4 December 2017
S Ashworth
[FYI request #6752 email]
[email address]
[email address]
[email address]
Dear Ms Ashworth Reference: 0050875
Official Information Act Request
Thank you for your requests of 25 October 2017, asking for the following information under
the Official Information Act 1982 (the Act):
1. When ACC makes a decision to decline cover does it reference in the
letter communicating the decision which section(s) of the ACC Act 2001
the decision to deny cover was based on? If not, why not?
2. On what grounds can an in-house ACC medical advisor ignore or overrule
medical evidence provided by a medical specialist? If this happens, what
are the checks and balances around this process?
3. For the last 10 years, can ACC provide the number of accepted
Treatment Injuries as a result of the use of surgical instruments, including
sub-totals for the use of drills and saws?
4. For the last 10 years, can ACC provide the number of accepted / declined
ACC claims for CRPS (Chronic Regional Pain Syndrome) following
surgery.
For those declined, what were the reasons provided and against which
section(s) of the ACC Act was the decision made against? ACC may
provide summary information to ensure client confidentiality where the
reason(s) may potentially identify individuals.
In our acknowledgement email of 26 October 2017, we advised that we would be combining
our responses to your requests into one letter. We also wrote to you on 22 November 2017
to advise you that we required an extension to 6 December 2017 in order to make a decision
on your requests. Our response to each request is below.
Request One
The relevant sections of the Accident Compensation Act 2001 (AC Act) are not usual y
referred to explicitly in a decline letter, however, the reasons for a decline decision wil
always be outlined, and these are based on the provisions of the AC Act. For example, a
decline letter may state that “we can only cover accidents that result in a physical injury” or
“we’re unable to cover injuries that happened before the Accident Compensation Act came
into effect on 1 April 1974”.
Using the treatment injury decline letter as an example, it refers to the requirement for a
claim to meet the criteria for a treatment injury. In addition to this, the specific legislative
requirements for a treatment injury claim are referred to in section two of the treatment injury
report attached to the cover letter.
The legislative criteria for a treatment injury are:
the client must have suffered a personal injury
the injury must have happened in the context of treatment
there must be a clear causal link between the treatment and the injury
the injury must not be a necessary part or ordinary consequence of the treatment
the claim must not fall under any of the treatment injury exclusions from cover.
Reference is also made to the Accident Compensation Act 2001 at the bottom of the report.
The Accident Compensation Act 2001 is publicly available. You can access it online at
http://www.legislation.govt.nz/act/public/2001/0049/latest/whole.html.
Request Two
ACC medical advisors do not overrule a medical specialist’s opinion. ACC medical advisors
provide advice to case owners on various aspects of a claim. The case owner will also
consider the advice of technical specialists, who provide advice relating to legislative
requirements, along with other sources of information specific to a claim, such as medical
notes and reports from other health providers. If appropriate, they wil also seek input from
more experienced staff. Al of this information is used by the case owner to determine
whether an injury meets the requirements of the legislation and to make a decision on a
claim.
There are various medical advisors within ACC who a case owner can approach for advice.
For example, branch medical advisors help case owners understand clinical conditions to
assist them to make decisions on claims. This may relate to cover, rehabilitation, treatment
or other entitlements. ACC also has specialist medical advisors who provide advice on
claims related to their areas of expertise, such toxicology, dentistry and psychology.
Al case owners are monitored under a quality checking process to ensure that cover
decisions are consistent and robust with regard to the legislation.
Using treatment injury as an example again, when a claim is lodged, ACC seeks relevant
clinical evidence on the treatment giving rise to an injury. The opinion from the medical
specialist and/or the clinical evidence provides information to ACC about the clinical facts
specific to the client.
The investigating Treatment Injury Cover Specialists then apply the legislative criteria to the
clinical evidence to determine whether the claim meets the criteria for cover.
The Treatment Injury Cover Specialists may call on other advisors, such as ACC medical
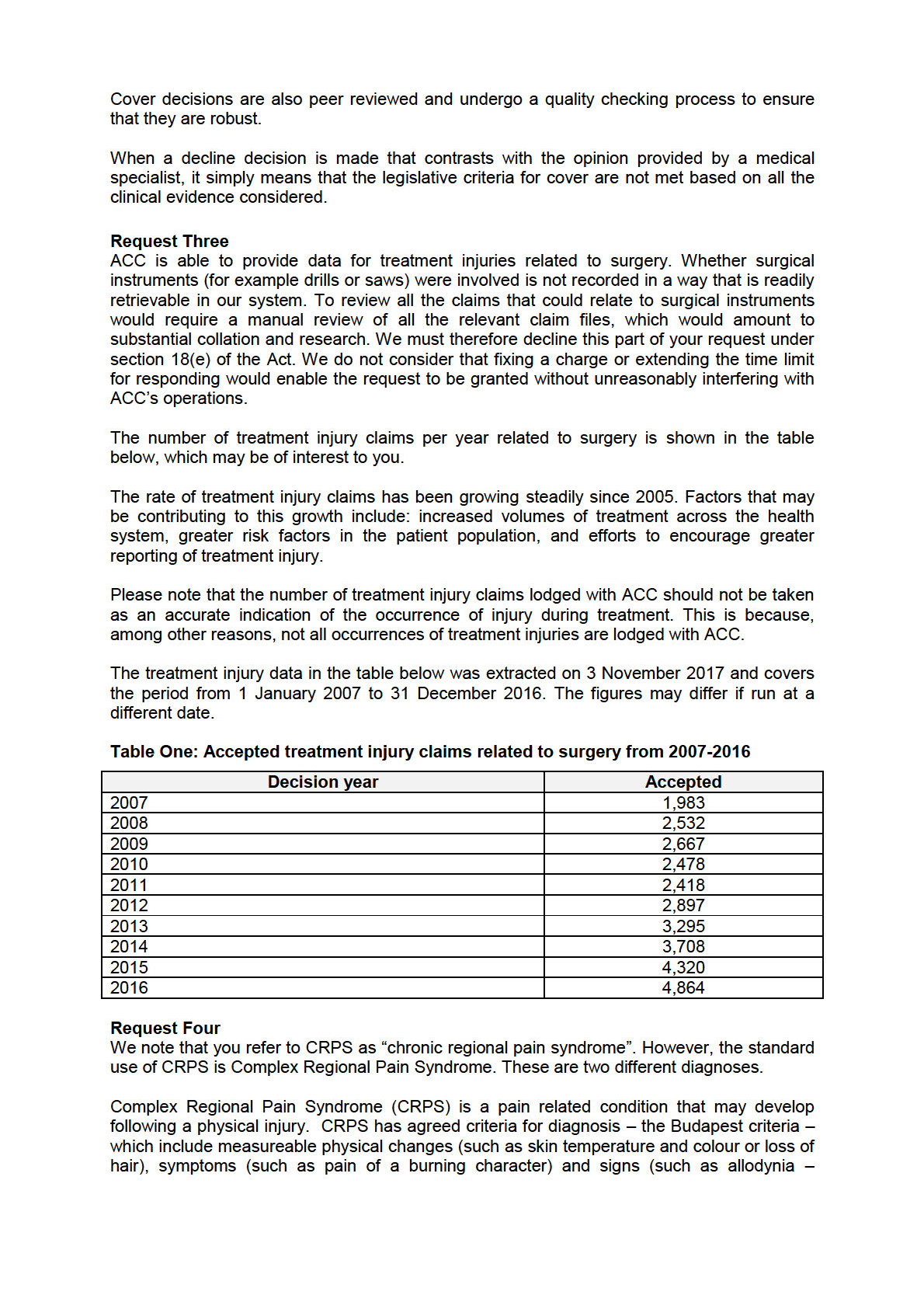
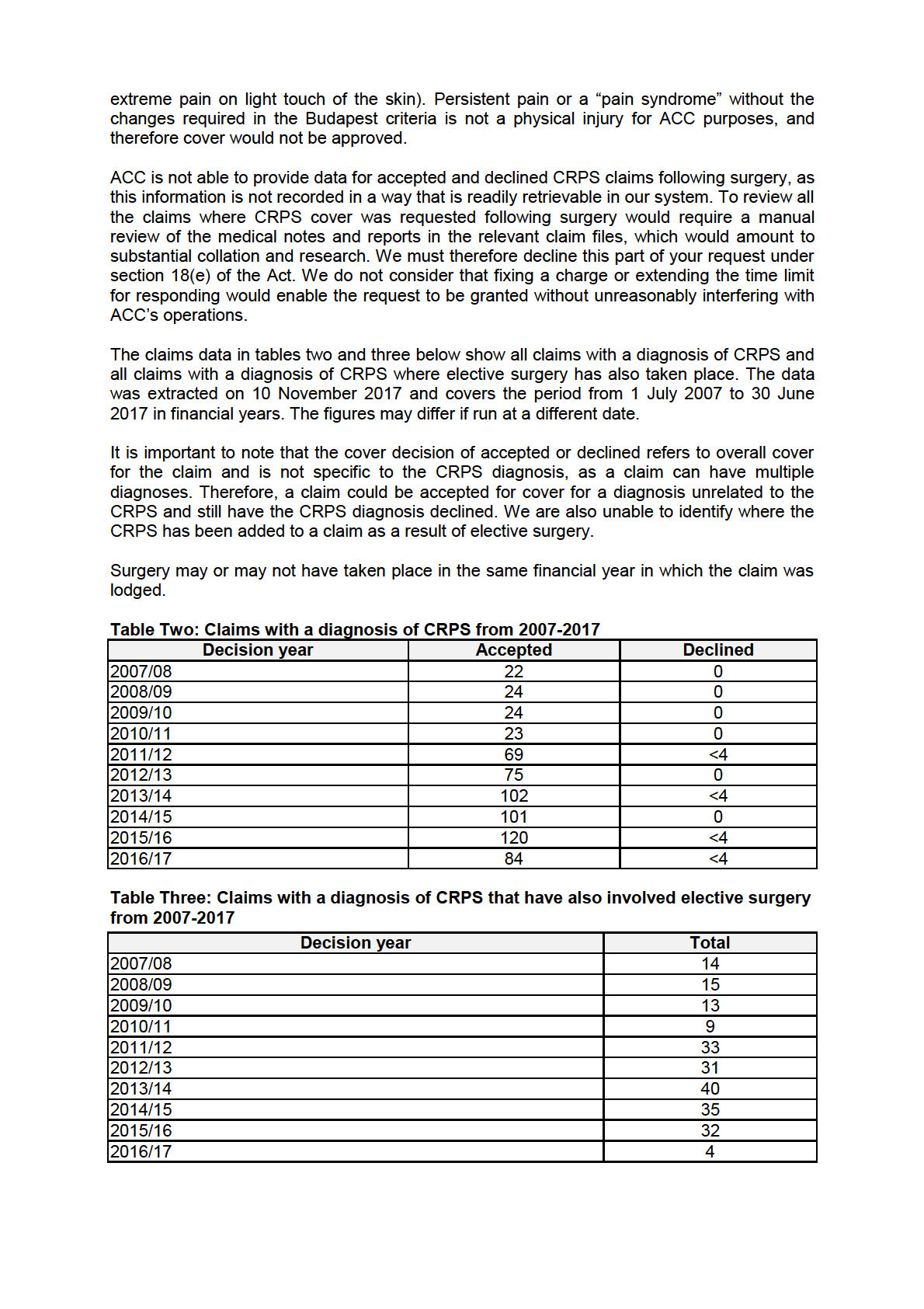
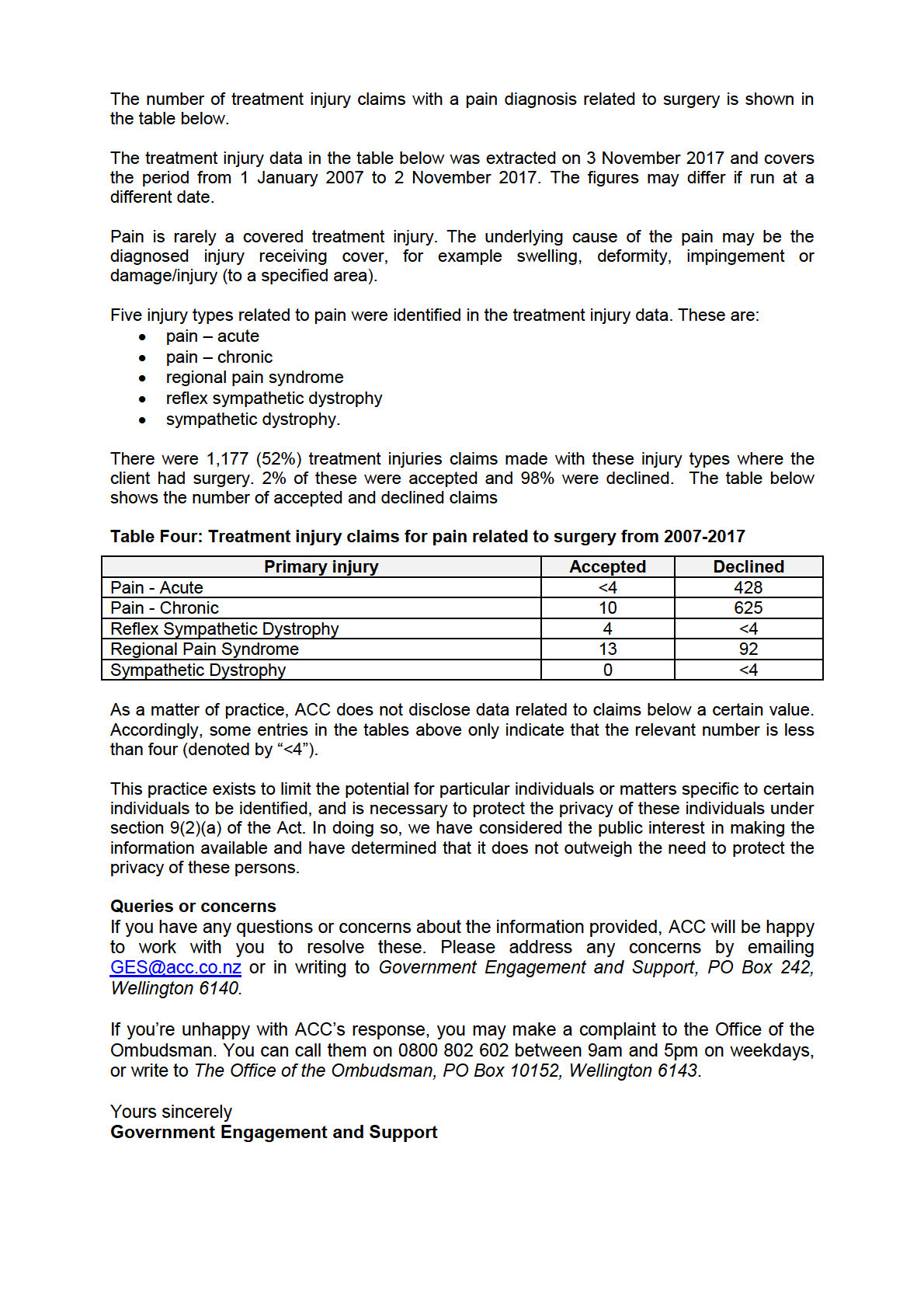
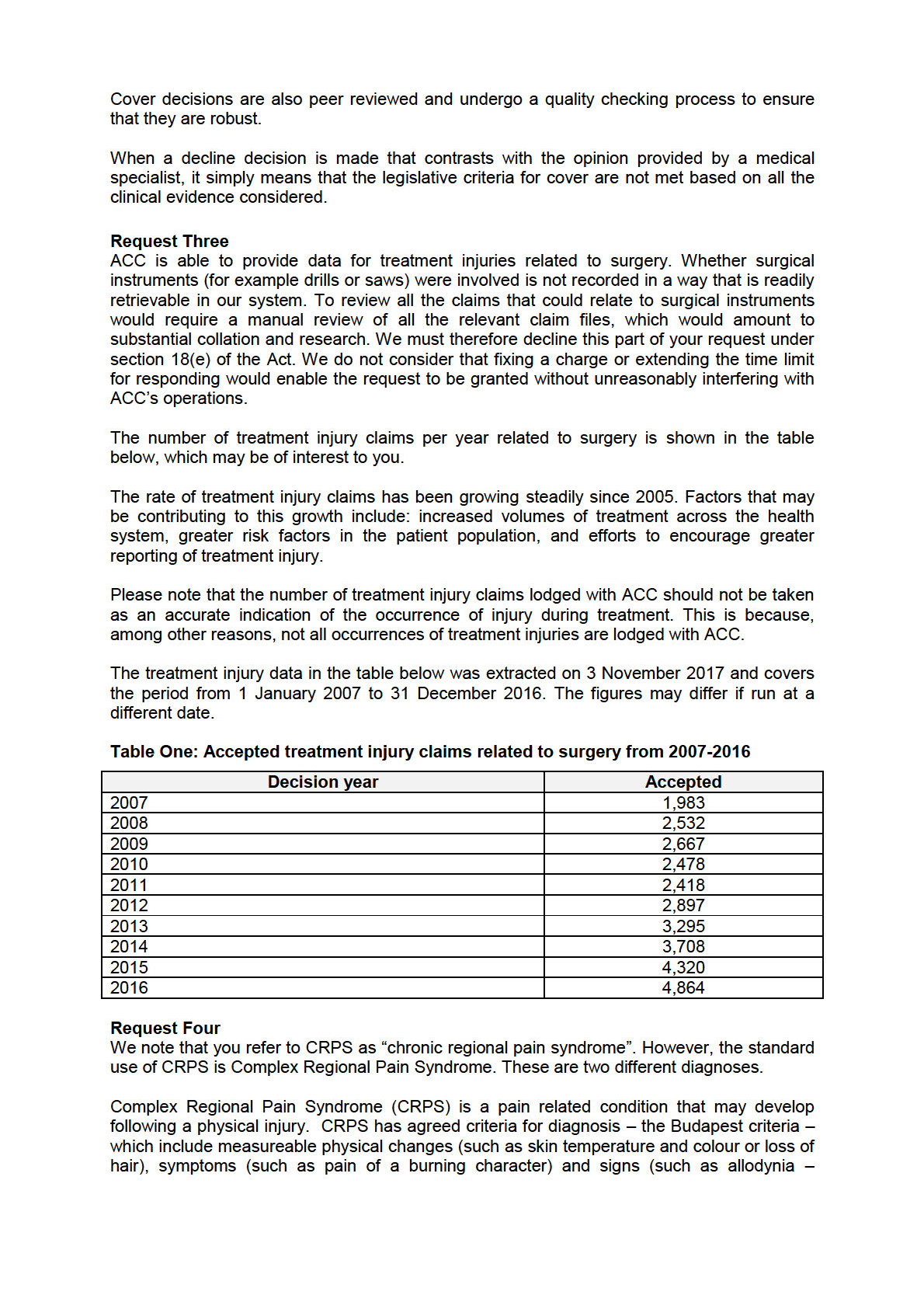
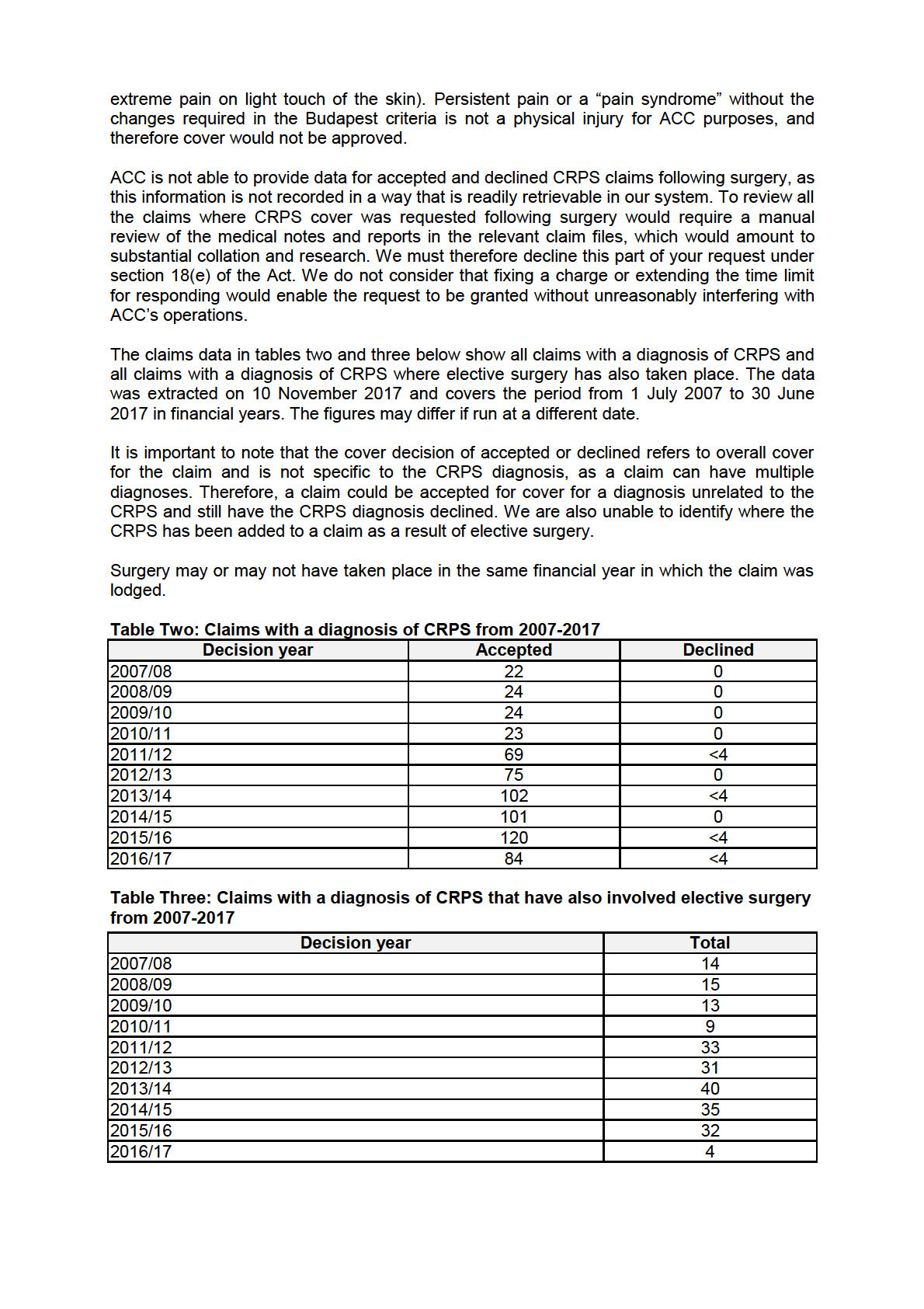
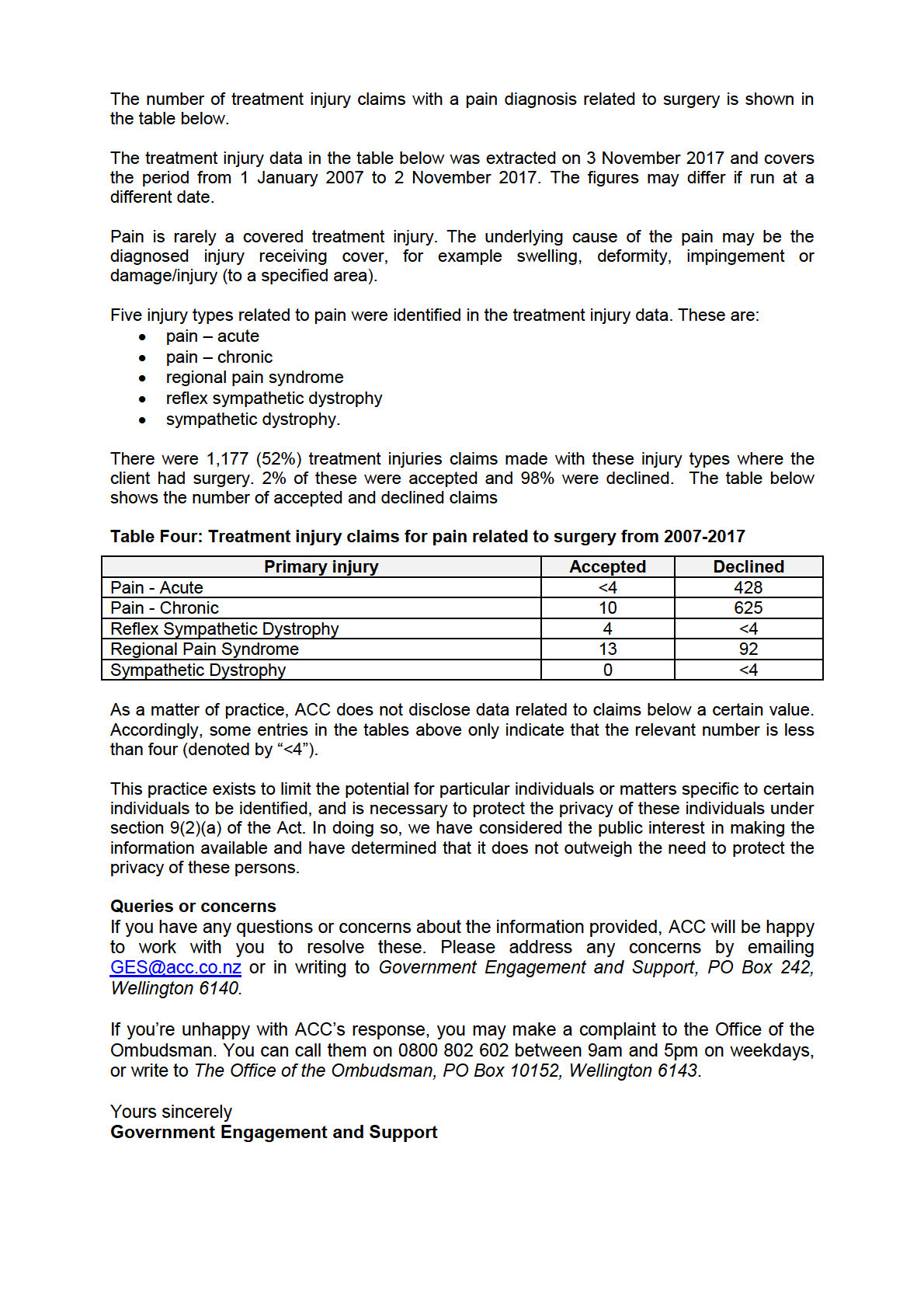
advisors or external clinical advisors, to provide advice on a claim and inform their decision.