contact the Provider
ic
Contact Centre on
0800 222 070 or email
[email address]. We also recommend
oi
using the list of treatments and procedures from the
Schedule of the Regulations to find
the most appropriate category.
Inv
Accident Compensation Corporation
Page 82 of 128
ACC Treatment Provider Handbook 2016
Joint medical practitioner and nurse treatment costs
Our contribution to joint treatment costs
If both a nurse and a medical practitioner treat a client during the same consultation/visit,
and if both make relevant clinical notes, we contribute to both aspects of the treatment
costs:
a joint consultation rate for a covered injury. The rate we pay depends on the
client’s age and is specified in the
Regulations. We pay a higher rate for clients under
13 years old than for other clients. The higher rate is to compensate medical
practitioners and nurses for providing free visits to under 13s.
specific treatments or procedures a client receives during a consultation/visit.
The treatment or procedure must be listed under the heading
‘Medical practitioners’,
nurses’ and nurse practitioners’ costs’. We pay the amounts stated in the
Schedule of
the Regulations.
Only use the medical practitioner’s provider number when you invoice for a joint
consultation/visit.
When we contribute to the costs of a joint consultation/visit we don’t pay:
more than once for the same treatment
the individual consultation/visit costs specified for a registered nurse, nurse
practitioner or medical practitioner.
Invoicing for joint work on multiple treatments and procedures
If a client has more than one injury and needs two or more treatments or procedures from
a nurse and a medical practitioner working together at the same consultation/visit, the
rates we pay are scaled.
We pay:
the full amount stated in the Schedule for the most expensive treatment or procedure
the client receives
50% of the amount stated in the Schedule for any other treatment or procedure the
client receives.
Example 2: An adult client needs three treatments or procedures for more than one injury.
At a joint consultation/visit a nurse and a medical practitioner work together on each
ments
treatment or procedure.
y
Example 2
Regulated amount
Invoice shows
Treatment/Procedure A
$34.83
@ 50% = $17.42
ng and pai
Treatment/Procedure B
$75.44 (highest-cost
@ 100% = $75.44
c
procedure)
oi
Treatment/Procedure C
$40.35
@ 50% = $20.18
Inv
Accident Compensation Corporation
Page 83 of 128
ACC Treatment Provider Handbook 2016
Joint consultation/visit
$32.90
$32.90
Invoice total
$145.94
Note: This example is based on indicative rates and isn’t intended to reflect any
amounts in the
Regulations o
r Schedule.
Invoicing for joint work when the same injury needs different treatments
If at a joint consultation a client receives a basic treatment or procedure and a more
comprehensive treatment or procedure during the same consultation/visit, we pay only the
rate for the more comprehensive service.
If you need help clarifying whether the criteria for dual treatments apply, contact the
Provider Contact Centre on
0800 222 070 or email
[email address]. We also
recommend using the list of treatments and procedures from the
Schedule of the
Regulations to find the most appropriate category.
Working separately on multiple treatments or procedures
When a nurse and a medical practitioner work separately to provide more than one
treatment or procedure for a client for more than one injury during a joint consultation/visit,
we contribute according to the following table:
The nurse
The medical practitioner
The full amount specified in the Schedule for
The full amount stated in the Schedule
the most expensive treatment/procedure the
for the most expensive treatment/
client is given by the nurse.
procedure the client is given by the
practitioner.
50% of the amount stated in the Schedule for
every other treatment/procedure given by the
50% of the amount stated in the
nurse.
Schedule for every other treatment/
procedure given by the practitioner.
Example 3: An adult client needs several treatments or procedures for more than one
injury. At a joint consultation/visit a nurse and medical practitioner work separately on each
treatment or procedure.
Example 3
Regulated
Invoice shows
Provider number
amount
mentsy
Treatment/Procedure by
$34.83
@ 100% = $34.83
Nurse
nurse A
Treatment/Procedure by
$32.16
@ 50% = $16.08
Nurse
nurse A
ng and paicoi
Treatment/Procedure by
$113.09
@ 100% = $113.09
Medical
medical practitioner B
practitioner
Inv
Accident Compensation Corporation
Page 84 of 128
ACC Treatment Provider Handbook 2016
Treatment/Procedure by
$68.59
@ 50% = $34.30
Medical
medical practitioner B
practitioner
Joint consultation/visit
$32.90
$32.90
Medical
practitioner
Invoice total
$231.20
Note: This example is based on indicative rates and isn’t intended to reflect any amounts
specified in the late
st Regulations o
r Schedule.
Specified treatment providers
Defining specified treatment providers
Specified treatment providers are acupuncturists, chiropractors, occupational therapists,
osteopaths, physiotherapists, podiatrists and speech therapists, as listed in
section 3 of
the Regulations.
Rule for invoicing
Specified treatment providers can provide services to our clients either under contract or
under the
Regulations.
Invoicing under contract
Providers invoicing for services given under contract should follow the invoicing
requirements specified in the contract.
Invoicing under the Regulations
All specified treatment providers invoicing under the Regulations must choose whether
they want to be paid per hour or per treatment.
When you start invoicing, we take your approach as your chosen option. To change your
invoicing option, please write with your reasons to ACC Provider Registration, PO Box
30823, Lower Hutt 5040 or email
[email address]
When you request a change to your invoicing option you won’t be eligible to receive any
back-payments for services. Your new invoicing option will be effective from the date of
receipt of the change request.
ments
The Regulations specify the rates for invoices per hour and per consultation/visit. For more
y
information visit ou
r website, contact the Provider Contact Centre on
0800 222 070 or
email
[email address].
Invoicing per hour
ng and pai
If you provide ‘direct treatment’ for less than one hour, we calculate the payment in
c
increments of five minutes, e.g. if your treatment takes 44 minutes we pay for 45 minutes
oi
of the hourly rate (i.e. three-quarters of the hourly rate).
Inv
Accident Compensation Corporation
Page 85 of 128
ACC Treatment Provider Handbook 2016
Direct treatment
You provide ‘direct treatment’ when you directly apply your expertise to a client’s
treatment. Direct treatment includes:
assessing and/or reviewing the client’s injury
developing a treatment plan with the client (including taking a patient history and
writing clinical notes during the consultation/visit)
physically applying treatment(s)
observing the client while treatment(s) is in place.
If you’re only seeing one client at a time you can invoice ACC for the time you’re not
providing direct treatment, as long as you’re immediately available for the client should
they require assistance.
When attending to multiple clients you can’t invoice concurrently. Instead, calculate the
total time spent on direct treatment with each. You can’t invoice for more than one hour’s
treatment in any hour.
If you treat a client for less than 60 minutes or multiple clients within 60 minutes, the rates
in the part-hour payments table below apply.
You can’t invoice ACC for more than 60 minutes in any given hour. The rules below for
invoicing for multiple clients per hour apply.
Specified treatment provider part-hour payments
Hourly rate
Hourly rate
Minutes
(GST exclusive
(GST inclusive)
5
$4.73
$5.44
10
$9.46
$10.88
15
$14.19
$16.32
20
$18.92
$21.76
25
$23.65
$27.20
30
$28.38
$32.64
mentsy
35
$33.11
$38.07
40
$37.84
$43.51
45
$42.57
$48.95
ng and pai
50
$47.30
$54.39
c
oi
55
$52.03
$59.83
Inv
Accident Compensation Corporation
Page 86 of 128
link to page 29 link to page 25 link to page 26 link to page 44 link to page 44
ACC Treatment Provider Handbook 2016
Specified treatment provider part-hour payments
60
$56.76
$65.27
These prices came into effect in the
Regulations on 1 April 2014. In all cases your clinical
records must support and document your direct treatment. If it’s clinically justified you can
claim for a block of direct treatments of more than an hour’s duration, as long as you
document it in your clinical records.
We’ll follow up any invoicing patterns outside the expected norms for specific discipline.
For more information on provider monitoring and other quality assurance functions, see
Monitoring providers and fraud control and
Supporting quality.
Invoicing at the hourly rate for more than one client
If you treat more than one client in an hour, we pay only up to 60 minutes in total.
Example 3a: You treat six clients in a group for an hour.
You
can invoice us for six individual clients for 10 minutes each (i.e. invoice us for a total
of one hour of your time).
You
can’t invoice us for an hour for each client (i.e. invoice us for a total of six hours for
one hour of your time).
Your records must always demonstrate that your clinical input is necessary and
appropriate; s
ee Clinical records.
You can invoice us in five-minute increments for accuracy – that is for 5, 10, 15, 20, 25,
30, 35, 40, 45, 50, 55 or 60 minutes of treatment.
Example 3b: You treat a client from 10:00am to 10:30am (30 minutes), and another from
10:15am to 11:00am (45 minutes).
We’ll pay for the hour between 10:00am and 11:00am, but not for 75 minutes of treatment
time. However, if your second client’s 45-minute slot begins at 10:20am (so finishes at
11:05am) we’ll pay for one hour and five minutes.
You can’t invoice us for the overlap of the clients’ treatment during the hour, but you can
invoice us for the five minutes beyond the hour.
mentsy
Limitations to invoicing per treatment
If treatment profiles and their trigger numbers apply to your treatment, you can’t combine
the number of treatments for different injuries (i.e. the sum of different Read Codes) to give
an aggregated number of treatments. You can only provide treatments up to the highest
individual trigger number before you need to provide an
ACC32 Request for Prior Approval
ng and pai
of Treatment form.
c
oi
Example 4: A client has a mountain-bike accident and sustains multiple injuries.
Inv
Accident Compensation Corporation
Page 87 of 128
link to page 44 link to page 44 link to page 44 link to page 54
ACC Treatment Provider Handbook 2016
Example 4
Injury
Trigger number of treatment profiles
S50
Sprain shoulder
12
SE31
Contusion elbow
12
S5400
Sprain knee joint
14
The injury that allows the most treatments before you need to get ACC approval for
additional treatment is the S5400 sprain knee joint. You can invoice us for up to 14
treatments in this example, but not the sum of the treatment trigger numbers for all the
injuries, which would be 38 treatments.
Similarly, if you’re dual ACC registered you can’t combine the number of treatments under
both provider types to give an aggregated number of treatments. You can only provide
treatments up to the highest individual trigger number before you need to provide an
ACC32 Request for Prior Approval of Treatment form.
Example 4a: A chiropractor can provide up to 18 treatments before prior approval is
required, and an acupuncturist can provide up to 16 treatments. A dual-registered
chiropractor/ acupuncturist can invoice us for up to 18 treatments (the larger number of the
two) before prior approval is required. The treatment numbers can’t be combined to 34
treatments before prior approval is sought.
If none of the injuries has a treatment profile with a treatment trigger, you can provide six
treatments before requesting approval for additional treatments.
If you anticipate that you’ll need ACC prior approval for additional treatment funding or are
requesting funding for additional splinting costs, you need to complete an ACC32 Request
for Prior Approval of Treatment form. For more information, see
Requesting further
treatment: referring clients via the ACC32 Request for Prior Approval of Treatment form.
Payment for counsellors
How to invoice
The
Regulations specify counsellors’ invoicing and payment arrangements. They require
you to provide treatment face to face.
s
Exception
You can invoice for one session of counselling provided in another way (e.g. by phone) if
menty
the client urgently needs it for mental injury caused by certain criminal acts outlined in
section 21 of the AC Act. See also
Mental injuries, sensitive claims and counselling.
ACC will pay either the:
ng and pa
hourly rate fixed in the
Regulations for treatment provided by a counsellor who’s a
ic
medical practitioner, or
oi
hourly rate fixed in the
Regulations for treatment provided by a counsellor.
Inv
Actual rates may be adjusted from time to time. For the latest rates, contact the Provider
Contact Centre on
0800 222 070 or email
[email address].
Accident Compensation Corporation
Page 88 of 128
ACC Treatment Provider Handbook 2016
Different invoicing and payment arrangements may apply to counsellors who deliver
treatments or services under contracts with ACC.
Invoicing for services under contract
If you’re providing services under an ACC contract, you need to follow the invoicing and
payment arrangements in the contract, not the
Regulations.
Services and reports
Invoicing for imaging services
You’ll find a list of imaging services and fixed rates for treatments and procedures in the
Schedule of the Regulations. The Schedule covers a wide range of radiological
procedures used in everyday practice, including mammography, ultrasound and special
procedures such as myelogram and arthrogram.
High-tech imaging
The Schedule doesn’t cover high-technology items such as MRI scans. You can only
access them and have us pay for them if you’re working under contract for these services.
Invoicing for supplying reports and records
If we ask you to provide a report you can invoice us for a report fee at the rate quoted in
our request letter. You need to cite the purchase order number and the appropriate report
code, e.g. ‘STPR’ for specified treatment providers and ‘MEDR’ for medical practitioners.
The standards we expect in your reports are the same as those of your professional
organisation, i.e. they must be honest, impartial, unbiased, clear and relevant. They will
serve your patients’ interests best if they focus on verifiable clinical evidence wherever
possible.
We sometimes ask for copies of existing clinical notes and typically pay the expenses for
providing this information at identified rates. You can get the latest rates from your local
Supplier Manager or by phoning the Provider Contact Centre on
0800 222 070 or emailing
[email address].
Section 309(4) of the AC Act requires you to provide us with any information we request if
the client has authorised us to make the request and you have notice of that authorisation.
Clients give us this authority when they sign their ACC45 Injury Claim forms.
We use the information to make decisions about entitlements and to detect fraud. It’s an
mentsy
offence to not supply the information to us without a reasonable excuse.
If a patient asks for their own medical records, you must supply them free of charge unless
the patient has requested the same information within the previous 12 months, or the
information includes video recordings, X-rays and CAT scans.
ng and paicoi
Inv
Accident Compensation Corporation
Page 89 of 128
link to page 90 link to page 93
ACC Treatment Provider Handbook 2016
Invoicing correctly
Procedures for invoicing ACC
How you invoice ACC will depend on the conditions of your contract, the purchase order or
the Regulations.
If you’re contracted to ACC, follow the invoicing process in the contract.
If you’re seeking payment for services that we’ve asked you to provide, make sure you
have a seven-digit purchase order number from us and include it in your invoice to the
requesting unit. It will be processed by our Accounts Payable team.
If you’re invoicing under the Regulations, see ou
r website.
A claim needs to be lodged prior to submitting an invoice. When invoicing, please be
aware that:
only one consultation/visit per day/per client can be invoiced to ACC
where there are exceptional circumstances and a client returns for a second
consultation/visit on the same day, full details of this (including the relevant clinical
records) should be provided to ACC for consideration
where multiple claims are being managed at the same consultation/visit, you can only
invoice ACC for one consultation/visit against one claim – normally the most
significant injury being treated
if, as an individual provider, you choose to utilise elements of more than one
treatment modality, e.g. chiropractic and acupuncture, at the same consultation/visit
(or on the same day), you can only invoice ACC once under one provider number
all invoices need to be complete and accurate
at times ACC will request copies of clinical records. Failure to provide these could
result in non-payment.
Ensure that the following information is correct for every line:
ACC claim number or ACC45 number, or both
READ code
full client name (no abbreviations or incorrect spelling)
date of injury
date of service
date of birth.
Completing and sending a bulk-billing schedule
mentsy
ACC recommends that all provide
rs invoice electronically as it is a faster process, but we
still enable a manual process (see
Electronic invoicing: eSchedule).
The bulk-billing process applies to all invoices from treatment providers. It enables you to
send several invoices at once on either an ACC40 schedule (for medical practitioners) or
ng and pai
an ACC47 schedule (for other treatment providers).
c
oi
Every schedule must show your GST number.
Inv
Directions for bulk-billing are on ou
r website.
Accident Compensation Corporation
Page 90 of 128
link to page 6 link to page 6
ACC Treatment Provider Handbook 2016
Where to send your schedule
Please send your schedule to the Medical Fees unit for your area, see
Key ACC contacts
for treatment providers.
If you have any queries about the process, or about a specific payment, phone the
Provider Contact Centre on
0800 222 070 or
email
[email address].
mentsy
ng and paicoi
Inv
Accident Compensation Corporation
Page 91 of 128
ACC Treatment Provider Handbook 2016
9.
Working electronically with ACC
Digital certificates
How to get a digital certificate
In order to acce
ss ACC online services, including eLodgement, eSchedule and Online
Claims Queries, you need to apply for a digital certificate.
For more information:
download the application forms for your digital certificate on our website – see
Apply
for a digital certificate
visit HealthLink
’s website. HealthLink creates, distributes and supports digital
certificates
email the New Zealand Health and Disability Sector Registration Authority (NZHSRA),
which approves and administers digital certificates, a
t [email address] or call
0800 117 590.
Receiving and connecting your digital certificate
Complete and return the HealthSecure application forms, and NZHSRA will liaise with
HealthLink to create and courier your digital certificate on a CD-ROM. If you don’t have a
CD-ROM drive, please contact our eBusiness Support team, who will be able to help you.
Digital certificates are valid for one year. NZHRSA will send you an email each year to
confirm that you still require a digital certificate. When you reply to the email your new
certificate will be issued automatically.
If you’re eligible, ACC will cover the cost of your annual digital certificate.
When you receive your certificate you’ll need to have a password for installation. This will
usually be sent to you via text message from HealthLink. Alternatively, you can call
HealthLink on
0800 288 887 and request your certificate password. HealthLink can also
talk you through the installation if you need help.
The ACC eBusiness Support team will contact you to schedule a phone training session,
th ACC
which will take approximately 30 minutes. They’ll also monitor your progress to ensure
everything is running smoothly.
wiyl
Already have a current digital certificate?
al
If you’re already an ACC-registered vendor (and/or provider), complete Section 2 and
Section 7 of the
ACC1534 Change of vendor details form to request access to the ACC
tronic
eBusiness Gateway.
ec
Online claim lodgement: eLodgement
ng el
About eLodgement
orki
W
Any provider who submits ACC45 Injury Claim forms can use eLodgement. You can learn
about the benefits of using eLodgement on ou
r website.
Accident Compensation Corporation
Page 92 of 128
ACC Treatment Provider Handbook 2016
What you need to use eLodgement
To start using eLodgement you need:
a computer or compatible mobile device. You can find information on the minimum
computer specifications and browser settings on our website
a digital certificate – a software application that creates your unique digital signature.
Issued on CD-ROM and stored on your computer, your digital certificate authenticates
the origin of data and secures data as it travels between you and ACC. Your digital
certificate is free, renewed annually and issued by ACC. For more information see
Digital certificates
a compatible PMS. Your PMS will generate ACC45s completed with the data you
normally use and prompt you for any additional data needed. To find out about PMSs:
o see our online list o
f PMSs that support eLodgement o phone our Provider eBusiness Support team on
0800 222 994 option 1
o email
[email address].
If you don’t have a PMS you can still take advantage of the system by using our
eLodgement website. Please get in touch with the eBusiness Support team, who will
arrange access to the eLodgement website on your behalf.
You might also like to read ou
r Security Policy for Electronic Business.
Electronic invoicing: eSchedule
Who can use eSchedule?
You can use eSchedule if you submit invoices to us for payment under business rules
specified in a contract, purchase order or the
Regulations.
You can use the service to send us your ACC40 schedule (for medical practitioners) or
ACC47 schedule (for other treatment providers) electronically, either from your PMS or
through our eBusiness Gateway.
The benefits of eSchedule
eSchedule offers you the benefits of:
th ACC
faster payments, normally within seven working days, as electronic invoices have
priority
wiy
24-hour online tracking to check the progress of your schedules, payments and the
l
registration of ACC45 Injury Claim forms
al
online remittance advices
time and paper savings through streamlined processes
tronic
quality information between systems
ec
1
easy checking that a claim is for an Accredited Employer
schedule payments being processed within five days if the information is complete
and accurate
ng el
partial payments for incomplete schedules, rather than having them held for payment
in their entirety
orki
2
the ability to diagnose any invoicing and payment problems quickly and easily
W
not having to submit printed schedules or copies of referral forms and approval letters.
Accident Compensation Corporation
Page 93 of 128
3
ACC Treatment Provider Handbook 2016
Make sure you keep copies of referrals and approval letters, as we may need to see them
to validate your invoices.
What you need to use eSchedule
If you’re an existing vendor with ACC and have been sending your invoices to us by post,
you’ll need to complete a
n ACC1534 Change of vendor details form. You can indicate on
this form that you’re going to bill electronically. Providers not registered with us will need to
complete the
ACC24 Application for ACC Health Provider Registration form, which
includes a section on electronic claiming. The team will advise you in writing when your
request has been approved, usually within a week of your application being submitted.
How to send eSchedules
To send an eSchedule:
1. Check that your billing schedule is correct:
o send separate schedules for individual contracts. For example, physiotherapy
services can’t appear on the same schedule as GP services
o ensure that you use the correct service codes to avoid payment delays. If
you’re not sure what service code you should be using, contact the Provider
Contact Centre on
0800 222 070 or email
[email address]
o check that your claim numbers are correct and in the required format. Use
ACC45 numbers where possible, but be careful not to use zero in place of the
letter ‘O’ or vice versa. Enter alpha and numeric data only (i.e. not symbols
such as / and –)
o if you’re providing services on an hourly rate, list the service duration(s).
2. Before you send your first eSchedule, check that your ACC vendor ID is active and
you have a valid digital certificate installed. If you use a PMS, check with your PMS
vendor that your system is configured correctly to start sending eSchedules to ACC.
3. Don’t send test schedules. The eBusiness Support team will be happy to help you
remotely if you’d like some support and guidance with your first submissions.
4. The day after you send your first batch of schedules, phone the Provider Contact
Centre on
0800 222 070 to check that they have arrived. If you use a PMS you may
have received an acknowledgement, but there are occasions when acknowledged
schedules are rejected. The eBusiness Support team will let you know if you need to
fix your system or resubmit the schedules.
th ACC
If at any other time you want to check your payment schedules, you can use our
wi
eBusiness Gateway to run queries against the status of your invoice, or phone the
yl
Provider Contact Centre quoting your ACC vendor ID and each schedule number
al
you’re querying.
5. ACC pays the amount owing into the bank account you provided and sends you a
payment advice letter confirming the amount.
tronic
ec
Late invoicing
If you send us an invoice 12 months or more after providing a service, you’ll need to give
ng el
us extra information to show that we’re still liable to pay for the service. For further advice
contact the Provider Contact Centre on
0800 222 070, or conta
ct your local Supplier
orki
Manager.
W
Accident Compensation Corporation
Page 94 of 128
ACC Treatment Provider Handbook 2016
Querying payment delays
Where we have enough information we usually decide on cover for a claim within 24
hours. However, some claims (e.g. gradual process claims) can take longer because we
need additional information. In these cases delays in payment are unfortunately inevitable.
Payments can also be delayed if we’ve asked a client to visit another treatment provider
for a second opinion.
The bulk-billing payment advice and the Invoice Status Query on our eBusiness Gateway
web page will show you which payments have been withheld and why. Call the Provider
Contact Centre on
0800 222 070 or email
[email address] to discuss late
payments, or if you think a claim has been accepted for payment but you haven’t been
paid.
Online eBusiness Gateway queries
Invoice queries, payment advice and claim status
Online queries can be used by:
valid digital certificate holders with active ACC vendor IDs
providers with active ACC provider numbers who’ve been granted access to the
eBusiness Gateway.
With online queries you can:
query the status of an ACC45 claim number to check:
o whether the claim has been accepted or declined by ACC
o the client’s injury diagnosis
o the date of the client’s accident
o whether the claim is being managed by an Accredited Employer
o whether the injury has been resolved
query the current payment status of any invoice/schedule you’ve sent us, including:
o whether a schedule has been paid
o how much was paid
o the reason for a payment being put on hold or declined
download an online copy of your payment advices.
th ACC
Online claim queries
wiy
All you need to access query functions is a computer that meets the
specifications with an
l
internet connection and a Health Secure digital certificate.
al
If you’re already using a digital certificate for other health sector transactions such as
tronic
eLodgement or Special Authority, it’s likely to be a Health Secure digital certificate which
you can also use for running queries.
ec
To check if you have the right digital certificate phone our Provider eBusiness Support
ng el
team on
0800 222 994 option 1, or email
[email address].
orki
If you need to apply for a HealthSecure digital certificate, complete and return both the
W
HealthSecure Organisation Registration and
HealthSecure User Registration forms.
Accident Compensation Corporation
Page 95 of 128
ACC Treatment Provider Handbook 2016
Working online FAQs
Q: Why are claim numbers important?
A:
The ACC system checks that claims belong to the people whose services are being
claimed for.
If the ACC database and your database have different details for a client (such as
name and date of birth), the discrepancy will be flagged so all involved can make
sure they’re sharing the correct details.
Q: If we eLodge, do we still need to send printed copies to ACC?
A:
No, we only need the electronic copies. However, you must keep copies in paper or
image format of signed documents that show your patients have authorised you to
lodge claims on their behalf.
Q: Does the treatment provider who generates an ACC45 Injury Claim form during a
consultation/visit have to send it to ACC straight away?
A:
No. However, all ACC45 Injury Claim forms should be lodged on the day of the
consultations/visits to ensure that the patients can receive their ACC entitlements
as quickly as possible. If you have a network of practice computers, a practice
administrator can pick up the ACC45 forms on their computer, check that the
information is complete and submit them to ACC. This should be done at least once
a day.
Q: Do all treatment providers need computers?
A:
No, you can complete ACC45 forms by hand and give them to your administrative
staff for input that day to minimise the time required on a computer.
Q: We already send online invoices to ACC – how will lodging the ACC45 Injury Claim
form online affect our billing?
A:
The eLodgement system allows you to lodge your ACC45 forms online without
affecting your electronic invoicing. The process of invoicing ACC won’t change.
However, you’ll find that you can invoice us a lot faster when eLodging your ACC45
th ACC
forms as we’ll have details of your patients’ claims in our system at the time you
submit your invoices.
wiyl
Q: Will the information I send online be secure?
al
A:
Yes. The digital certificate protects the information you transmit by letting ACC
know that it was you or your organisation that sent the data. Your computer system
tronic
also encrypts (or ‘scrambles’) the data with your digital certificate to protect it as it
ec
travels from you to ACC.
Q: Does every treatment provider need a digital certificate?
ng el
A:
No. It will depend on whether you’re submitting invoices, medical certificates or
orki
medical reports or eLodging online.
W
Q: Is there any cost to me to start using ACC online services?
Accident Compensation Corporation
Page 96 of 128
ACC Treatment Provider Handbook 2016
A:
No. If you currently have a digital certificate for Ministry of Health access, we can
explore using this for your ACC access. Otherwise, ACC will cover the cost of your
new digital certificate and its annual renewal. You only incur the cost if you lose or
damage your certificate and require a replacement before its annual renewal. Our
eBusiness Support team is available Monday to Friday for free remote support if
you have any technical issues.
Q: Can I use my mobile device to lodge my ACC45 forms and eSchedules?
A:
Yes, if you have a compatible device. You’ll need to install your digital certificate on
your device – our eBusiness Support team will be happy to help you do this.
Q: My computer doesn’t have a CD drive; how do I install my digital certificate?
A:
If you can gain temporary access to a computer with a CD drive, you can transfer
your digital certificate to a USB drive or email the files to yourself. If you need any
assistance, contact the eBusiness Support team on
0800 222 994 option 1, or email
[email address].
th ACC
wiylalci
tron
ec
ng el
orki
W
Accident Compensation Corporation
Page 97 of 128
link to page 125
ACC Treatment Provider Handbook 2016
10. Consultation/Visit and procedure
costs and codes
Guide to invoicing for medical practitioners and nurses
This is a guide to invoicing under the
Regulations.
The guide should be read in conjunction with the
ACC1520 Medical practitioners', nurses’
and nurse practitioners’ costs 2014.
Section 8 of this handbook also carries detailed information about invoicing under the
Regulations.
What a consultation/visit covers
You can invoice ACC for a consultation/visit. A consultation/visit includes:
a face-to-face examination and/or assessment
a necessary and appropriate service or treatment, performed by a provider, for an
injury or condition covered by ACC
any claim-related advice, prescription or referral, and the issue of certificates as
appropriate following the consultation/visit
managing conditions, including providing a small range of minor
treatments/procedures, such as:
o removing sutures
o removing a non-embedded foreign body from eye, mouth, auditory canal or
odes
other site (excluding rectum or vagina) without incision
o re-dressing wounds that don’t require
significant dressings
o performing a plaster check
and c
o removing casts/splinting
ts
o removing packing of nose, or packed abscesses or haematomas
osc
o cleaning and minor dressings (e.g. small gauze or non-stick dressings) to
small burns or abrasions
re
o cleaning and minor dressings (e.g. plaster strips) to small, open wounds
o managing minor sprains that don’t involve significant splinting
edu
o completing clinical records.
What a consultation/visit doesn’t cover
A consultation/visit doesn’t include:
t and procisi
telephone consultations (except for a one-off phone-counselling session if required)
medical services where no substantial service is given by the provider and for which
the patient wouldn’t reasonably be expected to pay.
on/V
tati
All invoices for procedures, regardless of the number claimed, must be clinically justifiable.
ul
Understanding procedure codes
Cons
The procedure codes start with two letters:
Accident Compensation Corporation
Page 98 of 128
link to page 99 link to page 99 link to page 101 link to page 103 link to page 108 link to page 110 link to page 112 link to page 112
ACC Treatment Provider Handbook 2016
the first letter is M, which stands for ‘Management of’
the second letter is phonetic and covers the procedure code topic (e.g. B for burns
and D for dislocations).
The two letters are followed by a number that defines a sub-category within the code.
Summary of procedure codes
This table summarises the procedure codes, the injuries to which they refer and the
recommended maximum treatments per injury.
Procedure
Injury type
Recommended maximum treatments claimed
code
per injury
MB#
Burns and
4
abrasions
MD#
Dislocations
1
MF#
Fractures
1
(except MF7, MF9-MF12 = 3)
MM#
Miscellaneous
1
MW#
Open wounds
1
MT#
Soft tissue
1
odes
injuries
(except MT3 = 2 and MT5 = 3)
and c
ts
Burns and abrasions
osc
General invoicing criteria
re
Practitioners can invoice for treating burns and abrasions under the following eligibility
edu
criteria.
Eligible – all MB codes
Services that are eligible for invoicing include:
t and procisi
assessment
providing initial care and patient/caregiver education
treating significant skin damage
on/V
cleaning and debriding wound(s)
tati
managing significant wound dressings
ul
providing a significant amount of practitioner time
providing post-injury advice and patient education.
Cons
Accident Compensation Corporation
Page 99 of 128
link to page 99 link to page 100 link to page 99 link to page 100 link to page 99 link to page 100 link to page 99 link to page 100 link to page 99 link to page 100
ACC Treatment Provider Handbook 2016
Not eligible – all MB codes
Services that are not eligible for invoicing include:
treating trivial and superficial burns or abrasions at a first or subsequent
consultation/visit, and applying only a simple gauze or similar dressing. This is
covered as part of a consultation/visit
follow-up consultations/visits involving: dressing removal, or re-dressing where
significant dressings are not used; wound inspection; and recommendations about
infection control. These are covered as part of consultations/visits.
Invoicing criteria for each MB code
MB1 – Treatment of burns less than four square centimetres (m2) (e.g. 2cm x 2cm)
Included
See
Eligible – all MB codes.
Excluded
See
Not eligible – all MB codes.
Procedures per injury
Recommend: maximum of four procedure claims per injury.
MB2 – Treatment of burns greater than 4cm2 at a single site
Included
See
Eligible – all MB codes.
Note: Claims in this category are usually few.
Excluded
See
Not eligible – all MB codes.
odes
Procedures per injury
Recommend: maximum of four procedure claims per injury.
MB3 – Treatment of significant abrasions less than 4cm2 at a single site
and c
ts
Included
See
Eligible – all MB codes.
osc
Excluded
See
Not eligible – all MB codes.
re
Procedures per injury
Recommend: maximum of four procedure claims per injury.
edu
MB4 – Treatment of significant abrasions greater than 4cm2 at a single site
Included
See
Eligible – all MB codes.
t and proci
Excluded
See
Not eligible – all MB codes.
si
Procedures per injury
Recommend: maximum of four procedure claims per injury.
on/V
MB5 – Significant burns or abrasions (not including fractures) at multiple sites
tati
(greater than 4cm2), necessary wound cleaning, preparation and dressing
ul
Included
See
Eligible – all MB codes.
Cons
Excluded
See
Not eligible – all MB codes.
Accident Compensation Corporation
Page 100 of 128
ACC Treatment Provider Handbook 2016
Note: If there are multiple wounds but only one needs significant
time or dressing, only one claim would be made for the
significant wound under MB2 or MB4.
Procedures per injury
Recommend: maximum of four procedure claims per injury.
This section should be read in conjunction with the
ACC2136 MB and MW Codes.
For more information about ACC2136 see the link above and see
General practitioner
resources o
r Burns and scar management.
Dislocations
General invoicing criteria
Where there is evidence of significant joint dysfunction (e.g. major effusion or
haemarthrosis and/or ligament laxity), practitioners can invoice for treating confirmed
dislocations of any of the five joints listed in the table below, under the following eligibility
criteria.
Eligible – all MD codes
Services that are eligible for invoicing include:
assessment
providing initial care and patient/caregiver education
referral for, review of and action on an X-ray (if necessary)
odes
use of appropriate anaesthetic technique (including local, intravenous (IV) or regional
anaesthesia, or mild central sedation)
treating significant subluxation
and c
providing post-injury advice and patient education
ts
management using best-practice splinting techniques, which may include providing a
os
plaster cast. See a
lso ACC579 Treatment profiles 2001 and ACC2373 Practical
c
Techniques in Injury Management. ACC2373 isn’t available online but can be
re
obtained through your loca
l Supplier Manager.
edu
Not eligible – all MD codes
Services that are not eligible for invoicing include:
minor joint trauma, including minor sprains not involving confirmed dislocations or
significant subluxation, and where there is no evidence of serious subsequent joint
t and procis
dysfunction. These are covered as part of consultations/visits or by a soft tissue injury
i
procedure, whichever fits best
possible dislocations to joints not covered under the following five codes (MD1-5). In
on/V
that case a ‘nearest equivalent’ treatment or procedure will be considered. However,
tati
a soft tissue injury procedure may be appropriate
ul
treatment before referral to a specialist centre, including temporary splinting. This is
covered under a soft tissue injury procedure
follow-up assessments, including removal of splinting. These are covered as part of
Cons
consultations/visits
treatment of injury that doesn’t require the use of best-practice splinting with
Accident Compensation Corporation
Page 101 of 128
link to page 101 link to page 101 link to page 101 link to page 101 link to page 101 link to page 101 link to page 101 link to page 101 link to page 101 link to page 101
ACC Treatment Provider Handbook 2016
significant dressing cost. This is covered as part of a consultation/visit.
Invoicing criteria for each MD code
MD1 – Dislocation of finger or toe, with splint or strapping
Included
See
Eligible – all MD codes.
Excluded
See
Not eligible – all MD codes.
Procedures per
Recommend: one procedure claim per injury.
injury
MD2 – Dislocation of thumb, closed reduction and immobilisation
Included
See
Eligible – all MD codes.
Excluded
See
Not eligible – all MD codes.
Procedures per
Recommend: one procedure claim per injury.
injury
MD3 – Dislocation of elbow with radiological confirmation, closed reduction and
immobilisation
Included
See
Eligible – all MD codes.
Excluded
See
Not eligible – all MD codes.
odes
Procedures per
Recommend: one procedure claim per injury.
injury
and c
MD4 – Dislocation of shoulder, closed reduction and collar and cuff immobilisation
ts
os
Included
See
Eligible – all MD codes.
c
re
Excluded
See
Not eligible – all MD codes.
edu
Procedures per
Recommend: one procedure claim per injury.
injury
MD5 – Dislocation of patella, closed reduction and cast immobilisation
t and proc
Included
See
Eligible – all MD codes.
isi
Excluded
See
Not eligible – all MD codes.
on/V
Procedures per
Recommend: one procedure claim per injury.
tati
injury
ul
Cons
Accident Compensation Corporation
Page 102 of 128
link to page 103
ACC Treatment Provider Handbook 2016
Fractures
General invoicing criteria
Practitioners can invoice for treating diagnosed fractures under the following eligibility
criteria. If there is no diagnosis of a fracture, a soft tissue injury code (MT) may be
appropriate.
Each service code includes tasks that can and can’t be invoiced for, on top of the general
invoicing eligibility criteria below that cover all codes.
Eligible – all MF codes
Services that are eligible for invoicing include:
assessment
providing initial care and patient/caregiver education
X-ray confirmation (or clinical certainty) of a fracture
applying best-practice soft tissue splinting, or plaster cast immobilisation, for more
than three weeks
providing post-injury advice and patient education
management that may include (where clinically appropriate):
o the use of appropriate anaesthesia
o fracture reduction.
Not eligible – all MF codes
Services that are not eligible for invoicing include:
odes
undisplaced simple fractures that don’t need plaster cast immobilisation. These are
covered as part of a simple soft tissue injury procedure
and c
plaster checks and removal. These are covered as part of consultations/visits
ts
treatment before referral to a specialist centre, including providing temporary splinting.
os
This is covered as part of a soft tissue injury procedure.
c
re
For fractures that aren’t covered under these specific procedure codes, and where best
practice would suggest a plaster cast, a ‘nearest equivalent’ procedure will be considered.
edu
In other cases, a soft tissue injury procedure may be appropriate. See also
ACC579
Treatment profiles 2001 and ACC2373 Practical Techniques in Injury Management
(available through your loca
l Supplier Manager).
Invoicing criteria for each MF code
t and procisi
MF1 – Fractured finger or toe (proximal, middle or distal phalanx), closed reduction
and immobilisation
on/V
Included
See
Eligible – all MF codes.
tati
ul
Excluded
Follow-up treatments are usually covered as part of
consultations/visits as they don’t require the same degree of
assessment or significant new splinting.
Cons
Accident Compensation Corporation
Page 103 of 128
link to page 103 link to page 103 link to page 103 link to page 103 link to page 103 link to page 103 link to page 103 link to page 103
ACC Treatment Provider Handbook 2016
See a
lso Not eligible – all MF codes.
Procedures per
Recommend: one procedure claim per injury.
injury
MF2 – Fractured finger or toe (proximal, middle or distal phalanx), requiring digital
anaesthetic
Included
See
Eligible – all MF codes.
Excluded
Follow-up treatments are usually covered as part of
consultations/visits as they don’t require the same degree of
assessment or significant new splinting.
See a
lso Not eligible – all MF codes.
Procedures per
Recommend: one procedure claim per injury.
injury
MF3 – Fractured metatarsal: closed reduction (not requiring cast), closed reduction,
immobilisation by strapping
Included
See
Eligible – all MF codes.
Excluded
Follow-up treatments are usually covered as part of
consultations/visits as they don’t require the same degree of
assessment or significant new splinting.
odes
See a
lso Not eligible – all MF codes.
Procedures per
Recommend: one procedure claim per injury.
and c
injury
ts
MF4 – Fractured metacarpal(s) hand: with or without local anaesthetic,
osc
immobilisation by strapping
re
Included
See
Eligible – all MF codes.
edu
Excluded
Follow-up treatments are usually covered as part of
consultations/visits as they don’t require the same degree of
assessment or significant new splinting.
See a
lso Not eligible – all MF codes.
t and procisi
Procedures per
Recommend: one procedure claim per injury.
injury
on/V
MF5 – Fractured carpal bone, including scaphoid: treatment by cast immobilisation,
tati
not requiring reduction
ul
Included
See
Eligible – all MF codes.
Cons
Follow-up treatments that involve reapplying a plaster cast are also
Accident Compensation Corporation
Page 104 of 128
link to page 103 link to page 103 link to page 103 link to page 103 link to page 103 link to page 103 link to page 103
ACC Treatment Provider Handbook 2016
eligible under this code.
Excluded
If a new plaster cast isn’t required, invoice for a soft tissue injury
procedure if it involves significant best-practice soft tissue strapping
or splinting. If it doesn’t, invoice for a consultation/visit.
See a
lso Not eligible – all MF codes.
Procedures per
Recommend: three procedure claims per injury if repeated plaster
injury
casts are needed.
MF6 – Fractured tarsal or metatarsal bones (excluding calcaneum or talus):
treatment by cast immobilisation
Included
See
Eligible – all MF codes.
Excluded
If the injury needs significant best-practice soft tissue splinting (rather
than a plaster cast), invoice for a soft tissue injury procedure. If it
doesn’t, invoice for a consultation/visit.
See a
lso Not eligible – all MF codes.
Procedures per
Recommend: three procedure claims per injury if repeated plaster
injury
casts are needed.
MF7 – Fractured calcaneum or talus: treatment by cast immobilisation
Included
See
Eligible – all MF codes.
odes
Excluded
If the injury needs significant best-practice soft tissue splinting (rather
than a plaster cast), invoice for a soft tissue injury procedure. If it
and c
doesn’t, invoice for a consultation/visit.
ts
See a
lso Not eligible – all MF codes.
osc
Procedures per
Recommend: three procedure claims per injury if repeated plaster
re
injury
casts are needed.
edu
MF8 – Fractured clavicle
Included
See
Eligible – all MF codes.
Excluded
These follow-up treatments are usually covered as part of
t and proci
consultations/visits as they don’t need the same degree of
si
assessment, or any new splinting.
on/V
See a
lso Not eligible – all MF codes.
tati
Procedures per
Recommend: one procedure claim per injury.
ul
injury
MF9 – Fractured distal radius and ulna: cast immobilisation not requiring reduction
Cons
Accident Compensation Corporation
Page 105 of 128
link to page 103 link to page 103 link to page 103 link to page 103 link to page 103 link to page 103 link to page 103
ACC Treatment Provider Handbook 2016
Included
See
Eligible – all MF codes.
Follow-up treatments that involve reapplying a plaster cast are also
eligible under this code.
Excluded
Follow-up visits involving plaster checks or removal of plaster are
covered as part of consultations/visits.
See a
lso Not eligible – all MF codes.
Procedures per
Recommend: three procedure claims per injury.
injury
MF10 – Fractured distal radius and ulna requiring closed reduction, involving
regional or other form of anaesthesia
Included
See
Eligible – all MF codes.
This must involve the use of appropriate anaesthetic (intra-fracture,
arm block and/or IV sedation).
Excluded
Follow-up visits involving plaster checks or removal of plaster are
covered as part of consultations/visits.
Follow-up visits involving reapplying a plaster cast are invoiced under
MF9.
See a
lso Not eligible – all MF codes.
odes
Procedures per
Recommend: three procedure claims per injury.
injury
and c
MF11 – Fractured shaft radius and ulna: treatment by cast immobilisation
ts
osc
Included
See
Eligible – all MF codes.
re
Follow-up treatments that involve reapplying a plaster cast are also
eligible under this code.
edu
Excluded
Follow-up visits involving plaster checks or removal of plaster are
covered as part of consultations/visits.
See a
lso Not eligible – all MF codes.
t and procisi
Procedures per
Recommend: three procedure claims per injury.
injury
on/V
MF12 – Fractured distal humerus (supracondylar or condylar): by cast
tati
immobilisation
ul
Included
See
Eligible – all MF codes.
Cons
Follow-up treatments that involve reapplying a plaster cast are also
Accident Compensation Corporation
Page 106 of 128
link to page 103 link to page 103 link to page 103 link to page 103 link to page 103 link to page 103 link to page 103
ACC Treatment Provider Handbook 2016
eligible under this code.
Excluded
Follow-up visits involving plaster checks or removal of plaster are
covered as part of consultations/visits.
See a
lso Not eligible – all MF codes.
Procedures per
Recommend: three procedure claims per injury.
injury
MF13 – Fractured proximal or shaft humerus: immobilisation by collar and cuff or U-
slab
Included
See
Eligible – all MF codes.
Involves immobilisation by collar and cuff or U-slab.
Excluded
Follow-up visits involving fracture checks or removal of splinting are
covered as part of consultations/visits.
See a
lso Not eligible – all MF codes.
Procedures per
Recommend: one procedure claim per injury.
injury
MF14 – Fractured shaft tibia and/or fibula: treatment by cast immobilisation with
reduction
odes
Included
See
Eligible – all MF codes.
Follow-up treatments that involve reapplying a plaster cast are also
eligible under this code.
and c
ts
Excluded
Follow-up visits involving plaster checks or removal of plaster are
osc
covered as part of consultations/visits.
re
See a
lso Not eligible – all MF codes.
edu
Procedures per
Recommend: three procedure claims per injury.
injury
MF15 – Fractured distal tibia and/or fibula: treatment by cast immobilisation with
reduction
t and procisi
Included
See
Eligible – all MF codes.
Follow-up treatments that involve reapplying a plaster cast are also
on/V
eligible under this code.
tati
ul
Excluded
Follow-up visits involving plaster checks or removal of plaster are
covered as part of consultations/visits.
Cons
See a
lso Not eligible – all MF codes.
Accident Compensation Corporation
Page 107 of 128
link to page 103 link to page 103
ACC Treatment Provider Handbook 2016
Procedures per
Recommend: three procedure claims per injury.
injury
MF16 – Fractured fibula (without tibial fracture): immobilisation with soft tissue
splinting, strapping or cast
Included
See
Eligible – all MF codes.
Covers either best-practice soft tissue splinting or strapping, or
plaster cast if appropriate.
Follow-up treatments that involve reapplying appropriate splinting,
strapping or plaster cast are also eligible under this code.
Excluded
Follow-up visits involving fracture checks or removal of splinting are
covered as part of consultations/visits.
See a
lso Not eligible – all MF codes.
Procedures per
Recommend: one procedure claim per injury.
injury
Miscellaneous
Invoicing criteria for each MM code
MM1 – Abscess or haematoma: drainage with incision (with or without local
odes
anaesthetic agent)
Included
The incision and drainage of abscess or haematoma must involve a
and c
significant opening of lesion, drainage, and packing of cavity.
ts
os
Excluded
Simple needle aspiration without packing wound is covered as part of
c
a consultation/visit.
re
Wound check.
edu
Re-packing cavity.
Removal of dressings.
Procedures per
Recommend: one procedure claim per injury.
t and proci
injury
si
MM2 – Insertion of IV line to administer medications, electrolytes or transfusions (if
on/V
provided under local or national guideline approved by ACC)
tati
Included
Insertion of an IV cannula and administration of IV fluids or antibiotic
ul
infusion. This includes repeat infusions over a 24-hour period.
Note: This must be provided under a local or national guideline
Cons
Accident Compensation Corporation
Page 108 of 128
ACC Treatment Provider Handbook 2016
approved by ACC.
Excluded
Administration of medication into an existing IV cannula is covered as
part of a consultation/visit.
Procedures per
Recommend: one procedure claim per 24 hours. Normally no more
injury
than three IV insertions would be required.
MM3 – Nail: simple removal of
Included
Removal of an adherent nail and significant dressing of the wound.
Excluded
Removal of non-adherent nail with wounds not requiring significant
dressing.
Procedures per
Recommend: one procedure claim per injury.
injury
MM4 – Nail: removal of or wedge resection, requiring the use of digital anaesthesia
Included
Use of a digital anaesthesia, excision of wedge or whole nail,
cauterisation of wound (if necessary) and the dressing of a nail bed
with significant dressings.
Excluded
Simple nail removal.
Wound checks are covered as part of consultations/visits.
odes
Procedures per
Recommend: one procedure claim per injury.
injury
and c
MM5 – Removal of embedded or impacted foreign body from cornea or conjunctiva
ts
(with use of topical anaesthetic), or from auditory canal or nasal passages, or from
skin or subcutaneous tissue with incision, or from rectum or vagina
osc
Included
Foreign body that is impacted or embedded and requires active
re
removal.
edu
Excluded
Simple flushing or syringing, or removal using forceps or similar
instrument without use of anaesthetic or incision is covered as part
of a consultation/visit.
Fluorescein check of cornea/conjunctiva without removing
t and proci
embedded foreign body is covered as part of a consultation/visit.
si
Procedures per
Recommend: one procedure claim per injury.
on/V
injury
tati
MM6 – Pinch skin graft
ul
Included
Application of skin removed from separate site to cover open wound.
Involves the dressing of donor and graft sites.
Cons
Accident Compensation Corporation
Page 109 of 128
ACC Treatment Provider Handbook 2016
Excluded
Follow-up checks and re-dressing are covered as part of
consultations/visits unless the injury requires significant dressing, in
which case it can be invoiced for.
Procedures per
Recommend: one procedure claim per injury.
injury
MM7 – Dental anaesthetic
Included
Insertion of dental local anaesthetic using best-practice dental
treatments and procedures.
Excluded
Application of topical, oral or IV anaesthetic.
Procedures per
Recommend: one procedure claim per injury.
injury
MM8 – Epistaxis: arrest during episode by nasal cavity packing with or without
cautery
Included
Application of first-aid measures; packing of nasal cavity using ribbon
gauze; best-practice ear, nose and throat treatments and
procedures; and advice given to the client after treatment or
procedure.
Excluded
Simple first-aid epistaxis measures or simple cautery of nostril are
covered as part of consultations/visits.
odes
Removing the packing.
Procedures per
Recommend: one procedure claim per injury.
and c
injury
ts
os
c
re
Open wounds
edu
General invoicing criteria
Eligible – all MW codes
You can invoice for treating open wounds under the following eligibility criteria, if the
wounds have significant full-thickness skin damage.
t and procisi
Each service code includes tasks that can and can’t be invoiced for, on top of the general
invoicing eligibility criteria below that cover all codes.
on/V
Services that are eligible for invoicing include:
tati
ul
assessment
providing initial care, advice and patient/caregiver education
Cons
cleaning and debriding wound(s)
closing wounds by active apposition of wound edges using appropriate wound-closure
Accident Compensation Corporation
Page 110 of 128
link to page 110 link to page 111 link to page 110 link to page 111 link to page 110
ACC Treatment Provider Handbook 2016
materials, including wound-closure strips, surgical glue and equivalent adhesive and
suture materials
management by appropriate wound dressings
providing post-injury advice and patient education.
Not eligible – all MW codes
Services that are not eligible for invoicing include:
the treatment of trivial and superficial open wounds, at a first or subsequent
consultation/visit, that need no more than a minor clean, and no more than a simple
gauze, plaster strip or similar dressing. This is covered as part of a consultation/visit
follow-up consultations/visits involving wound inspections, recommendations about
infection control and dressing removal, or where re-dressings are not significant.
These are covered as part of consultations/visits.
Invoicing criteria for each MW code
The general invoicing criteria cover all MW codes, but each code may have additional
inclusions and exclusions. The details below show what can and can’t be invoiced for
under each code. MW codes are for procedures that occur within seven days of the initial
injury.
MW1 – Closure of open wounds less than 2cm
Included
Any necessary care and treatment, including cleaning, debriding,
exploration, administration of anaesthetic, and dressing. See also
Eligible – all MW codes.
odes
Excluded
See
Not eligible – all MW codes.
Procedures per
Recommend: one procedure claim per injury.
and c
injury
ts
osc
MW2 – Closure of open wound(s) of skin and subcutaneous tissue or mucous
membrane 2cm to 7cm long
re
Included
Any necessary care and treatment including cleaning, debriding,
edu
exploration, administration of anaesthetic, and dressing. See also
Eligible – all MW codes.
Excluded
See
Not eligible – all MW codes.
t and proci
Procedures per
Recommend: one procedure claim per injury.
si
injury
MW3 – Closure of open wound(s) of skin and subcutaneous tissue or mucous
on/V
membrane greater than 7cm long
tati
ul
Included
Any necessary care and treatment including cleaning, debriding,
exploration, administration of anaesthetic, and dressing. See also
Eligible – all MW codes.
Cons
Accident Compensation Corporation
Page 111 of 128
link to page 111 link to page 110 link to page 111
ACC Treatment Provider Handbook 2016
Excluded
See
Not eligible – all MW codes.
Procedures per
Recommend: one procedure claim per injury.
injury
MW4 – Amputation of digit: including use of anaesthetic, debridement of bone and
soft tissue, closure of wound
Included
Removal of the whole or part of a digit, requiring use of a local
anaesthetic, active excision and debridement of wound, attempted
stump closure using flap or equivalent technique, and appropriate
dressing of wound.
See a
lso Eligible – all MW codes.
Excluded
Follow-up wound checks.
Removal of dressings.
See a
lso Not eligible – all MW codes.
Procedures per
Recommend: one procedure claim per injury.
injury
This section should be read in conjunction with the
ACC2136 MB and MW Codes.
Soft tissue injuries
odes
General invoicing criteria
You can invoice for sprains or soft tissue injuries that need compression or other best-
and c
ts
practice splinting.
osc
Each service code includes tasks that can and can’t be invoiced on top of the general
invoicing eligibility criteria below that cover all codes.
re
Eligible – all MT codes
edu
Services that are eligible for invoicing include:
assessment
providing initial care, advice and patient education
t and proci
referral for and review of X-ray (if necessary)
si
management by best-practice splinting (this may include providing a plaster cast)
providing post-injury advice and patient education.
on/V
Not eligible – all MT codes
tati
ul
The service that isn’t eligible for invoicing is:
ons
minor soft tissue trauma involving the use of initial care and advice (such as rest, ice,
C
compression and elevation (RICE)), and not requiring the application of simple wound
compression, which is covered as part of a consultation/visit.
Accident Compensation Corporation
Page 112 of 128
link to page 112 link to page 112 link to page 112 link to page 112 link to page 112 link to page 112
ACC Treatment Provider Handbook 2016
Invoicing criteria for each MT code
The general invoicing criteria cover all MT codes, but each code may have additional
inclusions and exclusions. The details below show what can and can’t be invoiced for
under each code.
MT1 – Significant soft tissue injuries: managing simple sprain of
wrist/ankle/knee/elbow or other soft tissue injury requiring crepe bandage or similar
immobilisation not requiring formal strapping
Included
Splinting or compression dressings. Management of dislocations,
subluxations and minor fractures that don’t need plaster cast
immobilisation.
See a
lso Eligible – all MT codes.
Excluded
See
Not eligible – all MT codes.
Procedures per
Recommend: one procedure claim per injury.
injury
MT2 – Soft tissue injury (other than splinting of dislocated or fractured digit), unless
specified elsewhere
Included
Limited best-practice application of plaster cast, padded splint or
specific strapping to significant soft tissue injury (such as strained or
ruptured Achilles tendon or serious ankle sprain) that needs more
than three weeks’ immobilisation. See also
Eligible – all MT codes.
odes
Excluded
Soft tissue injuries requiring less than three weeks’ splinting or
compression are invoiced under MT1.
and c
ts
See a
lso Not eligible – all MT codes.
osc
Procedures per
Recommend: one procedure claim per injury.
injury
re
MT3 – Aspiration of inflamed joint, tendon, bursa or other subcutaneous tissue or
edu
space (with or without injection)
Included
Significant soft tissue inflammation requiring either aspiration or
injection of steroid, or both.
t and proci
See a
lso Eligible – all MT codes.
si
Excluded
See
Not eligible – all MT codes.
on/V
Procedures per
Recommend: two procedure claims per injury.
tati
injury
ul
MT4 – Extensor tendon, primary repair
Cons
Included
Primary repair of significantly damaged extensor tendon, requiring
Accident Compensation Corporation
Page 113 of 128
link to page 112 link to page 112 link to page 112 link to page 112
ACC Treatment Provider Handbook 2016
use of local anaesthetic and surgical repair using best-practice
techniques. Dressing of wound, splinting of limb or digit, and
providing post-operative advice. See a
lso Eligible – all MT codes.
Excluded
Follow-up checks, including removal of dressings, are covered as
part of consultations/visits.
See a
lso Not eligible – all MT codes.
Procedures per
Recommend: one procedure claim per injury.
injury
MT5 – Ruptured tendon Achilles: management by plaster immobilisation
Included
Rupture of Achilles tendon requiring plaster cast immobilisation for
more than three weeks. Repeat applications of plaster cast. See also
Eligible – all MT codes.
Excluded
Soft tissue splinting of strained or ruptured Achilles tendon for more
than three weeks is invoiced under MT2.
Soft tissue splinting or other care to strained Achilles tendon is
invoiced under MT1.
Follow-up checks, removal of plaster cast without re-applying the
cast are covered as part of the consultation/visit.
See a
lso Not eligible – all MT codes.
odes
Procedures per
Recommend: three procedure claims per injury.
injury
and c
ts
osc
re
edu
t and procisi
on/V
tati
ul
Cons
Accident Compensation Corporation
Page 114 of 128
link to page 48 link to page 48
ACC Treatment Provider Handbook 2016
11. Glossary
Introduction
Definitions relating to the Regulations
This glossary covers terms used by treatment providers working under ACC’s legislation.
Accordingly, most of the terms relate to the
AC Act and associated ACC-specific
regulations, such as the
Accident Compensation (Liability to Pay or Contribute to Cost of
Treatment) Regulations 2003.
Definitions specific to contracts are not covered
If definitions in this Glossary differ from terms and definitions in service specifications (for
example, the understanding of consultations/visits for providers working under the ACC
Rural General Practice Services contract), the contract versions apply.
Other definitions
You might also find the gene
ral Glossary of ACC terms helpful.
Definitions
Term
Meaning
ACC18 Medical
This certificate is completed by a medical practitioner or nurse
Certificate form
practitioner to describe how an injury has affected a patient’s capacity
for work when they can’t continue in their normal employment for a
time because of their injury; or to confirm that they’re now able to
return to their normal work.
We publish guidelines on how to complete the form and resources
that help medical and nurse practitioners to determine their
recommendations for time off work.
This certificate can also be used
to add or change a diagnosis.
ACC recommends that ACC18 Medical Certificate forms be submitted
electronically.
ACC32 Request
This form is completed by a specified treatment provider:
for Prior
Approval of
to add or change a diagnosis
Treatment form
when they believe a client needs additional treatment beyond the
treatment profile trigger numbers
when a client needs to resume treatment after more than 12
ary
months have passed
s
when a client presents for treatment for the first time for an injury
osl
more than 12 months old.
G
Accident Compensation Corporation
Page 115 of 128
ACC Treatment Provider Handbook 2016
Term
Meaning
ACC45 Injury
This form is used to lodge a new injury and to determine ACC cover
Claim form
on a person’s claim. It’s completed by both the client, who provides a
signed ‘patient authority and consent’, and the initial treatment
provider.
ACC705 Referral This form is used by a hospital to provide ACC with information about
for Support
a client’s needs when the hospital’s clinical team has identified that
Services on
the client will need home support services on discharge.
Discharge
An ACC staff member acknowledges receipt by returning the form
with details of action taken.
ACC706 Early
This form is used by a hospital to refer to ACC when the clinical team
Notification of
has identified that a patient has complex needs post-discharge and
Complex Case
will require a range of support services.
The form is sent to ACC as soon as possible so that ACC’s client
service staff can liaise with DHB staff to arrange for the required
support before the client is discharged. ACC staff return the form to
acknowledge receipt.
ACC1171
This form is used to request pharmaceutical funding approval and
Request for
should be completed by a provider and submitted to ACC before they
Funding from
prescribe a non-subsidised pharmaceutical for a client.
ACC for Non-
Subsidised
ACC may contribute towards the costs of partly and non-subsidised
Pharmaceuticals pharmaceuticals. Approvals are for a limited time.
ACC2152
This form is used by a treatment provider (always together with a new
Treatment Injury ACC45 Injury Claim form) when lodging a claim for an injury caused
Claim form
by treatment from a registered health professional.
Accident
This Act (and subsequent amendments) prescribes the ways in which
Compensation
ACC provides and pays for, or contributes to, the costs of
Act 2001
comprehensive, no-fault cover and entitlements for all New Zealand
citizens, residents and temporary visitors who sustain personal
(the
AC Act)
injuries in New Zealand.
Accredited
This is an employer who’s signed a contract with ACC to take
Employer
responsibility for the management and costs of their employees’ work-
related injuries and work related gradual process, disease or infection
claims for a specific period of time in exchange for a levy reduction.
Acute admission This is an admission to a publicly funded hospital within seven days of
a medical practitioner’s decision to admit the person to hospital,
unless otherwise specified in the
Regulations. An acute admission
ary
may be from an emergency department, outpatient department or a
s
GP/private specialist.
osl
G
Accident Compensation Corporation
Page 116 of 128
ACC Treatment Provider Handbook 2016
Term
Meaning
Acute treatment
In relation to a client, this means:
(a) the first visit to a treatment provider for treatment for a personal
injury for which the client has cover, and
(b) if, in the treatment provider’s reasonable clinical judgement, the
need for the treatment is urgent (given the likely clinical effect on
the client of any delay in treatment):
(i) any subsequent visit to that treatment provider for the
injury referred to in (a), and
(ii) any referral by that treatment provider to any other
appropriate treatment provider for the injury referred to in
(a).
From the AC Act, Part 1, Section 7
Advocacy
This service provides independent advocacy that’s free to patients
service
and funded by the
Health and Disability Commissioner. It can help
and support people to know their rights and the actions they can take
if they have concerns about any health or disability service, including
ACC.
Ancillary services These are services that are ‘ancillary’ to a client’s rehabilitation (i.e.
the client needs them to be able to access or receive their
rehabilitation).
They include emergency transport, non-emergency transport to and
from treatment, accommodation in relation to treatment, and payment
to enable a client to be escorted to and from treatment (e.g. if the
client is a child).
The
AC Act also classifies pharmaceuticals and laboratory tests as
ancillary services. Some ancillary services are funded through an
agreement with the Ministry of Health (e.g. community
pharmaceuticals and laboratory tests).
The eligibility for many ancillary services is determined by ACC’s
client service staff, taking into consideration the context of the
requests and the claims.
Annual practising This is a certificate issued annually to medical practitioners and other
certificate
health practitioners under the
HPCA Act, which allows them to
practise their professions in New Zealand. The certificate is intended
to ensure that health practitioners are competent and fit to practise.
Capacity for work This describes a person’s ability to perform work duties, based on
their education, experience or training (or any combination of these)
ary
in relation to the consequences of their personal injury.
s
osl
G
Accident Compensation Corporation
Page 117 of 128
link to page 98 link to page 98 link to page 119 link to page 119
ACC Treatment Provider Handbook 2016
Term
Meaning
Client
An ACC client is a person who’s sustained a personal injury and has
had their claim for ACC cover approved under the
AC Act or an
earlier Act.
Client consent
This is required when an ACC claim is lodged on a client’s behalf. It
authorises the treatment provider to lodge the claim and ACC to
collect and disclose certain information.
Clinical advisors
These are qualified health professionals ranging from medical
practitioners to specialist practitioners, nurses, pharmacists,
physiotherapists. Their role is to provide advice on claim cover and
entitlement, and to determine cover for treatment injury claims.
Code of Rights
All people who use health and disability services have the protection
of the ‘Code of Health and Disability Services Consumers’ Rights’. An
independent commissioner promotes and protects these rights under
legislation. More details can be found at the Health and Disability
Commissione
r website.
Consultation/Visit As defined by the
Regulations, this means an assessment in person
(face to face), and a necessary and appropriate service performed, or
treatment provided, by a provider for an injury or condition covered by
ACC. It includes providing claim-related advice, completing a
prescription or referral, and issuing any certificate to ACC as a result
of the consultation/visit.
A consultation/visit doesn’t include:
medical services where no substantial service is given by the
provider and for which the patient wouldn’t reasonably be
expected to pay
any telephone consultation
any informal encounter.
A number of minor treatments/procedures are also included in a
consultation/visit for billing purposes under the
Regulations. For
examples of these, see
Consultation/Visit and procedure costs and
codes.
Providers using hourly rates or variable fees should invoice ACC in a
way that shows the proportion of time spent directly treating the
clients’ ACC-covered injuries or conditions. (See a
lso Direct
treatment.)
Co-payment
This is a fee that a treatment provider can charge a client over and
above ACC’s contribution to the treatment, unless the provider has
ary
signed a contract with ACC that doesn’t permit them to charge co-
s
payments.
osl
G
Accident Compensation Corporation
Page 118 of 128
ACC Treatment Provider Handbook 2016
Term
Meaning
Criminal
ACC is unable to provide entitlements other than treatment to a client
disentitlement
who’s injured in the course of committing an offence for which they’re
subsequently charged, and then imprisoned or sentenced to home
detention for the offence.
Direct treatment
This means the amount of time a treatment provider directly applies
their expertise to a client’s treatment. It includes assessing and/or
reviewing their injury, developing a treatment plan with them and/or
applying direct hands-on treatment.
Discharge
This is a report prepared by a health care facility or service
summary
responsible for a person’s care when it discharges them from
inpatient, custodial or residential care.
It includes a statement on their health status immediately before
discharge, their prognosis, the nature, duration and objective of any
continuing treatment, care or support needed, and the ACC claim
number (the ACC45 number).
Doctors for
This is a professional organisation of doctors from many disciplines.
Sexual Abuse
Its prime focus is to educate and help medical practitioners to
Care (DSAC)
maintain international-best-practice medical and forensic standards
when managing victims of sexual assault. For more information, see
the DSA
C website.
Emergency
This is transport needed to get urgent treatment for a client who has a
transport
personal injury.
It must be dispatched by an Emergency Ambulance Communications
Centre from a contracted provider within 24 hours of the client
sustaining the personal injury or being found after sustaining the
injury (whichever is later). ‘Being found’ relates to situations such as
an injured person being located by a search and rescue service.
arys
osl
G
Accident Compensation Corporation
Page 119 of 128
link to page 13
ACC Treatment Provider Handbook 2016
Term
Meaning
Entitlement
A fundamental requirement of the ACC statutes is that people who
become clients with cover for personal injury can apply for
‘entitlements’. The entitlements provided under the
AC Act include:
a) rehabilitation, comprising treatment, social rehabilitation and
vocational rehabilitation
b) first-week compensation
c) weekly compensation
d) lump sum compensation for permanent impairment, or
independence allowance
e) funeral grants, survivors’ grants, weekly compensation for the
spouse (or partner), children and other dependants of a
deceased client, and child care payments.
If a client meets all the relevant statutory criteria, ACC has a legal
obligation to pay or contribute to the cost of entitlements. These are
often delivered by providers working under the
Regulations or ACC
contracts.
Hāuora Māori –
All contracts between ACC and providers include an organisational
Cultural
quality standard, a Hāuora Māori clause, which takes into account the
Competency
practical application of the articles of the Treaty of Waitangi when
providing services, and commits providers to complying with ACC’s
Guidelines on Māori Cultural Competencies for Providers.
Health
This Act supports the regulation of health practitioners in order to
Practitioners
protect the public where there is a risk of harm from the practice of
Competence
the profession.
Assurance Act
2003
(HPCA Act) This legislative framework allows for consistent procedures and
terminology across the many professions regulated by the Act. The
HPCA Act includes mechanisms to ensure that practitioners are
competent and fit to practise their professions through their working
lives.
arys
osl
G
Accident Compensation Corporation
Page 120 of 128
link to page 67
ACC Treatment Provider Handbook 2016
Term
Meaning
Home and
This service provides flexible, high-quality flexible home and
Community
community support services for Clients in their Homes and community
Support Services to support rehabilitation from their covered injury and to achieve, and
sustain, their maximum level of participation in everyday life.
There are three service types:
1. Initial Support Package: Allows DHBs to refer clients with low-
complexity and/or short-term home support needs directly to
suppliers. The service includes service set-up and up to 10 hours
of support in a two-week period.
2. Return to Independence: For clients with a time limited need for
support whilst they recover from their injuries. The service
assists clients to achieve pre-injury levels of independence in
their everyday lives.
3. Maximise Independence Service: For clients with long-term
needs for support to live their everyday lives.
Impairment
This is a general term for any loss or abnormality of the following
bodily structures or functions:
psychological (relating to the mental state)
physiological (relating to body function)
anatomical (relating to body structure).
1
Incapacity
This describes an injured person's inability to work owing to personal
injury, or an injured person’s absence from work for necessary
treatment owing to personal injury. See the
AC Act.
2
Independence
This is an entitlement for a client who, as a result of an ACC-covered
allowance
injury, has a permanent loss of bodily (physical and/or mental)
functions. The independence allowance compensates for significant
long-term impairment and is paid in addition to any other entitlements.
3
ACC requires a
n ACC18 Medical Certificate form from a medical
practitioner indicating that it’s likely there is impairment, and that the
condition is stable, before any assessment for this entitlement can be
carried out.
4
Individual
This is a plan that ACC develops in consultation with a client and their
rehabilitation
family, employer and treatment provider. It outlines the rehabilitation
plan
support needed to meet the client’s rehabilitation goals and
timeframes.
5
Injury
This was the name of the
AC Act before the passing of the Accident
Prevention,
Compensation Amendment Act 2010. Some of the regulations that
Rehabilitation,
pertain to the AC Act are still referred to as the Injury Prevention,
arys
and
Rehabilitation, and Compensation Regulations.
os6
Compensation
l
Act
G
7
Accident Compensation Corporation
Page 121 of 128
8
9
10
11
link to page 123
ACC Treatment Provider Handbook 2016
Term
Meaning
Medical advisors These are medical doctors, often with specialist qualifications, who
are part of ACC’s clinical advisor group. Their role is to provide
medical advice and guidance to case owners and other ACC staff
managing injury claims.
Medical Fees
This is ACC’s computer software system for provider contracting,
Processing
payments and service management.
(MFP)
The software:
is used to process health providers’ invoices using bulk-billing
and electronic schedules
can allow automatic approvals and payments for goods and
services that ACC purchases in relation to client rehabilitation
and treatment
handles some areas of contract management.
Mental injury
ACC covers the treatment of mental injury that is shown to be “a
clinically significant behavioural, cognitive, or psychological
dysfunction” and is the result of a covered personal injury (see
personal injury).
A mental injury must be substantial enough to be observed, be
diagnosable with a specific diagnosis and require treatment.
Missed
You can only invoice ACC for missed appointments or cancellations if
appointments
we made the appointment for the client and agreed to pay a non-
attendance fee.
National Serious This is a detailed support and rehabilitation plan developed with a
Injury Service:
client who has long-term or lifelong support needs due to a serious
Client
injury (i.e. spinal cord injury, moderate-to-severe traumatic brain
Support/Service
injury, multiple amputations or severe burns).
Plan
Each plan focuses on the client’s goals and identifies the support they
need to achieve an ‘everyday life’. The outcomes aim to maximise the
client’s independence and community participation and, if possible,
sustainable employment.
Natural use of
This means the normal use of teeth for eating, such as chewing and
teeth
biting, or using teeth to prise or tear food. Any injuries caused by the
natural use of teeth are excluded from cover under the
AC Act.
We’ll consider covering a claim for tooth damage that hasn’t been
caused by the natural use of teeth – such as a tooth damaged when a
person bites a foreign object while eating (e.g. a piece of glass in a
bread roll).
arys
osl
G
Accident Compensation Corporation
Page 122 of 128
link to page 37 link to page 37
ACC Treatment Provider Handbook 2016
Term
Meaning
Ordinarily
In general, to be ‘ordinarily resident’ a client must:
resident
hold the required citizenship, permit or visa of a New Zealand
resident, or
be the spouse or dependant of an ordinarily resident person and
generally accompany them, and have a permanent place of
residence in New Zealand, and
if overseas, have intended to return to New Zealand within six
months of leaving.
Other detailed conditions may apply.
Pain
These are designed to support a client’s broader rehabilitation goals
management
and act as an enabler for the client to access further rehabilitation
services
services that they can’t currently because of ongoing or chronic pain
conditions.
Personal injury
This means a:
physical injury
mental injury resulting from a physical injury
mental injury resulting from sexual assault or abuse
mental injury caused by a traumatic work-related event
person’s death.
Personal injury includes damage to:
dentures (other than wear and tear)
prostheses that replace a part of the human body (except for
hearing aids, spectacles and contact lenses).
Pharmaceuticals These are classified by the
AC Act as prescription medicines,
restricted medicines, pharmacy-only medicines and controlled drugs
specified in legislation controlling such substances.
ACC will only consider contributing to costs of pharmaceuticals within
this definition.
Physical injury
The category of ‘physical injury’ requires an actual diagnosis of the
injury and evidence that shows damage to the body. A diagnosis of
pain is insufficient for establishing a physical injury.
Provider claim
This framework lists injuries by description and Read Code and
lodgement
specifies the provider groups that are able to lodge
ACC45 Injury
framework
Claim forms for cover on each one.
arys
The framework is designed to support claim lodgement by providers
who are appropriate for specific types of injury.
osl
G
Accident Compensation Corporation
Page 123 of 128
link to page 126 link to page 125 link to page 75 link to page 64 link to page 64 link to page 127
ACC Treatment Provider Handbook 2016
Term
Meaning
Public Health
Acute services provided to ACC clients by DHBs are funded under
Acute Services
PHAS. ACC pays for these services through a bulk payment that’s
(PHAS)
given, via the Treasury, to the Ministry of Health.
The publicly funded acute services provided by a DHB to treat clients
for covered personal injuries are regulated by the
Injury Prevention,
Rehabilitation, and Compensation (Public Health Acute Services)
Regulations 2002. They include services provided:
as part of an acute admission
as part of an initial emergency department presentation, and any
subsequent services given by the emergency department within
seven days of that presentation
for an outpatient by a medical practitioner within six weeks of
acute discharge or emergency department attendance
by a medical practitioner within seven days of the date on which
a client is referred for those services by another medical
practitioner
that are ancillary to any of the above services, such as travel and
accommodation for a client, and an escort or support person, but
excluding emergency transport
to aid treatment as above, such as consumables, diagnostic
imaging and equipment.
PHAS also covers the costs of pharmaceuticals that are prescribed as
per the listings in all parts of the
Pharmaceutical Schedule and for
community laboratory/diagnostic tests.
Registered
This is defined in the
AC Act as:
health
professional
(a) a chiropractor, clinical dental technician, dental technician,
dentist, medical laboratory technologist, medical practitioner,
medical radiation technologist, midwife, nurse, nurse practitioner,
occupational therapist, optometrist, pharmacist, physiotherapist,
or podiatrist, and
(b) includes any person referred to in paragraph (a) who holds an
interim practising certificate but only when they’re acting in
accordance with any conditions of such interim certificate, and
(c) includes a member of any occupational group included in the
definition of ‘registered health professional’ by regulations made
unde
r section 322 of the Act.
Rehabilitation
This is a process of active change and support to help a person
regain their health and independence and therefore their ability to
participate in their usual activities as far as possible. It comprises
treatment, social rehabilitation, specialised rehabilitation, pain
sary
management and
vocational rehabilitation.
osl
G
Accident Compensation Corporation
Page 124 of 128
link to page 121
ACC Treatment Provider Handbook 2016
Term
Meaning
Rehabilitation
These are rehabilitation goals, objectives or results that may stem
outcomes
from a rehabilitation intervention, and are agreed by the client with
ACC through an
individual rehabilitation plan.
Review rights
A client has the right to have a decision made by ACC about their
claim independently reviewed within a specified timeframe. ACC is
required by its legislation to tell clients that they have the right to a
review and what the review timeframe is. Clients must be told early
enough to allow them the maximum amount of time to exercise the
right.
Scope of practice This means a health service that’s part of a health profession. Scopes
of practice for health professions covered by the
HPCA Act are
decided and published by the relevant registration authorities (e.g. the
Medical Council of New Zealand). A practitioner must practise within
any conditions imposed by their registering authority.
Self-inflicted
ACC has to decide if a self-inflicted injury or suicide was the result of
injury
a wilful act or a covered or coverable mental injury. If not, we may
withhold entitlements other than treatment.
Sensitive claims
For clients who’ve been injured by specific sexual crimes, ACC
covers mental injuries as well as any physical injuries. These are
called ‘sensitive claims’ owing to the sensitive and confidential nature
of the injuries.
ACC’s national Sensitive Claims Unit specialises in managing these
claims.
Short-term Claim ACC has Short-term Claim Centres in Christchurch, Dunedin,
Centre
Hamilton and Wellington. They typically manage claims involving mild
injuries, or injuries from which clients would usually make a complete
recovery within several weeks.
Significant
These are specialised dressings, usually of moderate to high cost per
dressings
application, or multi-layered dressings. This term doesn’t cover simple
gauze and tape, plaster strips or strips of adhesive tape, and non-
stick dressings.
Social
This helps clients to regain their independence in daily living activities
rehabilitation
as much as possible. It includes home and community services,
equipment for independence, training for independence, modification
of vehicles or home, and education support.
The provision of these services is based on the client’s injury-related
needs, identified through an appropriate assessment completed by a
ary
health professional.
s
osl
G
Accident Compensation Corporation
Page 125 of 128
link to page 67
ACC Treatment Provider Handbook 2016
Term
Meaning
Specialised
This aims to achieve the best possible rehabilitation and community
rehabilitation
participation outcomes for clients who have long-term or lifelong
support needs owing to significant injuries (e.g. spinal cord injuries or
TBI). Services include residential rehabilitation for clients who’ve
sustained spinal cord injuries, TBI residential rehabilitation, child and
adolescent rehabilitation, transition services, training for
independence, community-based rehabilitation, education support
and services for the blind.
Specified
Also known as allied providers, these are specified in the
Regulations
treatment
as acupuncturists, chiropractors, occupational therapists, osteopaths,
providers
physiotherapists, podiatrists and speech therapists.
Supervision for
Clinical supervision plays a fundamental role in the successful
counselling
progress of counselling. The
Regulations require counsellors, as
members of professional bodies, to have effective, regular and
ongoing supervision that involves ACC.
Telephone
ACC pays for counselling only when it’s provided on a face-to-face
counselling
basis. However, in a single exception under the
Regulations, we can
pay for one telephone counselling session for a client who has an
accepted sensitive claim, if they need it urgently.
Treatment
Treatment includes physical rehabilitation, cognitive rehabilitation and
an examination to provide a
medical certificate and the provision of it.
Treatment injury
This is a personal injury that’s occurred as a result of treatment
provided by, or at the direction of, one or more registered health
professionals. The injury must be directly caused by the treatment,
and can’t be a necessary part or ordinary consequence of the
required treatment.
Treatment profile These are a collection of injury profiles developed by a group of
independent practitioners that give providers standardised
expectations about treatment and incapacity. The information on each
injury includes:
appropriate treatment
the probable duration of the incapacity
the probable duration of the treatment
the possible complications
an illustration of the relevant injury site (for fractures).
Treatment profile This is the number of treatments for a specific diagnosis without
number
complications that’s been referred for treatment at an appropriate
stage in the healing process. Treatment profile numbers provide a
ary
consensus on acceptable treatment ranges.
s
osl
Treatment profile This indicates the number of treatments after which ACC would seek
G
trigger number
a review of a service that has been provided.
Accident Compensation Corporation
Page 126 of 128
ACC Treatment Provider Handbook 2016
Term
Meaning
Treatment
The following are treatment providers under the
AC Act and can lodge
provider
claims within their own scopes of practice.
acupuncturists
audiologists
chiropractors
counsellors
dentists
medical laboratory technologists
nurses and nurse practitioners
occupational therapists
optometrists
osteopaths
physiotherapists
podiatrists
medical practitioners (only medical practitioners and nurse
practitioners can give clients medical certificates for time off
work)
speech therapists.
See also ou
r Provider claim lodgement framework.
Visitors
Overseas visitors injured in New Zealand are covered by ACC, so we
can help pay for suitable treatment here if we accept their claims.
However, we can’t reimburse visitors for loss of income or for
treatment costs in their home countries.
Vocational
This means a client’s capacity, as determined by the
AC Act, to
independence
engage in work for which they’re suited by reason of experience,
education or training (or any combination thereof), and to do so for 30
hours or more a week.
Vocational
This helps a client to maintain or obtain employment, or regain or
rehabilitation
acquire vocational independence.
The employment must be appropriate to the client’s capacity to
function, and to their training and experience. Assessors are also
encouraged to take clients’ previous earning levels into account.
Weekly
This entitlement compensates a client for loss of earnings or loss of
compensation
potential earning capacity. A spouse, partner or dependant of a
deceased client may also be entitled to weekly compensation.
arys
osl
G
Accident Compensation Corporation
Page 127 of 128
ACC Treatment Provider Handbook 2016
Term
Meaning
Work-related
There are three key criteria for establishing cover for a personal injury
gradual process, caused by work-related gradual process, disease or infection.
disease or
infection
there is a particular property or characteristic in a work task or
the work environment that can be identified as having caused the
condition
the property or characteristic isn’t materially present outside the
person’s work activities or environment
those performing the work task or employed in that work
environment are at significantly greater risk of developing the
condition than those who don’t.
Any condition must meet all the criteria of the
AC Act, although some
occupational diseases are listed in Schedule 2 of the
AC Act and
have a simplified cover process.
arys
osl
G
Accident Compensation Corporation
Page 128 of 128