 West Coast District Health Board
Te Poari Hauora a Rohe o Tai Poutini
Corporate Office
Telephone 03 769-7400
High Street, Greymouth 7840
Fax 03 769-7791
West Coast District Health Board
Te Poari Hauora a Rohe o Tai Poutini
Corporate Office
Telephone 03 769-7400
High Street, Greymouth 7840
Fax 03 769-7791
22 December 2017
Health Sector Workers Network
Email: [FYI request #6981 email];
Dear Health Sector Workers Network
RE Official information request WCDHB 9067
I refer to your email dated 11 December 2017, requesting the following information under section 12
of the Official Information Act pertaining to West Coast DHB Restraint Policy and the use of
mechanical restraints in all services.
Can you please provide?
1. All policy documents relating to restraint practices at West Coast DHB
2. Are there instances in the last year (June 2016 to June 2017) of the use of mechanical restraints,
(I.e. strapping arms to bed) this is also referred to as physical restraint
3. Can you please provide this data for both physical and mental health services and identify the
service associated with this data
The West Coast DHB has recently aligned its internal policy approach toward restraint minimisation
and safe practice use with that of the Canterbury DHB.
This piece of work is part of a wider organisational trans-alpine partnership approach with all generic
type clinical activity currently in progress on a range of policies. Please refer to
Appendix 1 (attached)
for the Transalpine Restraint Minimisation and Safe Practice Policy (this was approved by West Coast
DHB Restraint Committee November 2017).
There are no recorded instances of mechanical restraint used within West Coast DHB facilities for the
time period June 2016 to June 2017.
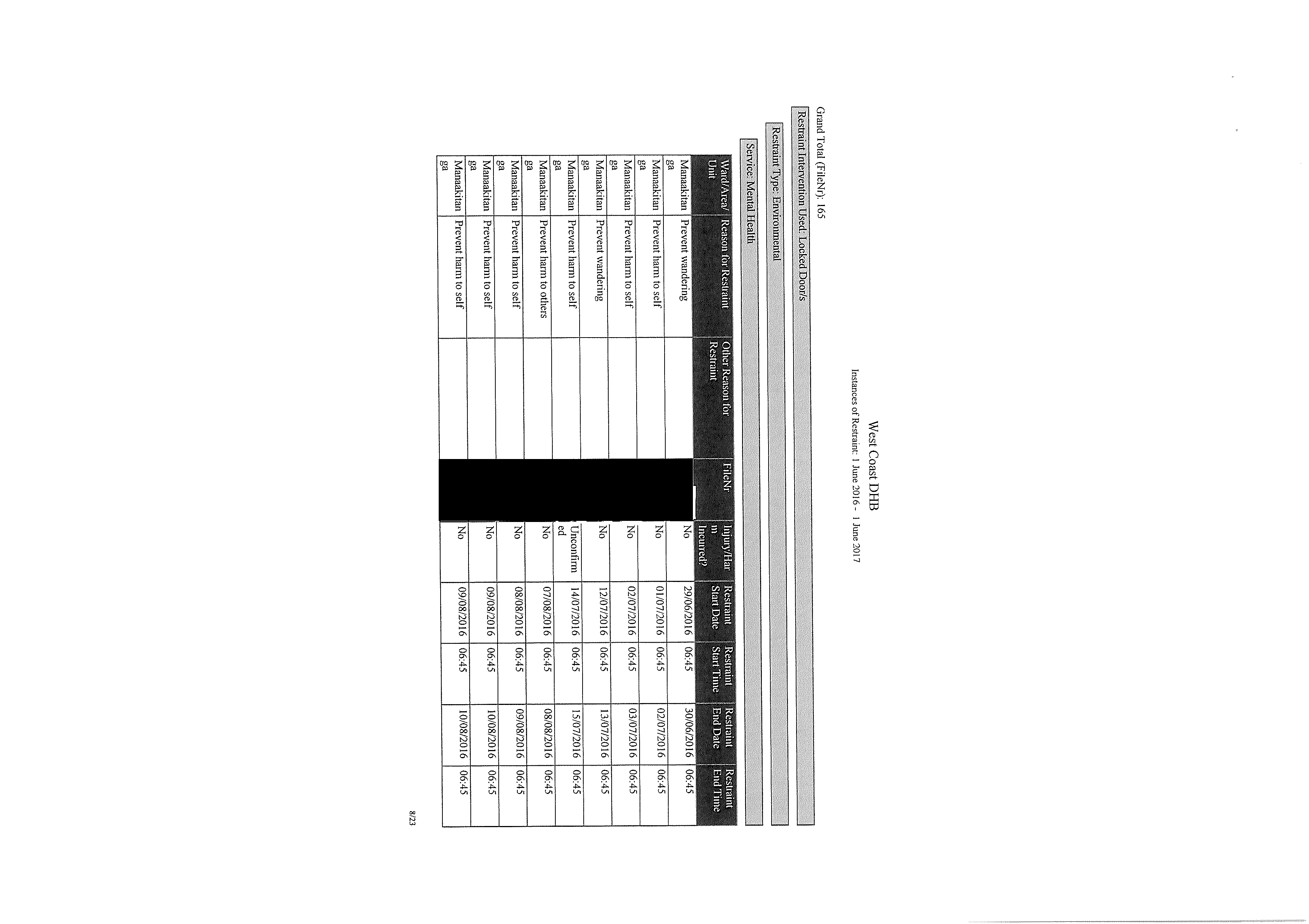
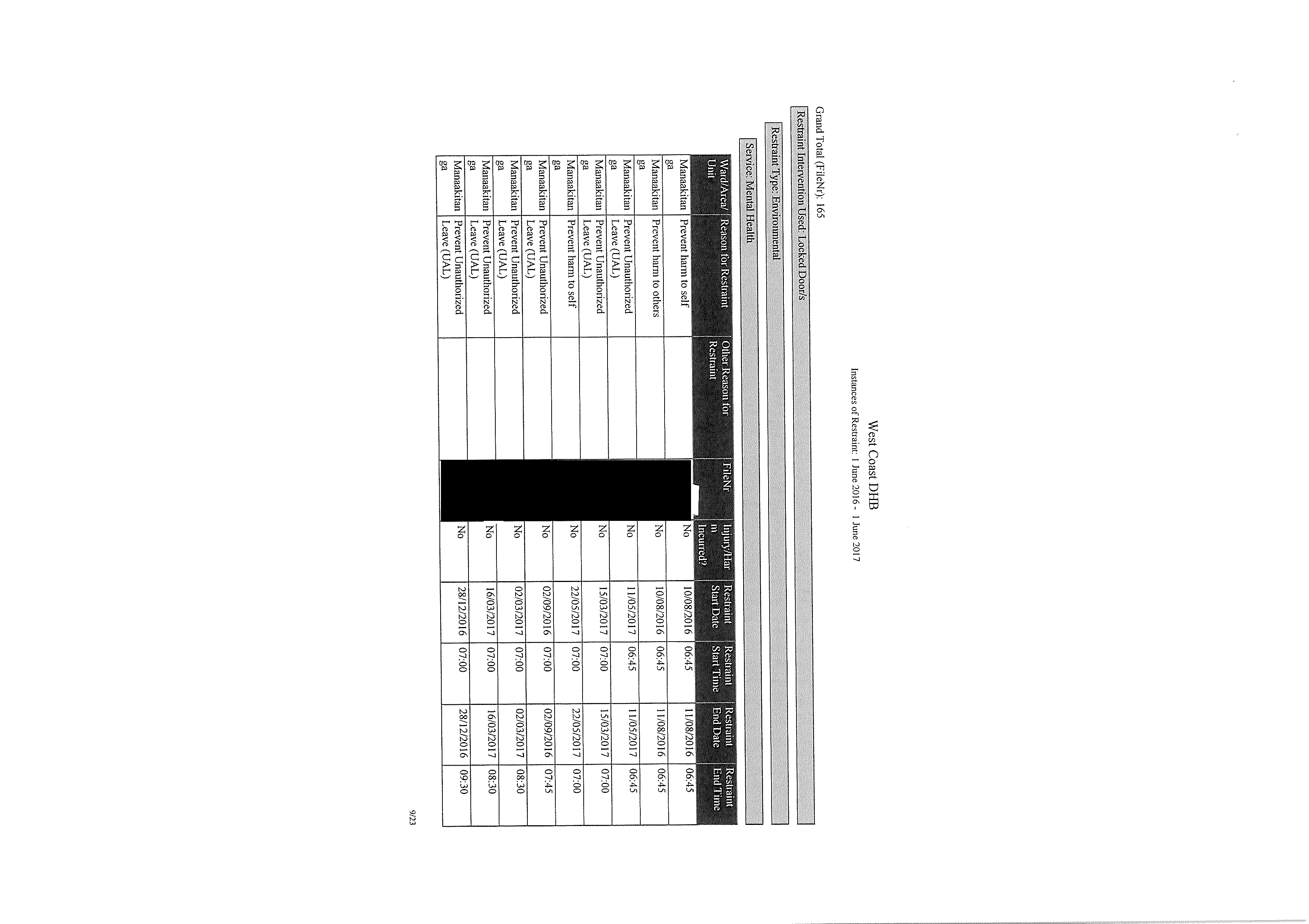
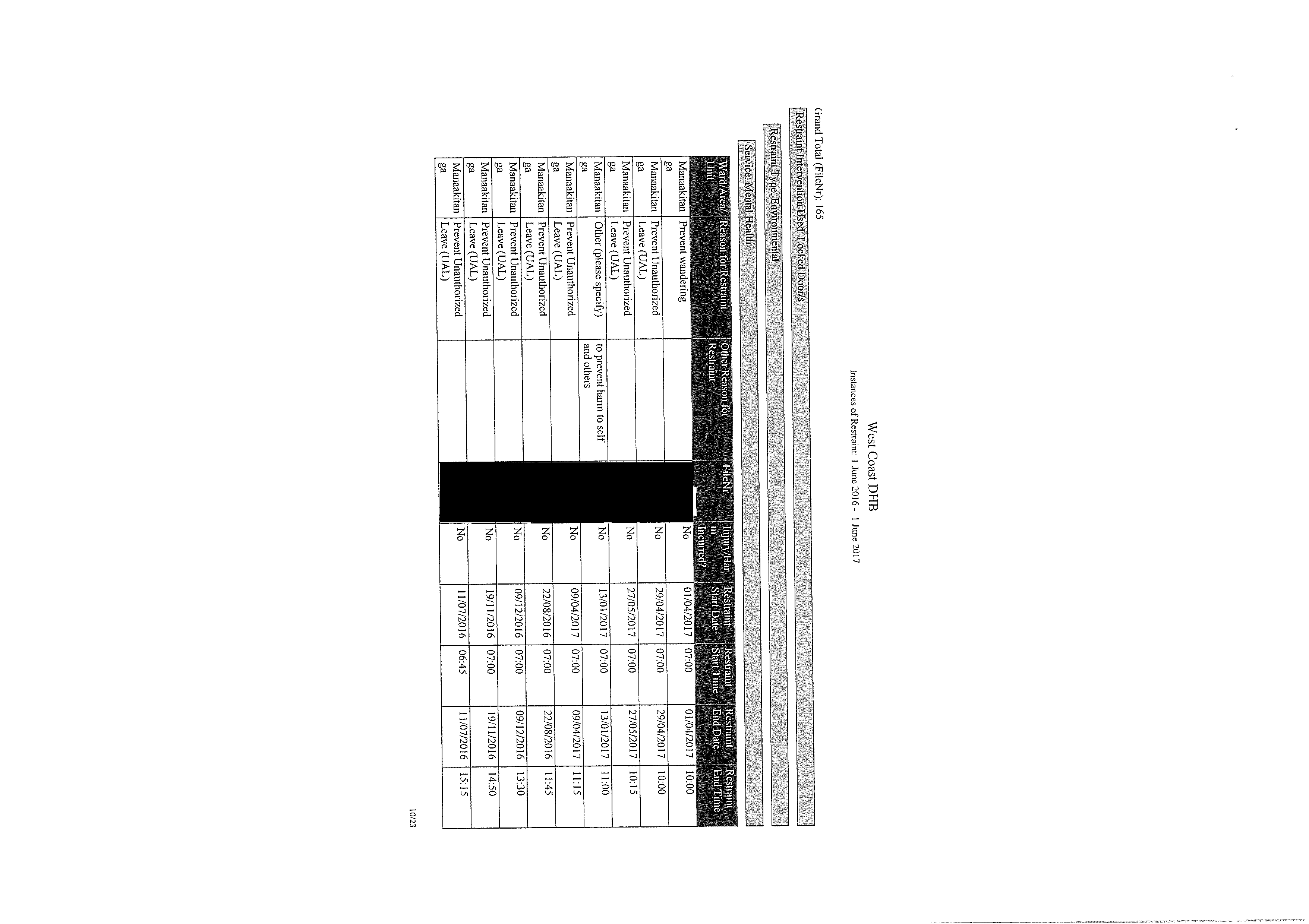
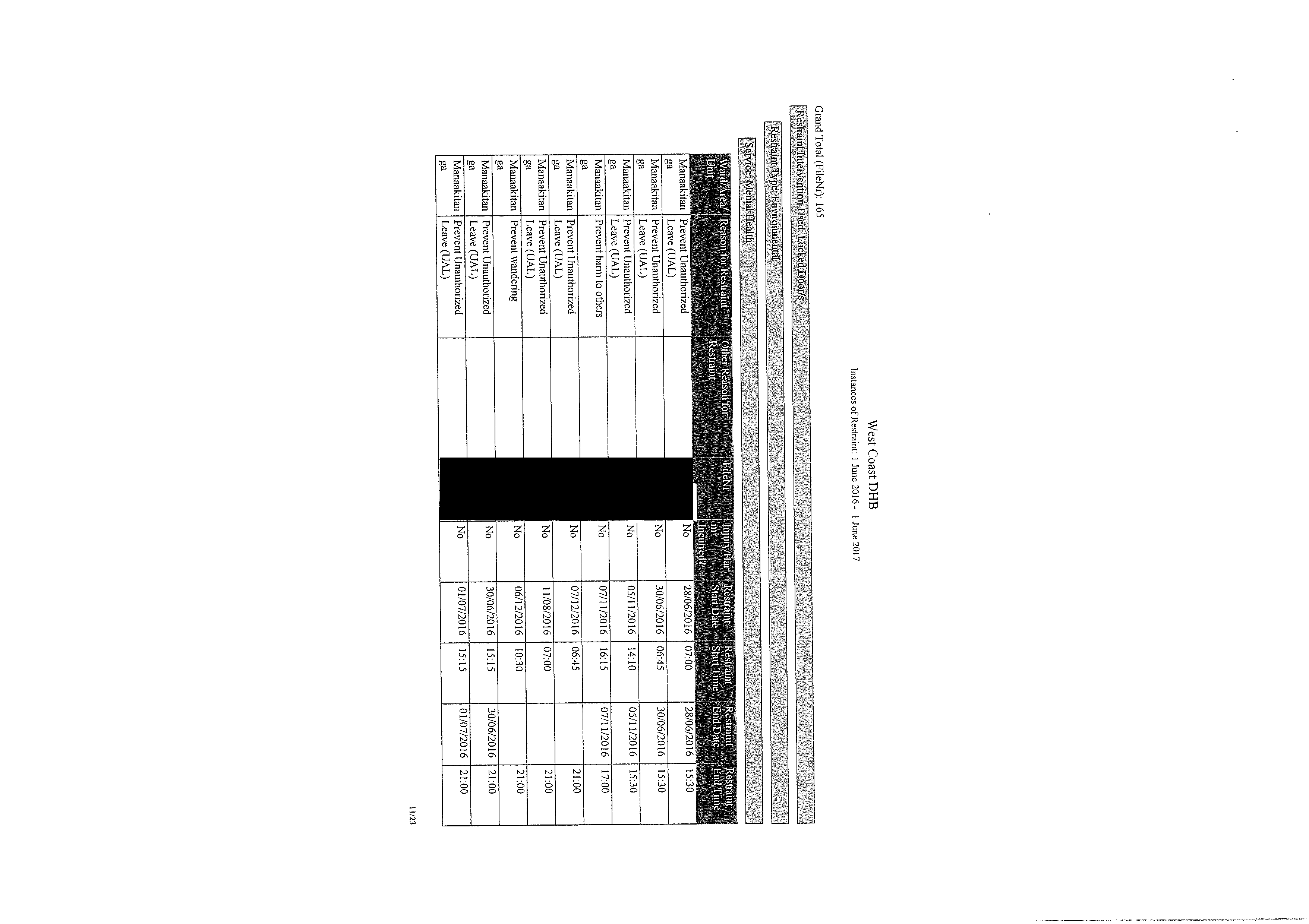
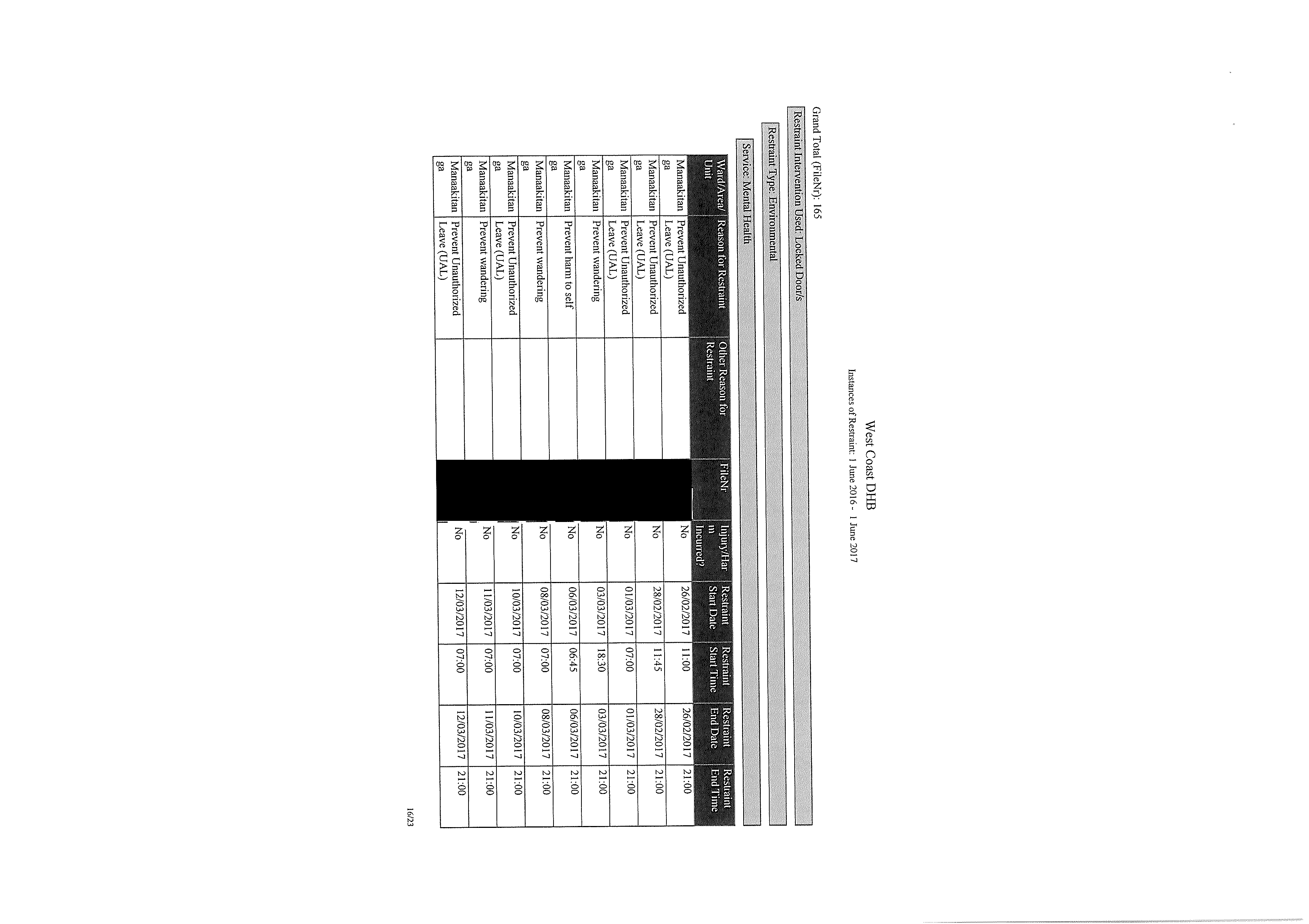
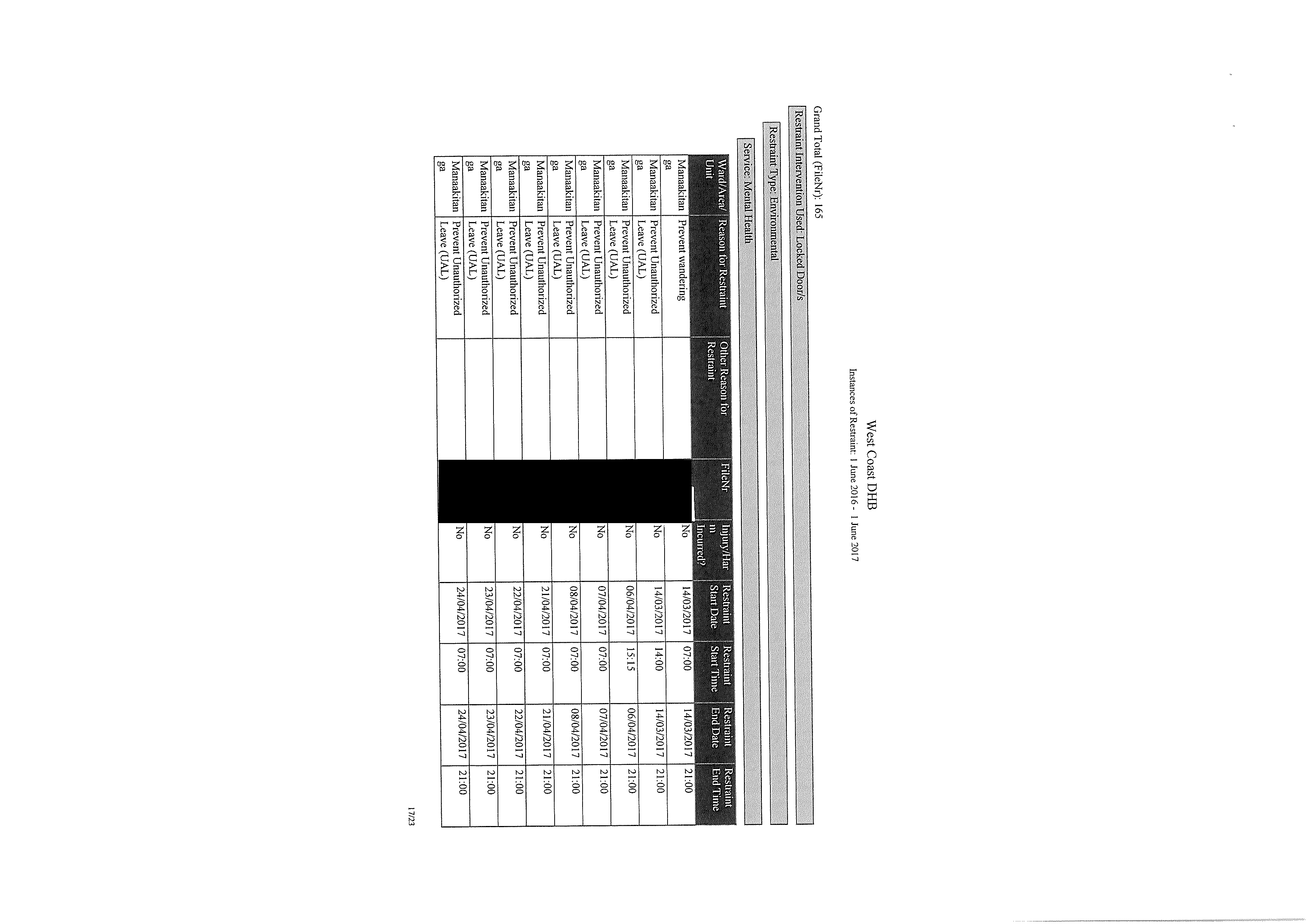
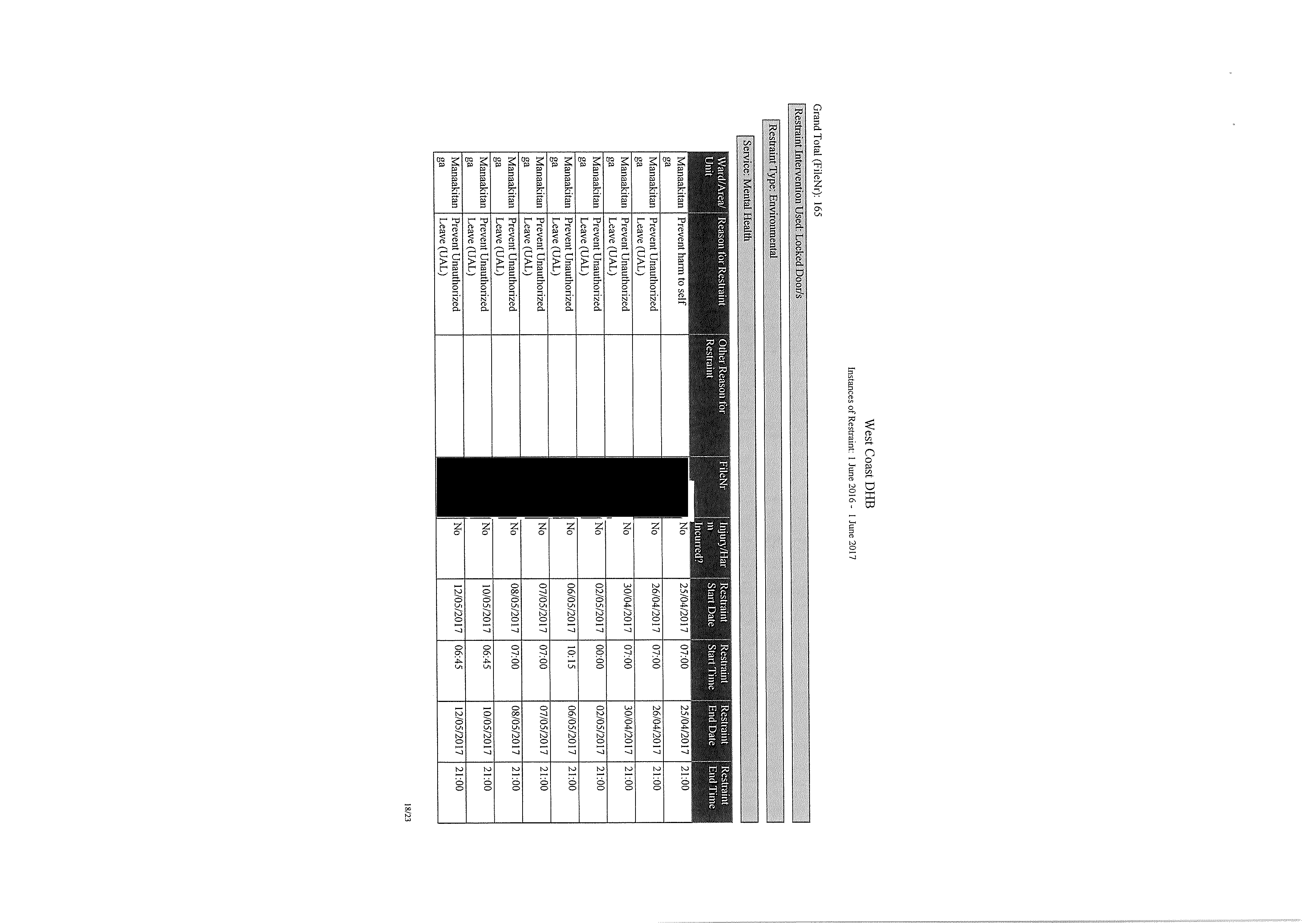
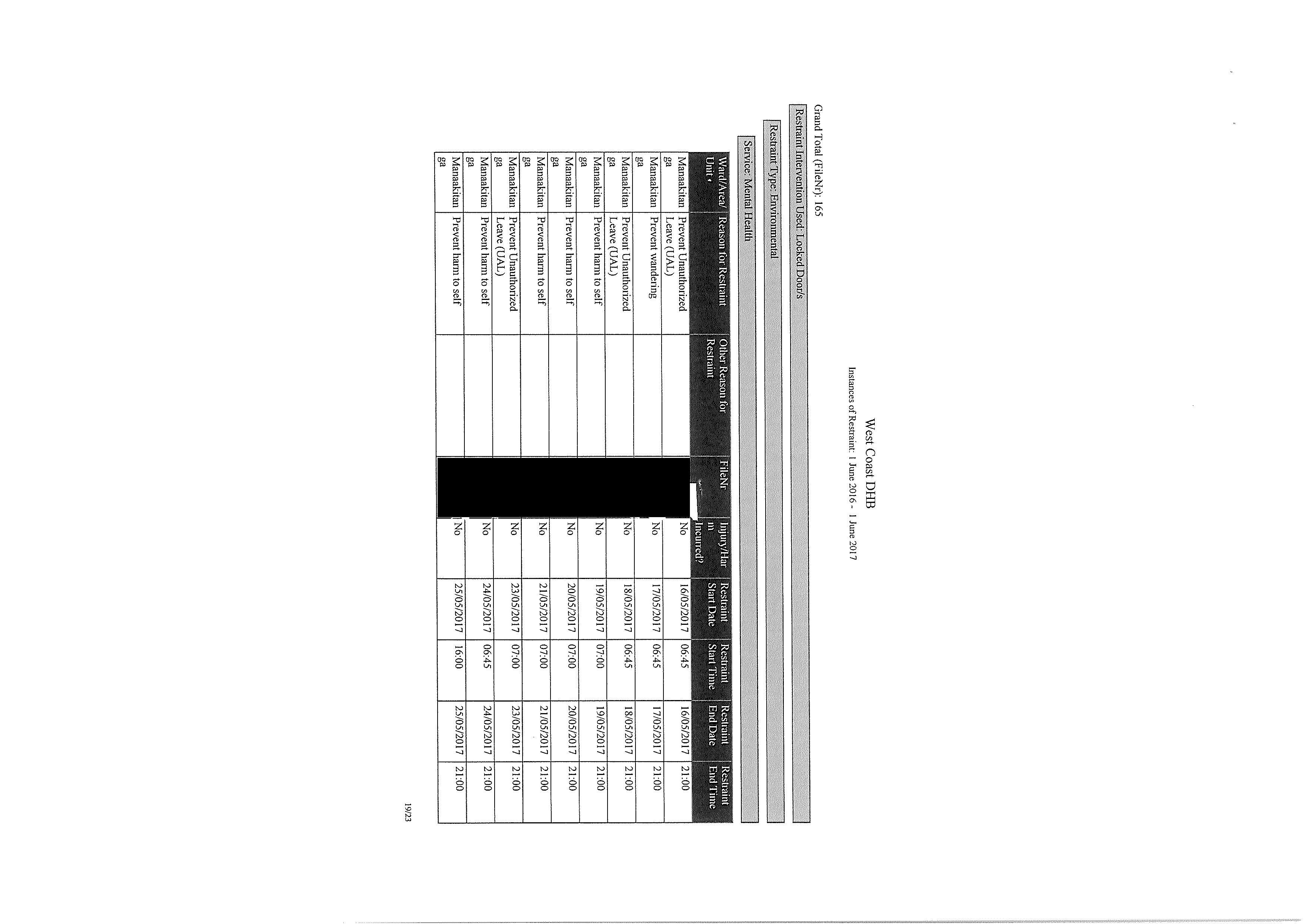
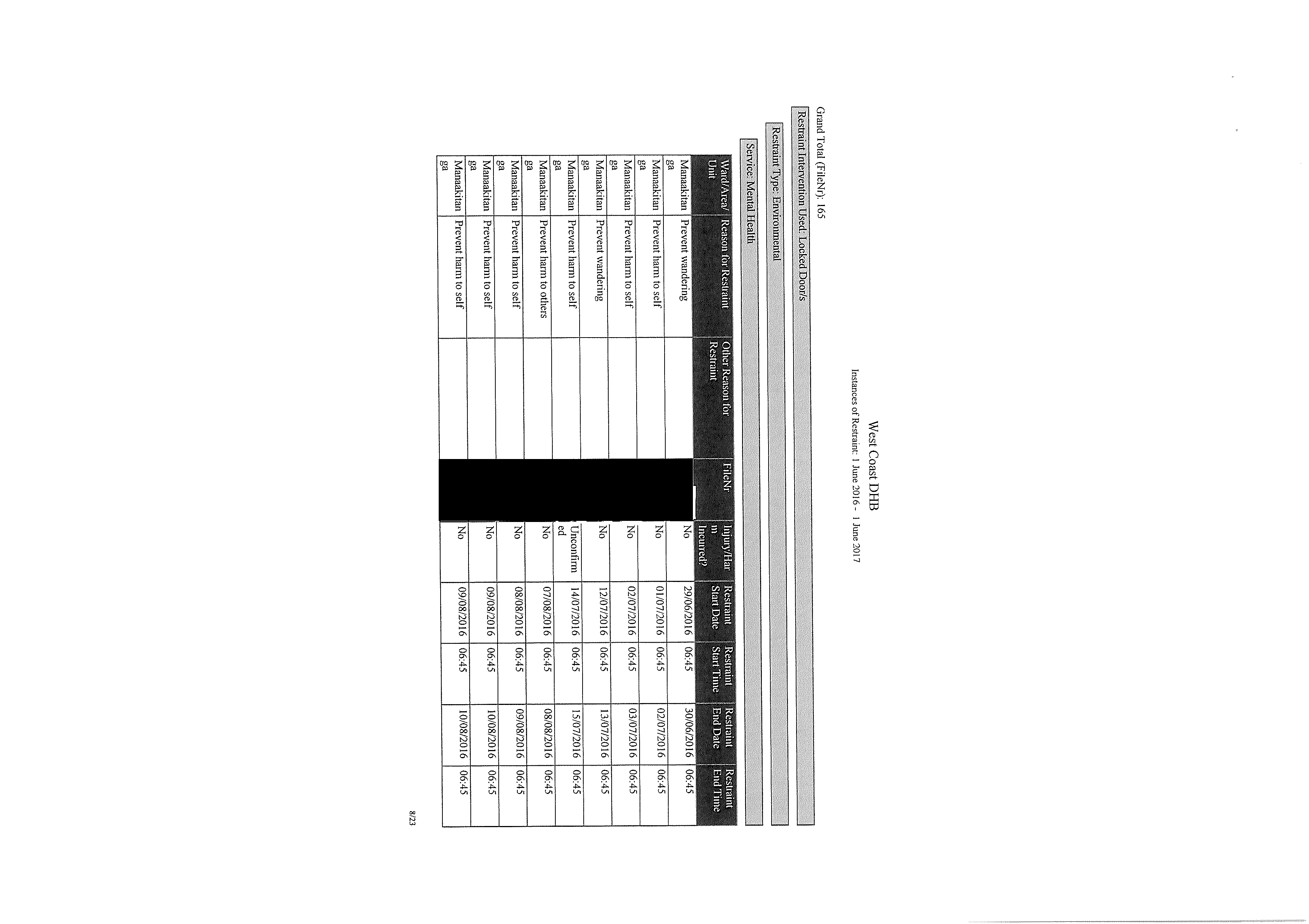
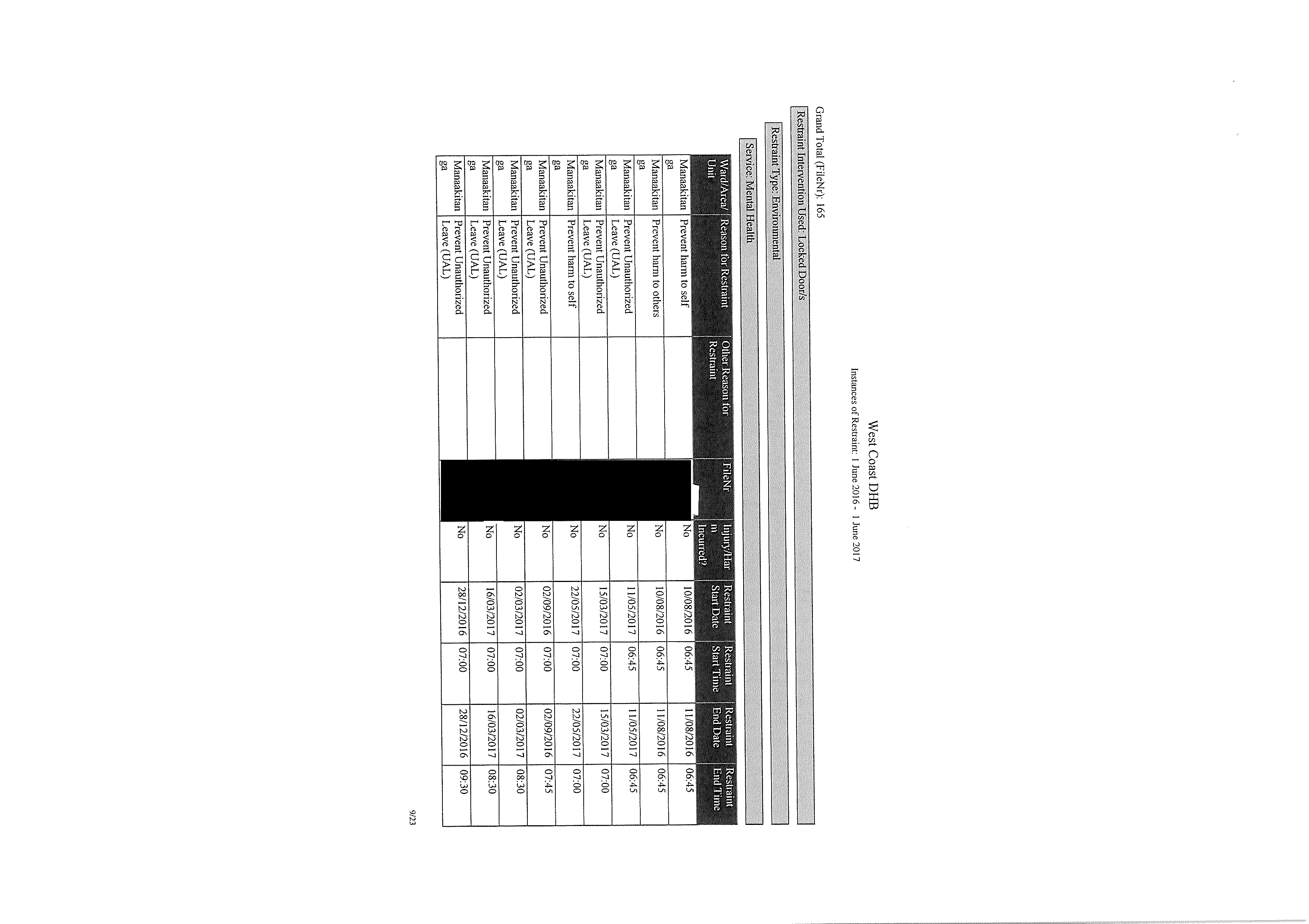
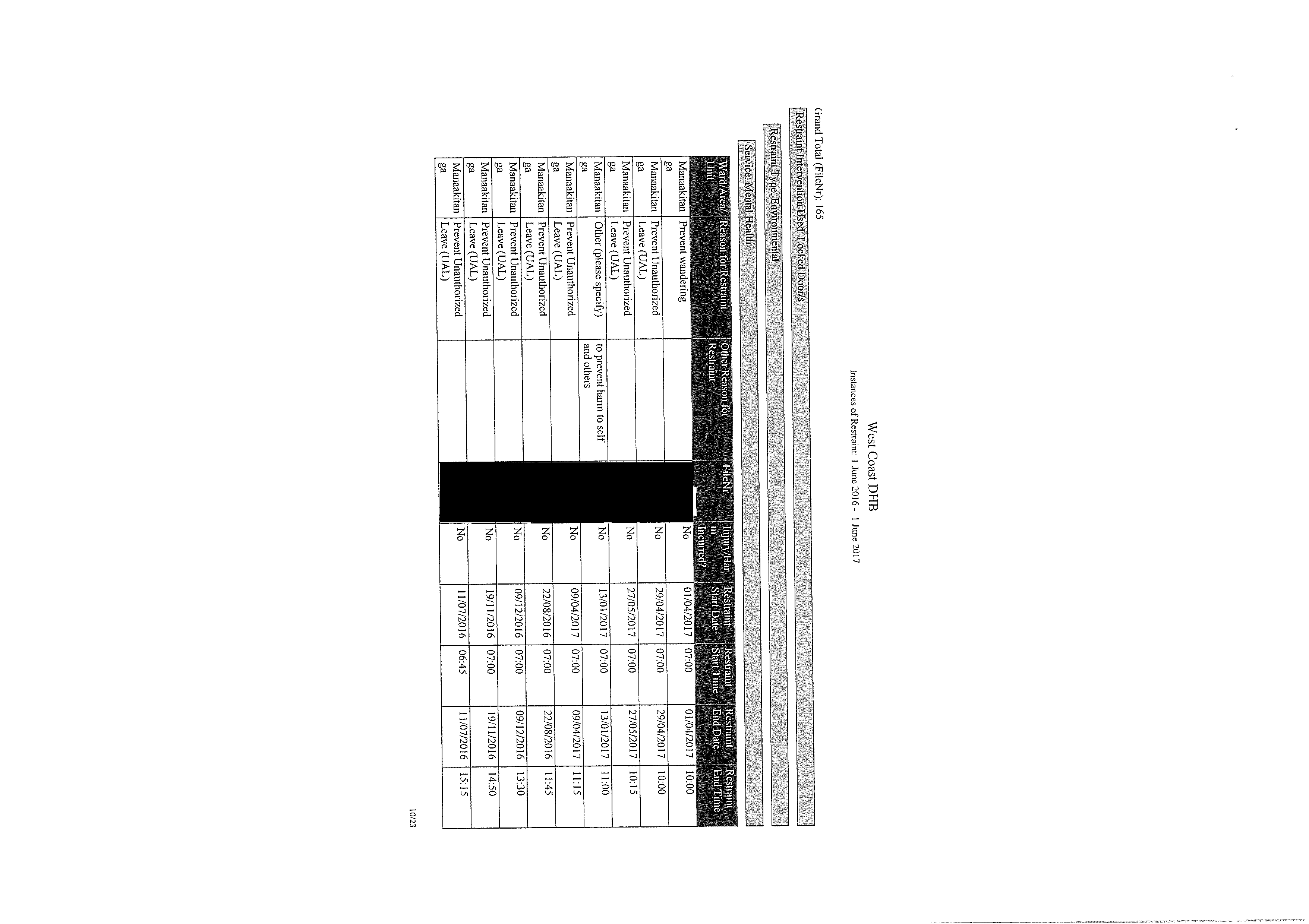
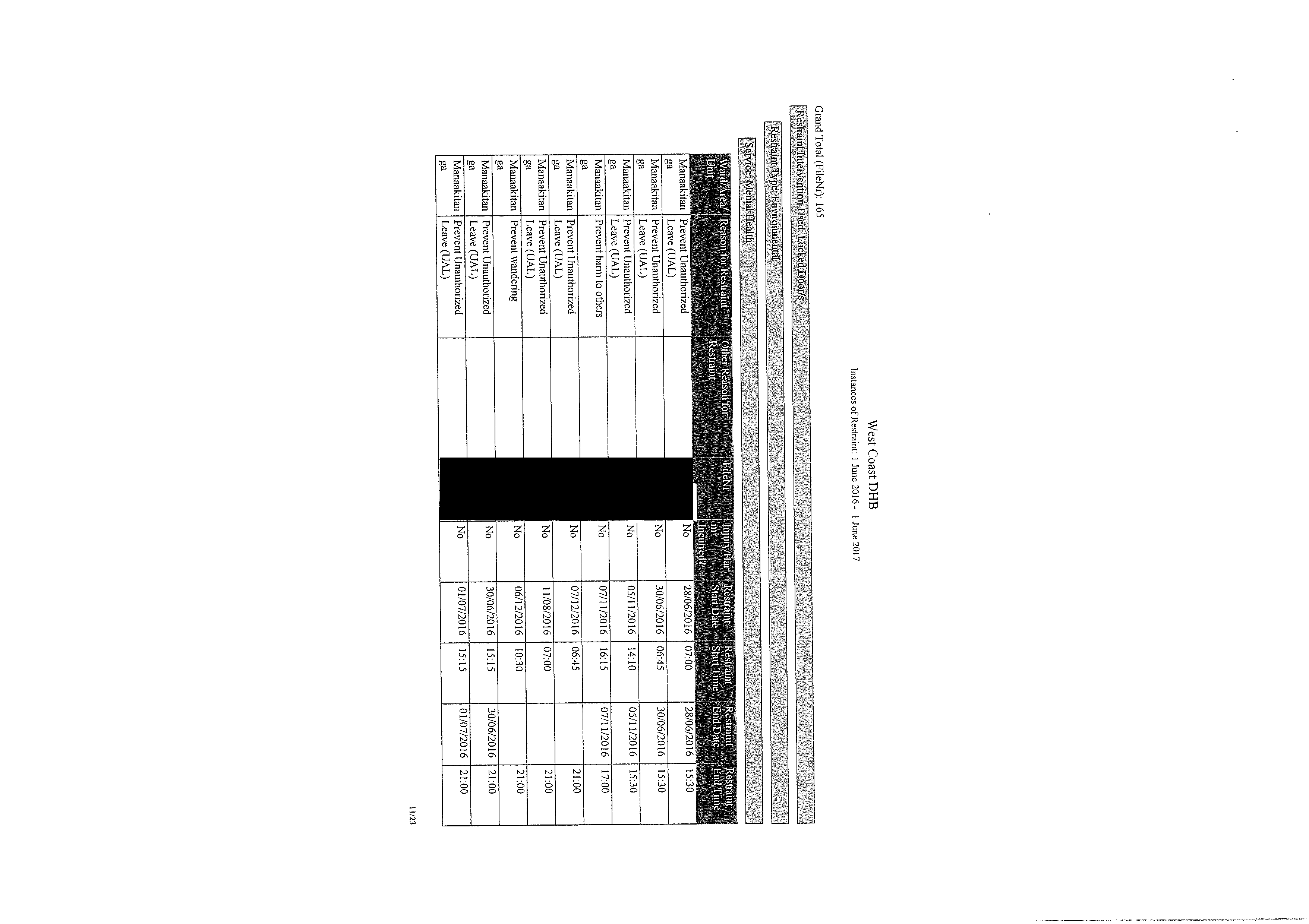
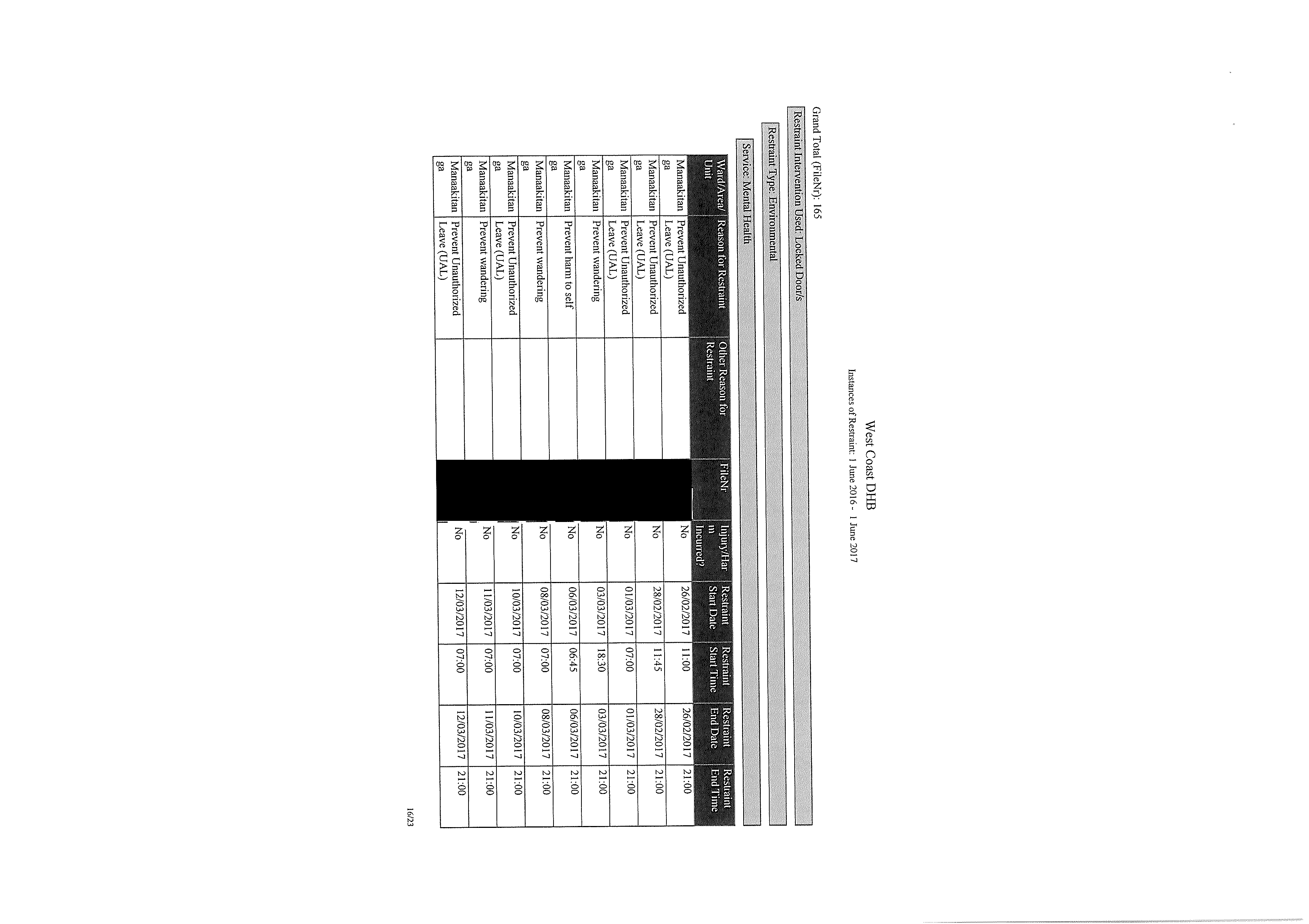
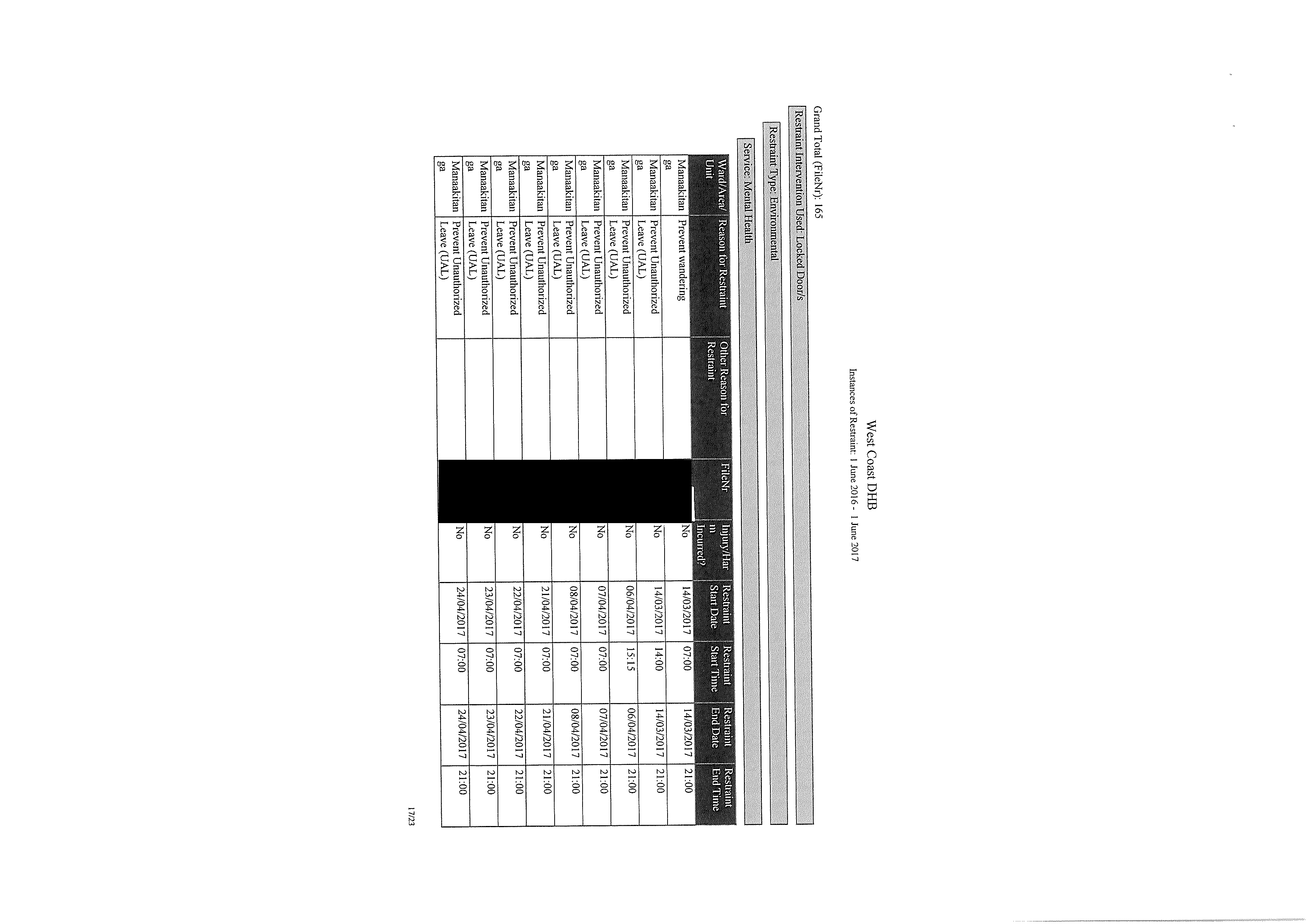
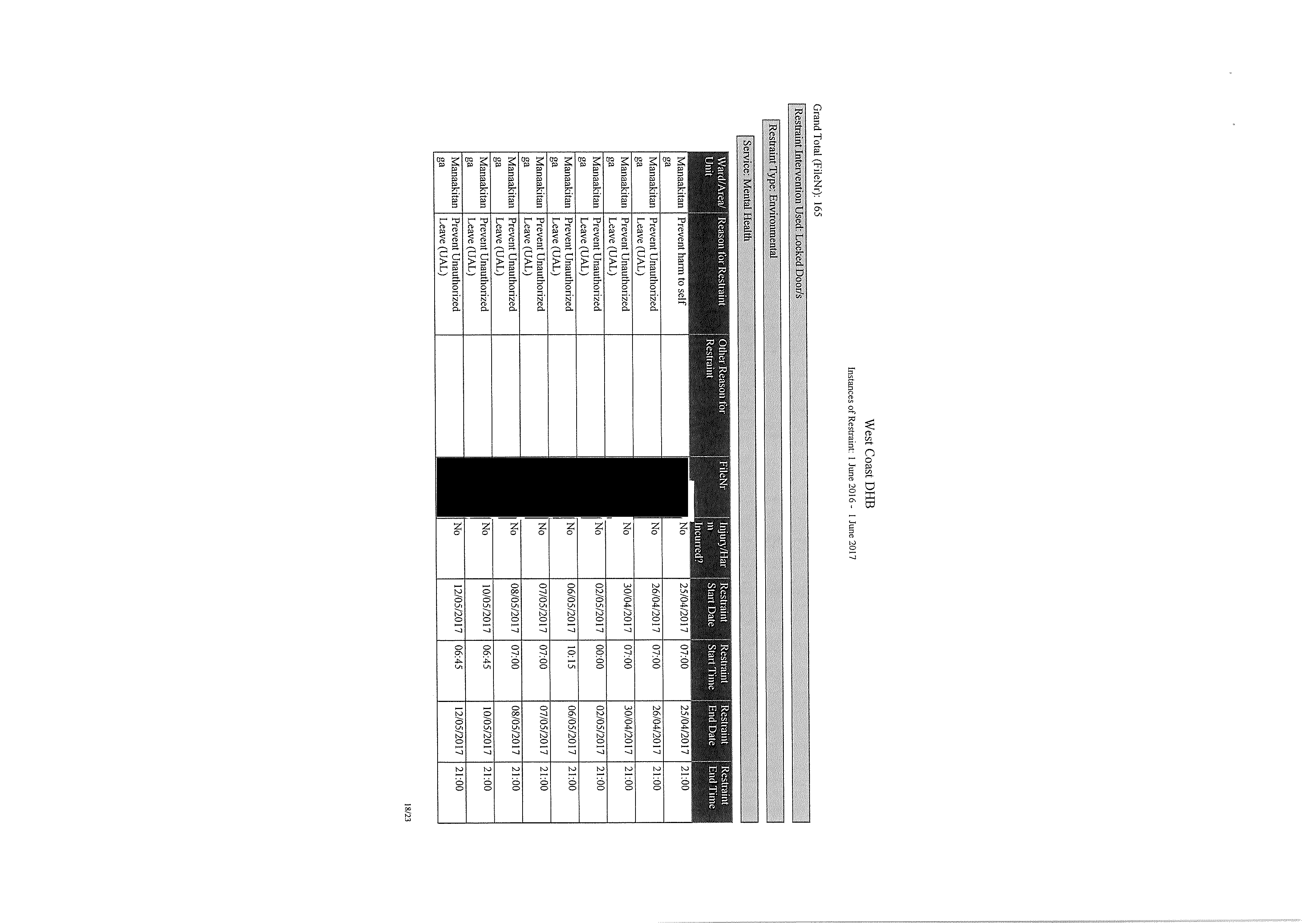
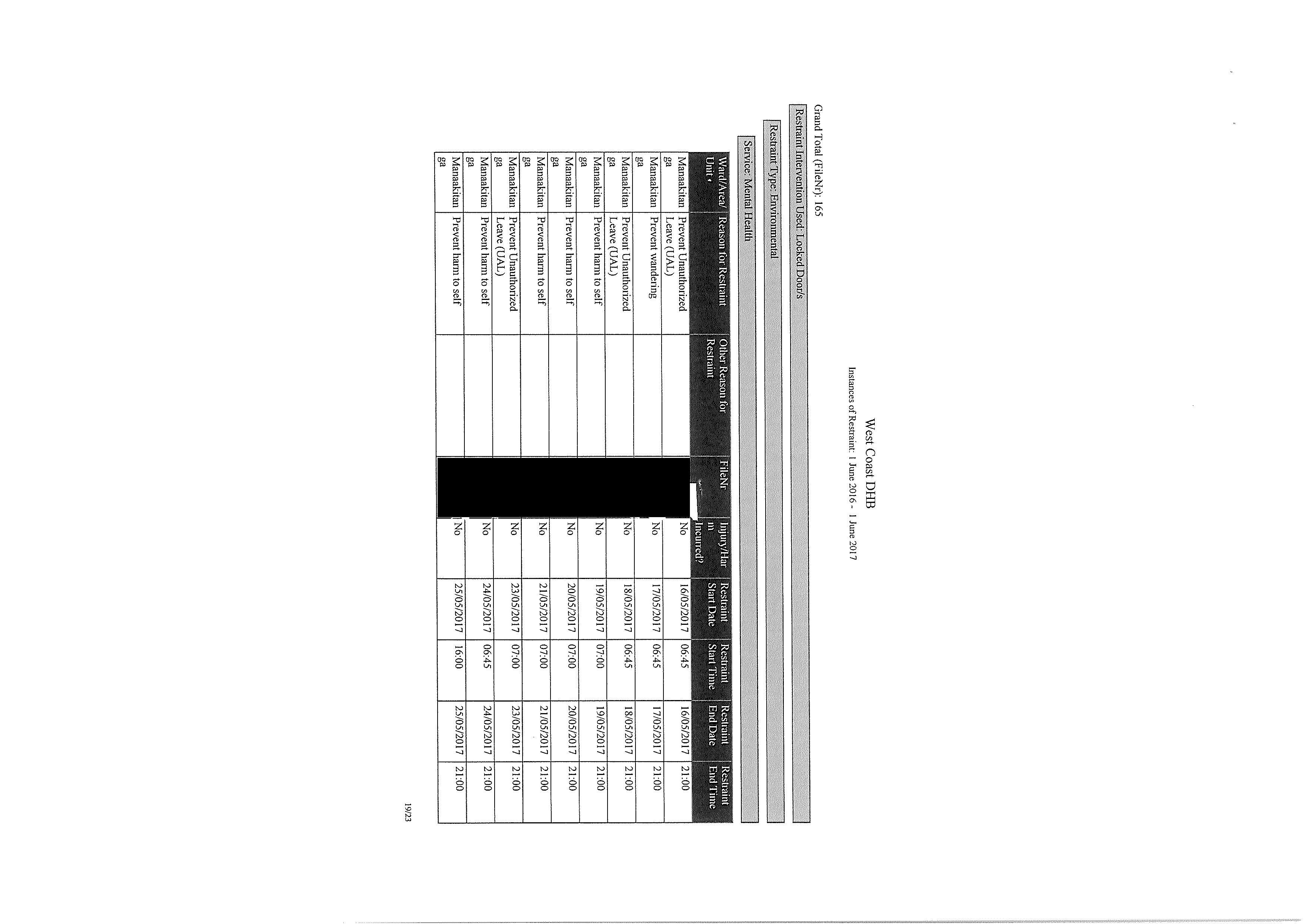
Attached as
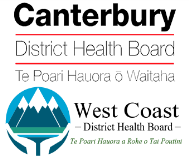
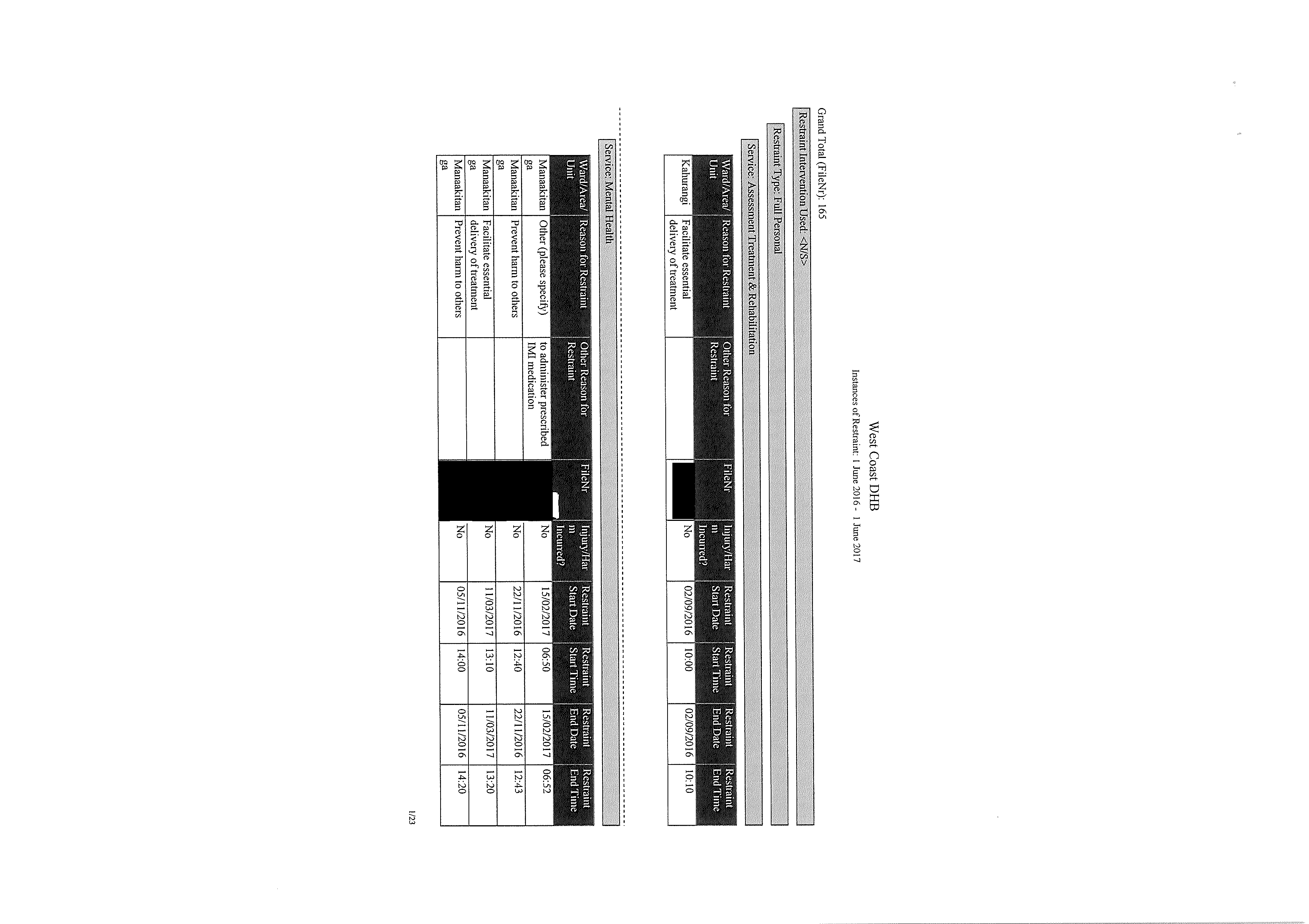
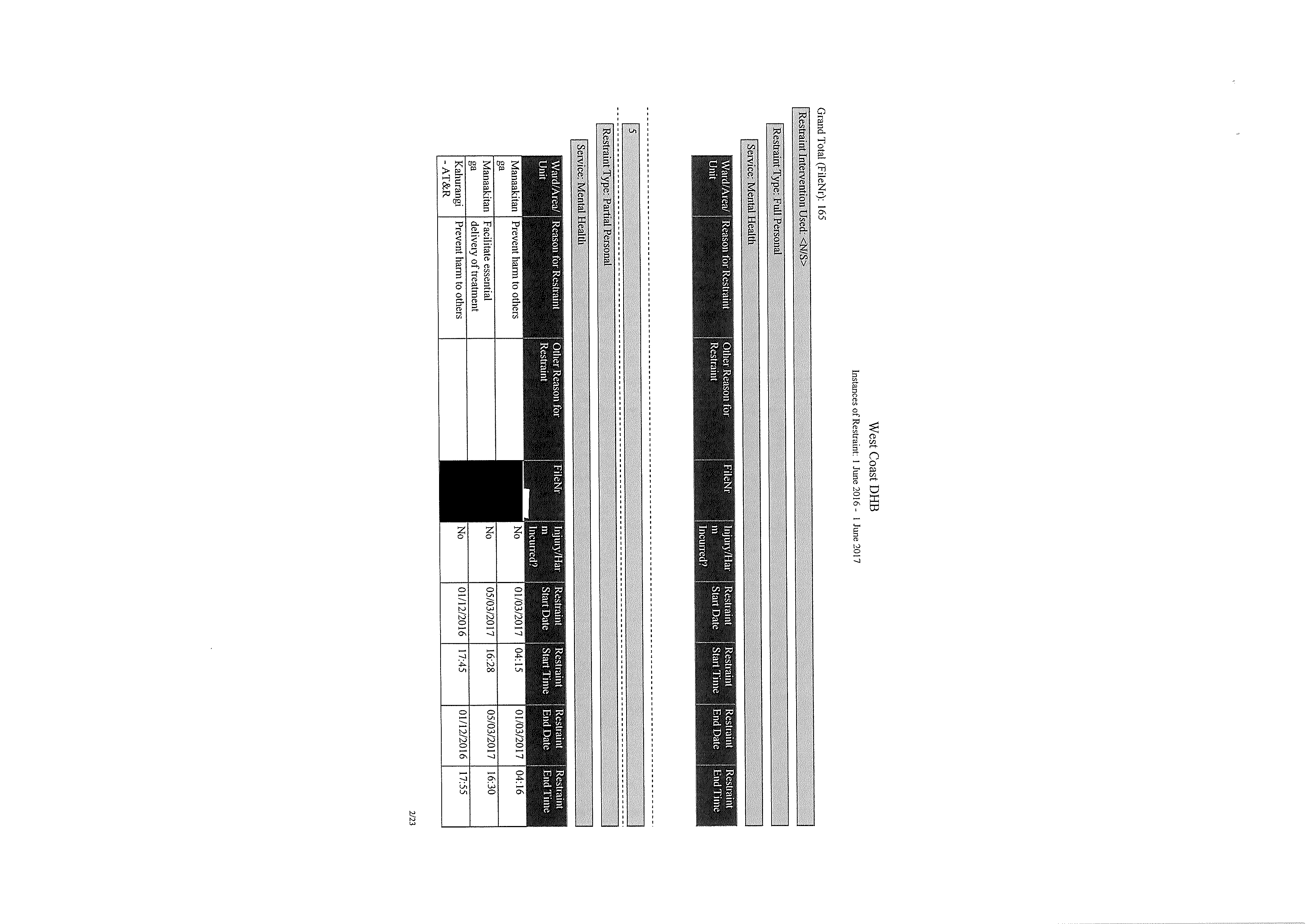
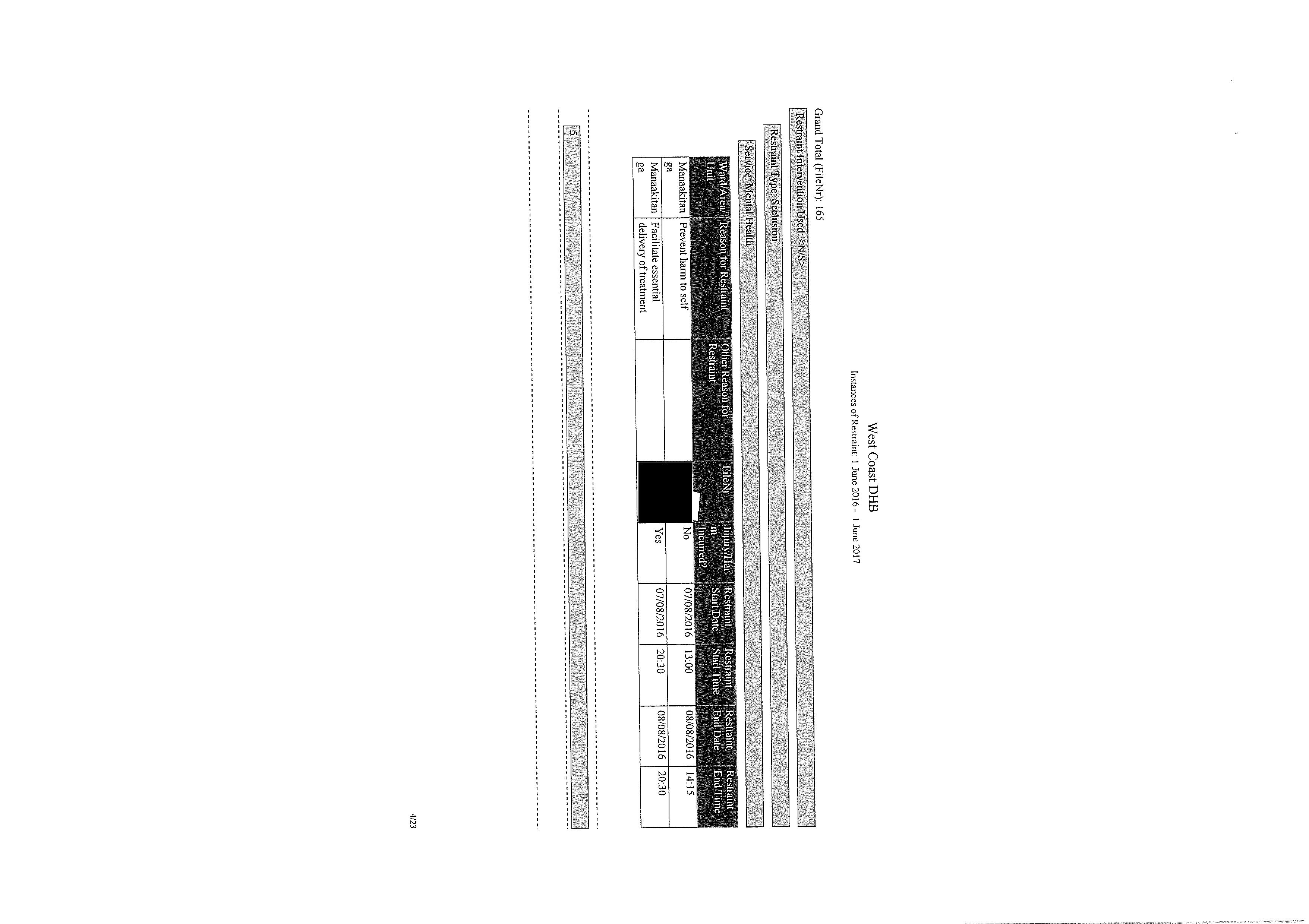
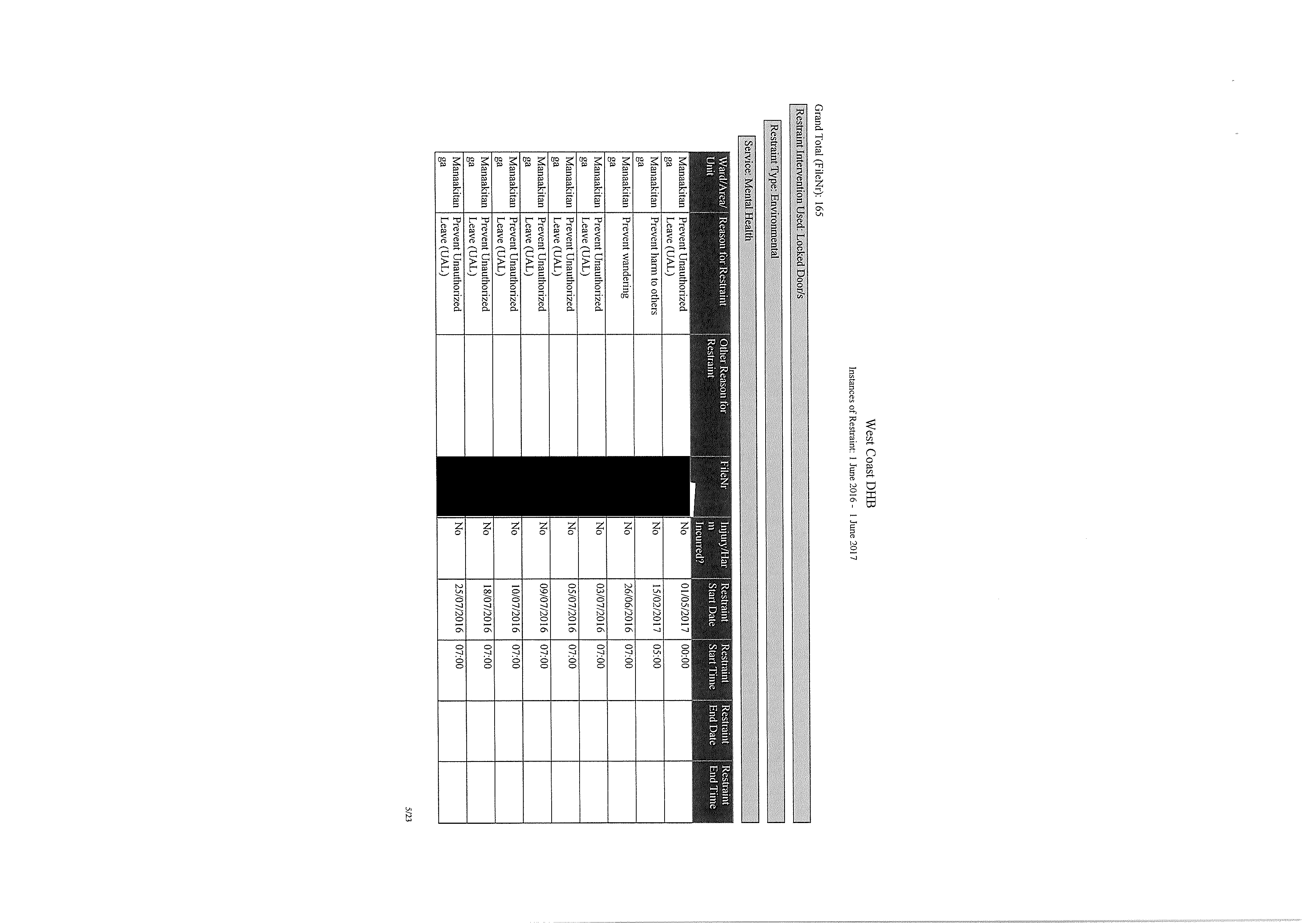
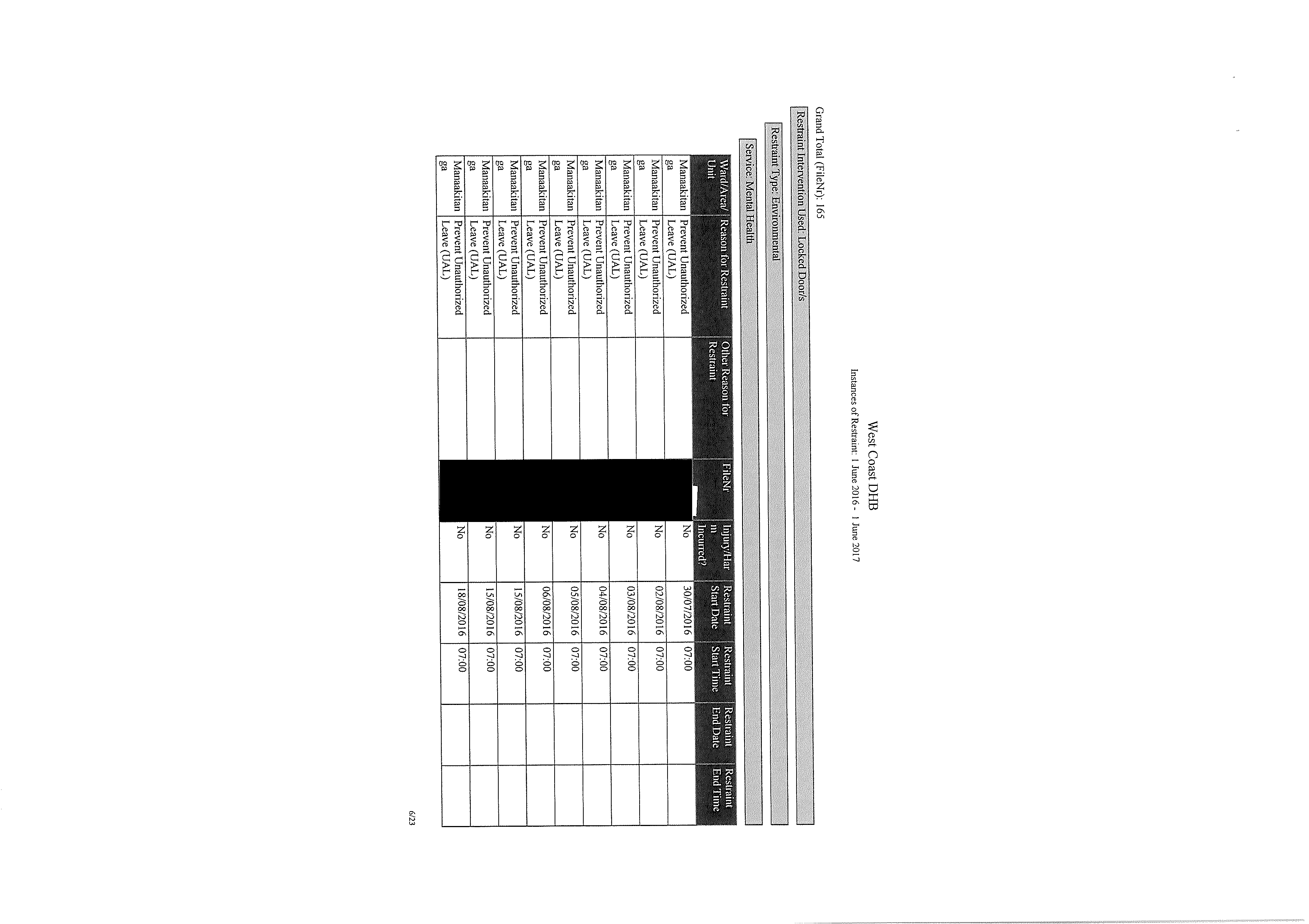
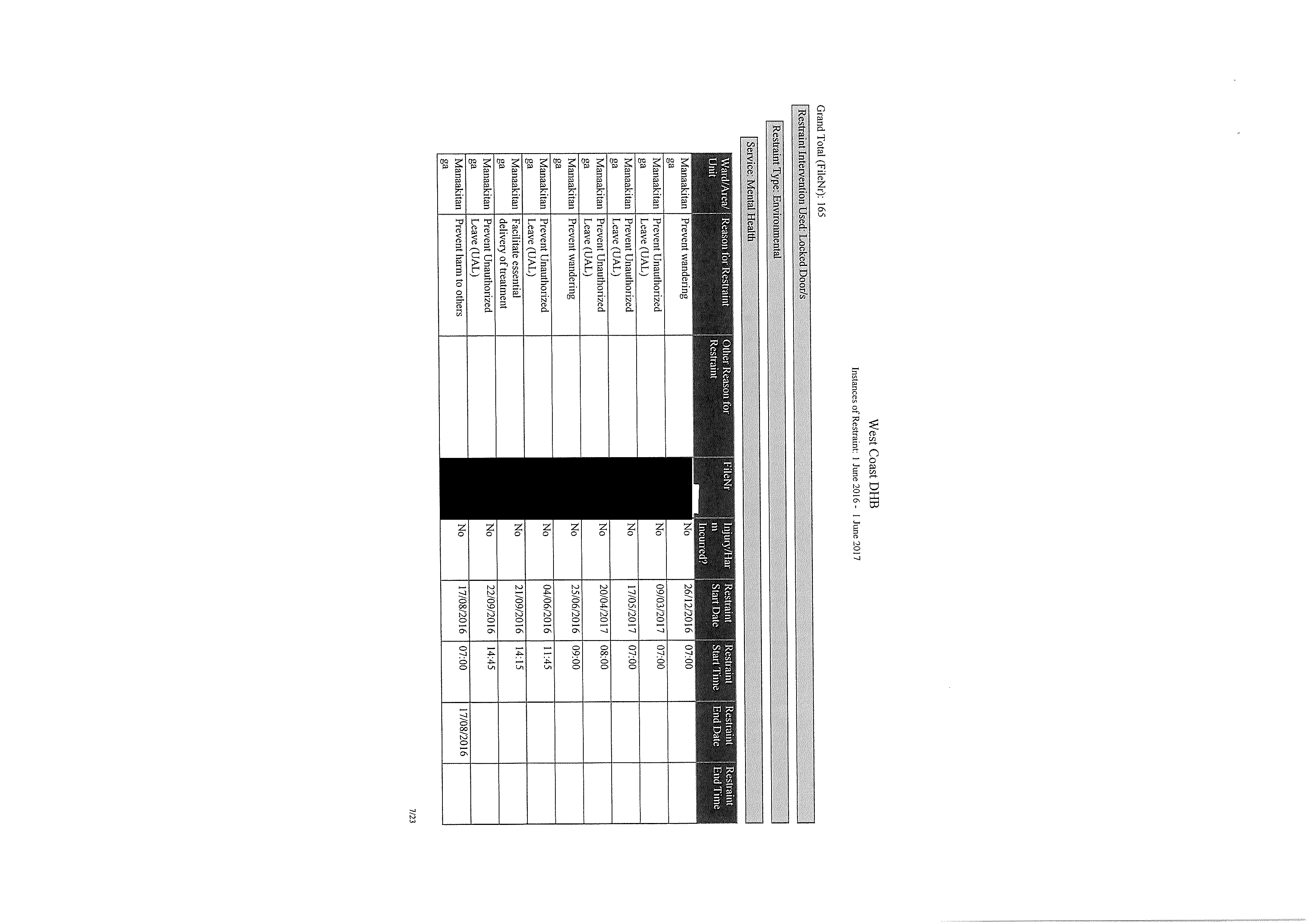
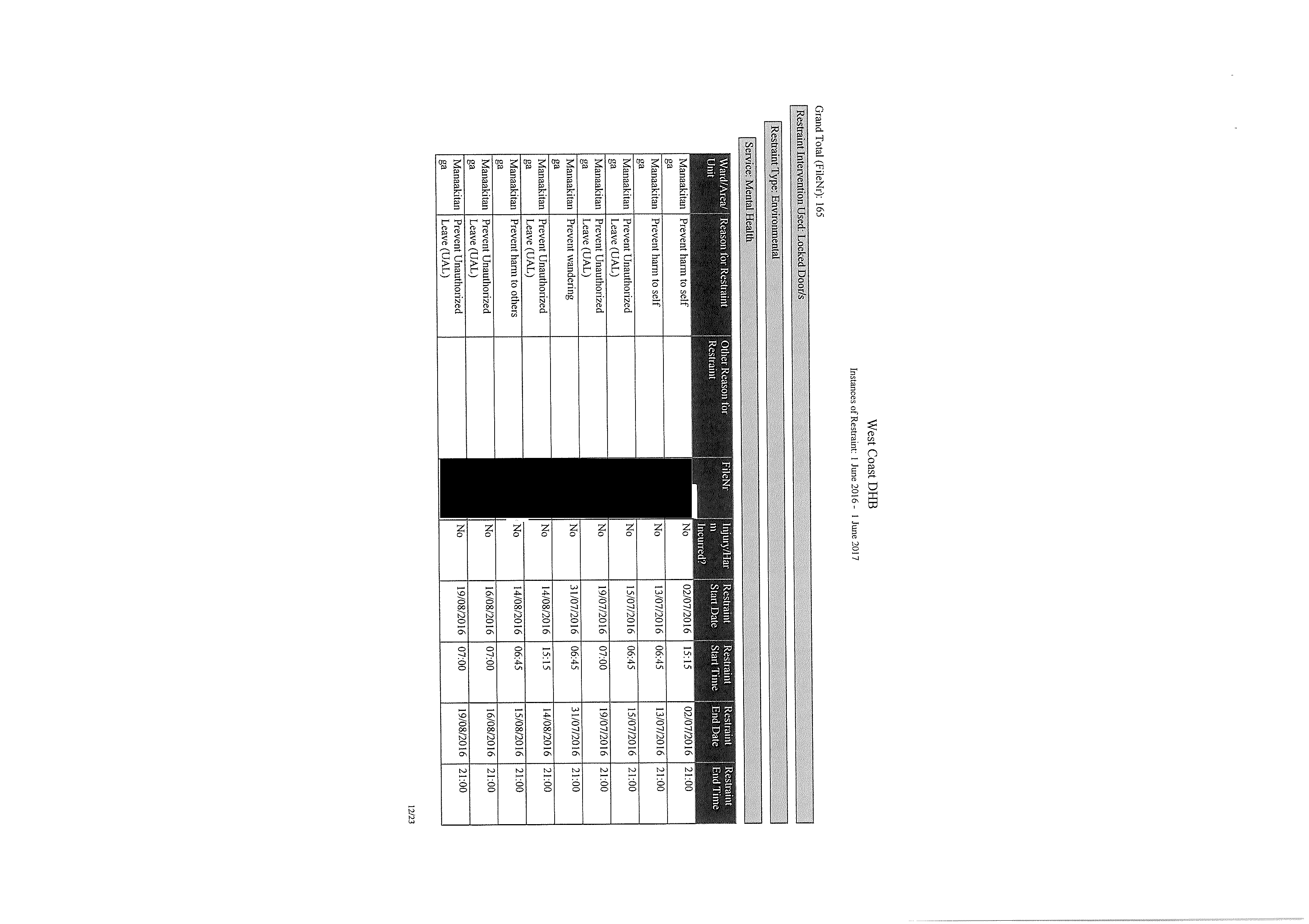
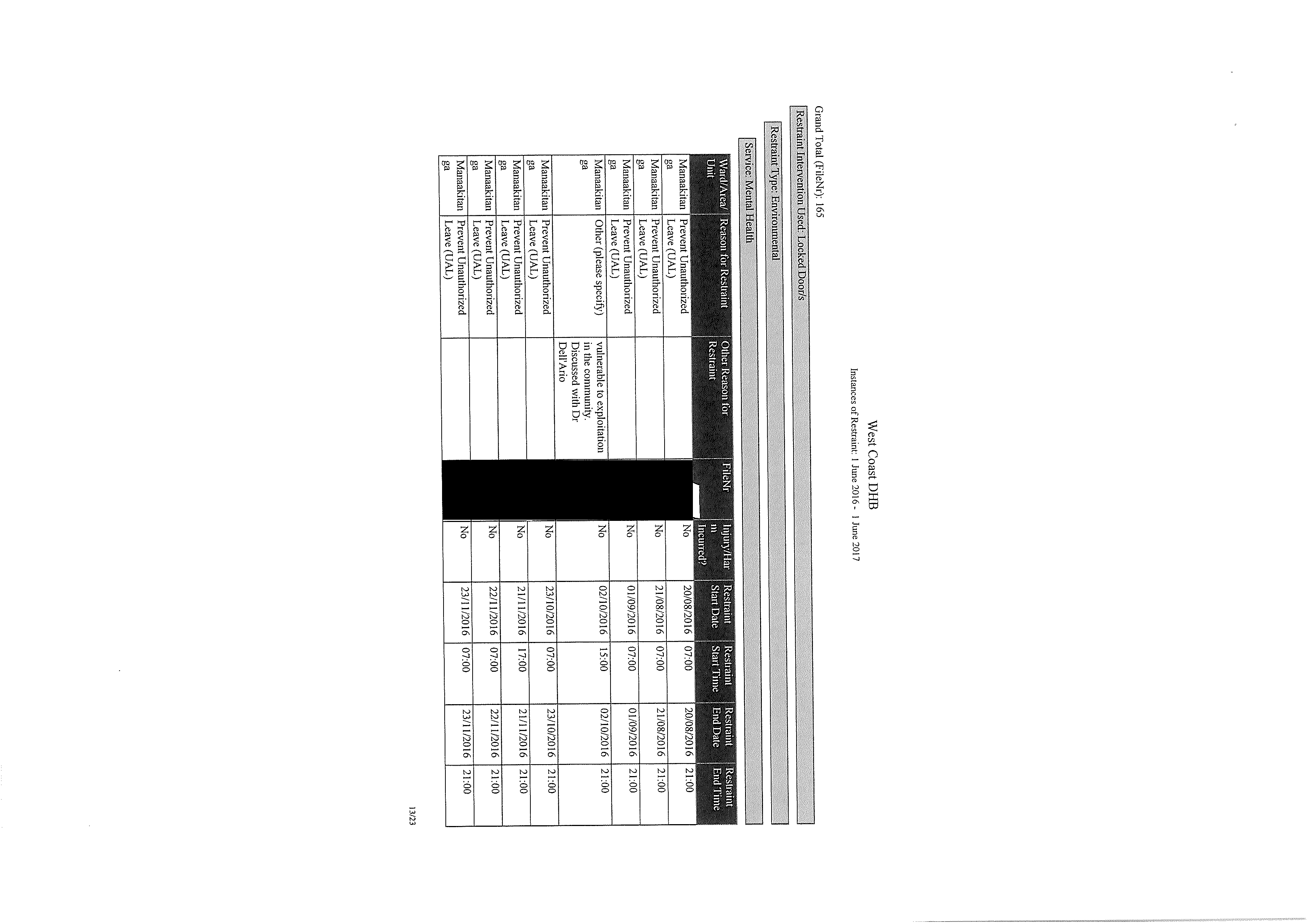
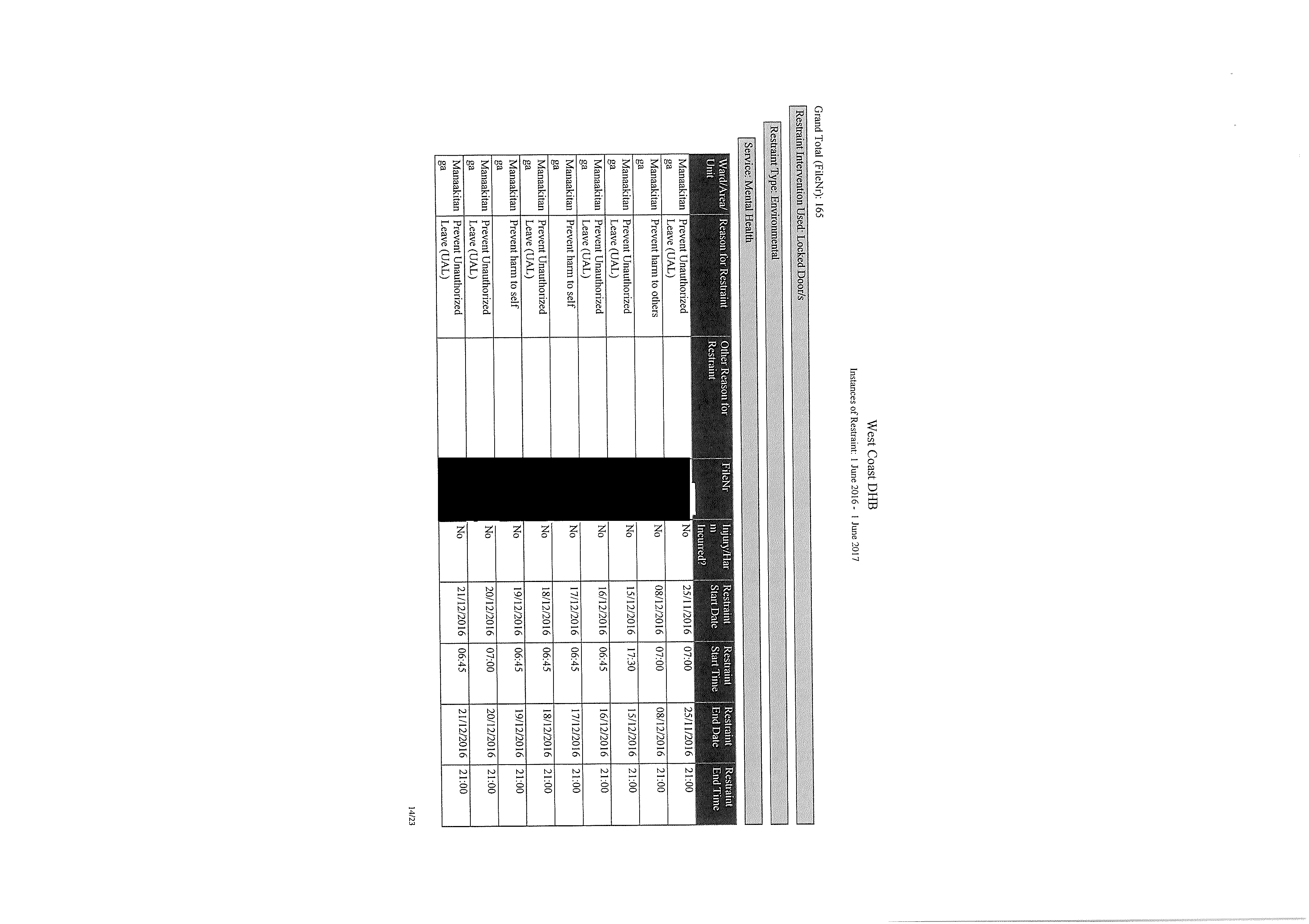
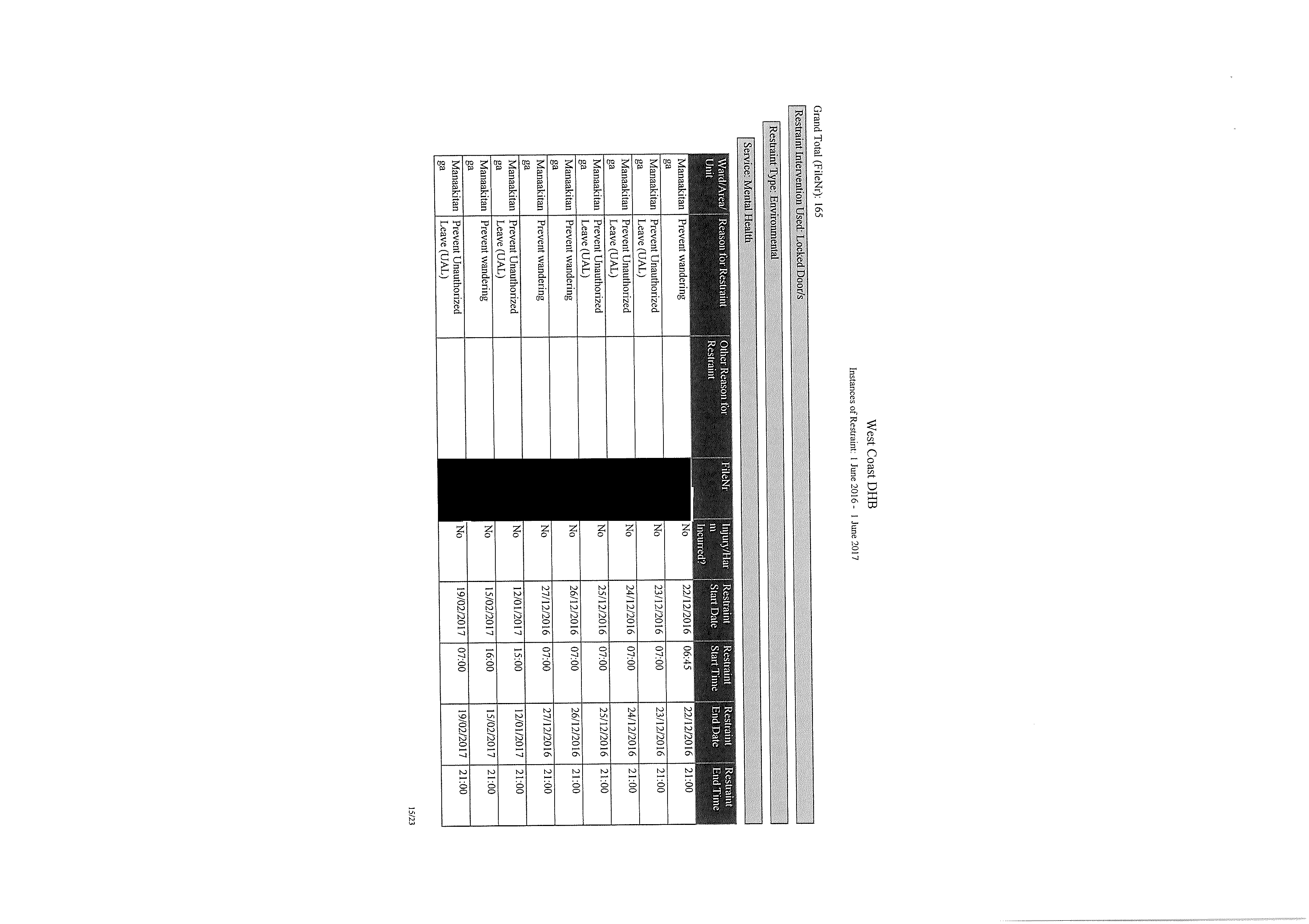
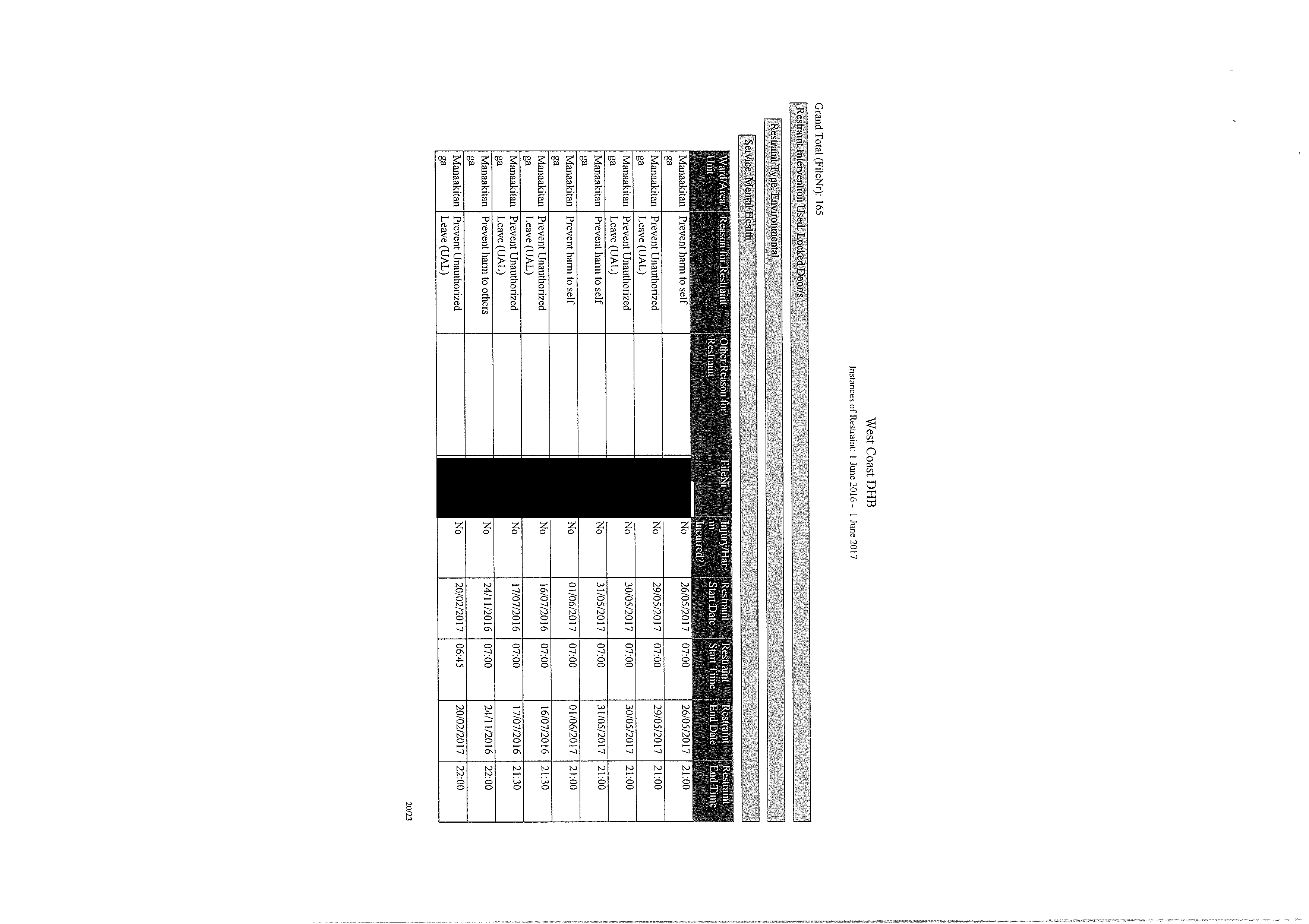
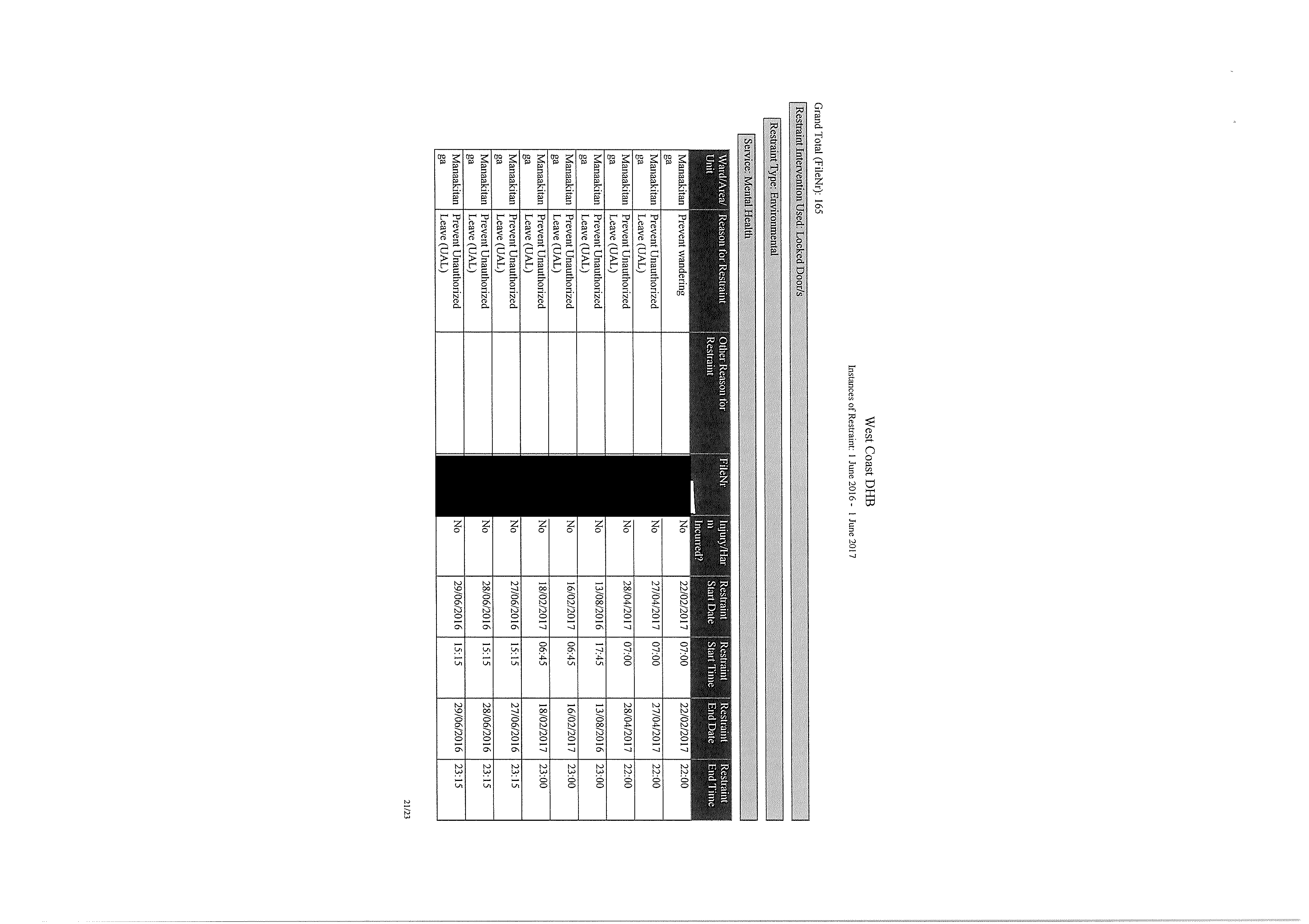
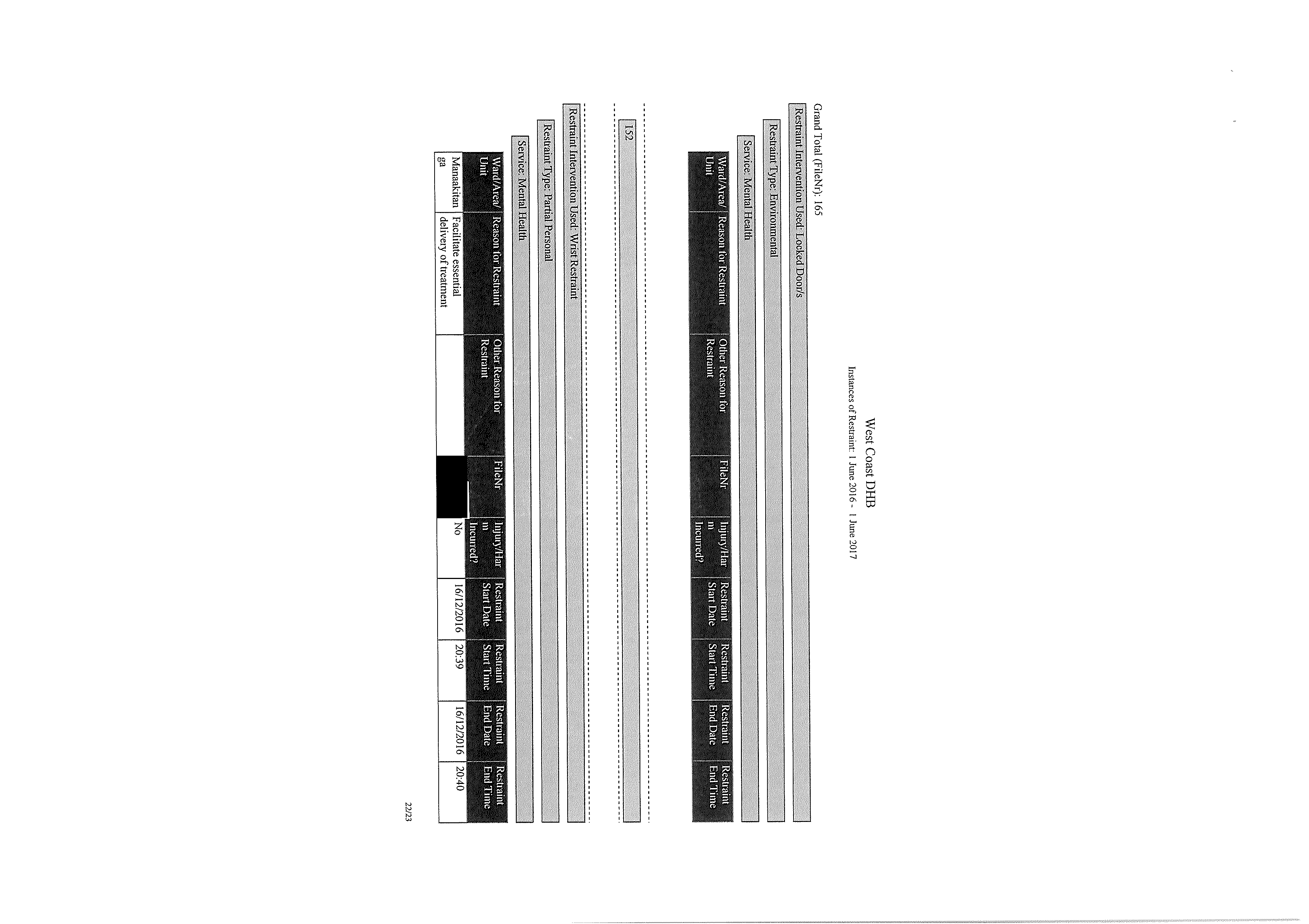
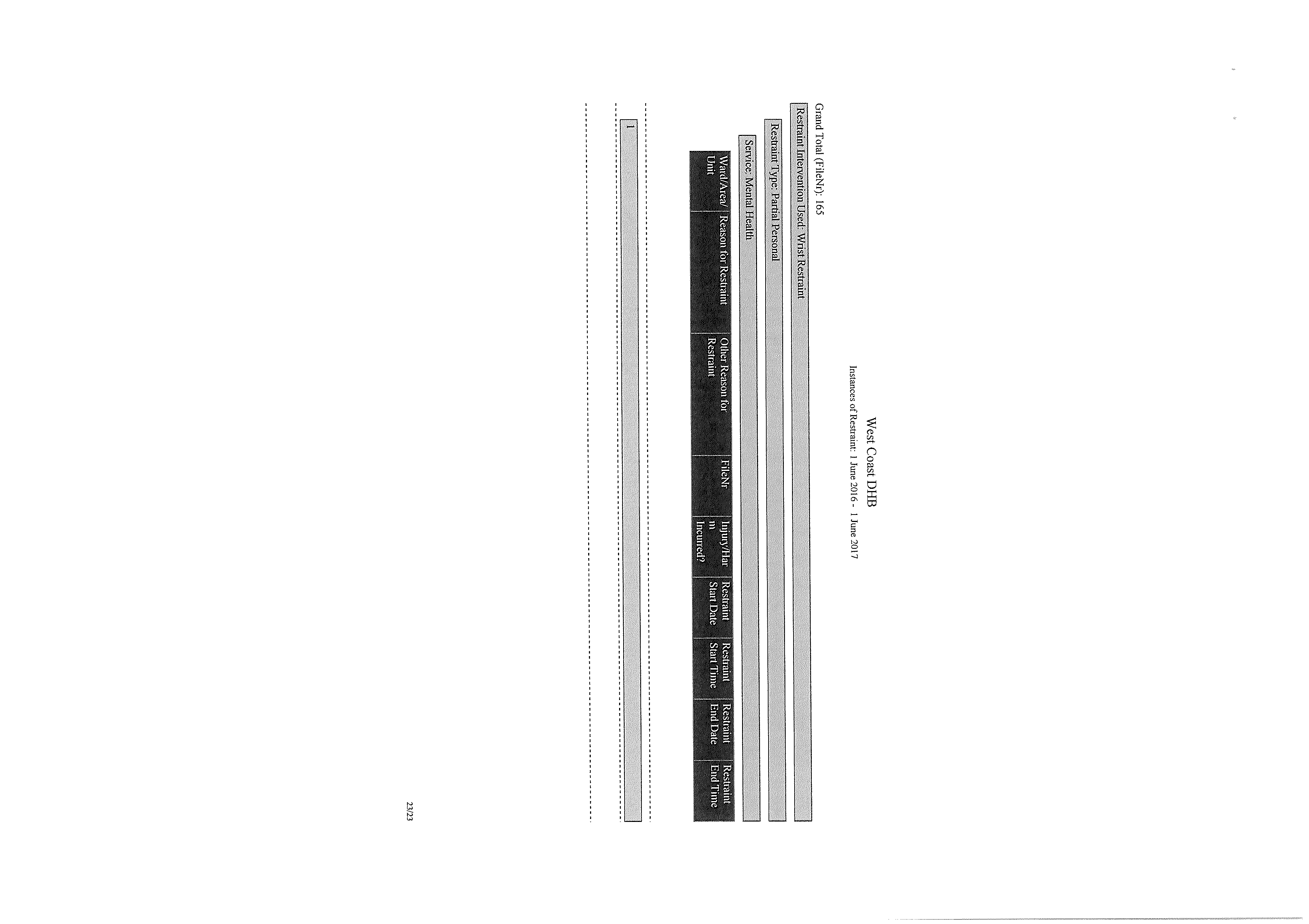
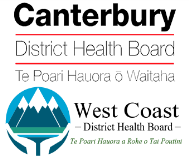
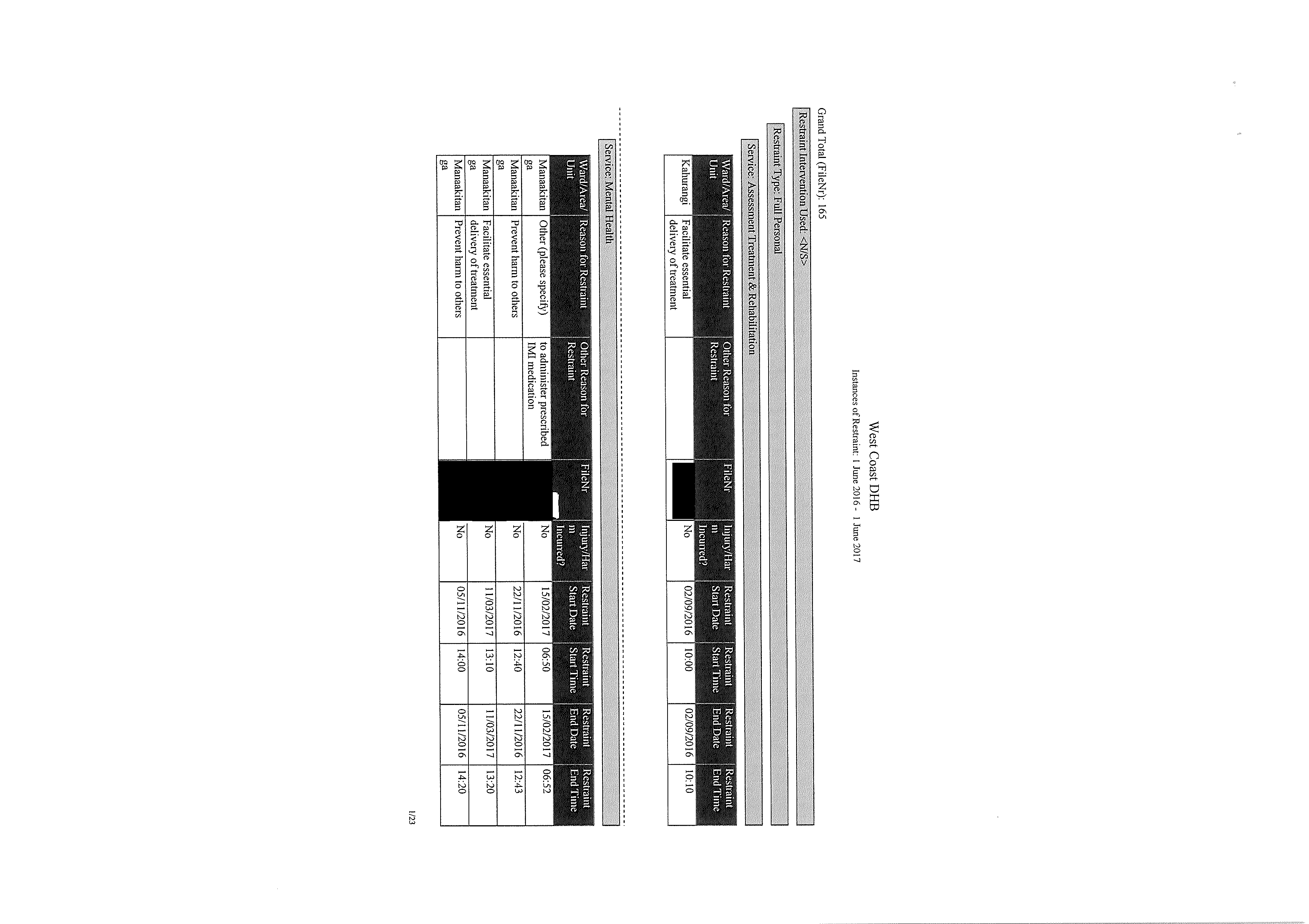
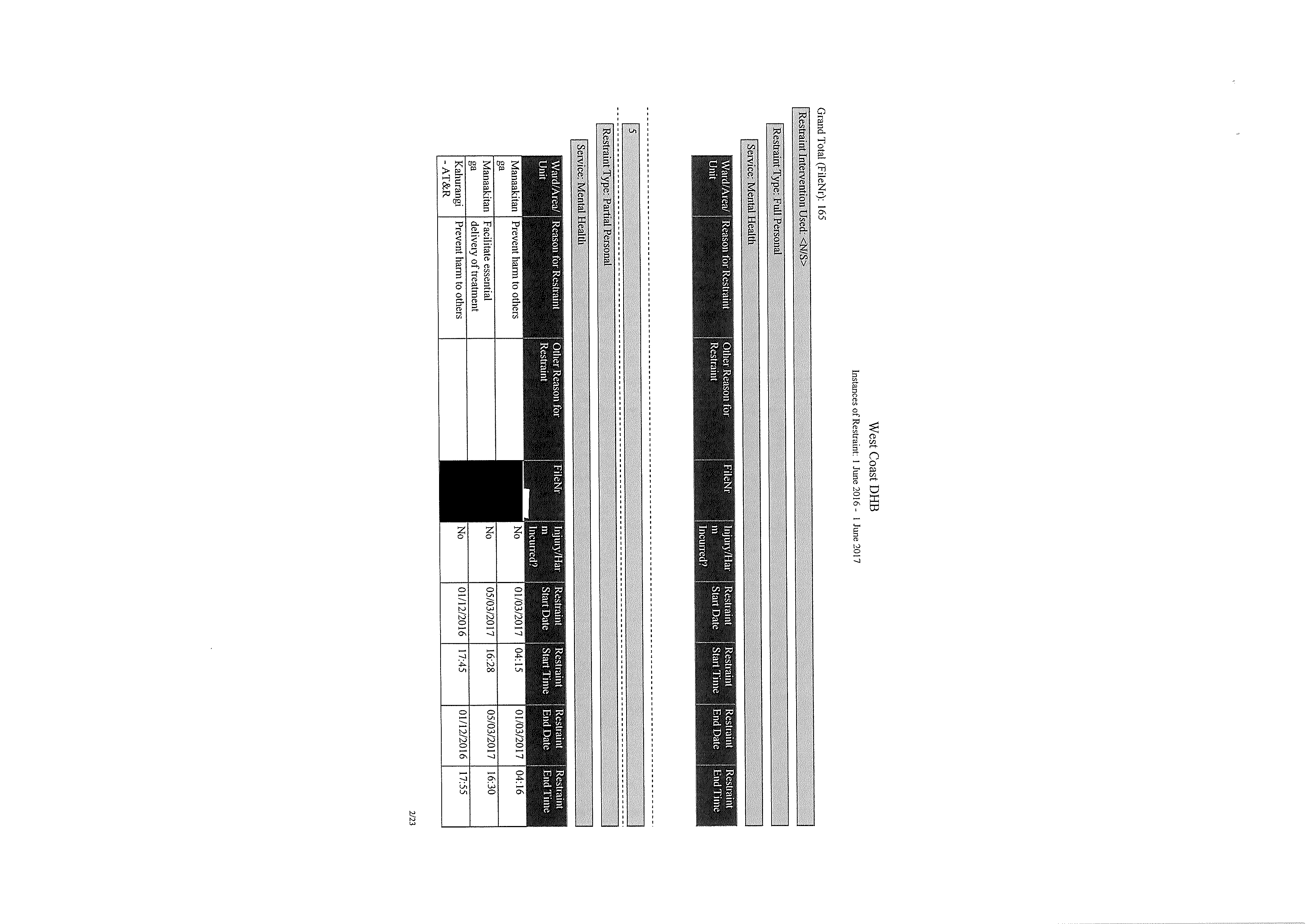
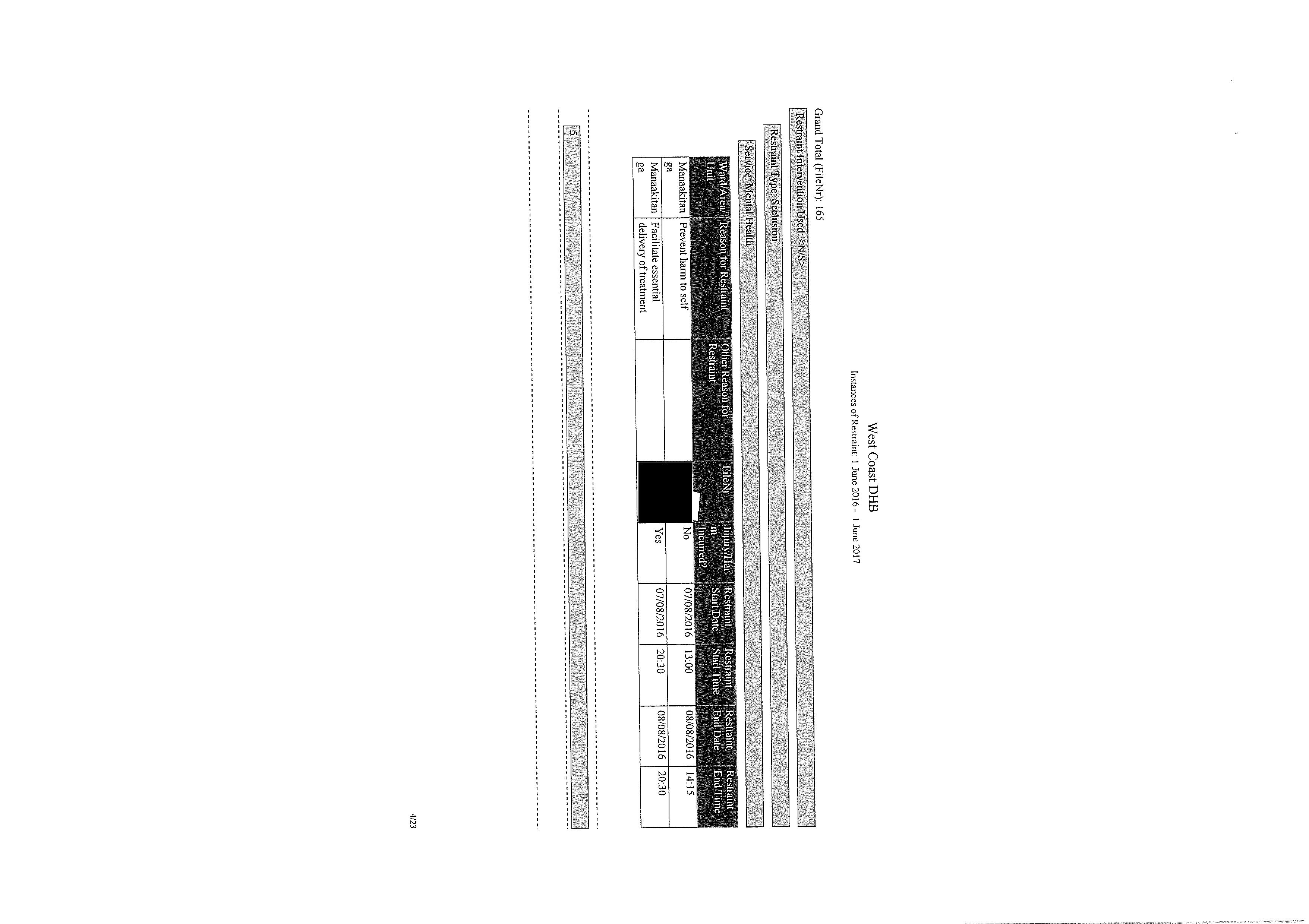
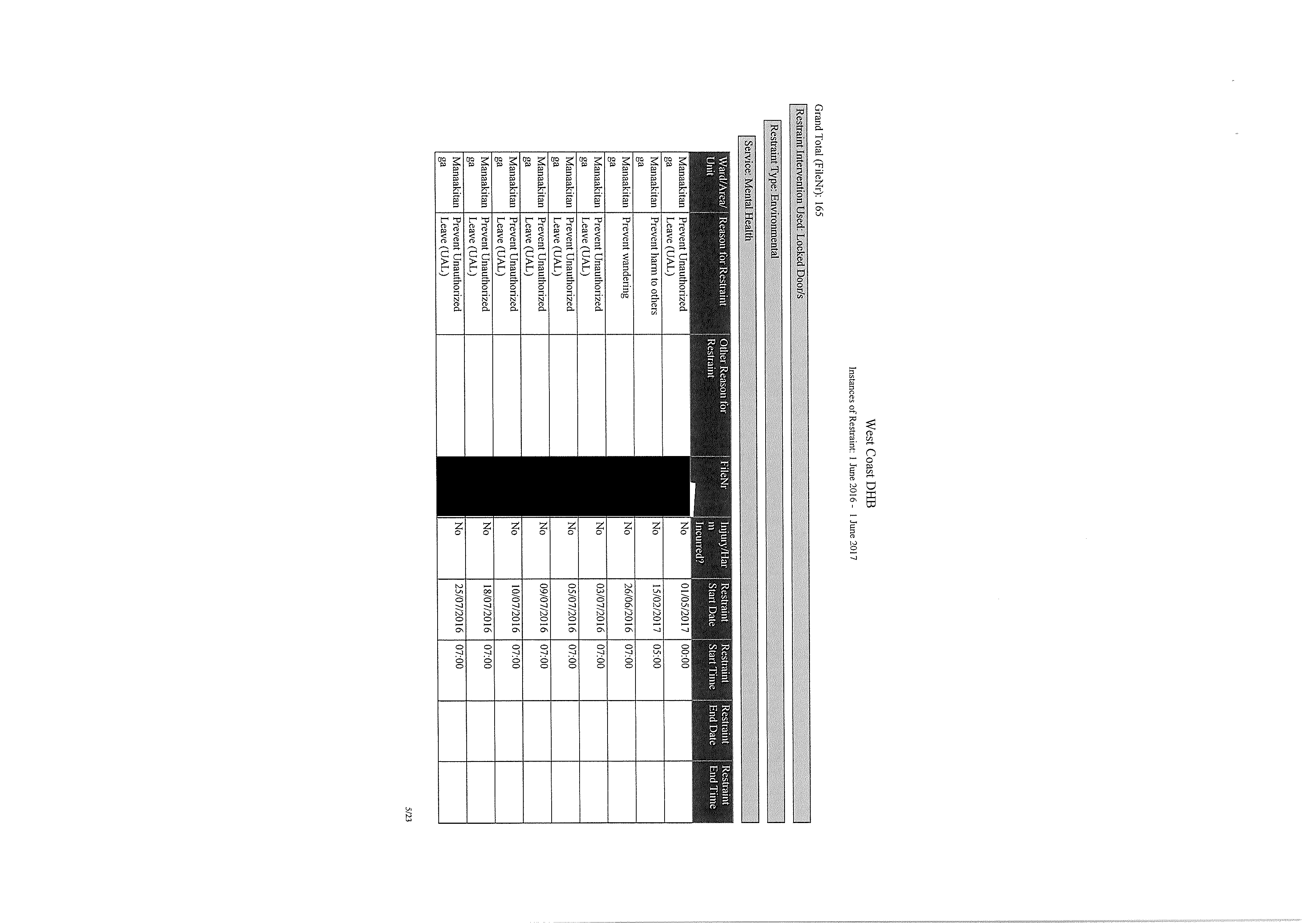
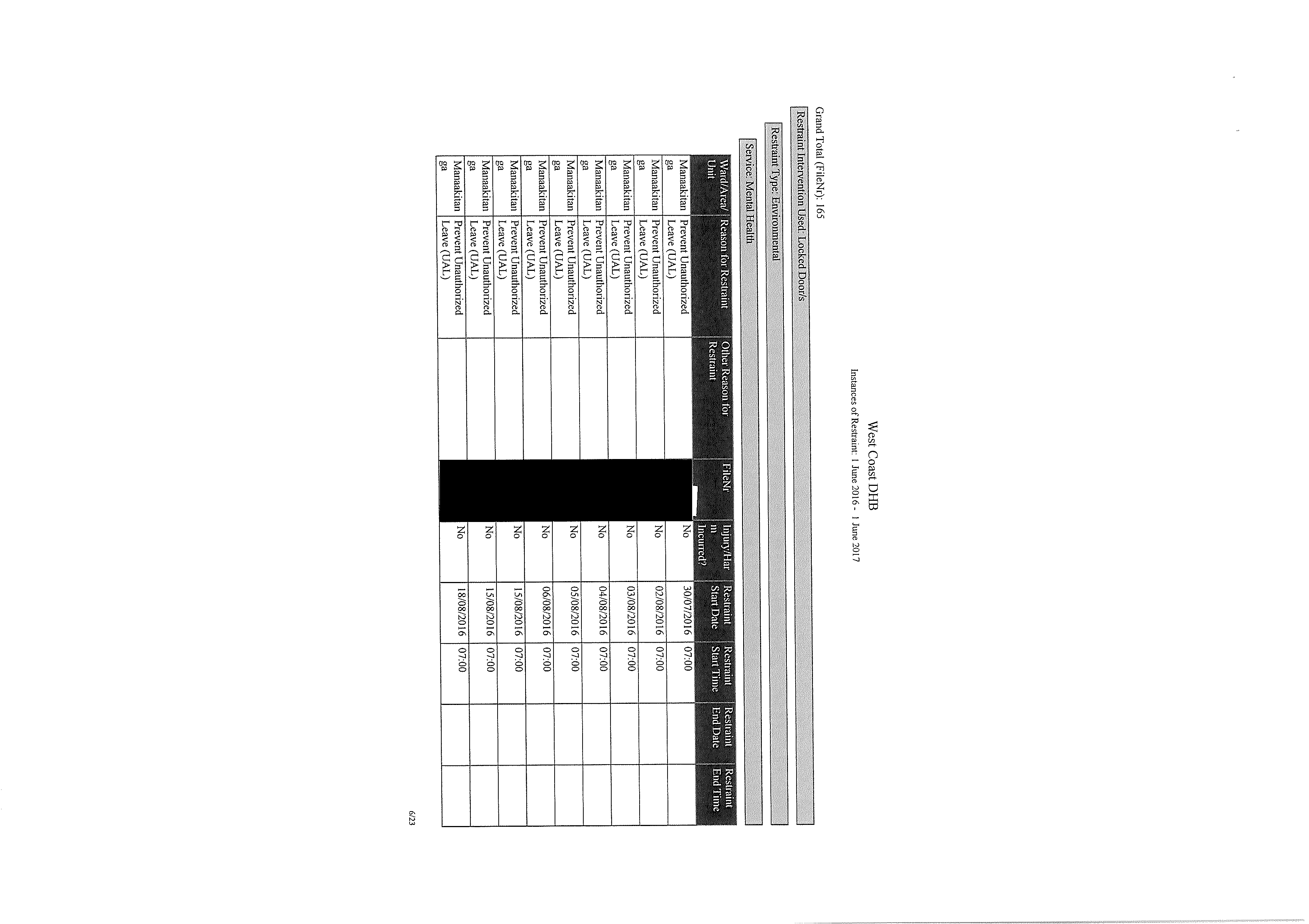
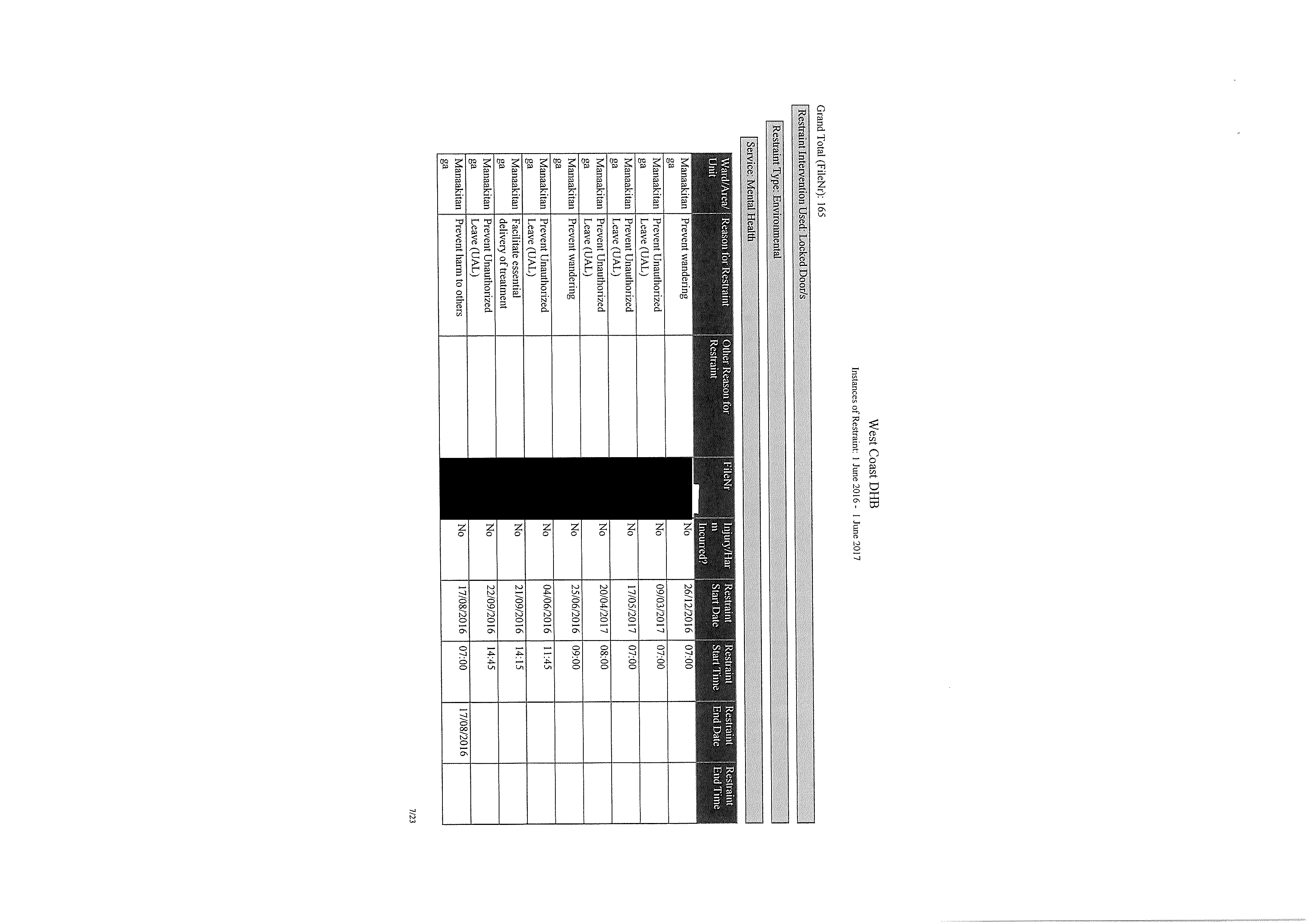
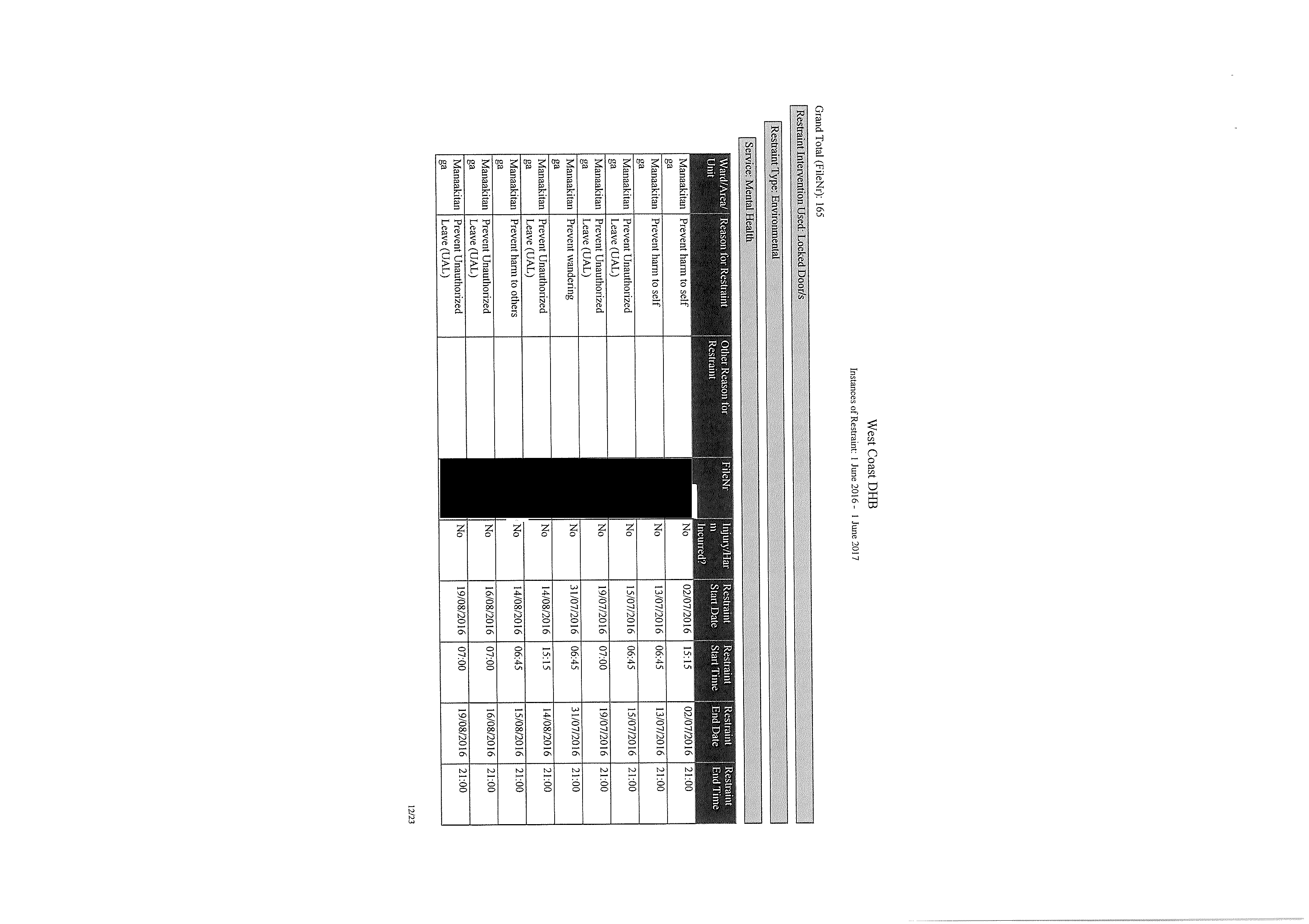
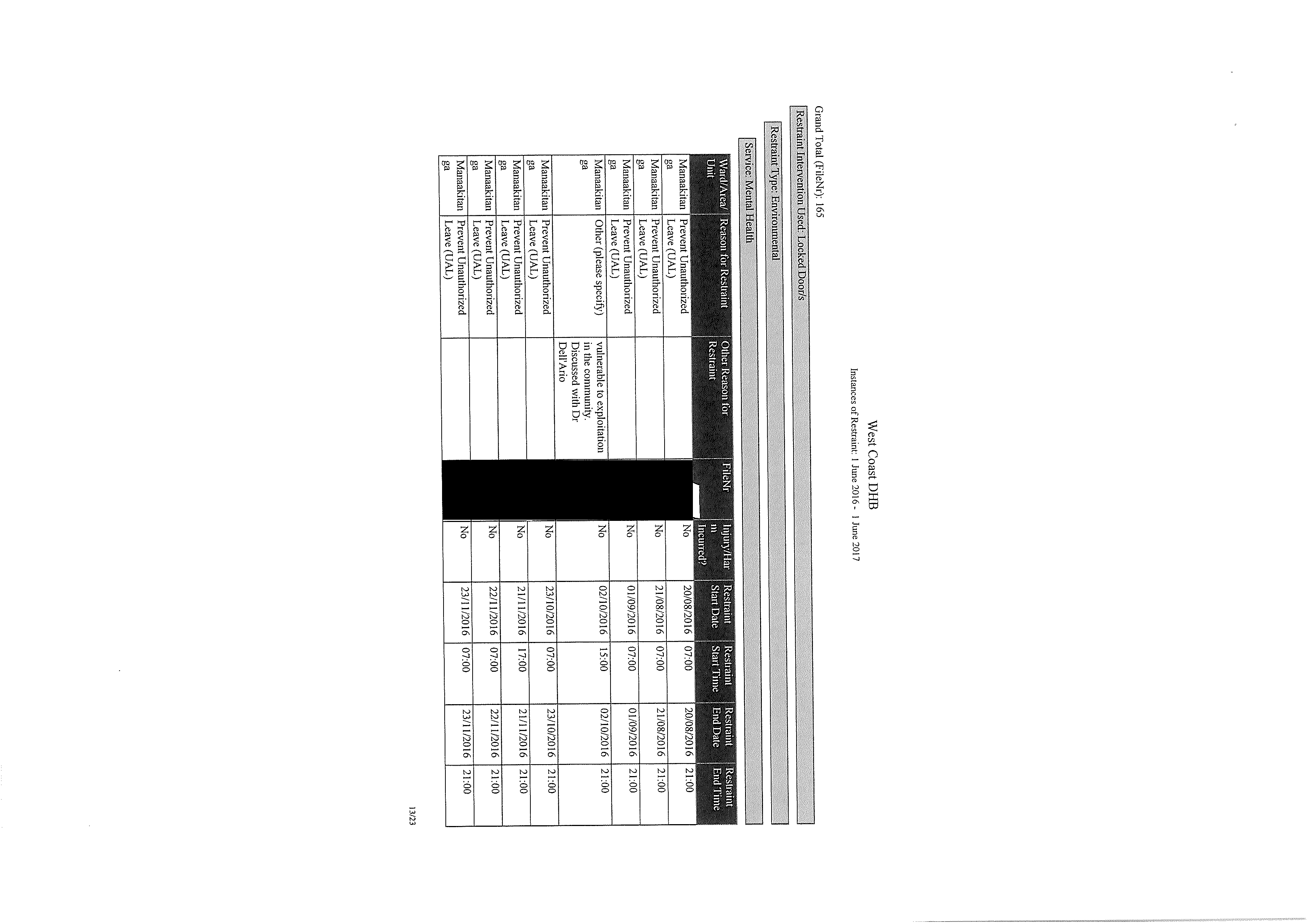
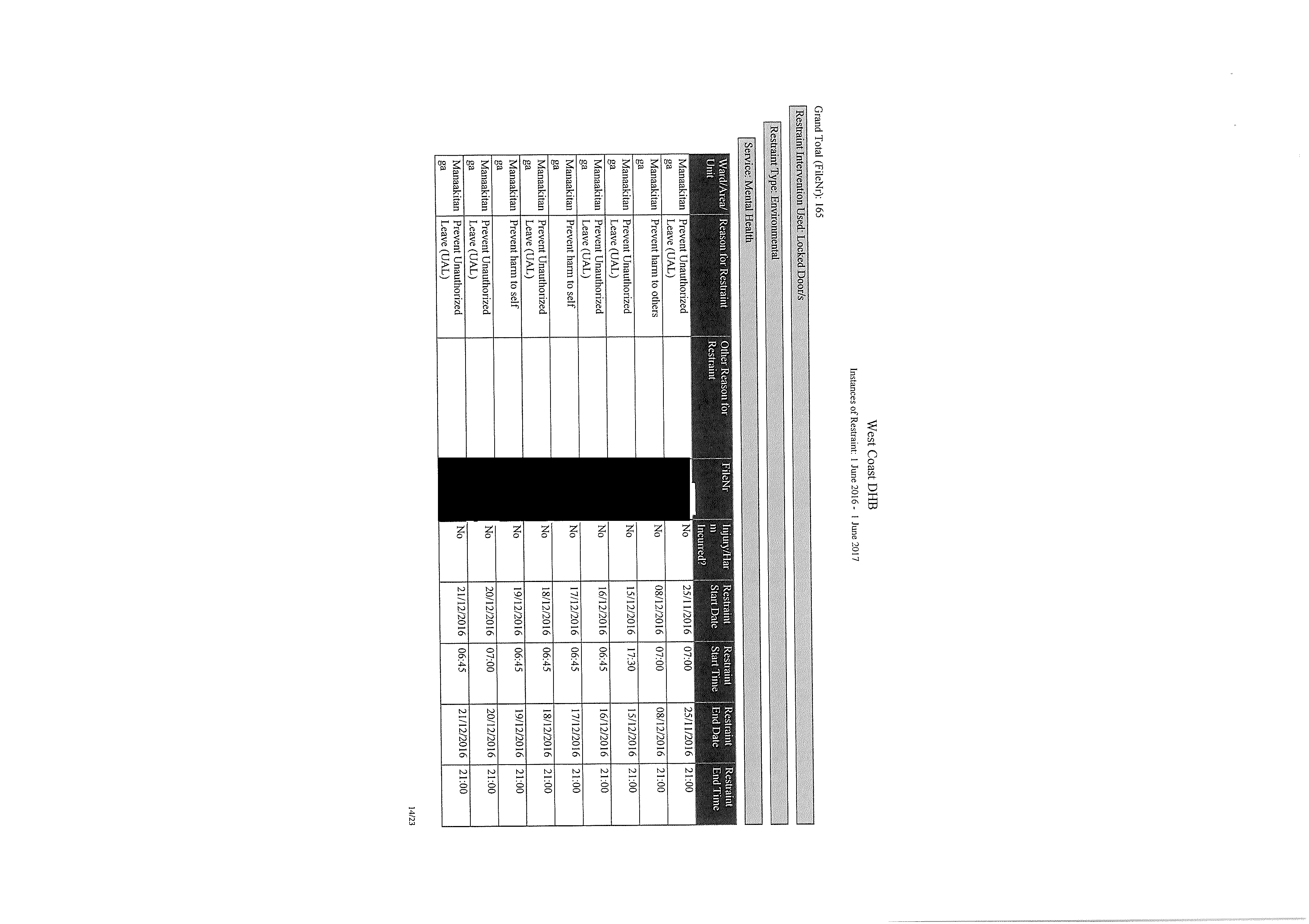
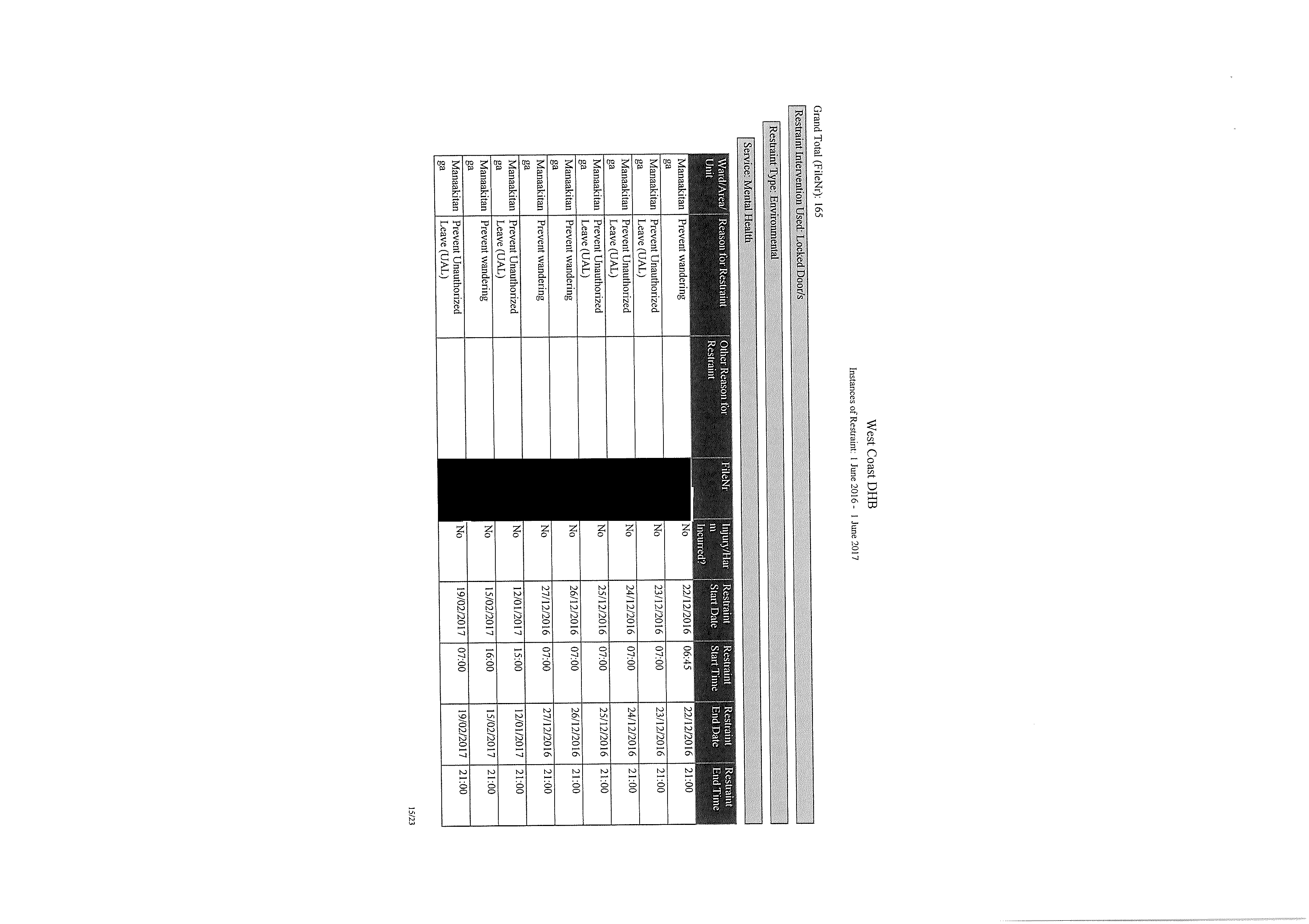
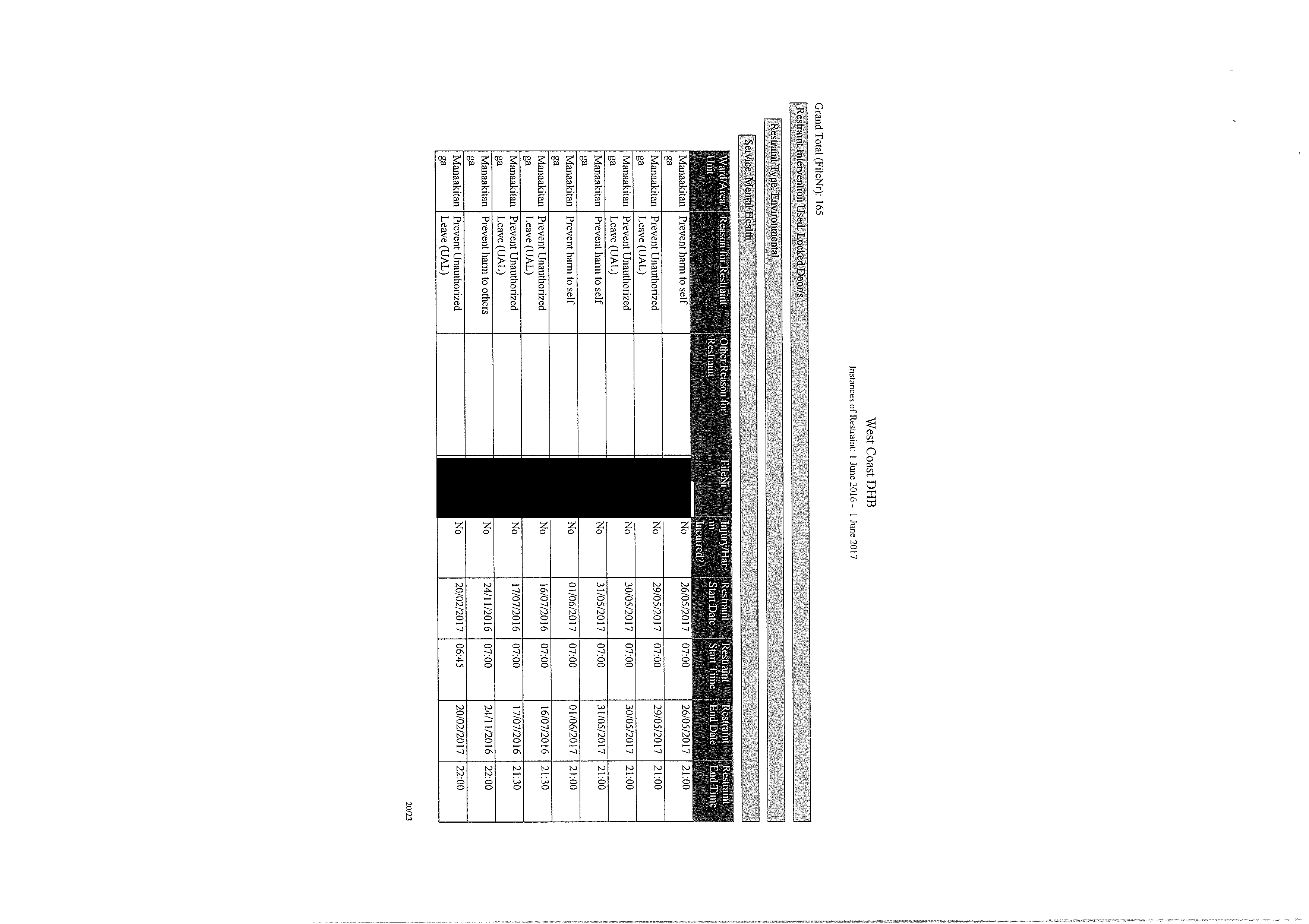
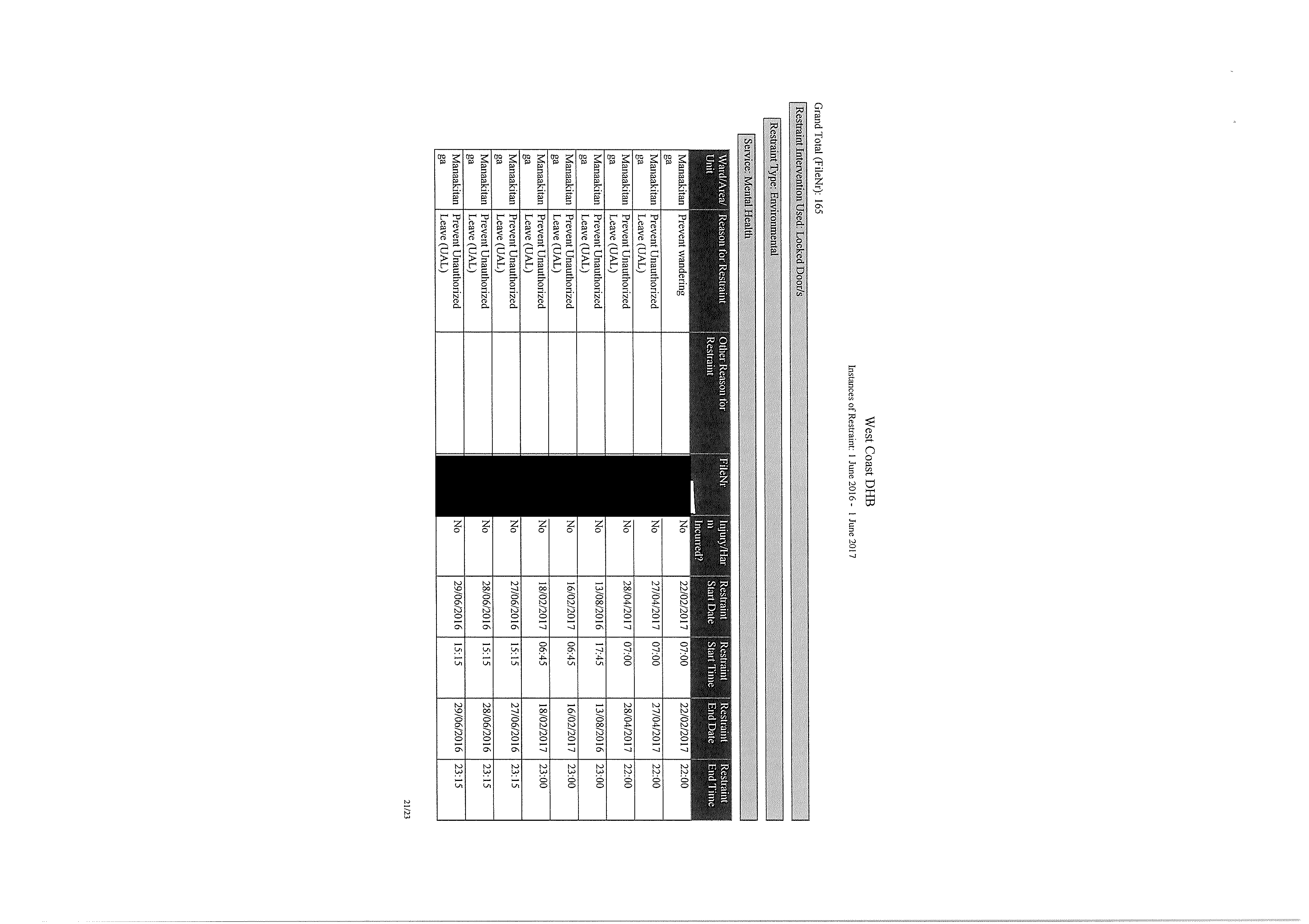
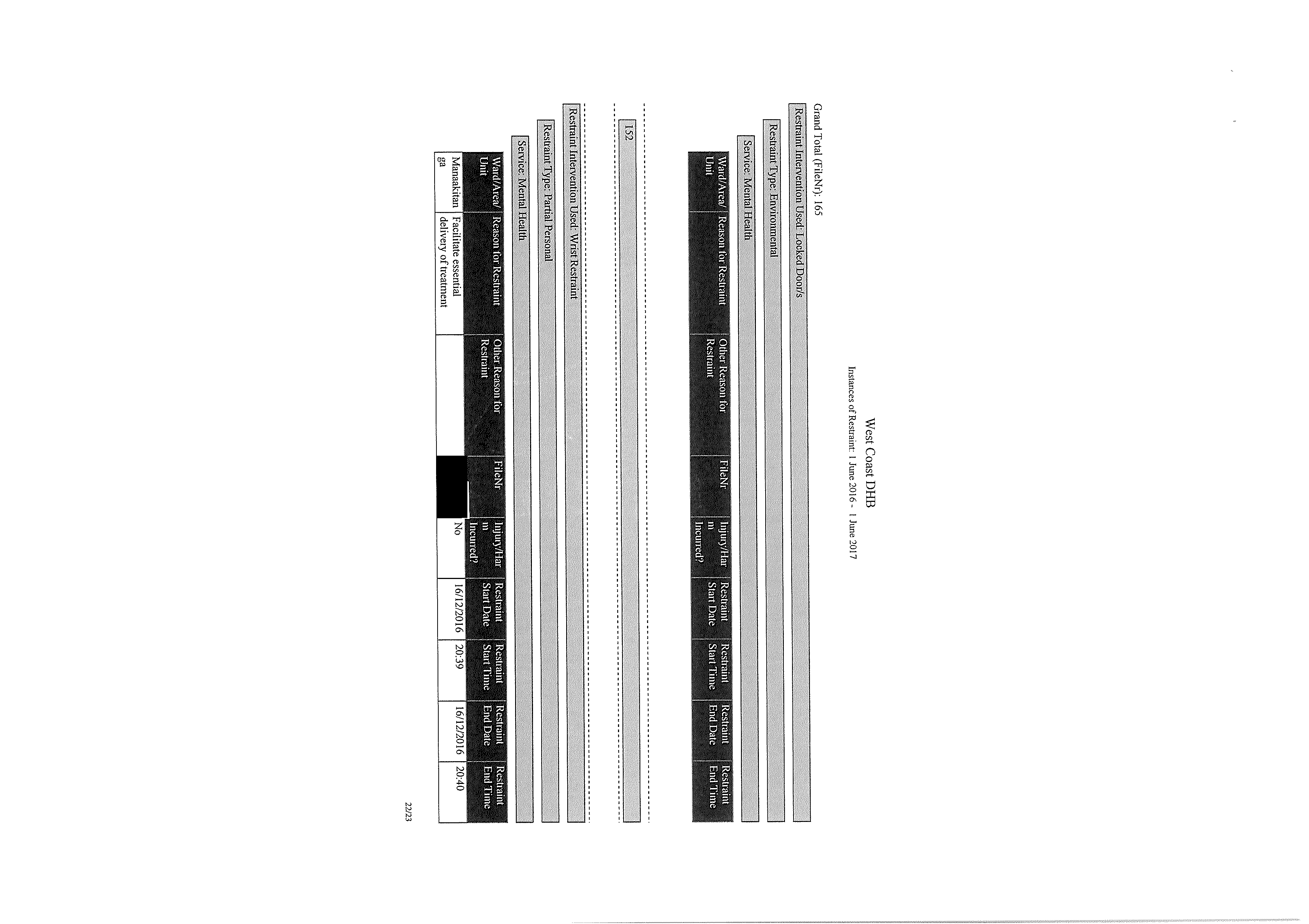
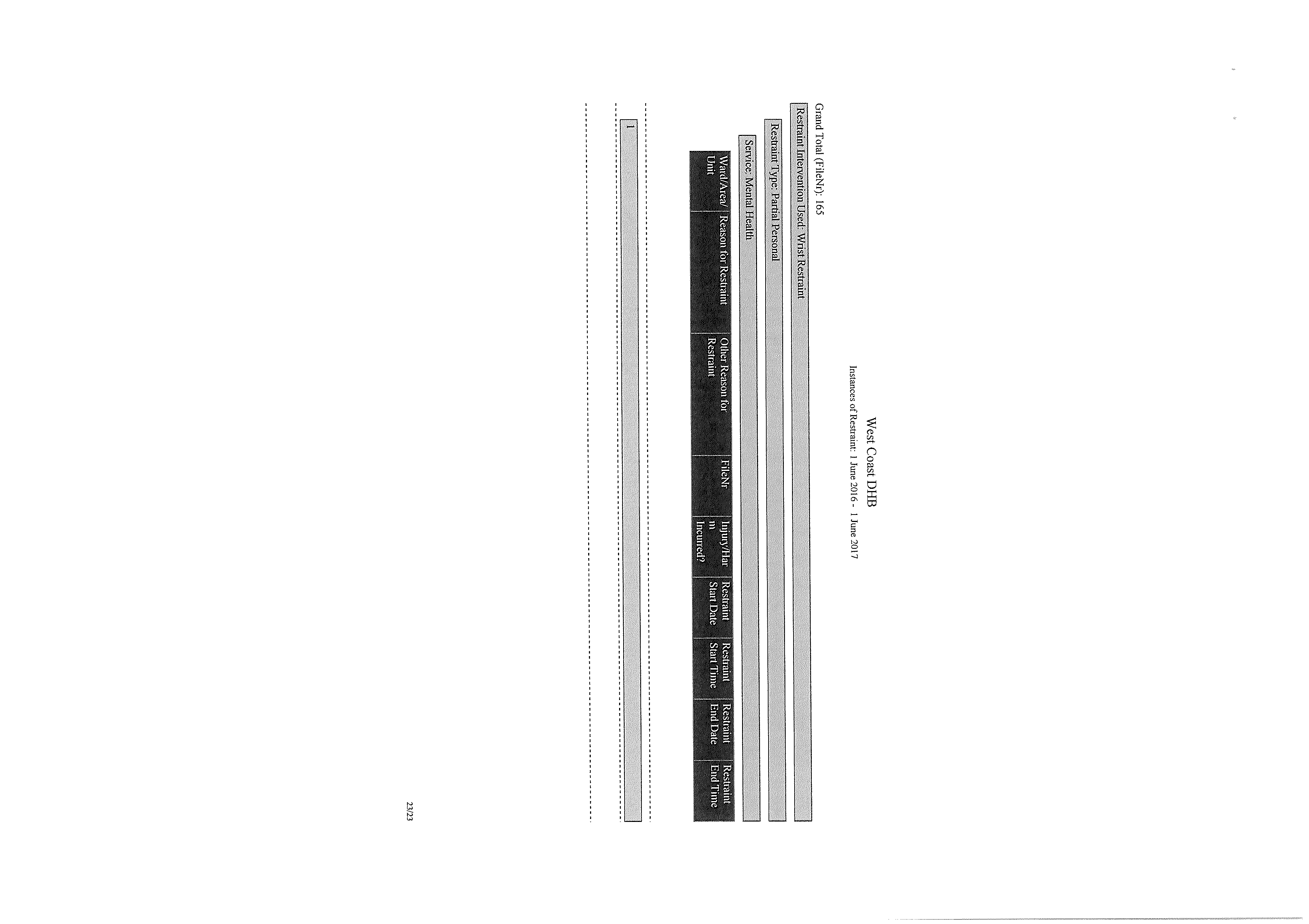
Appendix 2, for your reference, is raw data collated from our electronic Safety 1st Incident
Management System for the period in question. Please note, two onsite inpatient facilities exist in
Greymouth where logged restraint took place.
Manaakitanga Adult General Acute Psychiatric Inpatient Unit
Kahurangi Aged Residential Care Assessment Treatment rehabilitation / Dementia Service unit
P.O. Box 387, Greymouth 7840
We have redacted information in Appendix 2 under section 9(2)(a) of the Official Information Act i.e.
“to protect the privacy of natural persons, including those deceased”.
If you disagree with our decision to withhold information you may, under section 28(3) of the Official
Information Act, seek an investigation and review of our decision from the Ombudsman.
I trust that the information enclose answers your questions satisfactorily.
Yours sincerely
Carolyn Gullery
General Manager
Planning, Funding and Decision Support.
link to page 3 link to page 3 link to page 4 link to page 4 link to page 4 link to page 4 link to page 4 link to page 4 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 5 link to page 7 link to page 7 link to page 7 link to page 7 link to page 8 link to page 8 link to page 8 link to page 8 link to page 9 link to page 9 link to page 9 link to page 9
Clinical (Volume 11)
Restraint Minimisation and Safe Practice
Restraint Minimisation and Safe Practice
Table of Contents
Policy ......................................................................................................................................................
1
Purpose ..................................................................................................................................................
2
Scope/Audience .....................................................................................................................................
2
Associated documents ...........................................................................................................................
2
Definitions ..............................................................................................................................................
3
Restraint .............................................................................................................................................
3
Episode of Restraint ...........................................................................................................................
3
Chemical Restraint .............................................................................................................................
3
Categories of Restraint ..........................................................................................................................
3
Personal Restraint ..............................................................................................................................
3
Physical Restraint ...............................................................................................................................
3
Environmental Restraint ....................................................................................................................
3
Seclusion ............................................................................................................................................
3
Exclusions to this Policy .........................................................................................................................
4
Clinical Responsibilities ..........................................................................................................................
4
Divisional Responsibilities ......................................................................................................................
5
Corporate Responsibilities .....................................................................................................................
5
Measurement/Evaluation ......................................................................................................................
6
References .............................................................................................................................................
6
Policy
Restraint is a serious clinical intervention used only as a last resort
to protect patients/consumers, others, or property, from harm.
The Canterbury DHB (CDHB) will meet the Restraint Minimisation
and Safe Practice Standard NZS 8134.2:2008 and all other relevant
legislation.
The CDHB is committed to:
Reducing the use of all forms of restraint
Ensuring that all restraint use is clinically justified
Ensuring restraint occurs for the least amount of time possible
The latest version of this document is available on the CDHB intranet/website only.
Printed copies may not reflect the most recent updates.
Authorised by: CMO
Issue Date: 14 January 2015
Ref 4631
Page
1 of
6
To be reviewed by: January 2017









Clinical (Volume 11)
Restraint Minimisation and Safe Practice
Ensuring restraint only occurs in a safe and respectful
manner under the direction and supervision of the most
appropriate Health Professionals
Purpose
To determine CDHB responsibilities and overarching processes
in relation to restraint.
Scope/Audience
The restraint of patients/consumers within CDHB Hospital and
Specialist Services under the direction and supervision of a
CDHB staff member who is registered with an authorising body.
Staff other than health professionals defined above may participate
in restraint episodes but only under the direction and supervision
of the most appropriate Health Professional.
Associated documents
CDHB Restraint Minimisation and Safe Practice SharePoint site
CDHB Restraint Minimisation and Safe Practice Self Directed
Learning Package
CDHB Restraint Minimisation and Safe Practice
Resource/Guidance
CDHB Restraint Minimisation and Safe Practice
Responsibilities
Older Person’s Health and Rehabilitation Restraint
Minimisation and Safe Practice Resource
Child Health Restraint Minimisation and Safe Practice Self
Directed Learning Package
NZS 8143.2:2008 Restraint Minimisation and Safe Practice
standard
Specialist Mental Health Services Restraint and Seclusion
policy and procedure
Personal Limb Holder or Soft Limb Restraint Policy –
Medical Surgical volume A
Psychiatric Services for Elderly and Specialist Mental
Health Services Seclusion Observation forms
Physical Restraint Monitoring forms
The latest version of this document is available on the CDHB intranet/website only.
Printed copies may not reflect the most recent updates.
Authorised by: CMO
Issue Date: 14 January 2015
Ref 4631
Page
2 of
6
To be reviewed by: January 2017
Clinical (Volume 11)
Restraint Minimisation and Safe Practice
Definitions
Restraint
The use of any intervention, by a service provider, that limits
a patient’s/consumer’s normal freedom of movement.
Episode of Restraint
For the purposes of restraint documentation and evaluation, a
restraint episode refers to a single restraint event, or, where restraint
is used as a planned regular intervention and is identified in the
consumer’s service delivery plan, a restraint episode may refer to a
grouping of restraint events.
Chemical Restraint –
PLEASE NOTE Chemical restraint is not
condoned by the CDHB and is considered abuse.
The use of medication solely for the purpose of limiting a
patient’s/consumer’s freedom of movement or to render them
incapable of resistance is considered chemical restraint.
Categories of Restraint
Personal Restraint
Where a service provider uses their own body to intentionally
limit the movement of a patient/consumer. For example, where a
consumer is held by a service provider.
Physical Restraint
Where a service provider uses equipment, devices or furniture that
limits the patient’s/consumer’s normal freedom of movement. For
example, where a patient/consumer is unable to independently get
out of a chair due to: the design of the chair; the use of a belt; or
the position of a table or fixed tray.
Environmental Restraint
Where a service provider intentionally restricts a
patient’s/consumer’s normal access to their environment. For
example, where a patient’s/consumer’s normal access to their
environment is intentionally restricted by locking devices on doors
or by having their normal means of independent mobility (such as a
wheelchair) denied.
Seclusion
Where a patient/consumer is placed alone in a room or area, at
any time and for any duration, from which they cannot freely exit.
The latest version of this document is available on the CDHB intranet/website only.
Printed copies may not reflect the most recent updates.
Authorised by: CMO
Issue Date: 14 January 2015
Ref 4631
Page
3 of
6
To be reviewed by: January 2017

Clinical (Volume 11)
Restraint Minimisation and Safe Practice
Seclusion is a specific type of Environmental Restraint and can only
be legally implemented for patients/consumers who are under the
Mental Health (Compulsory Assessment and Treatment) Act1992 or
the Intellectual Disability (Compulsory Care and Rehabilitation) Act
2003. Seclusion only occurs in approved and designated seclusion
rooms.
Exclusions to this Policy
1. The use of Enablers which are equipment, devices or furniture,
voluntarily used by a patient/consumer following appropriate
assessment, that limits normal freedom of movement, with the
intent of promoting independence, comfort and/or safety.
Please note: Both enablers and restraint limit a
patient’s/consumer’s normal freedom of movement; it is not the
properties of the equipment, device or furniture that determines
whether or not it is an enabler or restraint but rather the intent
of the intervention and more importantly whether it is voluntarily
used by the consumer/patient.
An enabler can become a restraint if it is not removed when
the consumer/patient requests i.e. the enabler ceases to be
voluntarily used.
2. Environmental isolation and/or detainment of patients/consumers
for infection prevention and control purposes. Refer to the
Canterbury DHB intranet for Volume 10, Infection Prevention
and Control manual.
3. The restraint of patients/consumers who are prisoners for
security purposes. Refer to the Canterbury DHB intranet
Volume 11, Patients who are Prisoners policy.
4. The restraint of patients/consumers being transported and
subject to specific provisions under The Mental Health
(Compulsory Assessment and Treatment) Act 1992 or The
Intellectual Disability (Compulsory Care and Rehabilitation) Act
2003.
Clinical Responsibilities
The following are clinical activities and decisions which are to be
undertaken by the most appropriate Health Professional/s:
Undertaking a Restraint Minimisation and Safe
Practice Assessment
Making the decision to use restraint
Monitoring and documenting the consumer’s/patient’s health
and wellbeing during the restraint episode
The latest version of this document is available on the CDHB intranet/website only.
Printed copies may not reflect the most recent updates.
Authorised by: CMO
Issue Date: 14 January 2015
Ref 4631
Page
4 of
6
To be reviewed by: January 2017

Clinical (Volume 11)
Restraint Minimisation and Safe Practice
Monitoring the consumer’s/patient’s ongoing need for restraint
and ensuring restraint is used for the least amount of time
Making the decision to cease using restraint
Undertaking an evaluation of the restraint episode in
collaboration with the patient/consumer, including future
options to avoid restraint
Reporting the restraint episode on the CDHB Incident
Management System ‘Safety 1st (in services where ‘Safety 1st ‘
is yet to be deployed staff are to report restraint on their
divisional restraint reporting form until such time as Safety 1st is
deployed).
Documenting the restraint episode in Safety 1st and
in patient’s/consumer’s clinical record
Divisional Responsibilities
The following reponsibilites are largely undertaken by the division
Restraint Monitoring Committees:
Maintaining approved Restraint Minimisation and Safe
Practice procedures - approval is through the CDHB Restraint
Approval and Monitoring Group
Promoting the intent of the Restraint Minimisation and
Safe Standards and CDHB policy
Monitoring compliance with the Restraint Minimisation and
Safe Practice Standard and CDHB policy
Providing or facilitating approved education appropriate to
clinical settings - approval is through the CDHB Restraint
Approval and Monitoring Group
Providing representation on the CDHB Restraint Approval
and Monitoring Group
Monitoring the use of restraint in the division
Providing bi-annual reports on the use of restraint to the
CDHB Restraint Approval and Monitoring Group
Corporate Responsibilities
The following responsibilities are largely undertaken by the CDHB
Restraint Approval Monitoring Group and the CDHB Nurse Co-
ordinator Restraint Minimisation and Safe Practice
Organisational-wide restraint Minimisation and Safe Practice
policy
The latest version of this document is available on the CDHB intranet/website only.
Printed copies may not reflect the most recent updates.
Authorised by: CMO
Issue Date: 14 January 2015
Ref 4631
Page
5 of
6
To be reviewed by: January 2017

Clinical (Volume 11)
Restraint Minimisation and Safe Practice
The approval and review of all forms of restraint, restraint
education, restraint policy and restraint procedures across
the CDHB.
Maintaining an approved restraints database and 2 yearly review
Providing Restraint Minimisation and Safe Practice advice and
leadership
Assisting in the review of restraint issues/adverse events
Ensuring appropriate Restraint Minimisation and Safe Practice
guidance is readily available
Monitoring and Quality review of restraint use
Measurement/Evaluation
Evaluation of every episode of restraint
Monitoring of restraint data by the divisional Restraint
Monitoring Committees
Biannual Divisional Restraint Monitoring Committee reports to
RAMG
Biannual reports to the Clinical Board supplied by the Nurse
Co-ordinator Restraint Minimisation and Safe Practice on behalf
of the Restraint Approval and Monitoring Group
Safety 1st reports
References
NZS 8143.2:2008 Restraint Minimisation and Safe
Practice standard
The Mental Health (Compulsory Assessment and Treatment)
Act 1992
The Intellectual Disability (Compulsory Care and Rehabilitation)
Act 2003
Memorandum of Understanding between the Ministry of
Justice and the Ministry of Health
Policy Owner
Restraint Approval and Monitoring Group
Policy Authoriser
Chief Medical Officer or Executive Director of Nursing on
behalf of Clinical Board
Date of Authorisation
January 2015
The latest version of this document is available on the CDHB intranet/website only.
Printed copies may not reflect the most recent updates.
Authorised by: CMO
Issue Date: 14 January 2015
Ref 4631
Page
6 of
6
To be reviewed by: January 2017
Document Outline